Abstract
Background
The teach-back method, also known as the “show-me” method, has been endorsed by many medical and health care societies. However, limited investigation has been conducted regarding its association with patient outcomes.
Objectives
To examine the association between patient teach-back experience and the risk of hospitalizations and length of hospital stay among patients with ambulatory care sensitive conditions (ACSCs).
Design
A matched cohort study.
Setting
Data from the 2011–2015 Longitudinal Medical Expenditure Panel Survey (panels 16–19).
Participants
Three thousand nine hundred ninety-four US adults aged ≥ 18 years with any of 5 ACSCs (hypertension, type 2 diabetes, heart disease, asthma, and chronic obstructive pulmonary disease [COPD]).
Measurements
Hospital admissions (all-cause or ACSC-related) and the length of stay of the first admission were examined by teach-back during interaction with a health provider.
Results
Patients with teach-back experience were less likely to experience hospitalization for an ACSC-related condition (relative risk, 0.85; 95% CI, 0.71 to 0.99) and had a lower risk for a condition-related readmission (hazard ratio, 0.77; 95% CI, 0.60 to 0.99), compared with those without teach-back experience. The median length of hospital stay did not differ between patients with teach-back experience and those without teach-back experience (median 3 days [IQR 1 to 8 days] and median 3 days [IQR 0 to 8 days], respectively; P = 0.84). Subgroup analysis showed that the association of reported teach-back experience on the outcomes was relatively stable among those with hypertension, diabetes, and heart disease, but was not among those with asthma or COPD.
Limitation
Teach-back exposure relied on patient self-reported information.
Conclusions
Our findings suggest that patient teach-back method is associated with reduced risk of hospitalization for those with ACSCs, especially among patients with cardiovascular diseases and type 2 diabetes. Encouraging providers to utilize the teach-back method at every visit has the potential to further reduce hospitalizations for individuals with ACSCs.
Electronic supplementary material
The online version of this article (10.1007/s11606-019-05135-y) contains supplementary material, which is available to authorized users.
INTRODUCTION
Unnecessary hospitalizations and readmissions drive spending growth and reportedly constitute one-third of the nation’s total health care expenditures in the USA.1,2 Approximately 15% of total hospital admissions in the USA are for ambulatory care sensitive conditions (ACSCs).3 ACSCs refer to conditions for which hospitalizations could be prevented or reduced through appropriate management in primary care.4,5 Empirical studies have demonstrated that timely and effective care delivery could help to reduce the risks of the unnecessary hospitalization for ACSCs.5–7 However, interventions that are employed among patients with ACSCs to improve health outcomes have had limited success in clinical settings.
A technique to improve patient health literacy known as the “teach-back” has been promoted by national agencies with the goal of improving health outcomes.8–10 The teach-back method is intended to enhance and assess patient engagement and knowledge during a clinical encounter, by creating an interactive communication loop between provider and patient.11 In this method, health care providers ask patients to describe (or repeat back) in their own words what they need to know or do pertaining to their health conditions, creating an immediate opportunity for providers to assess patient understanding and intervene with education.8,12 This approach facilitates patient-centered communication13 and helps providers to close the “loop” by assessing patients’ comprehension and recall, thereby, promoting adherence.11
This interactive communication approach is also linked with healthier outcomes including better self-management skills among patients with chronic conditions.14 Preliminary studies report that patient teach-back can reduce hospital readmissions by 4–12% for those at high risk of acute conditions.15–17 However, these studies were performed using data from local clinical settings and have limited generalizability. Moreover, no published study has examined the association between teach-back and hospital admission for ACSCs using nationally representative data. We sought to address these gaps via an analysis of the Longitudinal Medical Expenditure Panel Survey with the following objectives: (1) describe the prevalence and demographic correlates of teach-back experience in US adults with ACSCs and (2) assess whether patient-reported teach-back is associated with a reduced risk of hospitalization.
METHODS
Study Design and Data
We conducted a retrospective matched cohort study using data from the 2011–2015 Longitudinal Medical Expenditure Panel Survey (MEPS). The MEPS is a well-established source of national data on access to health services, health care utilization, and health care expenditures.18 Medical conditions of MEPS respondents are collected in a narrative form and then coded by trained coders using the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes. The Clinical Classification Category (CCC) codes—clinically meaningful combinations of ICD-9-CM codes classified into 274 mutually exclusive categories created by AHRQ—are also provided in the MEPS data.19 We used 5 years of overlapping MEPS Longitudinal Survey data (2011–2015; panels 16–19). For each panel, we merged data from Medical Conditions19 and Hospital Inpatient Stay Files20 using a unique person identifier. This study used deidentified and publicly available data and was deemed exempt from review by the University of Florida institutional review board.
Study Cohort: Ambulatory Care Sensitive Conditions
Our initial analytic sample included 24,296 US adults aged 18 years or older with any of the following 5 ACSCs: (1) hypertension, (2) type 2 diabetes, (3) heart disease, (4) asthma, and (5) chronic obstructive pulmonary disease (COPD).21 We used a two-step approach to identify participants with ACSCs. First, we identified these ACSCs using patient self-reported data on medical conditions. Participants who responded “Yes” to one or more of the following question “Have you ever been told by a doctor or other health professional that you had the health condition?” for hypertension, type 2 diabetes, heart disease (coronary heart disease, angina, myocardial infarction, and other unspecified heart disease), asthma, or COPD (emphysema and chronic bronchitis) were identified. Next, we validated ACSC among these participants using specific ICD-9-CM or CCC. A full list of these codes appears in Online Appendix Table 1. Having identified individuals with ACSCs, we further excluded patients if (1) they reported never receiving instructions about a specific illness or health condition (n = 2087) because receiving instruction from a health care provider is a prerequisite to having teach-back experience, (2) the patient was a pregnant female at the time of survey (n = 2273) due to the likelihood of hospital admission for delivery, (3) the patient was diagnosed with any cancer (n = 2185), because they may have unusual patterns of health services use due to severe conditions, or (4) the health services utilization data were missing (n = 3641).
Main Exposure: Patient-Reported Teach-Back Experience
After identifying the initial ACSC cohort, we determined their exposure to teach-back. For this purpose, we used a question from the Consumer Assessment of Healthcare Providers and Systems (CAHPS®), which measures the patient’s perceived quality of health care services received in the last 12 months.22 Teach-back experience was assessed and categorized according to patients’ response to the CAHPS® question asking, “How often doctors or other health providers asked you to describe how you are going to follow their instructions?” Individuals were defined as having the teach-back experience if they responded that they “always” received a teach-back. The question is administered once and it represents a summative assessment of all visits in the past 12 months. This definition of teach-back exposure is similar to that recommended by the AHRQ and used in previous studies to track teach-back 8,23. ACSC patients who responded to the question otherwise were considered not exposed, making the conservative assumption that a patient derived no benefit from the teach-back experience if they were not exposed to the teach-back technique. After identifying patients with teach-back experience, our total cohort included 14,110 patients with ACSCs.
Outcomes: Hospital Admission
Our primary outcome of interest was hospital admission during year 2 of follow-up (panel rounds 3–5). We identified and classified hospital admissions into two types: (1) “all-cause” which included hospital admission for any reason and (2) “ACSC-related” which included hospital admission with primary cause of visit listed as an ACSC condition. Secondary outcomes included (1) a second admission within 12 months of discharge of the first hospital admission and (2) length of stay (i.e., time from hospitalization until discharge) to assess the severity of exacerbation. Given the acuity of ACSCs3–5 and more than 95% of those hospitalized were discharged within 30 days, we censored those having more than 30 days of inpatient stay.
Individual Characteristics
Demographic and health characteristics that may affect health services utilization and confound the relationship between teach-back experience and hospital admission were included as covariates.24,25 These included age, sex, race/ethnicity, education, family income level, employment, marital status, census region, health insurance type, having a usual source of care, general health status, the SF-12 Physical and Mental Summary scores, current smoking status, and obesity (defined as a body mass index greater than 29.9 kg/m2).
Matching
Each patient with an ACSC and with teach-back experience was statistically matched with a similar patient who did not have the teach-back experience. Participant matching was performed using the nearest-neighbor propensity score matching technique to match teach-back individuals to control individuals.26 Propensity scores were computed using baseline individual characteristics listed above and the panel numbers. The variables in the propensity score model were selected using a stepwise procedure to predict the probability of having the teach-back experience.
Statistical Analysis
Baseline cohort characteristics were described using proportions and means as appropriate. We tested for statistically significant differences in demographics and health status by teach-back experience using a chi-square or Fisher’s exact test for categorical variables and t tests for continuous variables. We used Poisson regression models to test whether teach-back experience was associated with hospital admission (for all-cause as well as ACSC-related condition). The association between teach-back experience and duration of the first hospital admission was estimated using Kaplan-Meier survival curves, and the statistical significance of differences by teach-back experience was determined using the log rank test.27 The association between teach-back experience and risk of second admission within 12 months of initial hospital discharge was estimated using Cox proportional hazards models.
We also tested the sensitivity of results to the operational definition of teach-back experience. First, patients were defined as being exposed to the teach-back experience if they reported “usually” and “sometimes” having a teach-back (rather than just “always”, as in the primary analyses). Sensitivity analysis was also conducted to evaluate the effect of English proficiency and for this purpose we excluded those who were not born in the USA and having difficulties in communication using English. We also performed subgroup analyses to examine the differences in the outcome measures by the five specific ACSCs and combination of more than one ACSC; individuals were matched according to the specified ACSCs separately. We used an alpha level of 0.05. The PROC SURVEY in SAS® (9.4, SAS Institute) and Complex Survey procedures in SPSS (24, IBM) were used for analyses accounting for the MEPS sampling weights and the complex survey design.
RESULTS
Patterns of Teach-Back Experience Among ACSC Patients
In the sample of 14,110 ACSC patients (pooled weighted N = 76,664,359), 26.7% (95% CI, 25.4–27.7%; 19.8 million) reported having a teach-back experience at each care visit. Nearly one-third (30.8%, 95% CI, 29.5–32.0%; 22.9 million) reported never having a teach-back experience during interaction with their health care providers.
The prevalence of patient-reported teach-back experience by demographic and health-related characteristics is summarized in Table 1. ACSC patients who reported having a teach-back experience at each visit statistically significantly differed from those who did not report a teach-back experience. We observed differences in sex, race/ethnicity, educational attainment, and type of health insurance.
Table 1.
National Patterns in Teach-Back Experience by Demographic and Health-Related Characteristics of ACSC Patients, MEPS 2011–2015
| Characteristics | Teach-back/total*, unweighted | Teach-back/totala, weighted | Prevalence % (95% CI)† | P value |
|---|---|---|---|---|
| Age group (years) | 0.16 | |||
| 18–34 | 469/1680 | 2,069,158/8,446,339 | 24.5 (21.6–27.4) | |
| 35–44 | 476/1721 | 1,973,279/8,402,815 | 23.5 (20.9–26.1) | |
| 45–54 | 907/2903 | 4,149,342/14,928,010 | 27.8 (25.8–29.8) | |
| 55–64 | 993/3381 | 4,777,220/18,401,672 | 26.0 (24.0–27.9) | |
| 65–74 | 759/2553 | 3,773,172/14,653,576 | 25.7 (23.4–28.1) | |
| 75+ | 559/1872 | 3,065,563/11,831,947 | 25.9 (23.3–28.5) | |
| Sex | < .001 | |||
| Male | 1805/5965 | 9,443,342/34,460,428 | 27.4 (25.8–29.0) | |
| Female | 2358/8145 | 10,364,391/42,203,931 | 24.6 (23.3–25.8) | |
| Race/ethnicity | < .001 | |||
| Non-Hispanic White | 1678/7233 | 12,945,134/56,617,713 | 22.9 (21.6–24.2) | |
| Non-Hispanic Black | 1173/3076 | 3,078,090/8,311,346 | 37.0 (34.7–39.4) | |
| Hispanic | 967/2660 | 2,520,969/7,172,852 | 35.1 (32.6–37.7) | |
| Non-Hispanic Asian | 244/784 | 785,226/2,655,026 | 29.6 (25.2–34.0) | |
| Other/multiple group | 95/337 | 454,456/1,825,044 | 24.9 (18.9–30.9) | |
| Education | < .001 | |||
| Less than high school | 1048/2641 | 3,285,579/9,152,502 | 35.9 (33.2–38.5) | |
| High school/GED | 1248/4049 | 5,959,342/21,025,358 | 28.3 (26.4–30.3) | |
| Some college | 1105/3995 | 5,668,660/23,160,109 | 24.5 (22.8–26.2) | |
| 4-year college or higher | 762/3425 | 4,894,152/23,326,390 | 21.0 (19.3–22.6) | |
| Family income | < .001 | |||
| Poor | 1130/3392 | 3,834,831/13,045,232 | 29.4 (27.2–31.5) | |
| Low income | 739/2162 | 2,835,991/9,698,936 | 29.2 (26.5–32.0) | |
| Middle income | 1168/4023 | 5,639,736/21,905,460 | 25.7 (23.9–27.6) | |
| High income | 1126/4533 | 7,497,176/32,014,731 | 23.4 (21.7–25.1) | |
| Marital status | 0.03 | |||
| Not married | 2065/6535 | 8,524,767/31,605,423 | 27.0 (25.7–28.3) | |
| Married | 2098/7575 | 11,282,966/45,058,936 | 25.0 (23.6–26.5) | |
| Employment | 0.21 | |||
| Not employed | 2111/6807 | 9,288,217/34,999,491 | 26.5 (25.0–28.1) | |
| Employed | 2052/7303 | 10,519,516/41,664,868 | 25.2 (23.8–26.7) | |
| Census region | 0.84 | |||
| Northeast | 711/2366 | 3,618,853/14,014,888 | 25.8 (22.7–28.9) | |
| Midwest | 809/2889 | 4,566,881/17,702,912 | 25.8 (23.7–27.9) | |
| South | 1636/5432 | 7,359,999/29,003,477 | 25.4 (23.7–27.0) | |
| West | 1007/3423 | 4,262,000/15,943,083 | 26.7 (24.4–29.1) | |
| Health insurance | < .001 | |||
| Private | 2235/8395 | 12,675,117/52,250,159 | 24.3 (23.0–25.5) | |
| Public | 1567/4562 | 5,931,438/19,793,824 | 30.0 (27.9–32.0) | |
| Uninsured | 361/1153 | 1,201,179/4,620,376 | 26.0 (22.7–29.3) | |
| Having usual source of care provider | 0.34 | |||
| No | 345/1248 | 1,473,368/6,057,910 | 24.3 (20.9–27.7) | |
| Yes | 3775/12,708 | 18,167,606/69,892,325 | 26.0 (24.9–27.1) | |
| General health status | 0.78 | |||
| Fair to poor | 1253/4101 | 4,647,346/18,133,117 | 25.6 (23.9–27.3) | |
| Excellent to good | 2909/9999 | 15,156,413/58,483,793 | 25.9 (24.6–27.2) | |
| Smoking | 0.25 | |||
| No | 3386/11,648 | 16,445,488/64,249,233 | 25.6 (24.4–26.8) | |
| Yes | 698/2242 | 3,088,467/11,451,180 | 27.0 (24.9–29.1) | |
| Obesity | < .001 | |||
| No | 2375/8341 | 11,593,887/46,887,361 | 24.7 (23.4–26.0) | |
| Yes | 1788/5769 | 8,213,846/29,776,998 | 27.6 (25.9–29.3) | |
| High blood pressure | < .001 | |||
| No | 1232/4737 | 6,387,541/27,641,918 | 23.1 (21.5–24.7) | |
| Yes | 2930/9370 | 13,418,381/49,001,532 | 27.4 (26.0–28.8) | |
| Diabetes | < .001 | |||
| No | 3005/10,622 | 15,214,812/60,525,788 | 25.1 (23.9–26.4) | |
| Yes | 1158/3486 | 5,492,921/16,130,741 | 28.5 (26.5–30.4) | |
| Heart disease | 0.08 | |||
| No | 3064/10,252 | 14,264,819/54,012,404 | 26.4 (25.1–27.7) | |
| Yes | 1099/3858 | 55,542,914/22,651,955 | 24.5 (22.6–26.3) | |
| Asthma | 0.16 | |||
| No | 3337/11,318 | 16,208,111/61,953,245 | 26.2 (25.0–27.4) | |
| Yes | 825/2790 | 3,590,869/14,699,507 | 24.4 (22.2–26.7) | |
| COPD | 0.88 | |||
| No | 3825/12,984 | 18,216,705/70,452,239 | 25.9 (24.7–27.0) | |
| Yes | 338/1125 | 1,591,028/6,209,266 | 25.6 (22.6–28.6) | |
GED, general educational development; COPD, chronic obstructive pulmonary disease
*Teach-back includes patients with ambulatory care sensitive conditions (ACSCs) with teach-back experience; total includes total number of ACSC patients with the demographic or health-related characteristics
†Percentages represent US population estimates accounting for MEPS sampling weights and the complex survey design
Primary and Secondary Outcomes
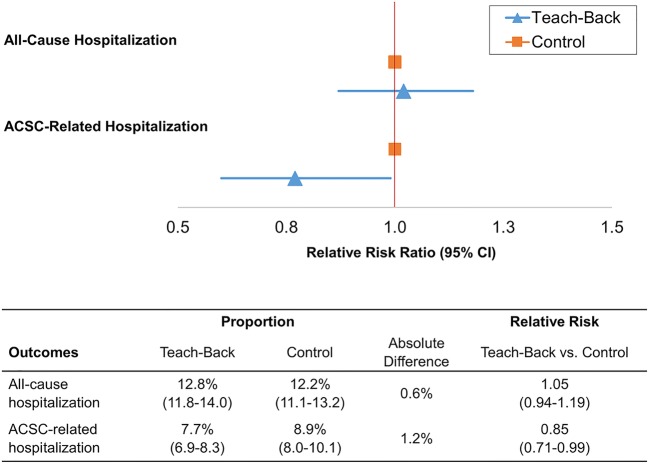
A total of 3994 ACSC patients with self-reported teach-back experience were successfully matched to patients without teach-back experience. Matching reduced standardized differences in all baseline characteristics below the absolute value of 10% (Online Appendix Figure). Statistically significant differences in observed patient demographics and health characteristics before matching were no longer statistically significant after matching (Table 2). In the sample of patients with teach-back experience matched to patients without teach-back experience, there were 511 hospital admissions among patients with teach-back experience (12.8%; 95% CI, 11.8–14.0%), compared with 483 hospital admissions among patients not reporting teach-back experience (12.2%; 95% CI, 11.1–13.2%) (Fig. 1).
Table 2.
Demographic and Health-Related Characteristics of Teach-Back Cohort Before and After Matching
| Prior to matching | After matching | ||||||
|---|---|---|---|---|---|---|---|
| Total | Teach-back | Control | P value | Teach-back | Control | P value | |
| Characteristics Sample no. | 14,110 | 4163 | 9947 | 3994 | 3994 | ||
| Age group (years), no. (%) | 0.10 | 0.48 | |||||
| 18–34 | 1680 (11.9) | 469 (11.3) | 1211 (12.2) | 458 (11.5) | 453 (11.3) | ||
| 35–44 | 1721 (12.2) | 476 (11.4) | 1245 (12.5) | 463 (11.6) | 460 (11.5) | ||
| 45–54 | 2903 (20.6) | 907 (21.8) | 1996 (20.1) | 867 (21.7) | 865 (21.7) | ||
| 55–64 | 3381 (24.0) | 993 (23.9) | 2388 (24.0) | 955 (23.9) | 977 (24.5) | ||
| 65–74 | 2553 (18.1) | 759 (18.2) | 1794 (18.0) | 719 (18.0) | 721 (18.1) | ||
| 75+ | 1872 (13.3) | 559 (13.4) | 1313 (13.2) | 532 (13.3) | 518 (13.0) | ||
| Sex, no. (%) | 0.09 | 0.85 | |||||
| Male | 5965 (42.3) | 1805 (43.4) | 4160 (41.8) | 1730 (43.3) | 1664 (41.7) | ||
| Female | 8145 (57.7) | 2358 (56.6) | 5787 (58.2) | 2264 (56.7) | 2330 (58.3) | ||
| Race/ethnicity, no. (%) | < .001 | 0.89 | |||||
| Non-Hispanic White | 7233 (51.3) | 1678 (40.4) | 5555 (55.9) | 1643 (41.1) | 1622 (40.6) | ||
| Non-Hispanic Black | 3076 (21.8) | 1173 (28.2) | 1903 (19.2) | 1090 (27.3) | 1110 (27.8) | ||
| Hispanic | 2660 (18.9) | 967 (23.3) | 1693 (17.0) | 931 (23.3) | 921 (23.1) | ||
| Non-Hispanic Asian | 784 (5.6) | 244 (5.9) | 540 (5.4) | 238 (6.0) | 237 (5.9) | ||
| Other/multiple group | 337 (2.4) | 95 (2.3) | 242 (2.4) | 92 (2.3) | 104 (2.6) | ||
| Education, no. (%) | < .001 | 0.80 | |||||
| Less than high school | 2641 (18.7) | 1048 (25.2) | 1593 (16.0) | 984 (24.6) | 989 (24.8) | ||
| High school/GED | 4049 (28.7) | 1248 (30.0) | 2801 (28.2) | 1187 (29.7) | 1155 (28.9) | ||
| Some college | 3995 (28.3) | 1105 (26.5) | 2890 (29.1) | 1075 (26.9) | 1100 (27.5) | ||
| Bachelor’s or beyond | 3425 (24.3) | 762 (18.3) | 2663 (26.8) | 748 (18.7) | 750 (18.8) | ||
| Family income, no. (%) | < .001 | 0.66 | |||||
| Poor | 3392 (24.0) | 1130 (27.1) | 2262 (22.7) | 1070 (26.8) | 1076 (26.9) | ||
| Low income | 2162 (15.3) | 739 (17.8) | 1423 (14.3) | 697 (17.5) | 696 (17.4) | ||
| Middle income | 4023 (28.5) | 1168 (28.1) | 2855 (28.7) | 1121 (28.1) | 1118 (28.0) | ||
| High income | 4533 (32.1) | 1126 (27.0) | 3407 (34.3) | 1106 (27.7) | 1104 (27.6) | ||
| Marital status, no. (%) | < .001 | 0.96 | |||||
| Not married | 6535 (46.3) | 2065 (49.6) | 4470 (44.9) | 1967 (49.2) | 1965 (49.2) | ||
| Married | 7575 (53.7) | 2098 (50.4) | 5477 (55.1) | 2027 (50.8) | 2029 (50.8) | ||
| Employment, no. (%) | < .001 | 0.64 | |||||
| Not employed | 6807 (48.2) | 2111 (50.7) | 4696 (47.2) | 2004 (50.2) | 1959 (49.0) | ||
| Employed | 7303 (51.8) | 2052 (49.3) | 5251 (52.8) | 1990 (49.8) | 2035 (51.0) | ||
| Census region, no. (%) | 0.22 | 0.35 | |||||
| Northeast | 2366 (16.8) | 711 (17.1) | 1655 (16.6) | 679 (17.0) | 681 (17.1) | ||
| Midwest | 2889 (20.5) | 809 (19.4) | 2080 (20.9) | 783 (19.6) | 745 (18.7) | ||
| South | 5432 (38.5) | 1636 (39.3) | 3796 (38.2) | 1557 (39.0) | 1630 (40.8) | ||
| West | 3423 (24.3) | 1007 (24.2) | 2416 (24.3) | 975 (24.4) | 938 (23.5) | ||
| Health insurance, no. (%) | < .001 | 0.88 | |||||
| Private | 8395 (59.5) | 2235 (53.7) | 6160 (61.9) | 2171 (54.4) | 2161 (54.1) | ||
| Public | 4562 (32.3) | 1567 (37.6) | 2995 (30.1) | 1477 (37.0) | 1496 (37.5) | ||
| Uninsured | 1153 (8.2) | 361 (8.7) | 792 (8.0) | 346 (8.7) | 337 (8.4) | ||
| Having usual source of care provider, no. (%) | 0.13 | 0.60 | |||||
| No | 1248 (8.9) | 345 (8.4) | 903 (9.2) | 337 (8.4) | 350 (8.8) | ||
| Yes | 12,708 (91.1) | 3775 (91.6) | 8933 (90.8) | 3657 (91.6) | 3644 (91.2) | ||
| General health status, no. (%) | 0.08 | 0.87 | |||||
| Fair to poor | 4101 (29.1) | 1253 (30.1) | 2848 (28.7) | 1187 (29.7) | 1193 (29.9) | ||
| Excellent to good | 9999 (70.9) | 2909 (69.9) | 7090 (71.3) | 2806 (70.3) | 2797 (70.1) | ||
| Health score (SF-12), mean (SD) | |||||||
| Physical component | 43.3 (12.2) | 43.4 (12.2) | 43.2 (12.2) | 0.34 | 43.4 (12.3) | 43.3 (12.0) | 0.69 |
| Mental component | 49.1 (11.0) | 50.5 (11.0) | 48.5 (10.9) | < .001 | 50.4 (11.1) | 50.3 (10.0) | 0.76 |
| Smoking, no. (%) | 0.05 | 0.79 | |||||
| No | 11,648 (83.9) | 3386 (82.9) | 8262 (84.3) | 3314 (83.0) | 3305 (82.7) | ||
| Yes | 2242 (16.1) | 698 (17.1) | 1544 (15.7) | 680 (17.0) | 689 (17.3) | ||
| Obesity, no. (%) | < .001 | 0.93 | |||||
| No | 8341 (59.1) | 2375 (57.1) | 5966 (60.0) | 2273 (56.9) | 2277 (57.0) | ||
| Yes | 5769 (40.9) | 1788 (42.9) | 3981 (40.0) | 1721 (43.1) | 1717 (43.0) | ||
| High blood pressure, no. (%) | < .001 | 0.82 | |||||
| No | 4737 (33.6) | 1232 (29.6) | 3505 (35.2) | 1192 (29.8) | 1171 (29.3) | ||
| Yes | 9370 (66.4) | 2930 (70.4) | 6440 (64.8) | 2802 (70.2) | 2823 (70.7) | ||
| Diabetes, no. (%) | < .001 | 0.82 | |||||
| No | 10,622 (75.3) | 3005 (72.2) | 7617 (76.6) | 2888 (72.3) | 2897 (72.5) | ||
| Yes | 3486 (24.7) | 1158 (27.8) | 2328 (23.4) | 1106 (27.7) | 1097 (27.5) | ||
| Heart disease, no. (%) | 0.10 | 0.78 | |||||
| No | 10,252 (72.7) | 3064 (73.6) | 7188 (72.3) | 2941 (73.6) | 2952 (73.9) | ||
| Yes | 3858 (27.3) | 1099 (26.4) | 2759 (27.7) | 1053 (26.4) | 1042 (26.1) | ||
| Asthma, no. (%) | 0.93 | 0.85 | |||||
| No | 11,318 (80.2) | 3337 (80.2) | 7981 (80.2) | 3203 (80.2) | 3210 (80.4) | ||
| Yes | 2790 (20.0) | 825 (19.8) | 1965 (19.8) | 791 (19.8) | 784 (19.6) | ||
| COPD, no. (%) | 0.68 | 0.90 | |||||
| No | 12,984 (92.0) | 3825 (91.9) | 9159 (92.1) | 3673 (92.0) | 3699 (92.6) | ||
| Yes | 1125 (8.0) | 338 (8.1) | 787 (7.9) | 321 (8.0) | 295 (7.4) | ||
GED, general educational development; SF-12, the 12-Item Short Form Health Survey; SD, standard deviation; COPD, chronic obstructive pulmonary disease
Figure 1.
Risk and proportion of ACSC patients having hospitalization. Parentheses indicate 95% confidence interval.
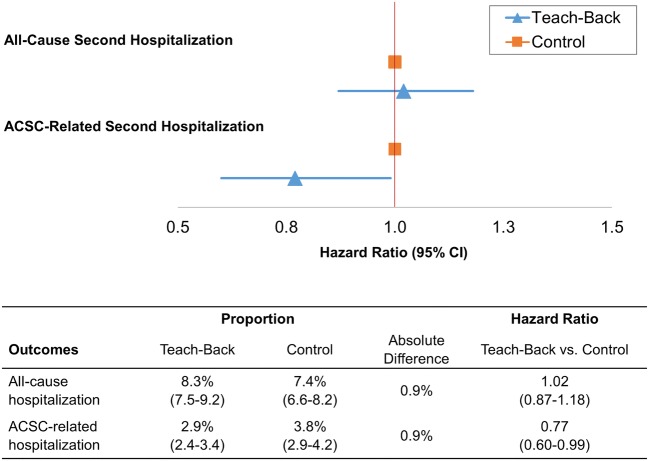
We initially estimated multivariate regression models and found no statistically significant difference in the likelihood of hospital admission or risk of second admission (P = 0.28 to 0.79; Online Appendix Table 2). After matching, patients with teach-back experience were less likely to experience hospitalization for ACSC-related condition (relative risk, 0.85; 95% CI, 0.71 to 0.99; Fig. 1) in year 2 and had a lower risk for ACSC-related second admission (hazard ratio, 0.77; 95% CI, 0.60 to 0.99; Fig. 2) within 12 months of the first hospitalization. We did not observe a statistically significant difference in risk of all-cause hospitalization by teach-back experience (P = 0.34 for the initial admission and P = 0.81 for the second).
Figure 2.
Risk and proportion of ACSC patients having a second hospitalization within 12 months. Parentheses indicate 95% confidence interval.
The median length of hospital stay did not statistically differ between patients reporting teach-back experience and those not reporting the experience (median 3 days, interquartile range [IQR; 1 to 8 days] and median 3 days, [IQR, 0 to 8 days], respectively; P = 0.84). Survival curves of hospital inpatient stay also suggested that teach-back experience was not associated with the length of stay for either all-cause or ACSC-related admission (P = 0.61 to 0.82) (Fig. 3).
Figure 3.
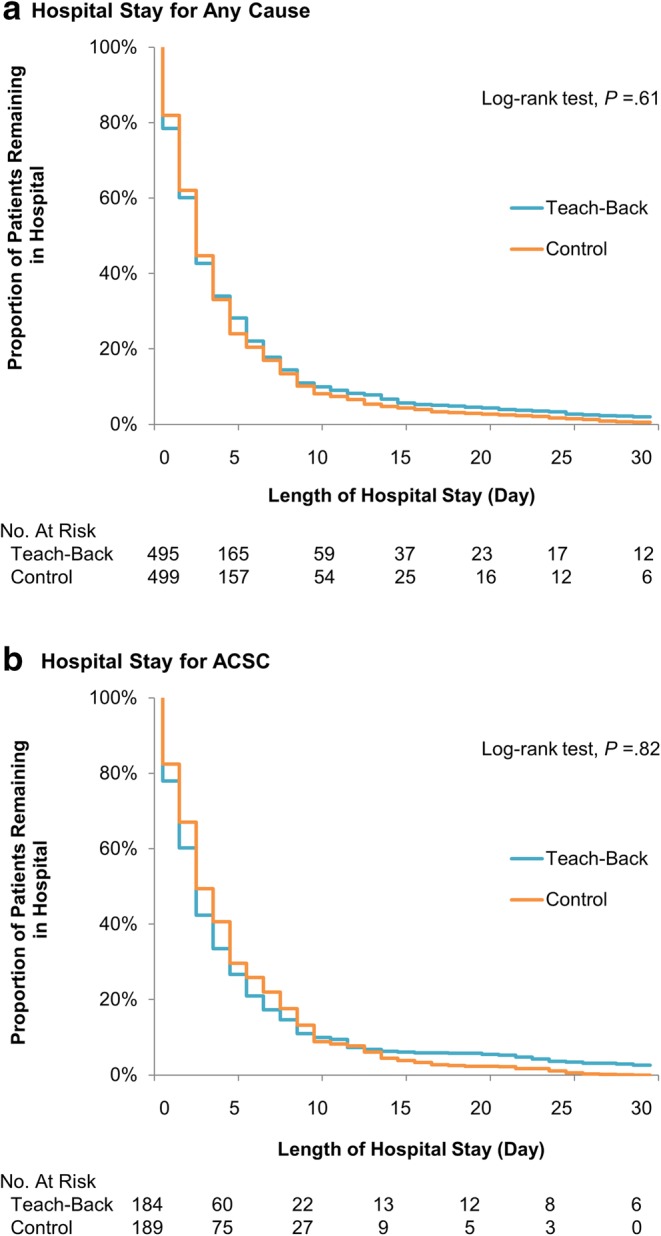
Kaplan-Meier curves for length of hospital stay: due to any cause (a) and ACSCs (b), stratified by teach-back exposure.
Sensitivity Analyses
We performed a sensitivity analysis on the primary outcomes by varying the definition of patient-reported teach-back exposure. We found no significant effect modification when including those answered “usually” or “sometimes” to the teach-back group. Differences in the risk for hospitalization for all-cause remained statistically insignificant and the effect estimates for ACSC-related admission remained relatively consistent with those of the main analysis, except for second hospitalization (when including those with “sometimes”, P = 0.17; Online Appendix Table 3). Exclusion of those not born in the USA and having difficulties in English communication had minimal effect on the outcomes. The results of sensitivity analysis based on English language proficiency are presented in Online Appendix Table 4.
Subgroup of ACSCs
In the subgroup analyses, we stratified outcomes by specific ACSC conditions and different combinations of ACSCs. Our findings varied by conditions, indicating that the association of the teach-back experience with the risk of hospitalization differs by type of ACSC. The association between teach-back and hospitalization among those with hypertension, diabetes, or heart disease was significant, but the effect estimates were not statistically significant among those with asthma or COPD (Online Appendix Table 5). Having diabetes and heart disease concurrently was found to be larger in magnitude of the effect than other combination of ACSCs (Online Appendix Table 6).
DISCUSSION
Our primary finding is that there is a significant association between reporting teach-back experience and hospital admission for ACSC-related conditions. Specifically, we found that patients with teach-back experience had 15% lower risk of being admitted (23% lower for repeated hospitalization) than those without. Although we expected that patient teach-back experience might be associated with decrease in length of inpatient stay as secondary outcome, no significant difference was observed between the teach-back and control groups. Our subgroup analysis also demonstrated that teach-back decreased risks of hospitalization among patients with hypertension (12% lower), type 2 diabetes (23% lower), and heart disease (36% lower risk of having a second admission), albeit no significant reduction among those with asthma and COPD. Taken together, our study suggests that this relatively simple “asking to explain back to me” technique is associated with reduced hospitalization for those with ACSCs, especially for those with cardiovascular disease and type 2 diabetes.
Our findings are consistent with previous studies examining the effect of teach-back on patient outcomes.12,15–17 In a cohort of patients hospitalized with heart failure (HF) (n = 469), Peter et al.15 found that patients who received an intensive teach-back strategy (3-day patient education during their stay) completed tests of knowledge of the disease and basic self-management skills after discharge effectively (90–94% correct responses) and had 12% lower readmission rates compared with those who did not receive teach-back. White et al.17 reported that integration of the teach-back method into practice improved the retention of health knowledge among elderly HF patients (aged ≥ 65 years). Similar to our findings, 30-day readmission rates for all-cause were not statistically different among those who received teach-back compared with those who did not (due to prevalent other chronic conditions among the elderly). However, the researchers found that there was relatively small number of the HF-specific readmissions (12.4% of total number of readmission) among patients answering teach-back questions correctly.17 It is possible that having teach-back experience may have improved the comprehension of diagnosed conditions, increased adherence to prescribed treatment/medication plans, and/or improved self-management care skills among ACSC patients evaluated in our study.8,12,28 This may result in better hospitalization outcomes among those with the experience.23,28 The teach-back method has the potential to improve provider-patient relationships by requiring providers to use patient-centered communication skills (e.g., paraphrasing, asking open-ended questions) that not only enhance patient knowledge/comprehension but facilitates trust between patient and provider.29–31 We also found that ACSC patients of racial/ethnic minorities or low socioeconomic status are more likely to report teach-back when receiving care. Collectively, the teach-back appears to be a viable intervention for those likely having low health literacy or limited English use from the standpoint of reducing health disparities gap, consistent with previous literature.23,32
Our subgroup analysis showed no association of the patient-reported teach-back experience with the hospitalization risk among those with asthma and COPD. A possible explanation for these findings is that patients with respiratory conditions may require rigorous patient education and “show-me” approach (for instance, demonstrating how to use an inhaler) to confirm patients’ ability to follow/perform given specific instruction,8 rather than simply asking to describe what to do. It has been estimated that a majority (up to 75%) of patients with asthma or COPD are not able to perform an inhalation technique correctly,33,34 due to inadequate understanding of instructions,35 complexity of use,34,35 and divergent techniques for different inhaler devices.35,36 Another possible explanation is that patients with COPD are at increased risk of developing heart disease37,38 and more than 50% of COPD patients hospitalized have coexisting cardiac diseases.39 Thus, it is possible that those with COPD are more likely experience an acute exacerbation of heart failure and hospitalization for cardiovascular events, rather than for COPD-related conditions.38,39
There are several limitations to this study and interpretation of the results warrants some caution. First, the exposure to teach-back was identified among patients who responded that they were always asked by their health care provider to describe how they were going to follow instructions; however, the teach-back method can be framed in multiple ways (e.g., open-ended questions).40 We were not able to measure how interactive the communication actually was between the patient and provider during a visit. Second, despite that we attempted to minimize the selection bias and possible confounding, it is still possible that other individual-level variables we were not able to capture may affect outcome measures or patients’ ability to follow the instructions given. Practice or health provider characteristics may affect interaction quality with patients,41 in particular the propensity of individual to report teach-back experience in this study. Third, although we pooled 5 years of data to enhance our sample size, subgroup samples of those with asthma and COPD were relatively small, compared with other ACSC subgroups. This may have resulted in insignificant statistical power for our analyses. Finally, some of clinical measures relied on self-reported information derived from individual interviews, subject to reporting biases. However, medical information in the MEPS is processed by professionally trained MEPS coders and verified by cross-checking with records obtained from providers and insurers.18–20 Despite these limitations, our study fills important gaps in the current literature regarding teach-back prevalence among ACSC population in the USA and its association with hospitalization risk.
Conclusions
About one-third of the ACSC patients do not ever report teach-back experience when seeking health care in the USA. Our findings suggest that having consistent patient-reported teach-back experience may lower the risk of hospitalization among patients with ACSCs, in particular, patients with cardiovascular disease and type 2 diabetes. Increased efforts towards the adoption of teach-back might reduce the burden of hospitalization among patients with certain ACSCs.
Electronic Supplementary Material
(DOCX 284 kb)
Acknowledgments
We thank Dr. Arch G. Mainous III, Florida Blue Endowed Professor of Health Administration at the University of Florida, for his review and comments on earlier copies of this manuscript. We also thank the JGIM Co-Editor-in-Chief, Dr. Jeffrey L. Jackson, and anonymous reviewers for their careful review and thoughtful feedback.
Authors’ Contribution
• Study conception and design: Hong, Sonawane, Cardel, Pavela, and Fisher
• Acquisition, analysis, or interpretation of data: All authors
• Drafting of manuscript: Hong
• Critical revision of the manuscript for important intellectual content: Hong, Sonawane, Cardel, Pavela, Fisher, and Deshmuk
• Statistical analysis: Hong, Sonawane, and Pavela
• Administrative, technical, or material support: Hong, Suk, and Vaughn
• Study supervision: Sonawane, Cardel, and Fisher
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hartman Micah, Martin Anne B., Espinosa Nathan, Catlin Aaron, The National Health Expenditure Acc National Health Care Spending In 2016: Spending And Enrollment Growth Slow After Initial Coverage Expansions. Health Affairs. 2018;37(1):150–160. doi: 10.1377/hlthaff.2017.1299. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Medicare and Medicaid Services. National Health Expenditure Data. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/index.html. Published 2018. Accessed 3 May 2019.
- 3.Fingar KR, Barrett ML, Elixhauser A, Stocks C, Steiner CA. Trends in Potentially Preventable Inpatient Hospital Admissions and Emergency Department Visits: Statistical Brief #195. Healthc Cost Util Proj Stat Briefs. 2015;(November):1–20. http://www.ncbi.nlm.nih.gov/pubmed/26741014. Accessed 11 Nov 2018. [PubMed]
- 4.Gao J, Moran E, Li Y-F, Almenoff PL. Predicting potentially avoidable hospitalizations. Med Care. 2014;52(2):164–171. doi: 10.1097/MLR.0000000000000041. [DOI] [PubMed] [Google Scholar]
- 5.Bindman AB, Grumbach K, Osmond D, et al. Preventable hospitalizations and access to health care. JAMA. 1995;274(4):305–311. doi: 10.1001/jama.1995.03530040033037. [DOI] [PubMed] [Google Scholar]
- 6.Roos LL, Walld R, Uhanova J, Bond R. Physician Visits, Hospitalizations, and Socioeconomic Status: Ambulatory Care Sensitive Conditions in a Canadian Setting. Health Serv Res. 2005;40(4):1167–1185. doi: 10.1111/j.1475-6773.2005.00407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yoon J, Yano EM, Altman L, et al. Reducing costs of acute care for ambulatory care-sensitive medical conditions: The central roles of comorbid mental illness. Med Care. 2012;50(8):705–713. doi: 10.1097/MLR.0b013e31824e3379. [DOI] [PubMed] [Google Scholar]
- 8.Agency for Healthcare Research and Quality. Health Literacy Universal Precautions Toolkit, 2nd Edition. http://www.ahrq.gov/professionals/quality-patient-safety/quality-resources/tools/literacy-toolkit/healthlittoolkit2-tool5.html. Published 2015. Accessed 3 May 2019.
- 9.National Quality Forum. Safe Practices for Better Healthcare–2010 Update: A Consensus Report. Washington, DC; 2010. http://www.qualityforum.org/Publications/2010/04/Safe_Practices_10_Full.aspx. Accessed 6 Apr 2018.
- 10.The Joint Commission. “What Did the Doctor Say?:” Improving Health Literacy to Protect Patient Safety. Oakbrook Terrace; 2007. https://www.jointcommission.org/assets/1/18/improving_health_literacy.pdf. Accessed 6 Apr 2018.
- 11.Schillinger D, Piette J, Grumbach K, et al. Closing the Loop. Arch Intern Med. 2003;163(1):83. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 12.Weiss B. Health Literacy and Patient Safety: Help Patients Understand. Chicago; 2007. https://med.fsu.edu/userFiles/file/ahec_health_clinicians_manual.pdf. Accessed 6 Apr 2018.
- 13.Badaczewski A, Bauman LJ, Blank AE, et al. Relationship between Teach-back and patient-centered communication in primary care pediatric encounters. Patient Educ Couns. 2017;100(7):1345–1352. doi: 10.1016/j.pec.2017.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dinh HTT, Bonner A, Clark R, Ramsbotham J, Hines S. The effectiveness of the teach-back method on adherence and self-management in health education for people with chronic disease: a systematic review. JBI Database System Rev Implement Rep. 2016;14(1):210. doi: 10.11124/jbisrir-2016-2296. [DOI] [PubMed] [Google Scholar]
- 15.Peter D, Robinson P, Jordan M, Lawrence S, Casey K, Salas-Lopez D. Reducing readmissions using teach-back: Enhancing patient and family education. J Nurs Adm. 2015;45(1):35–42. doi: 10.1097/NNA.0000000000000155. [DOI] [PubMed] [Google Scholar]
- 16.Darcy AM, Murphy GA, DeSanto-Madeya S. Evaluation of discharge telephone calls following total joint replacement surgery. Orthop Nurs. 2014;33(4):188–195. doi: 10.1097/NOR.0000000000000062. [DOI] [PubMed] [Google Scholar]
- 17.White M, Garbez R, Carroll M, Brinker E, Howie-Esquivel J. Is “Teach-Back” Associated With Knowledge Retention and Hospital Readmission in Hospitalized Heart Failure Patients? J Cardiovasc Nurs. 2013;28(2):137–146. doi: 10.1097/JCN.0b013e31824987bd. [DOI] [PubMed] [Google Scholar]
- 18.Cohen JW, Cohen SB, Banthin JS. The Medical Expenditure Panel Survey: a national information resource to support healthcare cost research and inform policy and practice. Med Care. 2009;47(7 Suppl 1):S44–50. doi: 10.1097/MLR.0b013e3181a23e3a. [DOI] [PubMed] [Google Scholar]
- 19.Agency for Healthcare Research and Quality. MEPS HC-180: 2015 Medical Conditions File. https://meps.ahrq.gov/mepsweb/data_stats/download_data_files_detail.jsp?cboPufNumber=HC-180. Published 2017. Accessed 3 May 2019.
- 20.Agency for Healthcare Research and Quality. MEPS HC-178D: 2015 Hospital Inpatient Stays File. https://meps.ahrq.gov/mepsweb/data_stats/download_data_files_detail.jsp?cboPufNumber=HC-178D. Published 2017. Accessed 3 May 2019.
- 21.Agency for Healthcare Research and Quality. Guide to Prevention Quality Indicators: Hospital Admission for Ambulatory Care Sensitive Conditions. Rockville; 2001. https://www.ahrq.gov/downloads/pub/ahrqqi/pqiguide.pdf. Accessed 3 May 2019.
- 22.Agency for Healthcare Research and Quality. MEPS HC-181 2015 Full Year Consolidated Data File. https://meps.ahrq.gov/mepsweb/data_stats/download_data_files_detail.jsp?cboPufNumber=HC-181. Published 2017. Accessed 3 May 2019.
- 23.Jager AJ, Wynia MK. Who gets a teach-back? patient-reported incidence of experiencing a teach-back. J Health Commun. 2012;17(SUPPL. 3):294–302. doi: 10.1080/10810730.2012.712624. [DOI] [PubMed] [Google Scholar]
- 24.Andersen RM, Davidson PL, Baumeister SE. Improving Access to Care. In: Changing the US Health Care System: Key Issues in Health Services Policy and Management. Jossey-Bass San Francisco; 2013:33–69.
- 25.Hong YR, Jo A, Mainous AG. Up-to-Date on Preventive Care Services Under Affordable Care Act: A Trend Analysis From MEPS 2007-2014. Med Care. 2017;55(8):771–780. doi: 10.1097/MLR.0000000000000763. [DOI] [PubMed] [Google Scholar]
- 26.Parsons LS. Reducing bias in a propensity score matched-pair sample using greedy matching techniques. http://www2.sas.com/proceedings/sugi26/p214-26.pdf. Published 2001. Accessed 3 May 2019.
- 27.Bland JM, Altman DG. The logrank test. BMJ. 2004;328(7447):1073. doi: 10.1136/bmj.328.7447.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Griffey RT, Shin N, Jones S, et al. The impact of teach-back on comprehension of discharge instructions and satisfaction among emergency patients with limited health literacy: A randomized, controlled study. J Commun Healthc. 2015;8(1):10–21. doi: 10.1179/1753807615Y.0000000001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mainous AG, Baker R, Love MM, Gray DP, Gill JM. Continuity of care and trust in one’s physician: evidence from primary care in the United States and the United Kingdom. Fam Med. 2001;33(1):22–27. [PubMed] [Google Scholar]
- 30.Hong YR, Tauscher J, Cardel M. Distrust in health care and cultural factors are associated with uptake of colorectal cancer screening in Hispanic and Asian Americans. Cancer. 2018;124(2):335–345. doi: 10.1002/cncr.31052. [DOI] [PubMed] [Google Scholar]
- 31.Hong YR, Holcomb D, Ballard M, Schwartz L. Multigroup Path Analysis of the Influence of Healthcare Quality, by Different Health Insurance Types. J Healthc Manag. 2017;62(2):93–105. doi: 10.1097/JHM-D-17-00008. [DOI] [PubMed] [Google Scholar]
- 32.DeWalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes. J Gen Intern Med. 2004;19(12):1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khassawneh BY, Al-Ali MK, Alzoubi KH, et al. Handling of inhaler devices in actual pulmonary practice: metered-dose inhaler versus dry powder inhalers. Respir Care. 2008;53(3):324–328. [PubMed] [Google Scholar]
- 34.Leiva-Fernández F, Leiva-Fernández J, Zubeldia-Santoyo F, García-Ruiz A, Prados-Torres D, Barnestein-Fonseca P. Efficacy of two educational interventions about inhalation techniques in patients with chronic obstructive pulmonary disease (COPD). TECEPOC: study protocol for a partially randomized controlled trial (preference trial) Trials. 2012;13(1):64. doi: 10.1186/1745-6215-13-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haughney J, Price D, Kaplan A, et al. Achieving asthma control in practice: Understanding the reasons for poor control. Respir Med. 2008;102(12):1681–1693. doi: 10.1016/j.rmed.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 36.Thomas M, Price D, Chrystyn H, Lloyd A, Williams AE, von Ziegenweidt J. Inhaled corticosteroids for asthma: impact of practice level device switching on asthma control. BMC Pulm Med. 2009;9(1):1. doi: 10.1186/1471-2466-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hawkins NM, Virani S, Ceconi C. Heart failure and chronic obstructive pulmonary disease: the challenges facing physicians and health services. Eur Heart J. 2013;34(36):2795–2807. doi: 10.1093/eurheartj/eht192. [DOI] [PubMed] [Google Scholar]
- 38.Roversi S, Fabbri LM, Sin DD, Hawkins NM, Agustí A. Chronic Obstructive Pulmonary Disease and Cardiac Diseases. An Urgent Need for Integrated Care. Am J Respir Crit Care Med. 2016;194(11):1319–1336. doi: 10.1164/rccm.201604-0690SO. [DOI] [PubMed] [Google Scholar]
- 39.Laratta CR, van Eeden S. Acute Exacerbation of Chronic Obstructive Pulmonary Disease: Cardiovascular Links. Biomed Res Int. 2014;2014:1–18. doi: 10.1155/2014/528789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.National Institute of Diabetes and Digestive and Kidney Diseases. How to Talk with Patients About Their Prediabetes Diagnosis: Use the Teach-back Method. https://www.niddk.nih.gov/health-information/communication-programs/ndep/health-professionals/game-plan-preventing-type-2-diabetes/how-talk-patients-about-prediabetes-diagnosis/use-teach-back-method. Accessed 3 May 2019.
- 41.Wallis CJ, Ravi B, Coburn N, Nam RK, Detsky AS, Satkunasivam R. Comparison of postoperative outcomes among patients treated by male and female surgeons: a population based matched cohort study. BMJ. 2017;359:1–10. doi: 10.1136/bmj.j4366. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 284 kb)