Abstract
Aim
To investigate the single nucleotide polymorphism (SNP) of A118G and its interaction with smoking and drinking on oesophageal squamous cell carcinoma (ESCC) risk.
Methods
A total of 960 subjects (545 males and 415 females) with a mean age of 58.1 ± 13.4 years were selected, including 490 ESCC patients and 470 normal control subjects. A logistic regression model was used to examine the association between A118G and ESCC and its interaction with A118G and current smoking and drinking. The odds ratio (OR) and 95% confident interval (95%CI) were calculated.
Results
The frequency for the A allele of A118G was significantly higher in ESCC cases, OR (95%CI) = 1.22 (1.08–1.59). Logistic regression analysis showed a significant association between the A allele in A118G and increased ESCC risk. The ESCC risk was significantly higher in carriers of the A allele of the A118G polymorphism than those with GG (AG + AA vs. GG, adjusted OR (95%CI) = 1.20 (1.05–1.53)). We found that current smokers with AG or AA of the A118G genotype have the highest ESCC risk compared with never smokers with a GG genotype; the OR (95%CI) was 2.57 (1.66–3.33). Current drinkers with AG or AA of the A118G genotype have the highest ESCC risk compared with not currently drinking subjects with the GG genotype, OR (95%CI) = 2.36 (1.47–3.25), after adjusting for covariates.
Conclusion
The A allele of A118G and ESCC and additional interaction between the A allele of A118G and smoking or drinking were associated with increased ESCC risk.
Keywords: A118G, alcohol consumption, interaction, oesophageal squamous cell carcinoma, polymorphism, smoking
Introduction
Oesophageal squamous cell carcinoma (ESCC) is the sixth most common cause of cancer‐related death worldwide. ESCC is also a predominant histological subtype of oesophageal cancer and is characterised by a high mortality rate in China 1, 2. It is usually diagnosed at a relatively late stage, and treatment options are limited; the 5‐year survival rate for ESCC patients has been very low 3. Previous studies have determined several genetic factors for ESCC 4, 5, 6; however, the precise molecular mechanisms of carcinogenesis and progression are not well known. Thus, the identification of target genes for the determination of tumour development is urgently required for ESCC diagnosis and treatment.
Epidemiologic studies have suggested that patients who receive general anaesthesia with opioids rather regional anaesthetics are at higher risk of cancer recurrence 7, 8. Furthermore, in addition to the analgesic effect, μ‐opioid receptor activation may influence tumour growth and cancer progression 9. Several genetic variants have been identified within the μ‐opioid receptor gene 10. The most common and well‐known genetic variant is the single nucleotide polymorphism (SNP) A118G. However, no previous studies have focused on the impact of A118G polymorphism; additional interactions with environmental factors, such as smoking and alcohol consumption on ESCC risk, also remain to be conducted. Thus, the aim of this study was to investigate the impact of SNP of A118G and additional interactions with current smoking and drinking on ESCC risk in a Chinese population.
Materials and Methods
Subjects
This was a case‐controlled study on ESCC. Chinese patients with ESCC were consecutively recruited between March 2010 and September 2013 from Yixing People's Hospital. A total of 960 subjects (545 males, 415 females) with a mean age of 58.1 ± 13.4 years were selected, including 470 ESCC patients and 490 normal control subjects. All cases were confirmed via histopathological diagnosis. The subjects who received chemotherapy or radiotherapy prior to surgery were excluded from this study. Healthy controls were randomly selected from a population screening programme for risk factors of ESCC in the same regions and matched to cases on the basis of age (±3 years) and gender (Fig. 1). Blood samples were collected from each participant. Detailed personal information on demographic characteristics and smoking and drinking status were collected via interview. At recruitment, written informed consent was obtained from each participant.
Figure 1.
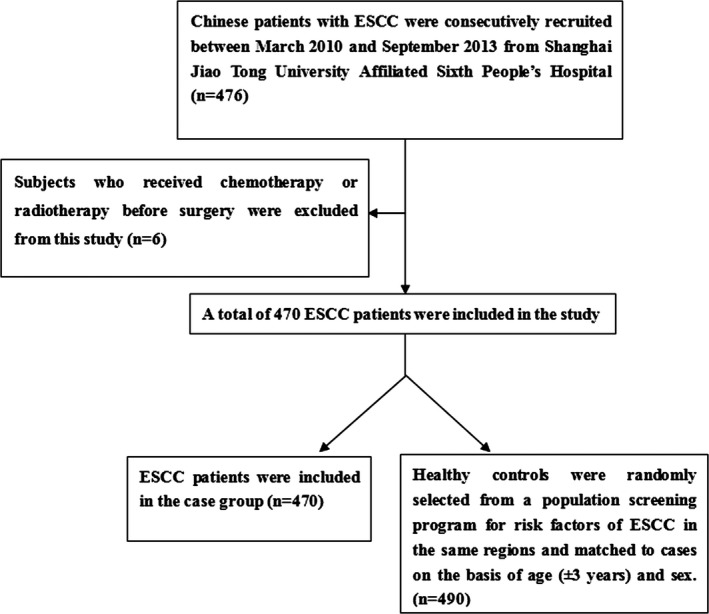
A flowchart of study population selection.
Body Measurements
Data on demographic information, diet, smoking, and drinking information for all participants were obtained using a standard questionnaire administered by trained staff. We defined current alcohol consumption as more than one drink of any type per month or not currently drinking as <1 drink of any type per month 11; current smokers were defined as those who have smoked at least 100 cigarettes and still smoked at the time of the interview; individuals with no history of cigarette smoking were considered to be never smokers 12, 13. A low‐fibre diet and high‐fat diet were defined according to the “Dietary Pyramid” 14. Body weight, height, and waist circumference (WC) were also measured according to standardised procedures 15. Body mass index (BMI) was calculated as weight in kilograms divided by the square of the height in metres. Blood samples were collected in the morning after at least 8 hr of fasting. All plasma and serum samples were frozen at –80°C until laboratory testing.
Genomic DNA Extraction and Genotyping
Approximately 2 ml of whole blood was collected from all participants in sterile EDTA‐coated vacutainers. Genomic DNA from participants was extracted from EDTA‐treated whole blood using the DNA Blood Mini Kit (Qiagen, Hilden, Germany) according to the manufacturer's instructions and stored at −80°C until used for genotyping. Genotyping of A118G SNP (rs1799971) was performed using the TaqMan platform produced by the BGI Company, China. Genotyping was repeated on a 10% random sample of study participants, and the results were 100% concordant. ABI Prism7000 software (Applied Biosystems, Carlsbad, CA) and an allelic discrimination procedure were used for genotyping. A 25‐μl reaction mixture included 1.25 μl SNP Genotyping Assays (20×), 12.5 μl Genotyping Master Mix (2×), 20 ng DNA, and conditions as follows: initial denaturation for 10 min and 95°C, denaturation for 15 sec and 92°C, and annealing and extension for 90 sec and 60°C (50 cycles).
Statistical Analysis
The mean and standard deviation (SD) were calculated for normally distributed continuous variables, and the t‐test was used for comparison between cases and controls; percentages were calculated for categorical variables, and the χ2 test was used for comparison between the case and control group participants (version 19.0; SPSS Inc., Chicago, IL). A Hardy–Weinberg equilibrium (HWE) was performed using SNPStats (available online at http://bioinfo.iconcologia.net/SNPstats). A logistic regression model was used to examine the association between A118G and ESCC and the interaction between A118G and smoking or alcohol consumption. The odds ratio (OR) and 95% confident interval (95%CI) were calculated. Odds were adjusted for gender, age, high‐fat diet, and low‐fibre diet.
Results
A total of 960 subjects (545 males and 415 females) with a mean age of 58.1 ± 13.4 years were selected, including 490 ESCC patients and 470 normal control subjects. Participant characteristics stratified by cases and controls are shown in Table 1. The distribution of current smokers, alcohol consumption, both smoking and drinking, and high‐fat diet significantly differed between the cases and controls. The mean WC was higher in the ESCC cases than the controls.
Table 1.
General Characteristic of Study Participants in Cases and Controls
| Variables | ESCC Cases (n = 490) | Controls (n = 470) | P‐values |
|---|---|---|---|
| Age (year) | 58.70 ± 12.3 | 57.43 ± 14.1 | 0.138 |
| Males N (%) | 256(52.2) | 269(57.2) | 0.136 |
| Alcohol consumption N (%) | 213(43.4) | 166(35.3) | 0.012 |
| Current smokers N (%) | 203 (41.4) | 154 (32.8) | 0.007 |
| Both smoking and drinking N (%) | 118 (24.1) | 86 (18.3) | 0.028 |
| High‐fat diet N (%) | 159(32.4) | 124 (26.4) | 0.049 |
| Low‐fibre diet N (%) | 123 (25.1) | 109 (23.2) | 0.540 |
| BMI (kg/m2) | 23.4 ± 8.7 | 22.7 ± 8.2 | 0.200 |
| WC (cm) | 82.6 ± 15.3 | 80.4 ± 14.8 | 0.024 |
| FPG (mmol/l) | 5.02 ± 0.77 | 5.01 ± 0.74 | 0.837 |
| TG (mmol/l) | 1.27 ± 0.42 | 1.24 ± 0.46 | 0.292 |
| TC (mmol/l) | 5.00 ± 1.14 | 4.86 ± 1.10 | 0.053 |
| HDL (mmol/l) | 1.24 ± 0.58 | 1.31 ± 0.67 | 0.084 |
Means ± standard deviation for age, FPG, TC, HDL‐C, TG, WC, and BMI.
TC, total cholesterol; HDL, high density lipoprotein; FPG, fast plasma glucose; TG, triglyceride; WC, waist circumference; BMI, body mass index.
The genotypes of A118G were distributed according to Hardy–Weinberg equilibrium (P > 0.05). The frequency for the A allele of A118G was significantly higher in the ESCC cases, OR (95%CI) = 1.22 (1.08–1.59). Logistic regression analysis showed a significant association between genotypes of the A allele in A118G and increased ESCC risk after adjusting for gender, age, high‐fat diet, and low‐fibre diet. ESCC risk was significantly higher in carriers of the A allele of the A118G polymorphism than those with GG (AG + AA vs. GG, adjusted OR (95%CI) = 1.20 (1.05–1.53); Table 2). We also conducted an association analysis among smoking, drinking, and ESCC using logistic regression. We found that the OR (95%CI) was 1.48 (1.08–2.27) for always smokers compared with never smokers and 1.69 (1.10–2.18) for always drinkers compared with not current drinkers (Table 3).
Table 2.
Genotype and Allele Frequencies for A118G in Cases and Controls
| Genotypes and alleles | Frequencies N (%) | OR (95%CI)a | P‐values | HWE test | |
|---|---|---|---|---|---|
| Controls (n = 470) | ESCC Cases (n = 490) | ||||
| GG | 40 (8.5) | 23 (4.7) | 1.00 | 0.014 | 0.149 |
| AG | 170 (36.2) | 163 (33.3) | 1.18 (0.98–1.57) | ||
| AA | 260 (55.3) | 304 (62.0) | 1.29 (1.12–1.66) | ||
| AG + AA | 210 (44.7) | 186 (38.0) | 1.20 (1.05–1.53) | 0.022 | |
| A | 690 (73.4) | 771 (78.7) | 1.00 | 0.007 | |
| G | 250 (26.6) | 209 (21.3) | 1.22 (1.08–1.59) | ||
Adjusted for gender, age, high‐fat diet, low‐fibre diet, and WC.
Table 3.
The Association Between Smoking and Drinking and ESCC Risk
| Variables | Frequencies N (%) | OR (95%CI)a | P‐values | |
|---|---|---|---|---|
| Controls (n = 470) | ESCC Cases (n = 490) | |||
| Smoking | ||||
| Never | 316 (67.2) | 287 (58.6) | 1.00 | 0.016a |
| Currently | 154 (32.8) | 203 (41.4) | 1.48 (1.08–2.27) | |
| Drinking | ||||
| Not currently | 304 (64.7) | 277 (56.5) | 1.00 | 0.010b |
| Currently | 166 (35.3) | 213 (43.4) | 1.69 (1.10–2.18) | |
Adjusted for gender, age, high‐fat diet, low‐fibre diet, WC, and drinking.
Adjusted for gender, age, high‐fat diet, low‐fibre diet, WC, and smoking.
To obtain the odds ratios and 95%CI for the joint effects of A118G and smoking and alcohol consumption on ESCC, we conducted an interaction analysis between A118G and current smoking and drinking using logistic regression. We found that current smokers with AG or AA of the A118G genotype have the highest ESCC risk compared with never smoking subjects with the GG genotype (OR (95%CI) of 2.57 (1.66–3.33) after covariate adjustment; Table 4). We also found that current drinkers with AG or AA of the A118G genotype have the highest ESCC risk compared with not current drinking subjects with the GG genotype (OR (95%CI) of 2.36 (1.47–3.25) after adjusting for covariates; Table 5).
Table 4.
Interaction Between A118G and Smoking on ESCC Risk
| A118G | Smoking | OR (95% CI)a | P‐values |
|---|---|---|---|
| GG | Never | 1.00 | – |
| GG | Currently | 1.36 (1.18–1.65) | 0.001 |
| AG + AA | Never | 1.15 (0.92–1.41) | 0.102 |
| AG + AA | Currently | 2.57 (1.66–3.33) | <0.001 |
Adjusted for gender, age, high‐fat diet, low‐fibre diet, and WC.
Table 5.
Interaction Between A118G and Alcohol Consumption on ESCC Risk
| rs507392 | Alcohol consumption | OR (95% CI)a | P‐values |
|---|---|---|---|
| GG | Not currently | 1.00 | – |
| GG | Currently | 1.27 (1.12–1.59) | 0.002 |
| AG + AA | Not currently | 1.18 (0.98–1.51) | 0.068 |
| AG + AA | Currently | 2.36 (1.47–3.25) | <0.001 |
Adjusted for gender, age, high‐fat diet, low‐fibre diet, and WC.
Discussion
In this study, we found that A118G polymorphism was significantly associated with ESCC risk in a Chinese population, the A allele of A118G was significantly higher in ESCC cases and ESCC risk was also higher in the A allele of A118G carriers than that in subjects with the GG allele of A118G after adjustment. Although A118G polymorphism and its relationship with cancer susceptibility have been investigated in many studies, few have focused on an association between A118G polymorphism and ESCC. To our knowledge, this is the second epidemiologic study to evaluate the association between the A118G of the μ‐opioid receptor gene and ESCC risk. Up to now, we found only one human population study 16 investigating this aspect. In that study, Wang et al. conducted a case‐controlled study in Chinese Han and TuJia populations in the Enshi region, China. They found that the A118G polymorphism in the μ‐opioid receptor gene may be associated with a risk of ESCC; compared with the GG genotype, the AA genotype exhibited a significantly elevated risk for ESCC.
Interest in the direct effect of opioids and μ‐opioid receptors on tumour progression has grown in recent years. There is accumulating experimental evidence of a direct effect of μ‐opioid receptors on tumour progression or recurrence 8, 17, 18, 19, 20, particularly for breast cancer 5, 20. Direct mechanisms 8 for a direct effect of μ‐opioids on cancer progression were demonstrated. The μ‐opioid receptor is the main target for opiates such as morphine, fentanyl, and heroin and has a binding affinity two orders of magnitude greater than the affinity of other opioid receptors; in addition, a direct effect of opioids on tumour progression was observed during the development of the peripheral opioid antagonist methylnaltrexone for opioid‐induced constipation. Because methylnaltrexone does not cross the blood–brain barrier, centrally mediated analgesia is preserved 21.
Tobacco smoking and alcohol consumption were widely reported important environmental risk factors for ESCC 22, 23, 24, 25, 26. Some studies 27, 28 suggested a significant interaction between gene polymorphism (such as P21, XRCC1, GSTT1, and ERCC2) and current smoking or alcohol consumption in determining ESCC risk. In this study, we also found a significant interaction between the A allele of A118G plus current smoking or alcohol consumption in determining ESCC risk. Current smokers or drinkers with the A allele have the highest ESCC risk. A study by Wang et al. 16 revealed that the A118G polymorphism may be an important inherited genetic variable associated with ESCC risk, and their results implied an interaction with environmental factors (such as smoking) in individuals with more G alleles. They also found that non‐smoking may be more protective against ESCC occurrence, which was consistent with the results of our study. Evidence points to the endogenous opioid system (and the μ‐opioid receptor in particular) in mediating the rewarding effects of drug use, including those associated with nicotine, and OPRM1 A118G has been shown to alter the receptor protein level in preclinical models and smoking behaviour in humans 29.
The limitations of this study should be considered. First, although the number of study participants met the requirement for analysis, the present sample size was relatively small. The smoking and drinking rates in women were very low. These limited rates led to insufficient data for a gender difference analysis. Second, the gene–gene interaction with other SNPs of OPRM1 or other genes and interactions with other environmental risk factors (such as diet) should be investigated in future studies. Thirdly, OR values were relatively low in the correlation analysis, so this relation need to be verified in others population.
In conclusion, we found that A118G polymorphism was significantly associated with ESCC risk in our study, that the rate of the A allele of A118G was significantly higher in the ESCC cases than the controls, and that the ESCC risk was also higher in the A allele of A118G carriers than in subjects with the GG genotype. We also found a significant interaction between the A allele of A118G and current smoking or alcohol consumption. Current smokers or drinkers with the A allele have the highest ESCC risk.
Acknowledgements
The writing of this study was supported by the Department of Gastroenterology, Yixing People's Hospital. We thank all the partners and staffs who helped us in the process of this study.
References
- 1. Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: Defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol 2006;24:2137–2150. [DOI] [PubMed] [Google Scholar]
- 2. Eslick G. Epidemiology of esophageal cancer. Gastroenterol Clin North Am 2009;38:17–25. [DOI] [PubMed] [Google Scholar]
- 3. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin 2009;59:225–249. [DOI] [PubMed] [Google Scholar]
- 4. Kuwano H, Kato H, Miyazaki T. Genetic alterations in esophageal cancer. Surg Today 2005;35:7–18. [DOI] [PubMed] [Google Scholar]
- 5. Sugimoto T, Seki N, Shimizu S, et al. The galanin signaling cascade is a candidate pathway regulating oncogenesis in human squamous cell carcinoma. Genes Chromosom Cancer 2009;48:132–142. [DOI] [PubMed] [Google Scholar]
- 6. Qin YR, Wang LD, Fan ZM, Kwong D, Guan XY. Comparative genomic hybridization analysis of genetic aberrations associated with development of esophageal squamous cell carcinoma in Henan, China. World J Gastroenterol 2008;14:1828–1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bovill JG. Surgery for cancer: Does anesthesia matter? Anesth Analg 2010;110:1524–1526. [DOI] [PubMed] [Google Scholar]
- 8. Lennon FE, Moss J, Singleton PA. The mu‐opioid receptor in cancer progression: Is there a direct effect? Anesthesiology 2012;116:940–945. [DOI] [PubMed] [Google Scholar]
- 9. Afsharimani B, Cabot P, Parat MO. Morphine and tumor growth and metastasis. Cancer Metastasis Rev 2011;30:225–238. [DOI] [PubMed] [Google Scholar]
- 10. Shabalina SA, Zaykin DV, Gris P, et al. Expansion of the human mu‐opioid receptor gene architecture: Novel functional variants. Hum Mol Genet 2009;18:1037–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Freiberg MS, Cabral HJ, Heeren TC, Vasan RS, Ellison RC. Alcohol consumption and the prevalence of the metabolic syndrome in the US. Diabetes Care 2004;27:2954–2959. [DOI] [PubMed] [Google Scholar]
- 12. Tomar SL, Asma S. Smoking‐attributable periodontitis in the United States: Findings from NHANES III. National Health and Nutrition Examination Survey. J Periodontol 2000;71:743–751. [DOI] [PubMed] [Google Scholar]
- 13. Iida H, Kumar JV, Kopycka‐Kedzierawski DT, Billings RJ. Effect of tobacco smoke on the oral health of U.S. women of childbearing age. J Public Health Dent 2009;69:231–241. [DOI] [PubMed] [Google Scholar]
- 14. China Nutrition Society . 2008. Chinese residents dietary guide. Beijing: Tibet people's press; pp 15–55. [Google Scholar]
- 15. Lohman TG, Roche AF, Martorell R. (Eds.). 1988. Anthropometric standardization reference manual. Champaign: Human Kinetics Books. [Google Scholar]
- 16. Wang S, Li Y, Liu XD, Zhao CX, Yang KQ. Polymorphism of A118G in μ‐opioid receptor gene is associated with risk of esophageal squamous cell carcinoma in a Chinese population. Int J Clin Oncol 2013;18:666–669. [DOI] [PubMed] [Google Scholar]
- 17. Tavare AN, Perry NJ, Benzonana LL, Takata M, Ma D. Cancer recurrence after surgery: Direct and indirect effects of anesthetic agents. Int J Cancer 2012;130:1237–1250. [DOI] [PubMed] [Google Scholar]
- 18. Gach K, Wyrębska A, Fichna J, Janecka A. The role of morphine in regulation of cancer cell growth. Naunyn Schmiedebergs Arch Pharmacol 2011;384:221–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cieślińska A, Sienkiewicz‐Szłapka E, Kostyra E, et al. μ‐Opioid receptor gene (OPRM1) polymorphism in patients with breast cancer. Tumour Biol 2015;36:4655–4660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bortsov AV, Millikan RC, Belfer I, Boortz‐Marx RL, Arora H, McLean SA. μ‐Opioid receptor gene A118G polymorphism predicts survival in patients with breast cancer. Anesthesiology 2012;116:896–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Moss J, Rosow CE. Development of peripheral opioid antagonists’ new insights into opioid effects. Mayo Clin Proc 2008;83:1116–1130. [DOI] [PubMed] [Google Scholar]
- 22. Islami F, Fedirko V, Tramacere I, et al. Alcohol drinking and esophageal squamous cell carcinoma with focus on light‐drinkers and never‐smokers: A systematic review and meta‐analysis. Int J Cancer 2011;129:2473–2484. [DOI] [PubMed] [Google Scholar]
- 23. Morita M, Kumashiro R, Kubo N, et al. Alcohol drinking, cigarette smoking, and the development of squamous cell carcinoma of the esophagus: Epidemiology, clinical findings, and prevention. Int J Clin Oncol 2010;15:126–134. [DOI] [PubMed] [Google Scholar]
- 24. Toh Y, Oki E, Ohgaki K, et al. Alcohol drinking, cigarette smoking, and the development of squamous cell carcinoma of the esophagus: Molecular mechanisms of carcinogenesis. Int J Clin Oncol 2010;15:135–144. [DOI] [PubMed] [Google Scholar]
- 25. Zhang F, Han H, Wang C, et al. A retrospective study: The prognostic value of anemia, smoking and drinking in esophageal squamous cell carcinoma with primary radiotherapy. World J Surg Oncol 2013;11:249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Talukdar FR, Ghosh SK, Laskar RS, Mondal R. Epigenetic, genetic and environmental interactions in esophageal squamous cell carcinoma from northeast India. PLoS ONE 2013;8:e60996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Taghavi N, Biramijamal F, Abbaszadegan MR, Khademi H, Sotoudeh M, Khoshbakht S. P21 (Waf1/Cip1) Gene polymorphisms and possible interaction with cigarette smoking in esophageal squamous cell carcinoma in northeastern Iran: A preliminary study. Arch Iran Med 2010;13:235–242. [PubMed] [Google Scholar]
- 28. Sobti RC, Singh J, Kaur P, Pachouri SS, Siddiqui EA, Bindra HS. XRCC1 codon 399 and ERCC2 codon 751 polymorphism, smoking, and drinking and risk of esophageal squamous cell carcinoma in a North Indian population. Cancer Genet Cytogenet 2007;175:91–97. [DOI] [PubMed] [Google Scholar]
- 29. Ray R, Ruparel K, Newberg A, et al. Human Mu Opioid Receptor (OPRM1 A118G) polymorphism is associated with brain mu‐opioid receptor binding potential in smokers. Proc Natl Acad Sci USA 2011;108:9268–9273. [DOI] [PMC free article] [PubMed] [Google Scholar]


