Short abstract
See Article Schmucker et al
Keywords: Editorials, antiplatelet agent, antiplatelet therapy, antithrombotic
Not everything that can be counted counts, and not everything that counts can be counted.—Albert Einstein
In patients with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI), the more potent P2Y12 inhibitors ticagrelor and prasugrel are recommended over clopidogrel, in combination with aspirin, for the prevention of recurrent atherothrombotic events.1 However, compared with clopidogrel, the use of prasugrel and ticagrelor comes at the expense of increased bleeding, which may offset their ischemic benefit in more vulnerable patient cohorts. Among the latter, elderly subjects represent a challenging population because of their higher risk of both ischemic and bleeding complications after an ACS.2 In the TRITON TIMI‐38 trial (Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition With Prasugrel–Thrombolysis in Myocardial Infarction 38), there was no net clinical benefit of prasugrel over clopidogrel among elderly patients with ACS undergoing PCI.3 Consequently, in patients aged ≥75 years, the standard prasugrel maintenance dose of 10 mg is generally not recommended, and a reduced dose of 5 mg should be considered.1, 4 On the contrary, in the PLATO (Platelet Inhibition and Patient Outcomes) trial, despite increased rates of bleeding among elderly patients, the net clinical benefit still favored the use of ticagrelor over clopidogrel, regardless of bleeding definitions.5 Indeed, on the basis of these results, ticagrelor is recommended after ACS regardless of all age categories.1 However, it should be highlighted that in the PLATO trial, elderly patients, defined as those aged ≥75 years, were underrepresented (15% of overall ACS trial population). It also cannot be excluded that patients with a lower risk for bleeding might have been included, as typically occurs in clinical trials. Therefore, the net clinical benefit of ticagrelor compared with clopidogrel in a real‐world elderly population is not fully defined.
In this issue of the Journal of the American Heart Association (JAHA), Schmucker et al report 1‐year clinical outcomes of ticagrelor versus clopidogrel in elderly patients (aged ≥75 years) with ST‐segment–elevation myocardial infarction (STEMI) undergoing primary PCI with stent implantation included in the Bremen STEMI‐Registry.6 In particular, this registry includes 7466 patients with STEMI treated with primary PCI, of whom 1087 (15%) were elderly, who were overall equally treated with either ticagrelor (n=535, 49%) or clopidogrel (n=552, 51%) and were assessed in the present study. In an unadjusted analysis, the primary composite efficacy end point of all‐cause death, myocardial infarction, or stroke at 1 year was significantly lower with ticagrelor compared with clopidogrel (25.2% versus 32.4%; P=0.015). This difference was driven by lower rates of all‐cause mortality with ticagrelor (21.1% versus 26.8%; P=0.035; absolute difference, −5.7%, comprising −3.3% and −2.4% of in‐hospital and after discharge mortality, respectively). In a propensity score matched cohort including 238 pairs, the composite efficacy end point remained significantly reduced with ticagrelor compared with clopidogrel (hazard ratio, 0.69; 95% CI, 0.49–0.97; P=0.03), although there was no significant difference in all‐cause mortality (hazard ratio, 0.89; 95% CI, 0.67–1.28; P=0.52). In the unadjusted analysis, rates of bleeding after discharge, defined as a serious event requiring medical attention, were significantly higher among ticagrelor‐treated patients (1.8% versus 0.4%; P=0.03), whereas no significant difference between ticagrelor and clopidogrel was observed in overall bleeding, including events occurring in hospital plus those observed after discharge. However, the 1‐year net clinical benefit still significantly favored ticagrelor over clopidogrel (30.6% versus 37.3%; P=0.028). On the contrary, in the propensity‐matched population, the risk of bleeding after discharge was not statistically different between groups (hazard ratio, 0.67; 95% CI, 0.11–3.99; P=0.67), probably because of the small sample size of the matched cohorts, as also suggested by the wide 95% CI. The authors should be commended for reporting this study, which is the first to investigate the efficacy and safety of ticagrelor compared with clopidogrel in elderly patients with STEMI undergoing primary PCI from a large all‐comers real‐world registry. Of note, the study population was at high risk, as reflected by the patients’ mean age (81±5 years), with more than half of them being >80 years, and 1‐year mortality rate, which was ≈2‐fold higher than that observed in the elderly cohort of the PLATO trial.5 In light of the favorable net clinical benefit of ticagrelor over clopidogrel, the authors conclude that ticagrelor should be the P2Y12 inhibitor of choice in elderly patients with STEMI undergoing primary PCI. However, several considerations need to be made when interpreting study findings and ensuing practical implications.
The superior ischemic benefit of ticagrelor, including the reduced all‐cause mortality, in the setting of a registry can be affected by a possible unbalance between the compared cohorts. Indeed, it is reasonable to speculate that with the commercial availability of different P2Y12 inhibitors characterized by diverse pharmacologic properties, particularly with regard to their platelet inhibiting potency, clinicians would opt for an agent that they feel most appropriate for the individual patient on the basis of both the ischemic and the bleeding risk profiles. The latter is determined by several characteristics, which are known to impact outcomes, including mortality. These variables include the numerous comorbidities that frequently affect elderly patients as well as other factors, including social, functional, and cognitive (Figure). It is possible that an elderly patient judged to be at increased risk for bleeding with a potent antiplatelet agent (ie, ticagrelor) because of the presence of ≥1 of these conditions was prescribed with a less potent antiplatelet drug (ie, clopidogrel). However, these variables, which frequently affect elderly patients, were not reported and adjusted for in this Bremen STEMI‐Registry analysis (Figure). Therefore, it cannot be excluded that this could have contributed to the higher risk of events among clopidogrel‐treated patients. Therefore, rather than being “the P2Y12 inhibitor of choice,” a more attentive conclusion of the study from Schmucker et al6 should be that ticagrelor represents a “reasonable treatment option” even in a more vulnerable population, such as elderly patients, when wisely chosen on the basis of overall clinical judgment of potential risks and benefits.
Figure 1.
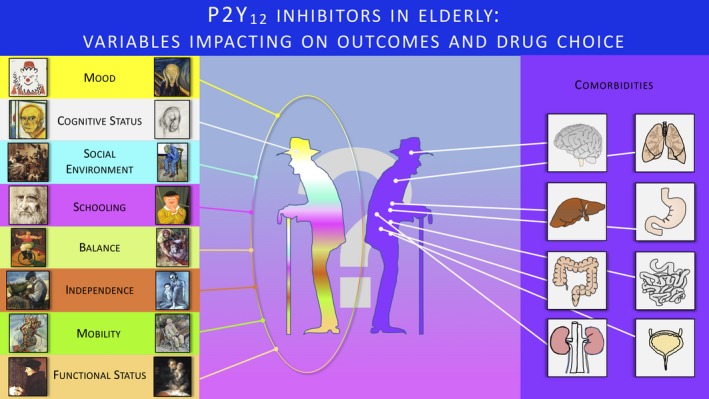
Variables affecting outcome and, thus, the selection of antiplatelet therapy in elderly patients. Paintings next to the variable name represent the “good and bad” of the specific variable. In the left column from top to the bottom, the paintings include the following: Pablo Picasso: Le Clown, 1961; William Utermohlen: Self‐Portrait, 1996; Jan Steen: The Artists Family, 1663; Leonardo Da Vinci: Self‐Portrait in Red Chalk, 1512; Fernando Botero: Circus Performer, 2007; Mino Lo Savio: Old Fisherman, 1982; Vittorio Corona: The Runner, 1923; Hans Holbein the Younger: Erasmus, 1523. In right column from top to the bottom, the paintings include the following: Edvard Munch: The Scream, 1893; William Utermohlen: Self‐Portrait, 2000; Vincent Van Gogh: At Eternity's Gate, 1890; Fernando Botero: Clown Smoking, 2008; Michelangelo Buonarroti: The Conversion of St. Paul, 1545; Pablo Picasso: Old Blind and Boy, 1903; Peter Gallen: Old Man Sitting on the Bench in Front of My Window, undated; Francisco Goya: Self‐Portrait With Dr Arrieta, 1820.
The above‐mentioned considerations are underscored by the fact that in the present Bremen STEMI‐Registry analysis focusing on elderly patients, ticagrelor compared with clopidogrel was associated with an ≈4‐fold increase in the rate of serious bleeding events after hospital discharge.6 If this increase in bleeding would have offset the ischemic benefits in a more risk‐balanced population remains unknown. More insights on the relative impact on bleeding and net clinical benefit of more potent P2Y12 inhibition among elderly patients will be provided by the POPular AGE study (NCT02317198) comparing ticagrelor or prasugrel with clopidogrel in patients (n=1000) aged >70 years with ACS.7 However, while waiting for further powered randomized evidence, the wide spectrum of possible risk profiles encountered in clinical practice prompts the need for accurate risk stratification among elderly patients. Indeed, although age is included as an independent factor in several scoring systems for bleeding, age by itself without other coexisting conditions has not been considered as a major bleeding risk factor in the recent Academic Research Consortium for High Bleeding Risk.8, 9 However, in both the Academic Research Consortium for High Bleeding Risk definitions and in available scores, age is considered as a binary variable, even though the relationship between age and bleeding appears to be continuous. Thus, it remains unknown if a certain chronological age threshold should be considered as a major bleeding risk by itself, warranting for studies focusing on patients at late stages of age. Moreover, it should be highlighted that risk stratification in elderly patients has to account for variables (Figure) that are not included in HBR definitions or scores, underscoring the need for further refinements of predictive tools that can assist therapeutic choices.
Beyond the selection of a P2Y12 inhibitor type, a strategy of switching the intensity of P2Y12 inhibition (ie, de‐escalation) may be considered in elderly patients to tackle the early high ischemic risk phase and minimize the risk of bleeding that prevails during the long‐term treatment.10, 11 In the Bremen STEMI‐Registry, the temporal trend of the comparative efficacy and safety of ticagrelor versus clopidogrel was not reported, thus not allowing speculation on the potential role of P2Y12 inhibitor de‐escalation.6 The time course of ischemic and bleeding events has been specifically assessed among elderly patients (aged ≥75 years) with ACS (n=1443) in a study comparing the reduced prasugrel dose with clopidogrel.12 The number of ischemic events was lower with prasugrel, 5 mg, within the first month after an ACS, whereas it was similar between the drug groups thereafter. On the contrary, bleeding events were similar between drugs within the first month, whereas they were halved in the clopidogrel group thereafter.12 These data would support a P2Y12 inhibitor de‐escalation strategy that should be preferably guided by platelet function testing or possibly genetic testing. Indeed, it should be emphasized that elderly patients have increased rates of clopidogrel resistance, which may contribute to their increased risk of thrombotic complications.13 However, the efficacy and safety of a guided P2Y12‐de‐escalation strategy has not been established among elderly patients. Indeed, elderly patients were poorly represented in the 2 available studies assessing the net clinical impact of P2Y12 inhibitor de‐escalation versus standard treatment, not allowing for definitive conclusions.14, 15 Moreover, in the ANTARCTIC (Assessment of a Normal Versus Tailored Dose of Prasugrel After Stenting in Patients Aged > 75 Years to Reduce the Composite of Bleeding, Stent Thrombosis and Ischemic Complications) trial focusing on elderly patients with ACS undergoing PCI, a strategy of platelet function testing–guided dose or drug adjustment of prasugrel, 5 mg, versus treatment with prasugrel, 5 mg, with no monitoring was not associated with improved net clinical outcomes.16 However, this lack of benefit should be interpreted in light of the fact that platelet function testing–guided adjustment led to de‐escalation from prasugrel, 5 mg, to clopidogrel in 39% of patients and to escalation to prasugrel, 10 mg, only in 4%.17 This resulted in a comparison between clopidogrel and prasugrel, 5 mg, that has never shown differences in clinical outcomes, probably because of the small difference in the level of platelet inhibition achieved with these 2 drug regimens.13, 17 Therefore, the ANTARCTIC trial does not allow us to refute the potential benefit of platelet function testing–guided P2Y12 inhibitor de‐escalation from standard doses of prasugrel or ticagrelor to clopidogrel.17 However, although elderly patients could be ideal candidates for tailored antiplatelet treatment regimens, currently the general recommendation is that a guided de‐escalation strategy of P2Y12 inhibition may be considered as an alternative to standard dual‐antiplatelet therapy (DAPT) only for patients with ACS who were deemed unsuitable for 12 months of potent platelet inhibition.11, 18
In conclusion, while waiting for future evidence on optimal antiplatelet treatment management of elderly patients with ACS undergoing PCI, tailoring P2Y12 inhibition on the basis of a multiparameter clinical assessment should be considered the strategy of choice in clinical practice. Indeed, a DAPT strategy using aspirin and ticagrelor for 12 months in this setting represents a reasonable treatment option, even in elderly patients. However, in elderly patients at high bleeding risk on the basis of Academic Research Consortium for High Bleeding Risk criteria or with coexisting comorbidities/general health status conditions (ie, factors associated with risk of fall, frail conditions, and cognitive disorders), it is also reasonable to consider bleeding reduction antiplatelet strategies. These may include a DAPT regimen with aspirin and clopidogrel, a DAPT strategy of P2Y12 inhibitor de‐escalation (ticagrelor to clopidogrel) at 1 to 3 months, a P2Y12 inhibitor monotherapy after dropping aspirin at 1 to 3 months, or shortening DAPT duration (eg, 3–6 months) overall. The use of less aggressive antithrombotic regimens should be coupled with other bleeding reduction approaches, such as the use of proton pump inhibitors, avoidance of nonsteroidal anti‐inflammatory drugs, and stricter follow‐up monitoring.
Disclosures
Dr Angiolillo declares that he has received consulting fees or honoraria from Amgen, Aralez, AstraZeneca, Bayer, Biosensors, Boehringer Ingelheim, Bristol‐Myers Squibb, Chiesi, Daiichi‐Sankyo, Eli Lilly, Haemonetics, Janssen, Merck, PLx Pharma, Pfizer, Sanofi, and The Medicines Company and has received payments for participation in review activities from CeloNova and St Jude Medical. Dr Angiolillo also declares that his institution has received research grants from Amgen, AstraZeneca, Bayer, Biosensors, CeloNova, CSL Behring, Daiichi‐Sankyo, Eisai, Eli Lilly, Gilead, Idorsia, Janssen, Matsutani Chemical Industry Co, Merck, Novartis, Osprey Medical, and Renal Guard Solutions. Dr Capranzano has no disclosures to report.
J Am Heart Assoc. 2019;8:e014000 DOI: 10.1161/JAHA.119.014000.
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
References
- 1. Capodanno D, Alfonso F, Levine GN, Valgimigli M, Angiolillo DJ. ACC/AHA versus ESC guidelines on dual antiplatelet therapy: JACC guideline comparison. J Am Coll Cardiol. 2018;72:2915–2931. [DOI] [PubMed] [Google Scholar]
- 2. Capodanno D, Angiolillo DJ. Antithrombotic therapy in the elderly. J Am Coll Cardiol. 2010;56:1683–1692. [DOI] [PubMed] [Google Scholar]
- 3. Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, Neumann FJ, Ardissino D, De Servi S, Murphy SA, Riesmeyer J, Weerakkody G, Gibson CM, Antman EM; TRITON‐TIMI 38 Investigators . Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357:2001–2015. [DOI] [PubMed] [Google Scholar]
- 4. Erlinge D, Gurbel PA, James S, Lindahl TL, Svensson P, Ten Berg JM, Foley DP, Wagner H, Brown PB, Luo J, Zhou C, Moser BA, Jakubowski JA, Small DS, Winters KJ, Angiolillo DJ. Prasugrel 5 mg in the very elderly attenuates platelet inhibition but maintains noninferiority to prasugrel 10 mg in nonelderly patients: the GENERATIONS trial, a pharmacodynamic and pharmacokinetic study in stable coronary artery disease patients. J Am Coll Cardiol. 2013;62:577–583. [DOI] [PubMed] [Google Scholar]
- 5. Husted S, James S, Becker RC, Horrow J, Katus H, Storey RF, Cannon CP, Heras M, Lopes RD, Morais J, Mahaffey KW, Bach RG, Wojdyla D, Wallentin L; PLATO study group. Ticagrelor versus clopidogrel in elderly patients with acute coronary syndromes: a substudy from the prospective randomized PLATelet inhibition and patient Outcomes: (PLATO) trial. Circ Cardiovasc Qual Outcomes. 2012;5:680–688. [DOI] [PubMed] [Google Scholar]
- 6. Schmucker J, Fach A, Mata Marin LA, Retzlaff T, Osteresch R, Kollhorst B, Hambrecht R, Pohlabeln H, Wienbergen H. Efficacy and safety of ticagrelor in comparison to clopidogrel in elderly patients with ST–segment elevation myocardial infarctions. J Am Heart Assoc. 2019. DOI: 10.1161/JAHA.119.012530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Qaderdan K, Ishak M, Heestermans AA, de Vrey E, Jukema JW, Voskuil M, de Boer MJ, van't Hof AW, Groenemeijer BE, Vos GJ, Janssen PW, Bergmeijer TO, Kelder JC, Deneer VH, ten Berg JM. Ticagrelor or prasugrel versus clopidogrel in elderly patients with an acute coronary syndrome: optimization of antiplatelet treatment in patients 70 years and older–rationale and design of the POPular AGE study. Am Heart J. 2015;170:981–985. [DOI] [PubMed] [Google Scholar]
- 8. Urban P, Mehran R, Colleran R, Angiolillo DJ, Byrne RA, Capodanno D, Cuisset T, Cutlip D, Eerdmans P, Eikelboom J, Farb A, Gibson CM, Gregson J1, Haude M, James SK, Kim HS, Kimura T, Konishi A, Laschinger J, Leon MB, Magee PFA, Mitsutake Y, Mylotte D, Pocock S, Price MJ, Rao SV, Spitzer E, Stockbridge N, Valgimigli M, Varenne O, Windhoevel U, Yeh RW, Krucoff MW, Morice MC. Defining high bleeding risk in patients undergoing percutaneous coronary intervention. Circulation. 2019;140:240–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Alatri A, Mazzolai L. The bleeding risk in antithrombotic therapies: a narrative review. Curr Vasc Pharmacol. 2019. Available at: 10.2174/1570161117666190212112743. Accessed August 30, 2019. [DOI] [PubMed] [Google Scholar]
- 10. Angiolillo DJ, Rollini F, Storey RF, Bhatt DL, James S, Schneider DJ, Sibbing D, So DYF, Trenk D, Alexopoulos D, Gurbel PA, Hochholzer W, De Luca L, Bonello L, Aradi D, Cuisset T, Tantry US, Wang TY, Valgimigli M, Waksman R, Mehran R, Montalescot G, Franchi F, Price MJ. International expert consensus on switching platelet P2Y12 receptor‐inhibiting therapies. Circulation. 2017;136:1955–1975. [DOI] [PubMed] [Google Scholar]
- 11. Sibbing D, Aradi D, Alexopoulos D, Ten Berg J, Bhatt DL, Bonello L, Collet JP, Cuisset T, Franchi F, Gross L, Gurbel P, Jeong YH, Mehran R, Moliterno DJ, Neumann FJ, Pereira NL, Price MJ, Sabatine MS, So DYF, Stone GW, Storey RF, Tantry U, Trenk D, Valgimigli M, Waksman R, Angiolillo DJ. Updated expert consensus statement on platelet function and genetic testing for guiding P2Y12 receptor inhibitor treatment in percutaneous coronary intervention. JACC Cardiovasc Interv. 2019;12:1521–1537. [DOI] [PubMed] [Google Scholar]
- 12. Crimi G, Morici N, Ferrario M, Ferri LA, Piatti L, Grosseto D, Cacucci M, Mandurino Mirizzi A, Toso A, Piscione F, De Carlo M, Elia LR, Trimarco B, Bolognese L, Bovenzi FM, De Luca G, Savonitto S, De Servi S. Time course of ischemic and bleeding burden in elderly patients with acute coronary syndromes randomized to low‐dose prasugrel or clopidogrel. J Am Heart Assoc. 2019;8:e010956 DOI: 10.1161/JAHA.118.010956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Capranzano P, Tamburino C, Capodanno D, Miccichè E, D'Urso L, Calvi V, Angiolillo DJ, Tamburino C. Platelet function profiles in the elderly: results of a pharmacodynamic study in patients on clopidogrel therapy and effects of switching to prasugrel 5 mg in patients with high platelet reactivity. Thromb Haemost. 2011;106:1149–1157. [DOI] [PubMed] [Google Scholar]
- 14. Sibbing D, Aradi D, Jacobshagen C, Gross L, Trenk D, Geisler T, Orban M, Hadamitzky M, Merkely B, Kiss RG, Komócsi A, Dézsi CA, Holdt L, Felix SB, Parma R, Klopotowski M, Schwinger RHG, Rieber J, Huber K, Neumann FJ, Koltowski L, Mehilli J, Huczek Z, Massberg S; TROPICAL‐ACS Investigators . Guided de‐escalation of antiplatelet treatment in patients with acute coronary syndrome undergoing percutaneous coronary intervention (TROPICAL‐ACS): a randomized, open‐label, multicenter trial. Lancet. 2017;390:1747–1757. [DOI] [PubMed] [Google Scholar]
- 15. Cuisset T, Deharo P, Quillici J, Johnson TW, Deffarges S, Bassez C, Bonnet G, Fourcade L, Mouret JP, Lambert M, Verdier V, Morange PE, Alessi MC, Bonnet JL. Benefit of switching dual antiplatelet therapy after acute coronary syndrome: the TOPIC (timing of platelet inhibition after acute coronary syndrome) randomized study. Eur Heart J. 2017;38:3070–3078. [DOI] [PubMed] [Google Scholar]
- 16. Cayla G, Cuisset T, Silvain J, Leclercq F, Manzo‐Silberman S, Saint‐Etienne C, Delarche N, Bellemain‐Appaix A, Range G, El Mahmoud R, Carrié D, Belle L, Souteyrand G, Aubry P, Sabouret P, du Fretay XH, Beygui F, Bonnet JL, Lattuca B, Pouillot C, Varenne O, Boueri Z, Van Belle E, Henry P, Motreff P, Elhadad S, Salem JE, Abtan J, Rousseau H, Collet JP, Vicaut E, Montalescot G; ANTARCTIC investigators . Platelet function monitoring to adjust antiplatelet therapy in elderly patients stented for an acute coronary syndrome (ANTARCTIC): an open‐label, blinded‐endpoint, randomised controlled superiority trial. Lancet. 2016;388:2015–2022. [DOI] [PubMed] [Google Scholar]
- 17. Sibbing D, Massberg S. Antiplatelet strategies in elderly people: still a long way to go. Lancet. 2016;388:1962–1964. [DOI] [PubMed] [Google Scholar]
- 18. Neumann FJ, Sousa‐Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferović PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO. ESC/EACTS Guidelines on myocardial revascularization. EuroIntervention. 2018;2019(14):1435–1534. [DOI] [PubMed] [Google Scholar]


