Abstract
Background
There is a scarcity of knowledge as to whether rates of myocardial reperfusion use and 30‐day mortality for patients with ST‐segment–elevation myocardial infarction are similar among patients using the Brazilian Public Health System (SUS) and those using the private healthcare system.
Methods and Results
A total of 707 patients were analyzed using the VICTIM (Via Crucis for the Treatment of Myocardial Infarction) register database; 589 patients from the SUS and 118 from the private network with ST‐segment–elevation myocardial infarction, who attended hospitals with the capacity to perform primary percutaneous coronary intervention (PCI) were investigated. The timeline, rates of use of PCI, and the 30‐day probability of death were investigated, comparing the SUS patients to those in the private system. The mean time between symptom onset and arrival at the PCI hospital was higher for SUS patients compared with users of the private system (25.4±36.5 versus 9.0±21 hours; P<0.001, respectively). Rates of primary PCI were low in both groups, but significantly lower for the SUS patients (45% versus 78%; P<0.001). The 30‐day mortality rate of SUS patients was 11.9% and of private patients was 5.9% (P=0.04). In the fully adjusted model, the odds ratio for 30‐day mortality for the SUS patients was higher (odds ratio, 2.96; 95% CI, 1.15–7.61; P=0.02).
Conclusions
The delay in reaching a PCI hospital was almost 3 times higher for the SUS patients. Primary PCI was underused in both groups, especially in the SUS patients. The SUS patients were more likely to die during the 30‐day follow‐up.
Keywords: acute myocardial infarction, health disparities, health policy and outcomes research, health services coverage
Subject Categories: Health Services, Quality and Outcomes, Myocardial Infarction, Cardiovascular Disease
Clinical Perspective
What Is New?
In Brazil, the VICTIM (Via Crucis for the Treatment of Myocardial Infarction) register discloses that the delay from symptoms to arrival at a percutaneous coronary intervention hospital is much higher for patients using the Brazilian Public Health System when compared with those using the private healthcare system.
Fibrinolytics were impressively underused equally for public and private patients, and any reperfusion for ST‐segment–elevation myocardial infarction is especially underused for patients using the Brazilian Public Health System.
Patients using the Brazilian Public Health System were significantly more likely to die during the 30‐day follow‐up.
What Are the Clinical Implications?
The VICTIM register underscores large room for improvement of quality of care for patients with ST‐segment–elevation myocardial infarction in Brazil.
Future studies should evaluate these findings at a national scale.
Urgent federal and regional public policies must be implemented to decrease the large disparities for patients with ST‐segment–elevation myocardial infarction in Brazil using the Brazilian Public Health System.
Introduction
Brazil ranks among the top 10 richest countries of the world, on the basis of gross domestic product, but is falling short, as it ranks in the 17th position in the degree of economic inequality.1, 2 In 1988, the new Brazilian Constitution established health as a universal right to be provided by the State and, in 1990, the Unified Health System (SUS) was created with the promise of improving the public healthcare system.3 The SUS was founded on the values of universality (for all), integrality (all levels of care), and equity (treatment as needed equally).4 Nevertheless, the Brazilian healthcare system design needs to be rethought, as Brazil occupies the 79th position in the human development index ranking, a measurement that uses health as one major dimension.2
Categorized as a middle‐income country, Brazil has entered the epidemiological transition era.5, 6 Cardiovascular disease is the leading cause of death, and it is a growing epidemic in all regions of the country. With more than 200 million inhabitants, one third of the deaths in Brazil are attributable to cardiovascular disease.7 In ST‐segment–elevation myocardial infarction (STEMI), responsiveness and access to an effective healthcare system is key to the implementation of timely reperfusion and to achieve better outcomes.8 Notwithstanding, very little is known regarding health insurance–related disparities in reperfusion and mortality for patients with STEMI in Brazil.7, 8
Advocating for public policies based on scientific evidence, the scarcity of data scrutinizing the effectiveness of the health care delivered by the SUS is notorious. Therefore, it is imperative to generate knowledge as to whether the SUS is fulfilling the constitutional guarantee of delivering high‐level quality of health care and promoting equity.9, 10 Small and nonrepresentative studies have pointed to the existence of huge disparities occurring between public and private healthcare system users.11 This is especially critical because ≈72.1% of the Brazilians are totally dependent on the SUS to receive health care, and only 27.9% of Brazilians also have private healthcare coverage.12
In the VICTIM (Via Crucis for the Treatment of Myocardial Infarction) register, we aimed to investigate disparities related to the time to access a primary percutaneous coronary intervention (PCI)‐capable hospital, use of reperfusion (fibrinolytics or primary PCI), use of any method of revascularization (nonprimary PCI and/or coronary artery bypass graft) during hospitalization, and 30‐day mortality for patients with STEMI using SUS, in comparison with those using private healthcare coverage. For the sample to be representative, the capital of the state of Sergipe was chosen, in which all the diagnosed cases of STEMI should be directed to 1 of the only 4 hospitals (3 private and 1 public) with the capacity for primary PCI care.
Methods
Study Population
Sergipe state, Brazil, has only 4 hospitals with PCI capabilities, for an estimated population of 2 million people. According to the Brazilian Institute of Geography and Statistics, 80.7% of the Sergipe population exclusively uses the SUS. The rest of the population (19.3%) also has access to a form of private health care.13 For the SUS users, there is only 1 hospital with a PCI facility, which receives only patients transferred with previous diagnosis of STEMI. On the other hand, those who use 1 of the 3 private hospitals in the state that has a PCI facility have private health care, or pay from their own pocket to receive care.
We used data from the VICTIM register, which is a prospective, observational, uniquely representative statewide registry in Brazil, involving all PCI hospitals of Sergipe, to investigate disparities in health insurance related to patients with STEMI. All consecutive patients with STEMI presenting to 1 of the 4 hospitals with PCI capatibilities were evaluated for inclusion in the VICTIM register. For purposes of comparison, the population was divided into public hospital patients (those covered by the SUS and admitted to the nonprofit hospital) and private hospital patients (those using private health insurance or having out‐of‐pocket expense and admitted to 1 of the 3 for‐profit hospitals). The data bank may be available from the corresponding author upon reasonable request.
The data were collected during the period from December 2014 to April 2017.Patients included in this study were those who came to 1 of the 4 PCI hospitals of Sergipe, in whom the diagnosis of acute STEMI was confirmed according to clinical presentation: pathological ST elevation in at least 2 contiguous leads, and after adjudication before hospital discharge by the VICTIM team. At the nonprofit hospital, which assists SUS patients, when troponin was used, it was used as a qualitative assay.
Patients excluded from the study were those who were admitted to the nonprofit hospital but used state healthcare insurance (n=38); died before signing the informed consent (n=36); had their initial diagnosis of STEMI changed after adjudication (n=25); had STEMI after their hospital admission (n=7); refused to participate in the study (n=7), or had the STEMI event characterized as reinfarction (new acute myocardial infarction occurring within 30 days of the incident infarction) (n=7) (Figure). The Federal University of Sergipe Ethics Committee and the review board at each hospital approved the study; all patients provided written informed consent as evidence of their agreement to participate in the survey.
Figure 1.
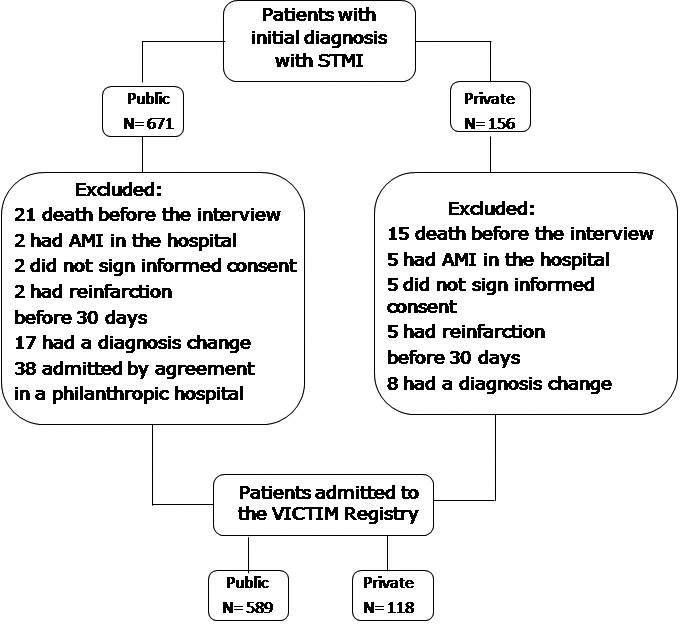
Study cohort. AMI indicates acute myocardial infarction; STEMI, ST‐segment elevation myocardial infarction.
Data Collection and Variables
Trained graduate students collected data related to this investigation. We performed abstraction from medical records and used a structured case report file developed for the VICTIM register.
We collected data regarding sociodemographic factors, previous cardiovascular risk factors, medical history, and symptoms at presentation to the PCI hospital. We estimated rates of utilization of cardiovascular‐related drugs within the first 24 hours of hospital admission at the PCI hospital, rates of reperfusion (total, fibrinolysis, and primary PCI), rates of nonprimary PCI, and rates of coronary artery bypass graft during the hospitalization.
We also collected data regarding the time from symptom onset to hospital discharge, including time from symptom onset to arrival at the PCI hospital, door‐to‐balloon time, and length of stay. We also investigated the distance from the scene of the chest pain to the PCI hospital and the number of hospitals visited before arriving at the PCI hospital.
Mortality rates were collected during hospitalization and up to 30 days after the index event by a structured telephone interview. To minimize missing data, when telephone contact was not possible, it was done through letters or e‐mails. Data to estimate in‐hospital mortality rates were available for 100% of the cohort population (N=707), and data to estimate 30‐day mortality were available for 97.6% of the cohort population (N=690).
Statistical Analysis
Data were analyzed using Stata software, version 14.2 (StataCorp, College Station, TX). Categorical variables were presented using counts and percentages, and the between‐group differences were tested using the chi‐square test or Fisher's exact test. Continuous variables were presented as means and standard deviations. The robust Levene test was used to evaluate the hypothesis of equality of variance between groups. Comparisons between continuous variables were tested using the unpaired Student t‐test, adjusted for heterogeneity of variance according to the Satterthwaite method. To check the assumption of normality of distribution, we applied the Shapiro‐Francia test. Continuous variables were summarized as means and SDs when the pattern of distribution was symmetric. Variables with skewed distribution were summarized as medians and interquartile range. For comparisons between ordinal or asymmetric variables, the Mann‐Whitney test was used.
Logistic regression models were used to predict mortality during the 30‐day period after hospital admission, starting from the unadjusted model, that is, having as a predictor only the type of hospital unit and then performing progressive adjustments in stages, using the variables age, sex, cardiovascular risk factors (hypertension, diabetes mellitus, dyslipidemia, and previous clinical history), and use of thrombolytic treatment or PCI. The effect size estimate was presented using an odds ratio, with 95% CIs. The Hosmer‐Lemeshow test was used to estimate goodness of fit. In all the estimates, the criterion of statistical significance was a 2‐tailed P<0.05.
Results
Patients Characteristics
From December 2014 to April 2017, we enrolled 707 patients admitted to 1 of the 4 hospitals of Sergipe state, Brazil, with primary PCI capabilities. Of the total, 589 (83.3%) STEMI patients were public patients and 118 (16.7%) were private patients. Baseline characteristics were similar regarding age, sex, Global Registry of Acute Coronary Events (GRACE) risk score, and electrocardiographic location of the acute myocardial infarction. Public hospital patients had less formal education (84.2% versus 29.6%; P<0.001) and were more likely to be current smokers (34% versus 9.3%; P<0.001). Patients in the private hospital had more dyslipidemia (36.3% versus 55.9%; P<0.001), family history of coronary artery disease (29.4% versus 9.3%; P<0.001), previous myocardial infarction events (7.1% versus 16.1%; P<0.001), and previous coronary artery bypass grafting (0.8% versus 5.1%; P<0.001) (Table 1).
Table 1.
Patient Characteristics at Baselinea
| Variable | Public (N=589) | Private (N=118) | P Value |
|---|---|---|---|
| Age, y | 61.2±12.2 | 62.3±12.2 | 0.35 |
| Male sex, n (%) | 395 (67.1) | 84 (71.2) | 0.38 |
| Education, n (%) | |||
| Less than high school | 496 (84.2) | 35 (29.6) | <0.001 |
| High school | 78 (13.2) | 31 (26.3) | |
| More than high school | 15 (2.6) | 52 (44.1) | |
| Cardiovascular risk factors, n (%) | |||
| Dyslipidemia | 214 (36.3) | 66 (55.9) | <0.001 |
| Systemic arterial hypertension | 358 (60.8) | 84 (71.2) | 0.03 |
| Diabetes mellitus | 199 (33.8) | 42 (35.6) | 0.70 |
| Current smoker | 200 (34.0) | 11 (9.3) | <0.001 |
| Family history of coronary artery disease | 173 (29.4) | 52 (44.1) | <0.001 |
| Medical history, n (%) | |||
| Previous congestive heart failure | 22 (3.7) | 5 (4.2) | 0.79 |
| Previous myocardial infarction | 42 (7.1) | 19 (16.1) | <0.001 |
| Previous percutaneous coronary intervention | 29 (4.9) | 12 (10.2) | 0.03 |
| Previous coronary artery bypass grafting | 5 (0.8) | 6 (5.1) | <0.001 |
| Previous stroke | 41 (7.0) | 7 (5.9) | 0.68 |
| Presenting features | |||
| Systolic blood pressure, mm Hg | 142.3±28.8 | 141.7±30.3 | 0.85 |
| Diastolic blood pressure, mm Hg | 85.4±17.5 | 83.9±15.2 | 0.33 |
| Heart rate, bpm | 82.7±18.7 | 82.8±17.5 | 0.95 |
| Location of myocardial infarction—n/N (%)b | |||
| Anterior | 383/589 (65.0) | 71/117 (60.2) | 0.37 |
| Killip—n/N (%) | |||
| I | 493/586 (84.1) | 101/114 (88.6) | 0.19 |
| II | 74/586 (12.6) | 8/114 (7.0) | |
| III | 13/586 (2.2) | 2/114 (1.8) | |
| IV | 6/586 (1.1) | 3/114 (2.6) | |
| Creatinine, IU/L | 1.0±0.8 | 1.0±0.4 | 0.42 |
| Biomarker | |||
| Peak CK‐MB | |||
| Mean±SD | 282.9±406.5 | 228.4±260.7 | 0.09 |
| Median (IQR) | 171.0 (268) | 149.6 (205.6) | 0.18 |
| GRACE risk score | 141.8±32.6 | 145.3±34.9 | 0.32 |
CK‐MB indicates creatine kinase isoenzyme MB; GRACE, Global Registry of Acute Coronary Events; IQR, interquartile range.
Plus–minus values are means±SD.
Anterior location was defined by the use of electrocardiography as any contiguous ST‐segment elevation from V1 to V6.
Access and Timeliness to PCI Hospitals
The mean delay time from the onset of symptoms to the first medical contact (2.6±4.9 versus 2.6±5.3 hours; P=0.98) was similar, and the rate of self‐transport to reach the first institution (70.8% versus 87.3%; P<0.001) was high to public and private service, respectively (Table 2). In both services, the mean distance traveled by patients from chest pain scene to the hospital with angioplasty was 74±71.27 km versus 28.2±55.60 km (P<0.001), respectively; however, the patients of the public service went through 1 (77.1% versus 25.4%; P<0.001) or more institutions (21.7% versus 0.9%; P<0.001) (Table 2). The mean time between onset of symptoms and arrival at the PCI hospital was higher for the SUS patients compared with the users of the private system (25.4±36.5 versus 9.0±21 hours; P<0.001, respectively) (Table 2). For those patients who received primary PCI, symptom onset to arrival at the PCI hospital was also higher for the SUS patients (7.9±3.7 versus 3.8±3.9 hours; P<0.001) (Table 2). The mean hospital length of stay was higher for the SUS patients (9.8±7.2 versus 8.9±7.9 hours; P<0.001) (Table 2).
Table 2.
Access and Timeliness to PCI Hospitalsa
| Variable | Public (N=589) | Private (N=118) | P Value |
|---|---|---|---|
| Access | |||
| Means of transportation to first facility, n/N (%) | <0.001 | ||
| Self‐transported | 412/582 (70.8) | 103/118 (87.3) | |
| Emergency medical services | 49/582 (8.4) | 4/118 (3.4) | |
| Other | 121/582 (20.8) | 11/118 (9.3) | |
| Hospitals visited before PCI hospital, n (%) | |||
| 0 | 7 (1.2) | 87 (73.7) | <0.001 |
| 1 | 454 (77.1) | 30 (25.4) | |
| 2 | 113 (19.2) | 1 (0.9) | |
| 3 | 15 (2.5) | 0 | |
| Distance from scene of chest pain to PCI hospital, km | |||
| Mean±SD | 74±71.27 | 28.2±55.60 | <0.001 |
| Median (IQR) | 68.2 (101.7) | 6.2 (17.4) | <0.001 |
| Timeliness | |||
| Symptom onset to first medical contact, h | 2.6±4.9 | 2.6±5.3 | 0.98 |
| Medical contact to PCI hospital, h | 22.9±36.1 | 6.4±20.4 | <0.001 |
| Symptom onset to arrival at PCI hospital for all patients, h | 25.4±36.5 | 9.0±21 | <0.001 |
| Symptom onset to arrival at PCI hospital for patients who received PCI strategy, h | 7.9±3.7 | 3.8±3.9 | <0.001 |
| Door‐to‐balloon time, min | |||
| Mean±SD | 121.2±107.1 | 129.8±90.2 | 0.48 |
| Median (IQR) | 100 (80.2) | 115.5 (81.8) | 0.08 |
| ≤90 min, % | 123 (46.9) | 36 (38.3) | 0.15 |
| Length of stay, d | 9.8±7.2 | 8.9±7.9 | <0.001 |
| Length of stay, n (%) | |||
| ≥5 d | 187 (31.7) | 50 (42.4) | 0.04 |
| 6–10 d | 225 (38.2) | 43 (36.4) | |
| ≥10 d | 177 (30.1) | 25 (21.2) | |
IQR indicates interquartile range; PCI, percutaneous coronary intervention.
Plus–minus values are means±SD.
Medical Treatment, Reperfusion, and Revascularization Rates
The rates of use of clopidogrel (96.8% versus 31.4%; P<0.001) and angiotensin‐converting enzyme inhibitors (73.1% versus 29.7%; P<0.001) was higher for the SUS patients. On the other hand, the use of ticagrelor (0.7% versus 70.3%; P<0.001), β‐blockers (27.9% versus 47.5%; P<0.001), and angiotensin receptor blockers (7.3% versus 24.6%; P<0.001) was higher for private patients (Table 3).
Table 3.
Medical Treatment, Rates of Reperfusion, and Rates of Revascularizationa
| Variable | Public (N=589) | Private (N=118) | P Value |
|---|---|---|---|
| In‐hospital medications within 24 h, n/N (%) | |||
| Aspirin | 573/587 (97.6) | 113/118 (95.8) | 0.25 |
| Clopidogrel | 568/589 (96.8) | 36/118 (30) | <0.001 |
| Ticagrelor | 4/587 (0.7) | 82/118 (70) | <0.001 |
| Any ADP inhibitors | 571/587 (97.4) | 118/118 (100) | 0.09 |
| β‐Blocker | 164/587 (27.9) | 56/118 (47.5) | <0.001 |
| Statin | 516/587 (87.9) | 102/118 (86.4) | 0.65 |
| ACE inhibitor | 429/587 (73.1) | 35/118 (29.7) | <0.001 |
| ARB | 43/586 (7.3) | 29/118 (24.6) | <0.001 |
| Diuretics | 89/587 (15.2) | 12/118 (10.2) | 0.15 |
| Aldosterone antagonists | 34/587 (5.8) | 4/118 (3.4) | 0.29 |
| Calcium channel blockers | 67/587 (11.4) | 7/118 (5.9) | 0.08 |
| Nitrates | 197/587 (33.6) | 38/118 (32.2) | 0.77 |
| Heparin | 338/587 (57.8) | 74/118 (62.7) | 0.30 |
| Insulin | 86/587 (14.6) | 30/118 (25.4) | 0.004 |
| Reperfusion, n (%) | |||
| Total | 280 (47.5) | 94 (79.7) | <0.001 |
| Fibrinolytic therapy | 15 (2.5) | 2 (1.7) | 0.58 |
| Primary PCI | 265 (45.0) | 92 (78.0) | <0.001 |
| Revascularization, n (%) | |||
| Nonprimary PCI | 194 (32.9) | 23 (19.5) | 0.003 |
| CABG | 17 (2.9) | 7 (5.9) | 0.09 |
ACE indicates angiotensin‐converting enzyme inhibitor; ARB, angiotensin receptor blockers; CABG, coronary artery bypass grafting; PCI, percutaneous coronary intervention.
Plus–minus values are means±SD.
Rates of use of fibrinolytics before arriving at the PCI hospital were extremely low in both groups (2.5% versus 1.7%; P=0.58). Rates of primary PCI use were significantly lower for the SUS patients (45% versus 78%; P<0.001) (Table 3). Rates of nonprimary PCI were higher for the SUS patients (32.9% versus 19.5%; P<0.001) (Table 3).
Mortality Rates
A 30‐day mortality occurred in 70 of 589 of the SUS patients (11.9%), and in 7 of 118 patients (5.9%) in the private hospitals. In the unadjusted model, the odds ratio for 30‐day mortality for the SUS patients was higher (odds ratio, 2.96; 95% CI, 1.15–7.61; P=0.02; Table 4). In the model adjusted for age and sex, the odds ratio for 30‐day mortality for the SUS patients was 2.59 (95% CI, 1.12–5.97; P=0.02). When adjusted for age, sex, risk factors, family history of coronary artery disease, and GRACE risk score, it was 3.00 (95% CI, 1.20–7.52; P=0.02; Table 4). In the fully adjusted model, the odds ratio for 30‐day mortality for the SUS group, adjusted for age, sex, risk factors, family history of CAD, GRACE risk score, and reperfusion was 2.96 (95% CI, 1.15–7.61; P=0.02; Table 4).
Table 4.
Odds Ratio for 30‐Day Mortality Among SUS Users With STEMI, in Comparison With Users of Private Healthcare Insurance
| Model | Increase in Odds of 30‐Day Mortality | P Valuea |
|---|---|---|
| OR (95% CI) | ||
| Unadjusted | 2.21 (0.99–4.93) | 0.05 |
| Adjusted for age and sex | 2.59 (1.12–5.97) | 0.02 |
| Adjusted for age, sex, risk factors, family history of CAD, and GRACE risk score | 3.00 (1.20–7.52) | 0.02 |
CAD indicates coronary artery disease; GRACE, Global Registry of Acute Coronary Events; OR, odds ratio; STEMI, ST‐segment‐elevation myocardial infarction; SUS, Unified Health System.
P values based on adjustment for clustering of data within hospital.
Discussion
In this prospective, observational cohort study on the access, management, and outcomes of patients with STEMI, using data from the VICTIM register, it was found that, first, the mean time of delay from symptoms to arrival at a PCI hospital was much higher for the SUS patients; second, the SUS patients were less likely to receive reperfusion; and third, after several adjustments for confounders, the SUS patients presented a higher 30‐day mortality compared with private patients. These findings provide the best evidence so far that the Brazilian public healthcare system for patients with STEMI is falling short on equity.
Previously, a small and nonrepresentative study verified that 20.6% of the SUS patients with STEMI received fibrinolysis, compared with 54% of private patients. In addition, hospital mortality was 19.5% for the SUS patients, as compared with 4.8% for private patients.14 Unfortunately, no data were provided with respect to the prehospital phase of STEMI care, and for convenience the authors selected only 2 hospitals.
Our data showed that only 2.5% of the SUS patients, and 1.7% of private patients admitted to 1 of the 4 PCI‐available hospitals received fibrinolytic therapy before arriving. According to guidelines, all patients undergoing fibrinolysis must be sent to a PCI hospital within 24 hours.15 Therefore, these rates for the use of fibrinolysis may represent the current practice of nontertiary hospitals within Sergipe state.
These numbers contrast with the largest Brazilian registry, the BRACE (Brazilian Registry on Acute Coronary Syndromes) study,16 which enrolled, by convenience, 71 hospitals from all main regions of the country. The rates of use of reperfusion therapy varied between 52.5% in the north‐northeast region to 75.5% in the south‐southeast region. Nevertheless, no data were provided with respect to the distribution of the SUS and private patients or for rates of reperfusion between these 2 groups.
During the study period, only 45% of the SUS patients and 78% of the private hospital patients admitted to a PCI hospital received primary PCI. These data confirm a substantial underutilization of primary PCI therapy, even for patients who have access to what may represent the best scenario for treating STEMI, also found in other studies.17 From symptom onset to arrival at a PCI hospital, the delay for the SUS patients was ≈3 times higher. Approximately 50% of SUS patients arrived at the PCI hospital after the 12‐hour window for reperfusion. Even for those who arrived during the reperfusion window at the PCI hospital, the SUS patients spent twice the time of the private patients. For SUS patients, as it is required STEMI confirmation at a smaller center prior to referral to the PCI hospital, this delay could explain most of the observed disparities. Approximately two thirds of the STEMI population arrived at the first hospital by self‐ transportation, indicating the lack of effectiveness of the public emergency medical transport system to assist patients with STEMI. In addition, 73.3% of private patients had direct access to the PCI hospital, compared with only 1.2% of the SUS patients. Before arrival at the PCI hospital, 77.1%, 19.2%, and 2.5% of the SUS patients visited 1, 2, or 3 hospitals, respectively. Moreover, the distance traveled from the scene of the chest pain to a PCI hospital was higher for the SUS patients. The Sergipe public healthcare network is composed of 7 secondary hospitals distributed according to major regions and primary smaller healthcare clinics, some of these hospitals with capacity to perform ECG consultation by telemedicine service. Unfortunately, most of the SUS patients could have been given thrombolytics at this level and referred to the PCI hospital within 24 hours for pharmaco‐invasive treatment. Nevertheless, there are no evidence‐based reperfusion protocols to assist these patients with STEMI outside the public tertiary hospital. Therefore, SUS patients diagnosed at primary or secondary centers necessarily need to be referred to the public PCI hospital to receive reperfusion. SUS patients with STEMI arriving at a private PCI hospital must receive primary PCI before being referred to the public PCI hospital. Altogether, these data confirm that the Brazilian public healthcare system must improve substantially to reach the promise of offering equity on access and use of effective therapies for patients with STEMI. A hub‐and‐spoke model, as successfully implemented in India, could be an effective solution to mitigate such disparities observed in Brazil.18
At the PCI hospital level, door‐to‐balloon time was above the recommended time in both groups, higher than what has been recommended and found in other studies.19 Regarding medical treatment, β‐blockers were less likely to be prescribed within the first 24 hours for the SUS patients, despite similar GRACE risk scores between the 2 groups. As less than 50% of the SUS patients received primary PCI, β‐blocker underuse in the SUS patients might have been critical for the mortality outcome. Because of the restrictive national public healthcare policy in Brazil, the SUS patients have access to only clopidogrel, despite the current evidence of superiority of ticagrelor.15, 20 In contrast, in private patients, and as recommended by current guidelines, ticagrelor was the preferred ADP inhibitor.15, 20, 21 ACE inhibitors were more likely to be prescribed for the SUS patients, and angiotensin receptor blockers were more likely to be prescribed for private patients. As this practice is not supported by guidelines, marketing and commercial issues might explain the clinical decision‐making process at private hospitals.
Despite similar levels of disease severity, as evaluated by the GRACE risk score, the SUS patients presented twice the 30‐day mortality when compared with private patients. The higher 30‐day mortality persisted even after the full adjustment, which included reperfusion access.22 We must point out that, in addition to the lower rates of reperfusion in the SUS patients, we also noted a higher delay from symptom onset to arrival at a PCI hospital, experienced by the SUS patients who received primary PCI, than for private hospital patients, indicating that for those who received primary PCI, its effectiveness might have been lower for the SUS patients.
Compared with previous studies, our study has a major strength. Our registry covered all PCI hospitals of 1 Brazilian state and has a very low percentage of losses during follow‐up. Therefore, this is the most representative study addressing health insurance–related disparities in reperfusion and mortality for patients with STEMI in Brazil. The present study may serve as a template to create a national registry aimed at ameliorating quality‐of‐care data and, as a consequence, leveraging the cycle of improvement. Our study has important limitations. First, we collected data only from PCI hospitals. As we do not have data regarding rates of reperfusion and mortality at non‐PCI hospitals, disparities for the SUS patients not sent to PCI hospitals might have happened. Second, the longer delay to hospital arrival at the PCI hospital might have added survival bias to the SUS patients. Third, the low level of education, especially in the SUS group, compromised the self‐reported information with respect to personal medical history, with a trend to underreporting risk factors and comorbidities. Nevertheless, this fact might have attenuated the adjusted mortality difference between the SUS and private patients. In conclusion, this statewide‐level study demonstrates that the Brazilian healthcare system is deficient in providing care to its users. Fibrinolytics were impressively underused equally for public and private patients. Door‐to‐balloon time was above the recommendation at both public and private hospitals. The delay in reaching a PCI hospital was ≈3 times higher for the SUS patients. Primary PCI was underused in both groups, but especially in the SUS patients. More importantly, the SUS patients were significantly more likely to die during the 30‐day follow‐up, indicating that the Brazilian public health system may be falling short on equity. Our study underscores room for improvement for private and public users. Nevertheless, as the vast majority of the Brazilian population is dependent on SUS to have access to responsive cardiovascular health care, integrating the logistics of evidence‐based STEMI protocols at primary, secondary, and tertiary public hospitals will be the most important step to improve the quality of care and to decrease disparities for patients with STEMI in Brazil.
Sources of Funding
The VICTIM register was funded by the Universal Public Call No. 14/2013, developed by the National Council for Scientific and Technological Development (CNPq).
Disclosures
Dr Sousa reports that he has received speaking fees from Aché, Bayer and Pfizer. The remaining authors have no disclosures to report.
Supporting information
Appendix S1. All investigators described below worked actively collecting data during the study period, VICTIM register.
Acknowledgments
We thank the professionals of the collection institutions, the patients who agreed to participate in the study, and all the researchers participating in the VICTIM Study Group.
(J Am Heart Assoc. 2019;8:e013057 DOI: 10.1161/JAHA.119.013057.)
References
- 1. Brasil. Instituto de Pesquisa de Relações Internacionais . As 15 maiores economias do mundo. April. 2017. Available at: http://www.funag.gov.br/ipri/index.php/indicadores/47-estatisticas/94-as-15-maiores-economias-do-mundo-em-pib-e-pib-ppp. Accessed January 23, 2018.
- 2. United Nations Development Programme . Human Development Report. New York: UN Plaza. 2016. 286 p. Available at: http://www.br.undp.org/content/dam/brazil/docs/RelatoriosDesenvolvimento/undp-br-2016-human-development-report-2017.pdf. Accessed January 9, 2017.
- 3. Brasil. Constituição , Constituição da República Federativa do Brasil. Brasília, DF: Senado Federal; 1988. Available at: http://www.planalto.gov.br/ccivil_03/constituicao/ConstituicaoCompilado.htm. Accessed January 19, 2016.
- 4. Brasil . Presidência da República. Lei n° 8.080, de 19 de setembro de 1990. Dispõe sobre as condições para a promoção, proteção e recuperação da saúde, a organização e o funcionamento dos serviços correspondentes e dá outras providências. Brasília, DF; 1990. 2. Brasil. [Constituição (1988)]. Available at: http://www.planalto.gov.br/ccivil_03/Leis/L8080.htm. Accessed January 19, 2016.
- 5. Santosa A, Wall S, Fottrell E, Högberg U, Byass P. The development and experience of epidemiological transition theory over four decades: a systematic review. Glob Health Action. 2014;7:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ribeiro ALP, Duncan BB, Brant LCC, Lotufo PA, Mill JG, Barreto SM. Cardiovascular health in Brazil—trends and perspectives. Circulation. 2016;133:422–433. [DOI] [PubMed] [Google Scholar]
- 7. Piva e Mattos LA, Berwanger O, Santos ES, Reis HJ, Romano ER, Petriz JL, Sousa AC, Neuenschwander FC, Guimarães JI, Andrade JP. Clinical outcomes at 30 days in the Brazilian Registry of Acute Coronary Syndromes (ACCEPT). Arq Bras Cardiol. 2013;100:6–13. [DOI] [PubMed] [Google Scholar]
- 8. Wang R, Neuenschwander FC, Lima‐Filho A, Moreira CM, Santos ES, Reis HJL, Romano ER, Piva e Matos A, Berwanger O, Andrade JP. Use of evidence‐based interventions in acute coronary syndrome—subanalysis of the ACCEPT registry. Arq Bras Cardiol. 2014;102:319–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Oliveira JC, Barreto‐Filho JA. Public health policy based on “Made‐in‐Brazil” science: a challenge for the arquivosbrasileiros de cardiologia. Arq Bras Cardiol. 2015;105:211–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Krumholz HM. Outcomes research: generating evidence for best practice and policies. Circulation. 2008;118:309–318. [DOI] [PubMed] [Google Scholar]
- 11. Basu S, Andrews J, Kishore S, Panjabi R, Stuckler D. Comparative performance of private and public healthcare systems in low‐ and middle‐income countries: a systematic review. PLoS Med. 2012;9:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Instituto Brasileiro de Geografia e Estatísica . Pesquisa nacional de saúde : 2013: acesso e utilização dos serviços de saúde, acidentes e violências : Brasil, grandes regiões e unidades da federação. Rio de Janeiro: IBGE; 2015. Available at: http://biblioteca.ibge.gov.br/visualizacao/livros/liv94074.pdf. Accessed February 12, 2017.
- 13. Brasil Instituto Brasileiro de Geografia e Estatísica . Pesquisa Nacional de Saúde 2013: Acesso e Utilização dos Serviços de Saúde, Acidentes e Violências. Diretoria de Pesquisas, Coordenação de Trabalho e Rendimento, Pesquisa Nacional de Saúde. [publicação online]. Sergipe: IBGE; 2013. Available at: http://www.ibge.gov.br/estadosat/temas.php?sigla=se&tema=pns_2013_util_serv_saude. Accessed May 02, 2017.
- 14. Ferreira GM, Correia LC, Reis H, Filho CBF, Freitas F, Ferreira GM, Junir I, Oliveira N, Guimarãoes AC. Increased mortality and morbidity due to acute myocardial infarction in a public hospital, in Feira de Santana, Bahia. Arq Bras Cardiol. 2009;93:97–104. [DOI] [PubMed] [Google Scholar]
- 15. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli‐Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimsky P. ESC guidelines for the management of acute myocardial infarction in patients presenting with ST‐segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST‐segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:1991.29087463 [Google Scholar]
- 16. Nicolau JC, Franken M, Lotufo PA, Carvalho AC, Marin Neto JA, Lima FG, Dutra O, Knobel E, Oliveira CC, Timerman S, Stefanini E. Use of demonstrably effective therapies in the treatment of acute coronary syndromes: comparison between different Brazilian regions. Analysis of the Brazilian Registry on Acute Coronary Syndromes (BRACE). Arq Bras Cardiol. 2012;98:282–289. [DOI] [PubMed] [Google Scholar]
- 17. Li J, Li X, Wang Q, Hu S, Wang Y, Masoudi FA, Spertus JA, Krumholz HM, Jiang L. ST‐segment elevation myocardial infarction in China from 2001 to 2011 (the China PEACE Retrospective Acute Myocardial Infarction Study): a retrospective analysis of hospital data. Lancet. 2015;385:441–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Alexander T, Mullasari AS, Joseph G, Kannan K, Veerasekar G, Victor SM, Ayers C, Thomson VS, Subban V, Gnanaraj JP, Narula J, Kumbhani DJ, Nallamothu BK. A system of care for patients with ST‐segment elevation myocardial infarction in India: the Tamil Nadu‐ST‐Segment Elevation Myocardial Infarction Program. JAMA Cardiol. 2017;2:498–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Menees DS, Peterson ED, Wang Y, Curtis JP, Messenger JC, Rumsfeld JS, Gurm HS. Door‐to‐balloon time and mortality among patients undergoing primary PCI. N Engl J Med. 2013;369:901–909. [DOI] [PubMed] [Google Scholar]
- 20. Piegas LS, Timerman A, Feitosa GS, Nicolau JC, Mattos LAP, Andrade MD, Avezum A, Feldman A, De Carvalho ACC, Sousa ACS, Mansur AP, Bozza AEZ, Falcão BAA, Markman Filho B, Polanczyk CA, Gun C, Serrano Junior CV, Oliveira CC, Moreira D, Précoma DB, Magnoni D, Albuquerque DC, Romano ER, Stefanini E, Santos ES, God EMG, Ribeiro EE, Brito Júnior FS, Feitosa‐Filho GS, Arruda GDS, Oliveira GBF, Oliveira GBF, Lima GG, Dohmann HFR, Liguori IM, Costa JR, Saraiva JFK, Maia LN, Moreira LFP, Arrais M, Canesin MF, Coutinho MSSA, Moretti MA, Ghorayeb N, Vieira NW, Dutra OP, Coelho OR, Leães PE, Rossi PRF, Andrade PB, Lemos PA, Pavanello R, Vivacqua Costa RC, Bassan R, Esporcatte R, Miranda R, Giraldez RRCV, Ramos RF, Martins SK, Esteves VBC, Mathias Junior W. V Diretriz da Sociedade Brasileira de Cardiologia sobre Tratamento do Infarto Agudo do Miocárdio com Supradesnível do Segmento ST. Arq Bras Cardiol. 2015;105:1–105. [DOI] [PubMed] [Google Scholar]
- 21. Cannon CP, Brindis RG, Chaitman BR, Cohen DJ, Cross JT Jr, Drozda JP Jr, Fesmire FM, Fintel DJ, Fonarow GC, Fox KA, Gray DT, Harrington RA, Hicks KA, Hollander JE, Krumholz H, Labarthe DR, Long JB, Mascette AM, Meyer C, Peterson ED, Radford MJ, Roe MT, Richmann JB, Selker HP, Shahian DM, Shaw RE, Sprenger S, Swor R, Underberg JA, Van de Werf F, Weiner BH, Weintraub WS. 2013 ACCF/AHA key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes and coronary artery disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Acute Coronary Syndromes and Coronary Artery Disease Clinical Data Standards). Circulation.2013;127:1052–1089. [DOI] [PubMed] [Google Scholar]
- 22. Terkelsen CJ, Sørensen JT, Maeng M, Jensen LO, Tilsted HH, Trautner S, Vach W, Johnsen SP, Thuesen L, Lassen JF. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304:763–771. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. All investigators described below worked actively collecting data during the study period, VICTIM register.


