Abstract
Introduction
This study aimed to review the literature to establish whether there is a best treatment for low-risk ankle fractures in children.
Materials and methods
A systematic review and meta-analysis of trials was undertaken, which compared interventions for ‘low-risk’ ankle fractures in children. A meta-analysis was performed using a random effects model.
Results
Four trials were identified reporting outcomes from 256 patients. All trials reported results using a device that permitted ankle motion compared with more rigid immobilisation. Overall risk of bias was low for three trials and high for one trial. Two trials assessed time to return to normal function. Patients treated in a splint or with a bandage recovering 6–7.5 days sooner than those treated with rigid immobilisation. One trial demonstrated that children returned to school sooner if treated in a bandage rather than in a cast. Two trials found a higher Activity Scale for Kids performance score at four weeks for children treated with splint compared with rigid immobilisation. There was no clear advantage to any device in patient satisfaction, quality of life or total costs.
Discussion
There is no clear best treatment for these injuries. Studies had significant limitations and outcomes were heterogeneous, limiting meta-analysis.
Conclusion
There is a need for a definitive trial to establish the best treatment for ankle fractures and a core outcome set to ensure study findings are consistent and can be analysed in future meta-analyses.
Keywords: Ankle injuries, Ankle, Fractures, Pediatrics, Children, Systematic review
Introduction
Ankle fractures are common, with an annual incidence of 1/1,000 children.1,2 Despite being a common injury, ideal management is unclear, with clinicians unsure how best to immobilise a child with an ankle fracture.3
Ankle fractures in children can be divided into two categories. Fractures can be ‘high risk’ – fractures with significant displacement that require operative reduction to achieve a good outcome. ‘Low-risk’ fractures include occult fractures not visible on x-ray, Salter Harris type 1 fractures with minimal x-ray changes and avulsion fractures. Similarly, nondisplaced fractures in children are usually regarded as low-risk due to the intact periosteum.4
While there is broad agreement that high-risk fractures require intervention, there is less consensus about the ideal management of low-risk fractures. The described and widely-available treatment strategies for low-risk fractures are:
functional: no formal immobilisation beyond a supportive bandage, ice and elevation, enabling early mobilisation but potentially resulting in greater initial pain6,7
ankle brace: provides some support to the ankle with some designs permitting dorsiflexion and plantarflexion; removable to permit bathing and can be taken off at home when discomfort subsides8,9
casted splint: a custom-moulded splint typically formed of lightweight casting material and Velcro straps that can be removed for bathing and resists ankle dorsiflexion and plantarflexion9
cast immobilisation: maximum immobilisation and potential protection; can be weight bearing or non-weight bearing; may improve pain control but limits early motion. Cast treatment is not benign; it may result in additional pressure complications. Cast immobilisation in adolescents causes a decrease in bone mineral density.6,7
The aim of this review was to identify the best treatment for low-risk ankle injuries. The primary outcome was the time taken to recover sufficiently to return to normal activities. Additional outcomes evaluated were functional outcome, pain, complications, general quality of life, satisfaction and economic impact.
Methods
This review was prospectively registered on the PROSPERO database (CRD42018108938)10 and was conducted according Cochrane guidance.11 A protocol modification was introduced following registration to select the highest quality evidence by restricting the studies included to randomised controlled trials and quasi-randomised controlled trials.
Ovid MEDLINE, Embase and Cochrane CENTRAL were searched using a previously published strategy developed by Yeung et al.12 One researcher (BM) reviewed titles and abstracts. Full texts were reviewed by two reviewers (BM and JN) with data extracted using a standardised template. Risk of bias was assessed using the Cochrane revised risk of bias tool.13
Studies were included in this review if the participants enrolled were children aged 0–16 years and if the study described outcomes of ‘low-risk’ ankle fractures. Low-risk fractures were defined as avulsion fractures, fractures distal to the physis and occult fractures diagnosed based on clinical evaluation. To be included, trials also had to compare interventions and report relevant outcomes (but the outcome measures were not predefined).
Statistics and analysis
Outcomes were transformed into means, standard deviations and 95% confidence intervals (CI) in line with techniques in the Cochrane handbook.11 Outcomes were described in a narrative review format and using the forest plot script in R (the R Project).14 Where the data permitted, results were combined in meta-analysis using RevMan5.3, using a random effects model owing to the varied nature of the trials included.15
Results
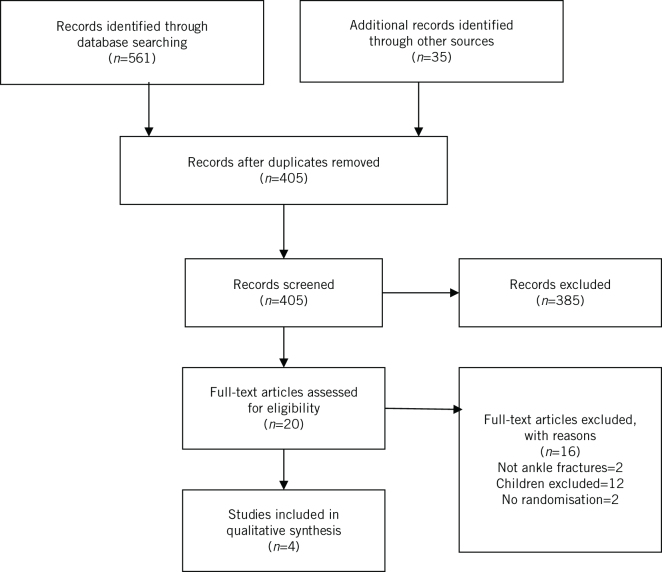
The PRISMA flow diagram is shown in Figure 1. The initial searches yielded 561 papers. Full text review was carried out for 20 papers and four trials met the inclusion criteria.
Figure 1.
PRISMA flow diagram.
Study characteristics
The study characteristics are summarised in Table 1. All four included trials were randomised controlled trials.6–9 One trial was designed as a superiority trial;6 two were non-inferiority trials,8,9 and one did not specify type.7 All trials originated from large, specialised children’s hospitals and, overall, they included 256 children.
Table 1.
Study characteristics for included trials.
| Study | Year | Setting | Participants | Injury | Intervention | Primary outcome | Risk of biasa | |||||||
| Type | (n) | 1 | 2 | 1 | 2 | 3 | 4 | 5 | Overall | |||||
| Boutis et al8 | 2006 | Children’s hospital | Children age 5–15 years, mean age 10 years | 104 | Nondisplaced SH1 with a clinical diagnosis, SH2, avulsion | Air-stirrup ankle brace, 5 days NWB then WBAT, remove brace when pain allows | Below-knee fiberglass cast, 5 days NWB then WBAT, cast off at 3 weeks | Modified ASK-p score at 4 weeks | L | L | L | L | L | L |
| Launay et al6 | 2008 | Children’s hospital | Children age 8–15 years, mean age 14 years | 62 | Ankle injury with no fracture on x-ray | 1-week functional treatment | 1-week plaster immobilisation | Number of days off school by 1 week | L | L | M | L | H | H |
| Barnett et al9 | 2012 | Children’s hospital | Children age 5–15 years, mean age 10 years | 45 | SH1 with tenderness over growth plate and normal x-ray, avulsion lateral talus or lateral malleolus | Air-stirrup ankle brace. WBAT For 2–-4 weeks based on examination at 12–16 days | Removable casted splint, WBAT, for 2–4 weeks based on examination at 12–16 days | ASK-p score at 4 weeks | L | L | L | L | L | L |
| Gleeson et al7 | 1996 | Children’s hospital | Children, unspecified range, mean age 9 years | 45 | Ankle injury with an assessment score > 10 including swelling, growth plate tenderness and inability to bear weight | Tubular bandage and crutches, WBAT | Below knee plaster cast, WBAT, cast off at 2 weeks | Custom score | L | L | M | L | L | L |
a (RoB 2.0)13; risk of bias domain 1: bias from randomisation; 2: bias from deviations from the intended interventions; 3: Missing outcome data; 4: measurement of the outcome; 5: Selection of reported result.
ASK-p, Activity Scale for Kids performance scale; H, high; L, low; M, medium/some concerns; NWB, non-weight bearing; SH1, Salter Harris type 1 fracture; SH2, Salter Harris type 2 fracture; WBAT, weight bearing as tolerated.
The included trials compared outcomes following ankle brace compared with fibreglass cast,8 ankle brace compared with removable casted posterior splint9 and elasticated tubular bandage, or bandage compared with plaster cast.7 For analysis, fibreglass cast, removable casted posterior splint and plaster cast were grouped as a rigid cast group (where ankle movement was restricted) and air-stirrup brace, tubular bandage and bandage were grouped as a mobile brace group. Reported follow-up duration varied between studies from seven days to three months.
Outcome measures
Primary outcome measures are shown in Table 1. Boutis et al reported a modification of the Activity Scale for Kids Performance scale (ASK-p)16 where eight additional ankle questions were added.8 Barnett et al reported the original ASK-p score as their primary outcome9 and Gleeson et al reported a custom composite score of pain, examination features and function.7 Launay et al reported school absenteeism as their primary outcome and also collected quality of life scores for children and their parents using the Vécu et Santé Perçue des Adolescents (VSPa) score.17
Additional outcomes were pain using the Bieri faces score,8 10-point score6 or number of days’ use of analgesia;9 ability to bear weight at four weeks;8,9 return to function;6–9 satisfaction8,9 and complications.8,9
Risk of bias
Risk of bias for three of the trials,7–9 as measured with the Cochrane Risk of Bias 2.0 tool,13 was low. The study by Launay et al was assessed as at a high risk of bias due to the statistical analysis and very high loss to follow-up.6 Their analysis was at high risk of type 1 error due to undertaking 10 t-tests per participant without reducing their alpha value. An additional cause of bias or uncertainty was that Barnett et al that had to close early with difficulties in recruitment.9 In the initial power calculation, 128 patients were due to be recruited but only 45 were randomised so the study was underpowered.
Outcomes
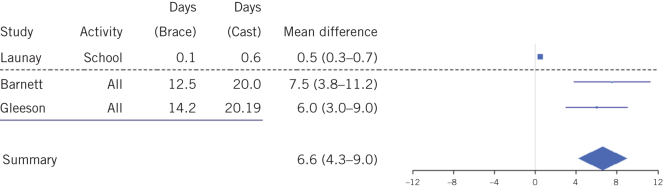
Recovery time to normal activities was reported in three trials.6,7,9 The proportion of children making a full return to activities at four weeks and three months was reported in one trial.8 A forest plot of results with meta-analysis for return to normal activity is shown in Figure 2. Launay et al identified a mean time from injury to return to school of 0.1 days (SD 0.4 days) for children treated with functional treatment compared with 0.6 days (SD 0.8 days) for children treated with a cast (P = 0.04).6 Barnett et al reported a median of 12.5 days (interquartile range, IQR, 8.0–17.5 days) for children to return to normal activity when issued with an ankle brace compared with 20 days (IQR 15.5–23 days) with a removable casted splint (no P-value reported).9 Gleeson et al showed a six-day improvement (95% CI 3–9 days, P = 0.002) in mean time to return to normal activities when a tubular bandage was prescribed compared with two weeks of treatment with a plaster cast.7 Boutis et al reported that 42 patients (80%) treated with a brace had returned to full activity at four weeks compared with 25 (60%) of those who treated in a below knee cast (P = 0.038).8 No rate of return to activity was reported in this study.
Figure 2.
Forest plot for three trials6,7,9 of return to function defined as return to school or all normal activities. Summary diamond for return to normal activities using random effect model. Positive values favour the use of a mobile brace (I2 = 0%).
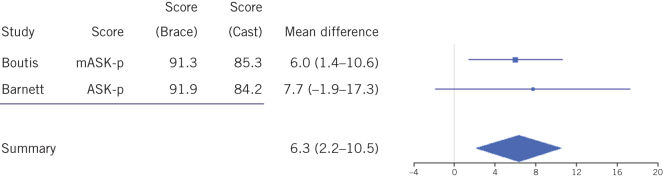
Outcome scoring was performed in three studies.7–9 Barnett et al measured functional outcome at four weeks using ASK-p.9 In Boutis et al’s study, ankle-specific questions were added to this scale to develop a custom modification (with no validation).8 In Gleeson et al, a non-validated performance scale was measured combining pain, tenderness and ability to weight bear at 28 days.7 Forest plot and meta-analysis of ASK-p scores are shown in Figure 3.
Figure 3.
Forest plot of mean difference in function for two trials8,9 at four weeks. Scores are the Activity Scale for kids given in %. Summary diamond constructed with random effects model. Positive values favour the use of a mobile brace (I2 = 0%).
In the largest trial, Boutis et al found a 6.0% improvement (95% CI 1.39–10.61) in the four-week modified ASK-p score when patients were randomised to receive a brace rather than three weeks in a weight-bearing fibreglass cast.8 Barnett et al also found a mean improvement in score of 7.7% (95% CI –1.89, –17.29) when children were treated with a brace rather than a removable casted splint, but this was not statistically significant (P = 0.13).9 Combining these two results in a random effects model gave a mean difference of 6.32% (95% CI 2.16–10.48) in favour of the brace.
Gleeson et al reported function using a non-validated performance tool. This score had a range of possible scores from 3 to 17, with 17 representing worst function. The mean scores were 3.8 for patients treated with a plaster cast and 3.4 for those treated with tubular bandage at 28 days following injury. This was not deemed statistically significant (precise P-value and standard deviations were not given).7
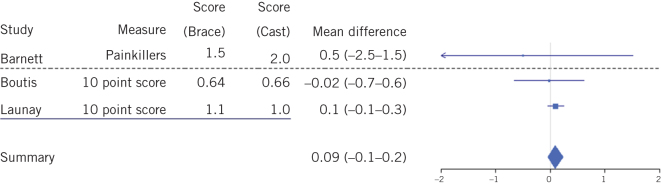
Direct measurements of pain were undertaken in two trials.6,8 Pain was measured indirectly by Barnett et al using numbers of days usage of simple analgesia (paracetamol and ibuprofen).9 Gleeson et al included pain measured on the Bieri faces scale as part of their composite score.7 A forest plot of pain scores is shown in Figure 4. Pain on walking at seven days as measured on a 10-point visual analogue scale was 2.1 (SD 1.8) for children treated with a cast compared with 1.8 (SD 1.1) for those treated with functional treatment in the study by Launay et al.6 Boutis et al reported pain on walking at four weeks, as measured on the five-point revised Bieri face scale, to be 0.33 (SD 0.92) for children treated in a fibreglass cast compared with 0.32 (SD 0.73) for those treated with a brace (P = 0.93).8
Figure 4.
Forest plot for pain reported in three studies.6,8,9 Barnett et al reported the number of days for which simple analgesia was required.9 Boutis et al reported pain at 4 weeks using the faces pain scale, this has been converted into 10-point scale for comparison.8 Launay et al reported pain on a 10-point score at 1 week post injury.6 Summary result is for pain scores. Positive values favour the use of a mobile brace (I2 = 0%).
Barnett et al reported pain as the median number of days requiring analgesia (usually ibuprofen and paracetamol). This was 2.0 days (IQR 0.0–6.0 days) for children treated with a removable casted splint compared with 1.5 days (IQR 1–4) for those treated in a brace (no P-values reported).9 Gleeson et al used pain as part of the composite assessment tool with no pain scores presented in their paper.7
Boutis et al presented 20 patients who needed additional healthcare appointments during their study period. Four patients treated with brace had problems (one rash, three range of motion and strength complaints). Sixteen patients treated in casts also had problems (poor fit, itchy leg range of motion and strength complaints – breakdown not given). This equated to an odds ratio of 0.17 (95% CI 0.05–0.55) in favour of brace treatment.8
Barnett et al reported 15 pressure-related complications. Ten patients treated in a brace developed marks, with three developing blisters. Five patients treated with the removable casted splint developed complications with one pressure mark, two blisters and two patients with heel pain. This equates to an odds ratio of 3.0 (95% CI 0.82–11.0) in favour of the removable casted splint. Of note, six of the patients prescribed the splint who subsequently developed complications were not wearing the recommended protective sock.9 Gleeson et al7 and Launay et al6 did not report any complications.
The trial by Launay et al6 was the only study to report quality of life scores. This trial measured the VSPa score.17 The study presented values for five of the six domains (school life was missing) and the index score. The mean scores were 5.4 points higher (95% CI 0.83–10.0) for physical wellbeing for children given functional treatment and 4.9 points higher (95% CI 2.66–8.58) for relationships with parents for children treated with a cast. Other domains and overall index score showed no difference. Parental scores taken at the same time showed a 10-point difference (95% CI 0.39–19.81) in self-esteem for families with children treated in a plaster, but no difference in any other domain.6
Patient and parent satisfaction was measured in two trials. Boutis et al found that 52.8% of patients treated with a brace were ‘very happy’ at four weeks compared with 18% treated in a cast (P < 0.0001).8 Barnett et al did not find a difference in parental satisfaction, with around 90% stating they would use the same device again.9
Cost was measured in one trial.8 This study found that the mean direct healthcare cost was Canadian $65.7 lower (95% CI 42.94–88.50) for children treated in a brace compared with treatment in a cast. However, the total cost was no different between the groups when parental work loss was included.
Discussion
This review has identified four trials and evaluated the reported outcomes. Despite being a common injury, there are few trials to guide the management of low-risk ankle fractures. Developing a firm conclusion is limited by significant study heterogeneity.
The most important sources of heterogeneity are as follows.
Study participants: all four studies had differing populations of children enrolled with different mean ages. This may have an influence on the reported outcomes.
Included injuries: two trials were clear on the inclusion criteria, with checks by clinicians within the first week of injury to exclude simple sprains.8,9 This may favour cast immobilisation while a fracture begins to unite. The other two trials were broader in terms of the inclusion criteria, and may have included more simple sprains that would have resolved with no intervention.6,7
Treatments: each study used different treatment regimens. Two studies used a similar brace,8,9 and it might be expected that a bandage would perform similarly to a tubular bandage.7 Studies used different forms of solid immobilisation with plaster,6,7 fibreglass casts8 or splint.9 However, the common feature is the prevention of ankle dorsiflexion and plantarflexion.
Outcome measures: none of the trials reported the same primary outcome measure and there was variable reporting of secondary measures and statistical analysis. Only one trial used a previously validated patient reported measure9 and one trial used a validated quality of life score.6
Power and sample size: three studies used a prospective sample size calculation. One trial did not present a sample size calculation so may be underpowered.7
One was not able to recruit and was therefore significantly underpowered.9 One study had a 40% loss to follow up.6 The impact on the findings is unclear. Allowing for these limitations, the trials identified suggest some benefits of permitting these injuries to heal with a brace or splint that allows for early mobilisation of the ankle joint. Meta-analysis showed benefit in favour of using a mobile brace in terms of return to function and functional score at four weeks. Pooled pain scores were higher in patients using a mobile brace, although this was not statistically significant and was less than half a point on a 10-point score.
The clinical significance of a six-day improvement in return to normal function is likely to be relevant to families. The relevance of a 6% higher in pooled ASK-p score is less clear. Children with no disability have been shown to have a mean ASK-p score of 93% and those with mild disability have a mean score of 8618,19 suggesting a clinical important difference of about 7%, although this has not been formally established as a minimal important clinical difference. The pooled effect is under this value, with confidence intervals that exceed it by 4%. It is unclear therefore if this observed improvement is clinically significant.
An important factor in these trials is the compliance with treatment. Surgeons report they are reluctant to issue splints due to fears of early removal.3 However, the pragmatic nature of the included trials accepted the early removal of treatments, and outcomes were at least as good with braces and bandages as with casts and removable splints.
Conclusions
There is insufficient high-quality evidence to conclusively establish the ideal treatment of low-risk ankle fractures. However, the current evidence suggest that there may be benefits in providing treatment that permits ankle plantarflexion and dorsiflexion, which is likely to reduce the time taken for children to return to activities and improve the functional outcome.
There is considerable heterogeneity in the outcomes reported from these trials. An agreed core outcome set would help to address this and ensure regular and robust reporting of relevant outcomes.20 There is also an urgent need for a definitive trial to identify the best treatment for these injuries. Review of the European Union Clinical Trials Registry, ClinicalTrials.gov and ISRCTN registry at 2 November 2018 revealed no ongoing studies.
References
- 1.Lyons RA, Delahunty AM, Kraus D et al. . Children’s fractures: a population based study. Inj Prev 1999; (2): 129–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Landin LA, Danielsson LG. Children’s ankle fractures: classification and epidemiology. Acta Orthop Scand 1983; (4): 634–640. [DOI] [PubMed] [Google Scholar]
- 3.Boutis K, Howard A, Constantine E et al. . Evidence into practice: pediatric orthopaedic surgeon use of removable splints for common pediatric fractures. J Pediatr Orthop 2015; (1): 18–23. [DOI] [PubMed] [Google Scholar]
- 4.Morrissy RT, Weinstein SL. Lovell and Winter’s Pediatric Orthopaedics, 6th ed Philadelphia, PA: Lippincott Williams and Wilkins; 2006. [Google Scholar]
- 5.Su AW, Larson AN. Pediatric ankle fractures: concepts and treatment principles. Foot Ankle Clin 2015; (4): 705–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Launay F, Barrau K, Simeoni M et al. . [Ankle injury without fracture in children: cast immobilization versus symptomatic treatment. Impact on absenteeism and quality of life]. Arch Pediatr 2008; (12): 1,749–1,755. [DOI] [PubMed] [Google Scholar]
- 7.Gleeson AP, Stuart MJ, Wilson B, Phillips B. Ultrasound assessment and conservative management of inversion injuries of the ankle in children: plaster of Paris versus Tubigrip. J Bone Joint Surg Br 1996; (3): 484–487. [PubMed] [Google Scholar]
- 8.Boutis K, Willan AR, Babyn P et al. . A randomized, controlled trial of a removable brace versus casting in children with low-risk ankle fractures. Pediatrics 2007; (6): e1256-63. [DOI] [PubMed] [Google Scholar]
- 9.Barnett PLJ, Lee MH, Oh L et al. . Functional outcome after air-stirrup ankle brace or fiberglass backslab for pediatric low-risk ankle fractures: a randomized observer-blinded controlled trial. Pediatr Emerg Care 2012; (8): 745–749. [DOI] [PubMed] [Google Scholar]
- 10.Marson BA, Deshmukh S, Ng J et al. . Outcome of ankle injuries in children: a systematic review. PROSPERO 2018 CRD42018108938 www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018108938 (cited February 2019).
- 11.Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions, version 6 Oxford: Cochrane Collaboration, 2018. [Google Scholar]
- 12.Yeung DE, Jia X, Miller CA, Barker SL. Interventions for treating ankle fractures in children. Cochrane Database Syst Rev 2016; : CD010836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higgins JPT, Altman DG, Gøtzsche PC et al. . The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011; : d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gordon M. Introduction to forest plots. https://cran.r-project.org/web/packages/forestplot/vignettes/forestplot.html (cited February 2019).
- 15.The Nordic Cochrane Centre Review Manager (RevMan), version 5.3 Copenhagen: Cochrane Collaboration, 2014. [Google Scholar]
- 16.Young NL, Williams JI, Yoshida KK, Wright JG. Measurement properties of the Activities Scale for Kids. J Clin Epidemiol 2000; (2): 125–137. [DOI] [PubMed] [Google Scholar]
- 17.Simeoni MC, Auquier P, Antoniotti S et al. . Validation of a French health-related quality of life instrument for adolescents: the VSP-A. Qual Life Res 2000; (4): 393–403. [DOI] [PubMed] [Google Scholar]
- 18.Young NL, Williams JI, Yoshida KK, Wright JG. Measurement properties of the activities scale for kids. J Clin Epidemiol 2000; (2): 125–137. [DOI] [PubMed] [Google Scholar]
- 19.Plint AC, Gaboury I, Owen J, Young NL. Activities scale for kids: an analysis of normals. J Pediatr Orthop 2003; (6): 788–790. [PubMed] [Google Scholar]
- 20.Sinha IP, Altman DG, Beresford M et al. . Standard 5: selection, measurement, and reporting of outcomes in clinical trials in children. Pediatrics 2012; (Suppl): S146–S152. [DOI] [PubMed] [Google Scholar]