Abstract
Tranexamic acid (TXA) has been used to manage menstrual bleeding and reduce bleeding during orthopedic procedures, but has not been widely used in urology. We present a patient with refractory gross hematuria with required therapeutic anticoagulation who failed multiple other measures to control prostatic bleeding. This patient's hematuria abated with endoscopic localized injection of tranexamic acid into the prostate. The effects were durable with no bleeding recurrence reported while maintaining therapeutic anticoagulation.
Introduction
Current methods for management of severe gross hematuria include continuous bladder irrigation, discontinuation of anticoagulation, bladder instillations of various hemostatic agents, percutaneous urinary diversion, or interventional radiology embolization. When severe gross hematuria occurs in the context of anticoagulation that cannot be stopped, a urologist is tasked with localized management of bleeding.. In this case, we describe a patient with a history of cryoablation and external beam radiation of the prostate who underwent mechanical aortic valve replacement with mandatory systemic anticoagulation and shortly thereafter developed severe refractory gross hematuria requiring multiple transfusions. The patient's hematuria was unresponsive to standard management modalities given that the source of his bleeding was the prostate as opposed to the bladder, and was ultimately managed with localized injection of tranexamic acid (TXA) into the prostate.
TXA has been used to mitigate menstrual bleeding and reduce bleeding in orthopedic procedures.1,2 Within a urologic context, TXA has been used via bladder instillation to reduce gross hematuria, as oral therapy to manage polycystic kidney disease-related hematuria, and during radical cystectomy.3, 4, 5 Herein, we describe the use of TXA directly injected into the prostate to gain local control of bleeding while maintaining full anticoagulation for recent placement of a mechanical aortic valve.
Case presentation
The patient is a 75-year-old man who underwent cystoscopic dilation of an incidentally diagnosed bladder neck contracture at the time of an aortic valve replacement after the cardiothoracic team was unable to place an intraoperative Foley catheter. A 16 French Foley catheter was left following the dilation. Valve replacement was performed successfully. Thereafter the patient developed gross hematuria with clots while therapeutically anticoagulated with a goal INR of 2.5–3.5 to prevent risk of thrombosis to the mechanical valve.
Over the next several weeks, multiple maneuvers were attempted to control bleeding without success, including traction and continuous bladder irrigation. The patient eventually re-presented following discharge in clot retention and with anemia requiring transfusion. Cystoscopy and fulguration was next performed, revealing a generally healthy-appearing bladder without radiation changes. The prostate appeared very white and friable with a few areas of punctate bleeding that were cauterized (Fig. 1). Following the procedure, the gross hematuria abated marginally, but the urine remained punch-red at time of discharge. The patient was discharged with the Foley in place. He returned again around one week later with worsening gross hematuria, clot retention, and anemia. Discussion with cardiology resulted in reduction of the patient's INR goal from 2.5 to 3.5 to 2 to 2.5, but they recommended against cessation of anticoagulation given that the patient was still fewer than six months from his original surgery.
Fig. 1.
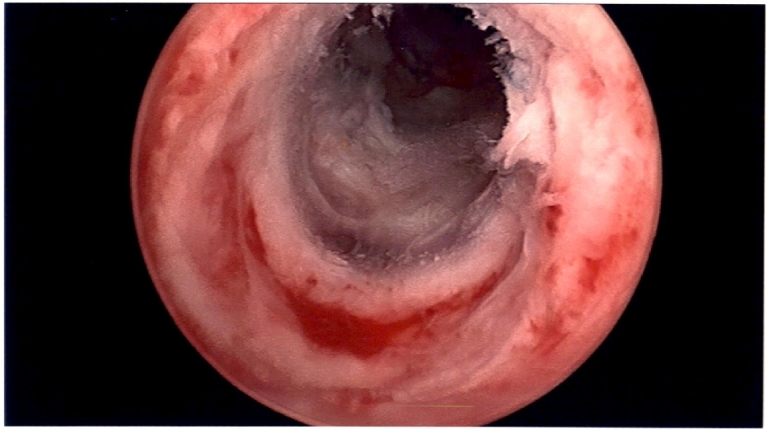
Cystoscopic appearance of bleeding prostate that had undergone cryoablation and radiation.
The patient's gross hematuria persisted, requiring additional transfusion. Alum irrigation was attempted, but was largely ineffective given that the source of bleeding was the prostate which was not effectively contacted during intravesical treatments with the catheter in place. Prostatic artery embolization was felt to be high-risk given the need for femoral artery access on a patient on therapeutic anticoagulation.
We finally elected to attempt TXA directly injected into the prostate under cystoscopic vision. The patient was consented and counseled about the specific nature and risks of this procedure. With the assistance of pharmacy colleagues, 1 gm of TXA (Cyklokapron) was dissolved in 50 ml of injectable 0.9% saline. Using an endoscopic 35cm 23GA 8mm urethral needle, a total volume of 20mL was injected into the prostate at five sites directly beneath the areas of suspected bleeding. Pinpoint areas were cauterized with monopolar electrocautery.
There was rapid improvement with yellow urine following evacuation of remaining clots and bladder irrigation. His pre- and postoperative INR remained stable at 2.5. He was discharged to home in stable condition the following day. At now over six months from this procedure, the patient has not been readmitted or reported any recurrence of gross hematuria.
Discussion
Tranexamic acid significantly reduces bleeding in a wide variety of applications and has been found to be safe in oral, IV and instillation forms. Because of its tolerability as an intravenous medication, we hypothesized that TXA would be safe if injected locally and thus safe to use in the context of the patient's systemic anticoagulation. Furthermore, with an injection, the medication could be better targeted and thus concentrated and sequestered to a local area. Though there was a historical concern for contraindication in its use for hematuria because of antifibrinolytic properties and concerns for clots obstructing the kidneys, a study from 2011 did not demonstrate this concern.4
From a theoretical standpoint, TXA injection offers several advantages. The methodology biologically modulates the balance of coagulation locally rather than systemically. By minimizing local injury such as through cautery, it does not restart the process of wound healing, which would be impaired in a fully anticoagulated patient. The approach was technically simple, and after weeks of ineffective treatments in a patient with a requirement for anticoagulation, worked rapidly. The results were durable at follow-up suggesting that the initial local control may possibly be permanent over time.
Managing refractory gross hematuria is challenging, but injection of TXA is another method available for management in complex situations. Though this case reports a situation where there were few other options available, one could make the case that the simplicity of the procedure may be effective in a wider range of applications. Tranexamic acid delivered impressive results in a fully-anticoagulated patient. With prior FDA approval already in place and widespread market availability, TXA could start being used immediately in refractory cases.
Conclusions
Tranexamic acid injection is an option to consider for management of refractory lower tract bleeding. It allows for local modulation of fibrinolysis pathway without systemic effects and can be used in conjunction with other modalities. More studies are needed to fully optimize protocols and application.
Acknowledgements
No source of funding.
Contributor Information
Brian Le, Email: leb@urology.wisc.edu.
Gray Roberge, Email: groberge@uwhealth.org.
References
- 1.Lukes A.S., Moore K.A., Muse K.N. Tranexamic acid treatment for heavy menstrual bleeding: a randomized controlled trial. Obstet Gynecol. 2010;116(4):865–875. doi: 10.1097/AOG.0b013e3181f20177. [DOI] [PubMed] [Google Scholar]
- 2.Luo Z.Y., Wang H.Y., Wang D., Zhou K., Pei F.X., Zhou Z.K. Oral vs intravenous vs topical tranexamic acid in primary hip arthroplasty: a prospective, randomized, double-blind, controlled study. J Arthroplast. 2018;33(3):786–793. doi: 10.1016/j.arth.2017.09.062. [DOI] [PubMed] [Google Scholar]
- 3.Moharamzadeh P., Ojaghihaghighi S., Amjadi M., Rahmani F., Farjamnia A. Effect of tranexamic acid on gross hematuria: a pilot randomized clinical trial study. Am J Emerg Med. 2017;35(12):1922–1925. doi: 10.1016/j.ajem.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 4.Alameel T., West M. Tranexamic Acid treatment of life-threatening hematuria in polycystic kidney disease. Int J Nephrol. 2011;2011:203579. doi: 10.4061/2011/203579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zaid H.B., Yang D.Y., Tollefson M.K. Efficacy and safety of intraoperative tranexamic acid infusion for reducing blood transfusion during open radical cystectomy. Urology. 2016;92:57–62. doi: 10.1016/j.urology.2016.02.044. [DOI] [PubMed] [Google Scholar]


