Abstract
Background
Injuries to the lateral collateral ligament (LCL) are most commonly associated with anterior cruciate ligament (ACL) injury than with posterior cruciate ligament (PCL) injury. There is currently a paucity in the literature in regards to treatment and outcomes of such lesions.
Methods
30 patients underwent surgical treatment of concomitant LCL and ACL injury or concomitant LCL and PCL injury with follow-up postoperative period of two years. The Lysholm score and varus stress radiographs was calculated and analysed before and at 6, 12, and 24 months postoperatively.
Results
There was a significant increase in scores between two timepoints over the follow-up period for both groups: before surgery and after 6 months, and between 6 and 12 months (p < 0.05). The lateral joint opening measured on the varus stress radiographs was greater in group 2 than in group 1 before surgery (p = 0.04). When assessing each group separately, the lateral joint opening decreased at each timepoint in the first year for both groups (p < 0.05).
Conclusion
Patients diagnosed with combined LCL and PCL injuries were shown to have a higher degree of lateral opening at the time of injury when compared to patients with combined LCL and ACL injuries. However, there was no difference in lateral joint opening on stress radiography after 12 months postoperatively in either group. Finally Lysholm scores for both groups significantly increased between the preoperative period and 6 months postoperatively, as well as between 6 months and 12 months postoperatively.
Level of evidence
III
Keywords: Lateral collateral ligament, Anterior cruciate ligament, Posterior cruciate ligament, Treatment, Stress radiographs, Lysholm score
1. Introduction
The lateral collateral ligament (LCL) is the primary restraint to varus stress of the knee and secondary restraint of external rotation.1 In general, its injury results from a rotational movement or laterally directed trauma to the medial region of the knee.2 Isolated LCL lesion of the knee is uncommon, affecting only 2–7% of cases.3, 4, 5 In most cases, the lesion of this structure occurs associated with lesions of the posterolateral compartment or the cruciate ligaments.6
Surgical treatment of combined lesions usually indicated.7, 8, 9 Depending on the structures involved and timing of surgical intervention, surgeons can choose to repair or reconstruct these structures. The literature has shown superior results for surgical reconstruction compared to primary repair, especially for the treatment of chronic injuries.10,11
Injuries to the LCL are most commonly associated with anterior cruciate ligament (ACL) injury, although traumatic LCL injuries can also be associated with posterior cruciate ligament (PCL) injury. There is currently a paucity in the literature in regards to treatment and outcomes of such lesions and if these metrics are dependent on the severity of the initial trauma.12, 13, 14
The aim of the present study was to evaluate and compare the knee lateral stability and function of patients following combined LCL and ACL reconstruction to patients following LCL and PCL reconstruction throughout the 24-month follow-up period. The hypothesis of the study is that both combined injury types could be treated with reconstruction of both injured ligaments, yielding good functional and stability results regardless of trauma pattern.
2. Material and methods
This study was evaluated and approved by the Research Ethics Committee (IRB No. 2697592). The present study design is a prospective cohort study of 30 patients undergoing surgical reconstruction of LCL injury associated with ACL or PCL injury from January 2014 to June 2015, with at least two years of postoperative follow-up.
The inclusion criteria were: patients age 18–55 years, clinically and radiographically (radiographs and magnetic resonance imaging) confirmed LCL and cruciate ligament injury, and appropriate alignment of the lower limbs. The non-inclusion criteria were: patients with associated posterolateral corner injuries; meniscal lesions amenable to repair; systemic, autoimmune, or infectious disease processes; and surgeries performed in the acute phase in which the ligament repair was chosen. Patients that abandoned or did not agree to continue with the study, those who changed their surgical procedure after enrolling in the study, as a diagnosis of new lesions, or the option to perform the two-step surgery were excluded in the analysis.
All patients were athletes, with most mechanisms of injury being indirect knee trauma. During the physical examination, the cruciate ligaments were tested, as was the posterolateral corner. ACL competence was assessed using the Lachman, anterior drawer and pivot shift maneuvers. The PCL was examined through the posterior drawer and Godfrey maneuvers. Finally the integrity of the LCL and lateral structures were assessed through the varus stress tests in extension and 30° of knee flexion, recurvatum test - external rotation and dial test in 30° and 60° degrees.11
The clinical evaluations were complemented with bilateral knee radiographs with standing anteroposterior (AP) and profile (P) views, varus-stress radiographs at 20° knee flexion and Magnetic Resonance (MRI) of the knee.15 The opening of the lateral compartment was measured and compared between groups according to the stress radiography protocol described by LaPrade et al.10 and ligament injuries were confirmed on MRI. Varus stress radiographs were obtained with the patient in supine position, knee flexed at 20° under maximum varus load applied by the physician. Lateral joint opening was measured by a vertical line drawn from the lower aspect of the lateral femoral condyle to the corresponding point on the lateral tibial plateau. This distance is compared with the value measured on the non-injured knee.
The patients included in the study were treated by the same surgeon (LA) with surgical repair occurring between 4 and 6 weeks after injury. Patients were divided into two groups according to the characteristics of the lesions identified through physical examination, radiographs, MRI, and confirmed during surgical procedure. Group 1: underwent LCL reconstruction and ACL reconstruction (n = 15); Group 2: underwent LCL reconstruction and PCL reconstruction (n = 15).
2.1. Surgical technique
The anterior and posterior cruciate ligaments were reconstructed using quadriceps tendon autograft, with femoral and tibial fixation with interference screws. The anatomical landmarks were noted and tibial fixation occurred after LCL reconstruction. The technique used to reconstruct LCL followed the principles described by Fanelli and Larson16; however, the anatomical bone references described by LaPrade and al.17 were used for the femoral and tibial tunnels. The gracilis and semitendinosus tendons autograft were used to reconstruct the LCL. (Fig. 1).
Fig. 1.
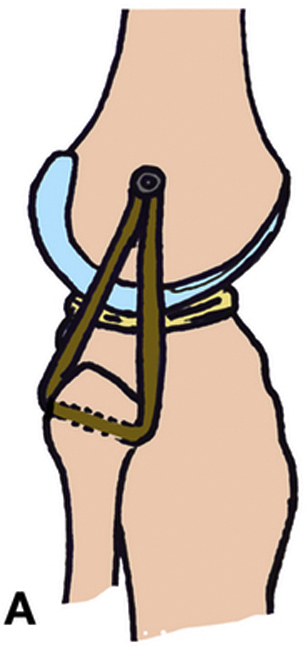
Diagram of the LCL reconstruction. This method used the basic principles described by Fanelli and Larsson, and the anatomical landmarks described by LaPrade for the femoral and fibular tunnel.
The patients were evaluated clinically after 7, 14 and 30 postoperative days. After this period, the patients were seen monthly for 9 months, and every six months thereafter. The Lysholm score18 was recorded before surgery and after 6, 12, and 24 months following surgery. The degree of lateral joint opening during varus stress radiography was evaluated at 12 and 24 months postoperatively of the surgical procedure.
2.2. Statistical analysis
The Kruskal-Wallis test was used to evaluate the evolution of the values obtained in the Lysholm scores and the lateral opening of the stress radiography for each of the groups. The Mann-Whitney test was used to compare Lysholm's preoperative and postoperative scores and the opening values on knee varus stress X-ray between groups. The significance level of 5% (p < 0.05) and power of 80% were adopted for the sample evaluated. Both intra and intergroup statistics were calculated and compared. .
3. Results
The mean age of the patients evaluated was 30.1 years (min-18, max-52, SD: 9.3 years) (Table 1). 88.23% of the patients were male (p < 0.001).
Table 1.
Distribution of age by group.a
| Group | n | Average | Mean | Min | Max | SD | P-value |
|---|---|---|---|---|---|---|---|
| ACL + LCL | 9 | 29.9 | 27 | 18 | 44 | 9.4 | 0.06 |
| PCL + LCL | 8 | 31.3 | 33 | 28 | 52 | 7.4 | |
| Total | 17 | 30.1 | 27 | 18 | 52 | 9.3 |
Values are presented as n (number of patients). SD: standard deviation, ACL, anterior cruciate ligament; LCL, lateral collateral ligament; PCL, posterior cruciate ligament.
There was no difference between the groups in the evaluation of the Lysholm score at any preoperative evaluation (before and after 6, 12, and 24 months) (p > 0.05). (Table 2). However, for both groups, the scores were increasing and significant over the periods before surgery and after 6 months, and between 6 and 12 months (p < 0.05). There was no difference when comparing the increase in scores between 12 and 24 months for group 1 or group 2 individually (p > 0.05). (Table 3).
Table 2.
Evaluation of the Lysholm score before and after 6, 12 and 24 postoperativelya.
| Time | Group | n | Average | Mean | SD | P-value |
|---|---|---|---|---|---|---|
| Pre-op | 1 | 9 | 43.1 | 43 | 1.8 | 0.11 |
| 2 | 8 | 44.3 | 43 | 2.9 | ||
| 6 mo | 1 | 9 | 52.1 | 51 | 1.5 | 0.14 |
| 2 | 8 | 50.7 | 51 | 1.8 | ||
| 12 mo | 1 | 9 | 77.8 | 80 | 4.4 | 0.13 |
| 2 | 8 | 73.8 | 70 | 5.2 | ||
| 24 mo | 1 | 9 | 78.9 | 80 | 3.3 | 0.11 |
| 2 | 8 | 76.3 | 80 | 5.2 |
Values are presented as n (number of patients); pre-op, pre-operative. SD: Standard deviation; mo, months.
Table 3.
Evaluation of the lateral joint opening during valgus stress radiograph before surgery and after 12 and 24 postoperatively.a
| Time | Group | n | Average | Mean | Min | Max | SD | P-value |
|---|---|---|---|---|---|---|---|---|
| Pre-op | 1 | 9 | 5.3 | 4.5 | 4.4 | 9.8 | 2.1 | 0.04 |
| 2 | 8 | 6.5 | 6.7 | 5.2 | 9.8 | 1.5 | ||
| 12 mo | 1 | 9 | 1.5 | 1.5 | 0.9 | 2.6 | 0.6 | 0.15 |
| 2 | 8 | 1.1 | 1.1 | 1.3 | 2.3 | 0.4 | ||
| 24 mo | 1 | 9 | 1.5 | 1.5 | 0.9 | 2.9 | 0.6 | 0.14 |
| 2 | 8 | 1.3 | 1 | 1.3 | 2.3 | 0.5 |
Bold indicates the values <0.05 are statistically significant results.
Values are reported in millimeters. SD: Standard deviation; mo, months.
Group 2 patients had greater lateral joint opening than group 1 before surgery (p = 0.04). In the postoperative moments there was no difference between the groups (p > 0.05) (Table 3). The lateral joint opening decreased in each of the groups when comparing the values before surgery, and after 12 and 24 months (p < 0.05). However, the degree of lateral joint opening between 12 and 24 months showed no difference in either group (p > 0.05) (Table 2, Table 3).
4. Discussion
The results of the present study support the hypothesis that reconstruction of both damaged ligaments in combined LCL and cruciate ligament injuries provide adequate functional and radiographic outcomes. LCL injury associated with cruciate ligament rupture has a distinct mechanism of injury and degree of energy, which may corroborate the patient's severity of symptoms and recovery capacity of patients who sustain these injuries.19 However, if the lesions were adequately treated with reconstruction, knee function was similar at 6 months postoperatively and remained good throughout the follow up period. This result provides support that reconstruction of both ligaments is an efficacious treatment for combined LCL and cruciate ligament injuries.
The Lysholm functional scores reported 2 years after surgery similar for both the ACL and PCL groups, with no statistical difference between them (p > 0.05 in all evaluated periods). On average, it increased from an average of 43.1 and 44.3 points, for groups 1 and 2 respectively, before the injury to 78.9 for group 1, and 76.3 for group 2 at two years follow up. Fanelli et al. evaluated the results after ACL reconstruction associated with the lateral compartment injury, showing that the mean Lysholm score improved significantly from 49 to 84 points after 2 and 10 years of surgery.20 Moulton et al. evaluated the anatomic reconstruction of LCL with concomitant ACL reconstruction and found significant improvement in subjective scores, indicating that the function and activity levels of these patients improved after the anatomical reconstruction of both ligaments.16 There is a lack of PCL/LCL reconstruction data in the literature. Therefore, even though PCL reconstruction considered a more complex surgery, surgical reconstruction of the LCL and PCL produced similar outcomes related to knee function and stability to those of combined LCL and ACL reconstruction, as shown by the present study.
When assessing the evolution of the scores for individual groups, there was a significant increase in the score for both group 1 and 2 seen at 6 months and 12 months, demonstrating the clinical improvement of the patient during the follow-up for corroborating with the data in the literature. Furthermore this score improvement was maintained through the end of the 2 year follow-up period, indicating that the surgery restored patients’ functional outcome. The same trend occurred for the lateral joint opening, indicating that the surgical treatment restored and maintained lateral stabilization.
Interestingly, the degree of lateral opening assessed preopertively showed a significant difference between the groups: the group with associated PCL injury had a mean of 6.5 mm of opening, versus 5.3 mm in the group with associated ACL injury (p = 0.04). LaPrade et al. reported that isolated LCL lesions increase the lateral joint space opening to varus stress by approximately 2.7 mm; a combined lesion of the ACL and LCL results in an opening of 5.3 mm when compared to the non-injured side.21 The results of the present study show that in the presence of PCL injury, this value is even higher, which could have important diagnostic ramifications. The dual LCL – cruciate reconstruction restored stability to the knee joint, as shown by the decreased lateral joint opening after surgery and lack of difference between the groups after 12 and 24 months postoperatively. Furthermore, the stability was maintained at 24 months postoperatively (p > 0.05).
Buzzi et al. evaluated the degree of lateral articular opening with Telos device in 13 cases of LCL reconstruction with ACL reconstruction (n = 6) or PCL reconstruction (n = 7), with mean follow-up of 60 months. In the LCL + ACL group there was a mean lateral joint opening of 7.16 mm versus 8.28 mm in the group associating the LCL + PCL group, corroborating our findings. In the postoperative evaluations, the stability was restored and maintained with an average lateral joint opening of 1.83 mm for the ACL group and 2.00 mm for the PCL group.22
The authors address some limiting factors of the study. First, there is no consensus in the literature on the best time to perform ligament reconstruction, and whether it should be performed in a one- or two-step operation. Even so, homogeneity of the patient population was maintained, and all patients were operated on at a single time, after the same, predefined post-injury timeframe. Second, the number of patients in each group was small, and future studies should strive to support the findings presented here with larger sample populations. However, the results remain valid despite the rarity of the injury pattern and difficulty of homogenizing the study population.
Function and stability were corrected by dual LCL and cruciate ligament reconstruction in the studied population. Patients diagnosed with combined LCL and PCL injuries were shown to have a higher degree of lateral opening at the time of injury when compared to patients with combined LCL and ACL injuries. However, there was no difference in lateral joint opening on stress radiography after 12 months postoperatively in either group. Finally Lysholm scores for both groups significantly increased between the preoperative period and 6 months postoperatively, as well as between 6 months and 12 months postoperatively. There was no significant difference between the groups at any examined timepoint (p < 0.05). This evidence supports the efficacy of reconstruction of the LCL in the setting of a cruciate ligament injury, with similar clinical results.
Conflicts of interest
There is no conflict of interest or potential disclosures for all authors.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jor.2019.05.010.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Gollehon D.L., Torzilli P.A., Warren R.F. The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. J Bone Joint Surg Am. 1987;69(2):233–242. [PubMed] [Google Scholar]
- 2.Bohm K.C., Sikka R.S., Boyd J.L., Yonke B., Tompkins M. An anatomic-based tunnel in the fibular head for posterolateral corner reconstruction using magnetic resonance imaging, part 1. Knee Surg Sport Traumatol Arthrosc. 2015;23(7):1889–1894. doi: 10.1007/s00167-014-3085-3. [DOI] [PubMed] [Google Scholar]
- 3.Bradley J., Honkamp N.J., Jost P., West R., Norwig J., Kaplan Incidence and variance of knee injuries in elite college football players. Am J Orthoped. 2008;37:310–314. [PubMed] [Google Scholar]
- 4.Bushnell B.D., Bitting S.S., Crain J.M., Boublik M., Schlegel T.F. Treatment of magnetic resonance imaging-documented isolated grade III lateral collateral ligament injuries in National Football League athletes. Am J Sports Med. 2010;38(1):86–91. doi: 10.1177/0363546509344075. [DOI] [PubMed] [Google Scholar]
- 5.DeLee J.C., Riley J.B., Rockwood C.A. Acute straight lateral instability of the knee. Am J Sports Med. 1983;11:404–411. doi: 10.1177/036354658301100605. 1983. [DOI] [PubMed] [Google Scholar]
- 6.Coobs B.R., LaPrade R.F., Griffith C.J., Nelson B.J. Biomechanical analysis of an isolated fibular (lateral) collateral ligament reconstruction using an autogenous semitendinosus graft. Am J Sports Med. 2007;35:1521–1527. doi: 10.1177/0363546507302217. [DOI] [PubMed] [Google Scholar]
- 7.Hughston J.C., Andrews J.R., Cross M.J., Moschi A. Classification of knee ligament instabilities: Part II. The lateral compartment. J Bone Joint Surg Am. 1976;58(2):173–179. [PubMed] [Google Scholar]
- 8.LaPrade R.F., Wentorf F. Diagnosis and treatment of posterolateral knee injuries. Clin Orthop Relat Res. 2002;402:110–121. doi: 10.1097/00003086-200209000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Strand T., Molster A.O., Engesater L.B., Raugstad T.S., Alho A. Primary repair in posterior cruciate ligament injuries. Acta Orthop Scand. 1984;55:545–547. doi: 10.3109/17453678408992956. [DOI] [PubMed] [Google Scholar]
- 10.LaPrade R.F., Heikes C., Bakker A.J., Jakobsen R.B. The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and grade-III posterolateral knee injuries. An in vitro biomechanical study. J Bone Joint Surg Am. 2008;90(10):2069–2076. doi: 10.2106/JBJS.G.00979. [DOI] [PubMed] [Google Scholar]
- 11.Wilson W.T., Deakin A.H., Payne A.P., Picard F., Wearing S.C. Comparative analysis of the structural properties of the collateral ligaments of the human knee. J Orthop Sport Phys Ther. 2012;42(4):345–351. doi: 10.2519/jospt.2012.3919. [DOI] [PubMed] [Google Scholar]
- 12.Grana W.A., Janssen T. Lateral ligament injury of the knee. Orthopedics. 1987;10:1039–1044. doi: 10.3928/0147-7447-19870701-08. [DOI] [PubMed] [Google Scholar]
- 13.Krukhaug Y., Molster A., Rodt A., Strand T. Lateral ligament injuries of the knee. Knee Surg Sport Traumatol Arthrosc. 1998;6(1):21–25. doi: 10.1007/s001670050067. [DOI] [PubMed] [Google Scholar]
- 14.Stevenson W.W., III, Johnson D.L. Management of acute lateral side ligament injuries of the knee. Orthopedics. 2006;29(12):1089–1093. doi: 10.3928/01477447-20061201-11. [DOI] [PubMed] [Google Scholar]
- 15.Devitt B.M., Whelan D.B. Physical examination and imaging of the lateral collateral ligament and posterolateral corner of the knee. Sports Med Arthrosc. 2015;23(1):10–16. doi: 10.1097/JSA.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 16.Moulton S.G., Matheny L.M., James E.W., LaPrade R.F. Outcomes following anatomic fibular (lateral) collateral ligament reconstruction. Knee Surg Sport Traumatol Arthrosc. 2015;23:2960. doi: 10.1007/s00167-015-3634-4. [DOI] [PubMed] [Google Scholar]
- 17.Serra Cruz R., Mitchell J.J., Dean C.S., Chahla J., Moatshe G., LaPrade R.F. Anatomic posterolateral corner reconstruction. Arthrosc Tech. 2016;5(3):e563–e572. doi: 10.1016/j.eats.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lysholm J., Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150–154. doi: 10.1177/036354658201000306. [DOI] [PubMed] [Google Scholar]
- 19.Noyes F.R., Barber-Westin S.D. Surgical restoration to treat chronic deficiency of the posterolateral complex and cruciate ligaments of the knee joint. Am J Sports Med. 1996;24:415–426. doi: 10.1177/036354659602400404. [DOI] [PubMed] [Google Scholar]
- 20.Fanelli G.C., Edson C.J., Maish D.R. Combined anterior and posterior cruciate ligament injuries. Techniques in orthopaedics. Arthroscopy. 2002;18(7):703–714. doi: 10.1053/jars.2002.35142. [DOI] [PubMed] [Google Scholar]
- 21.LaPrade R.F., Spiridonov S.I., Coobs B.R., Ruckert P.R., Griffith C.J. Fibular collateral ligament anatomical reconstructions: a prospective outcomes study. Am J Sports Med. 2010;38(10):2005–2011. doi: 10.1177/0363546510370200. [DOI] [PubMed] [Google Scholar]
- 22.Buzzi R., Aglietti P., Vena L.M., Giron F. Lateral collateral ligament reconstruction using a semitendinosus graft. Knee Surg Sport Traumatol Arthrosc. 2004;12(1):36–42. doi: 10.1007/s00167-003-0456-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


