Abstract
OBJECTIVES:
Caregivers frequently make mistakes when following instructions on discharge medications, and these instructions often contain discrepancies. Minimal literature reflects inpatient discharges. Our objective was to describe failures in caregiver management and understanding of inpatient discharge medications and to test the association of documentation discrepancies and sociodemographic factors with medication-related failures after an inpatient hospitalization.
METHODS:
This study took place in an urban tertiary care children’s hospital that serves a low-income, minority population. English-speaking caregivers of children discharged on an oral prescription medication were surveyed about discharge medication knowledge 48 to 96 hours after discharge. The primary outcome was the proportion of caregivers who failed questions on a 10-item questionnaire (analyzed as individual question responses and as a composite outcome of any discharge medication–related failure). Bivariate tests were used to compare documentation errors, complex dosing, and sociodemographic factors to having any discharge medication-related failure.
RESULTS:
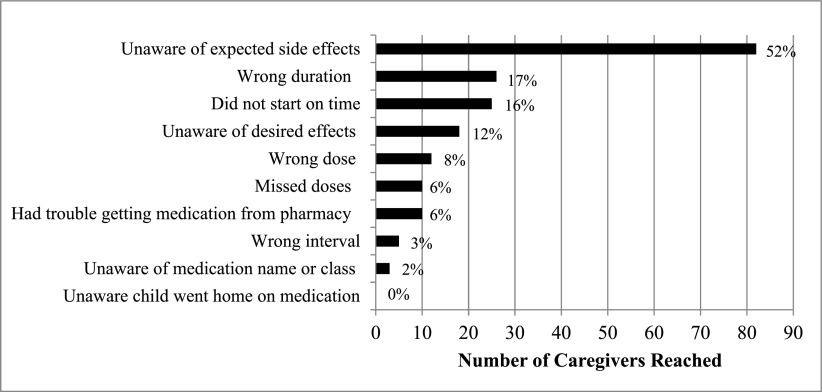
Of 157 caregivers surveyed, 70% had a discharge medication–related failure, most commonly because of lack of knowledge about side effects (52%), wrong duration (17%), and wrong start time (16%). Additionally, 80% of discharge instructions provided to caregivers lacked integral medication information, such as duration or when the next dose after discharge was due. Twenty five percent of prescriptions contained numerically complex doses. In bivariate testing, only race and/or ethnicity was significantly associated with having any failure (P = .03).
CONCLUSIONS:
The majority of caregivers had a medication-related failure after discharge, and most discharge instructions lacked key medication information. Future work to optimize the discharge process to support caregiver management and understanding of medications is needed.
Transition of care after pediatric hospitalization is complex and lacks quality standards.1,2 Discharge-related care failures occur in up to one-third of pediatric discharges, and pediatric adverse drug events are common in the outpatient setting.3,4 However, the discharge medication process remains an understudied area of research for children who are hospitalized.5 The aim of a 2018 Joint Commission national patient safety goal was to use medications safely by communicating “correct information about a patient’s medicines” and providing “written information on the medications…when discharged from the hospital.”6 Thus, confirming appropriate medication execution, adherence, and understanding by the patient’s caregiver and accuracy of discharge medication documentation are critical to ensuring a safe discharge.7
As the responsibility for medication administration shifts from hospital provider to home caregiver, children are vulnerable to failures in medication management and understanding. Studies from emergency departments (EDs) reveal that caregivers have difficulty managing all discharge instructions, especially those related to medications.5 Caregivers of children discharged from the ED frequently cannot recall medication name,8–11 frequency,8,9,11,12 duration,9,11,12 indications,8,12 and side effects.9 Additionally, up to 38% report medication nonadherence.5,8 More than 40% of caregivers make a mistake when dosing their child’s liquid medication, especially when health literacy rates are low.8,13,14 Furthermore, medication dose volumes are often rounded to several decimal places in electronic prescribing systems, making them difficult to understand and accurately administer and leaving children at risk for dosing errors.15,16 Because the majority of this work is focused on ED rather than inpatient discharge, the unique challenges related to caregiver medication management and understanding after pediatric hospital discharge remain understudied.5,8–13
In addition, medication documentation discrepancies at care transitions are common, disadvantaging caregivers in correctly conducting discharge tasks. Studies reveal that discrepancies in discharge documentation are found in 19% to 26% of pediatric charts, with medication duration being frequently omitted.17,18 A separate study with similar results revealed that one-third of unintentional discrepancies at the time of hospital admission had potential to cause adverse events.19 It is unknown if incomplete written discharge instructions are linked with worse caregiver medication management and understanding in an urban minority population with low health literacy.
Quantifying the frequency of discharge medication–related failures and identifying why caregivers mismanage and misunderstand medication instructions after inpatient hospitalization are a critical first step in designing future interventions to improve care transitions. It is also important to evaluate the quality of written discharge instructions in relation to medication management. Therefore, our primary objective was to describe the proportion of failures in caregiver management and understanding of inpatient discharge medications. We then tested the association of documentation discrepancies and sociodemographic factors with any medication-related failure. These data were used as a baseline for a subsequent improvement project.
Methods
Design and Setting
This study took place in an urban tertiary care academic children’s hospital. The hospital serves a low-income and primarily African American and Hispanic population, with one-third of adults not completing high school and therefore at high risk for low health literacy.20,21 It was conducted on the hospital medicine services of 2 general inpatient units (36 beds each) from January 2017 to March 2017. One to 3 service teams per unit care for general medical patients (<13 years old) and complex care and surgical patients (≤21 years old). Each team is an attending-led teaching service, run by house staff (physician assistants, residents, and interns). At discharge, house staff complete a discharge summary and an after-visit summary (AVS). The discharge summary sent to the patient’s general pediatrician includes hospital course, follow-up, and discharge medication information. The AVS provided to caregivers by the bedside nurse contains standardized section headers for anticipatory guidance and follow-up and medication information. The AVS automatically imports information contained in the electronic prescription (name, dose, route, and interval) during mandatory discharge medicine reconciliation. There is an optional dosing calendar completed by the bedside nurse as well as a free-text box for discharging providers to enter additional instructions if desired, although input is neither standardized nor mandatory. Verbal discharge medication counseling is not standardized and may be done by house staff, nursing, or the pharmacy. Four months before this study, a hospital-based outpatient pharmacy opened, dispensing discharge prescriptions on-site and performing bedside prescription delivery and medication counseling.
Subjects
The study subjects included English-speaking caregivers of patients <18 years old discharged from the pediatric inpatient unit on at least 1 new standing-prescription oral medication, including change in dose of a previous medication. Eligible caregivers had to be primarily responsible for managing medication administration after discharge.
Procedure for Identifying Eligible Caregivers
Eligible caregivers were identified via daily electronic medical record review of patients who were discharged. Each week a convenience sample of caregivers chosen via a quasi-randomized approach were called 48 to 96 hours after discharge and surveyed. Patients’ last names were alphabetized, and we started with a randomly chosen letter every week. Calls proceeded alphabetically for eligible caregivers during regular business hours, evening hours, and on weekends as the primary investigator’s (PI) schedule allowed. The number of completed calls per week ranged from 5 to 20 on the basis of the availability of eligible caregivers. For consistency in data collection, all calls, determination of failed responses, and chart review for sociodemographic and medication information were performed by the PI (K.P.).
Measures and Survey Tool
The primary outcome measure was the proportions of caregivers who failed each individual question on a 10-item postdischarge questionnaire administered via phone call (Table 1). We also calculated the overall proportion of discharge medication–related failures, a composite outcome in which ≥1 incorrect response defined a failure.
TABLE 1.
Survey Questions Used to Evaluate for a Discharge Medication–Related Failure
| Question | Category of Failure | Definition of Incorrect Answer |
|---|---|---|
| Did you go home on any medications? | Unaware prescription exists | Unaware child was to continue taking medication after discharge |
| What medication was it? | Unaware of name and/or class | Unaware of or wrong medication name or class |
| Did you have any trouble getting it from the pharmacy? | Pharmacy trouble | Did not pick up medication or delay in obtaining medication |
| When did you start the medication? | Wrong start time | Missed dose between discharge and when next dose was due |
| How much medication are you giving? | Wrong dose | Unaware of dose or reported dose differs by >10% of prescription29 |
| How many times a day are you giving the medication? | Wrong interval | Unaware of interval or reported interval does not match prescription |
| Was there ever a time you had to miss a dose? | Missed doses | Less than 80% reported adherence to dosing regimen30 |
| How long will you give the medication for? | Wrong duration | Unaware of total duration; stopping medication early, leading to <80% adherence30; or unaware that medication is chronic and has no end date |
| What are you watching for to know the medication is working? | Unaware of desired effects | Unaware of child taking medication, never told why child is taking medication, or never told how to know child is improved |
| Are there any side effects of the medication you are looking for? | Unaware of expected side effects | Unaware of or never told about any side effects of medication |
To develop the questionnaire, the research team integrated questions related to medication name, dose, frequency, duration, adherence, desired effects, and expected side effects from previous studies8–14 with questions related to knowledge of new prescriptions and timing of the next dose due after discharge. Lastly, a question for assessing caregiver difficulty in obtaining medications from the pharmacy was asked to analyze adherence behaviors and in preparation for work to improve our institution’s process. We pilot tested the questionnaire with 10 caregivers and modified the language on the basis of feedback.
Specific responses defined in Table 1 were required to determine if the question was correct or incorrect. For example, if the caregiver could not provide the exact name (eg, amoxicillin) or class of medication (eg, antibiotic), the answer to “What medication was it?” was incorrect. If the caregiver did not know why the child was taking the medication or did not know the desired signs that indicated improvement, the question “What are you watching for to know the medication is working?” was incorrect. If the caregiver was not told expected side effects, adjudicated from common resources for medication counseling, or could not list an appropriate one, the answer to “Are there any side effects of the medication you are looking for?” was incorrect.
Secondary measures included the proportion of charts with (1) incomplete medication information on the AVS, (2) discrepant medication information between the discharge summary and AVS, and (3) complex dosing. The AVS was considered incomplete if the information expected to be imported from the electronic prescription and/or completed on the dosing calendar was missing (name, dose, interval, duration, and next dose due). Medication desired effects and expected side effects information was not imported and was rarely included in free text and so was not included in this outcome. The discharge summary and AVS were considered discrepant if the medication name, dose, interval, and duration were not identical. Given the complicated process of pediatric dosing and limits of the electronic prescribing system to round doses appropriately, a dose was complex if rounded to any decimal other than a whole number or 0.5 mL.22 We aimed to quantify how often our electronic prescribing system generated a dose difficult for caregivers to accurately administer, placing children at risk for dosing errors.
Procedure for Administering Survey
Caregivers gave verbal consent before the survey proceeded. If the patient was discharged on >1 medication, questions were asked of the first eligible medication listed by the caregiver. Question responses were compared to medication information in the chart at the time of the call and deemed either correct/passed or incorrect/failed (Table 1). If the response was unclear, we attempted to clarify. For example, if the duration question response was “a couple more days,” we asked for a specific number. If the response was incorrect, we determined the danger of the response and either educated, referred the caregiver to his or her pediatrician, or provided the inpatient unit’s phone number to rectify discrepancies.
Procedure for Collection of Secondary Outcomes and Independent Variables
After the survey, the PI reviewed the chart to collect secondary outcome and independent variable data, including use of a hospital-based pharmacy, number and class of eligible medications, and discharge date. The PI also queried the institution’s medical database, Looking Glass Clinical Analytics (Streamline Health, Atlanta, GA), to collect length of stay, All Patient Refined Diagnosis Related Groups hospital code, and sociodemographic data (age, sex, race, ethnicity, and socioeconomic status [SES]).
Statistical Analysis
We describe the proportions of (1) failed question responses, (2) discharge medication–related failures, (3) incomplete AVS medication information, (4) discrepant medication information between the discharge summary and AVS, and (5) complex dosing. Regarding the primary outcome, if correct responses could not be verified because of lack of chart documentation or because caregiver responses revealed they had the information elsewhere (eg, printed on prescription), that question was excluded from the composite outcome results. As baseline data for an improvement project, this approach biases results toward the null hypothesis that there is no difference between the preintervention and postintervention periods. We also performed sensitivity analyses, and we either (1) considered unverifiable data as a failure or (2) excluded those caregivers with unverifiable data from the analysis. Given comparable sensitivity analyses results, caregivers with and without a discharge medication–related failure by using the primary analysis structure were compared on independent variables and secondary outcomes by using the Wilcoxon rank test for continuous variables and the χ2 test or Fisher’s exact test for categorical variables. We also tested the relationship between a missing medication category on the AVS and failure on the associated survey question. All analyses were performed by using Stata 14.0 (StataCorp, College Station, TX). This study was approved by the Institutional Review Board at the Albert Einstein College of Medicine.
Results
Analysis of Discharge Medication–Related Failures and Discharge Documentation
A total of 245 caregivers were called, and 157 were included in the final analysis (64% response rate). Of those not included, 80% did not answer, 7% requested a call back and were not subsequently reached, 5% were not interested in participating, and 8% were not able to complete the survey. The median patient age was 3 years (interquartile range: 1.6–6 years).
A total of 110 (70%) caregivers had a discharge medication–related failure (categorized in Fig 1). Of included caregivers, the most commonly failed question related to lack of awareness of expected side effects (52%), which was followed by wrong duration (17%), wrong start time (16%), and lack of awareness of desired effects (12%). In sensitivity analyses of unverifiable data (n = 17 caregivers), the failure rate was 81% if all unverified data were considered a failure and 77% if data were excluded. If “Are there any side effects of the medication you are looking for?” was eliminated from the primary analysis, the failure rate decreased to 46%.
FIGURE 1.
Categories of failures (n = 157). Percentages do not total 100% because caregivers may have >1 failure.
Eighty percent of AVSs lacked key medication information, most commonly duration (41%) and/or when the next dose was due after discharge (74%) (Table 2). There was no statistically significant association between missing duration or next dose due documentation and failing the associated survey question.
TABLE 2.
Descriptive Statistics for Secondary Outcomes
| n (%) | Totala | |
|---|---|---|
| AVS with missing information | 124 (80) | 155 |
| Discrepant medication information between discharge summary and AVS | 8 (5) | 152 |
| Prescriptions with complex medication dosing | 39 (25) | 157 |
Each secondary outcome has a different total because of 2 charts missing an AVS and 5 charts missing a discharge summary or AVS, making adjudication of these outcomes impossible.
Association Between Independent Variables, Secondary Outcomes, and Discharge Medication–Related Failures
In Table 3, we compare the sociodemographics, clinical variables, and secondary outcomes of caregivers with and without a discharge medication–related failure. There was a statistically significant association for race and/or ethnicity (P = .03). Hispanic and non-Hispanic African American caregivers had the highest failure rates (37% and 39%, respectively). Of 110 caregivers with a discharge medication–related failure, 39% were non-Hispanic African American and 12% were non-Hispanic other race. For those without a failure, 23.4% were non-Hispanic African American and 29.8% were non-Hispanic other race (Table 3). There was no statistically significant association between secondary outcomes and a discharge medication–related failure.
TABLE 3.
Comparison of Sociodemographics, Clinical Variables, and Secondary Outcomes for Caregivers With a Discharge Medication–Related Failure
| Failure (n = 110) | No Failure (n = 47) | P | |
|---|---|---|---|
| Independent variables | |||
| Age, y, median (IQR) | 3 (1.8 to 5.0) | 3 (1.2 to 7.0) | .93 |
| SES z score, median (IQR)a | −3.5 (−7.0 to −1.6) | −3.0 (−5.8 to −1.0) | .26 |
| LOS, d, median (IQR) | 1.9 (1.2 to 3.1) | 2.3 (1.7 to 3.2) | .06 |
| Sex of child, female, n (%) | 50 (46) | 26 (55) | .26 |
| Race and/or ethnicity, n (%) | .03 | ||
| Hispanic | 41 (37) | 16 (34) | |
| Non-Hispanic African American | 43 (39) | 11 (23) | |
| Non-Hispanic other race | 13 (12) | 14 (30) | |
| Unavailable | 13 (12) | 6 (13) | |
| Used hospital’s outpatient pharmacy, n (%) | 60 (55) | 28 (60) | .56 |
| No. eligible medications, n (%)b | .28 | ||
| 1 | 80 (73) | 38 (81) | |
| 2 | 23 (21) | 5 (11) | |
| ≥3 | 7 (6) | 4 (8) | |
| Class of medication, n (%)b | .79 | ||
| Steroid | 37 (34) | 13 (28) | |
| Antibiotic or antifungal | 44 (40) | 23 (49) | |
| Antiviral | 17 (15) | 6 (13) | |
| Other | 12 (11) | 5 (10) | |
| APR-DRG of hospitalization, n (%)b | .47 | ||
| Asthma | 34 (31) | 11 (23) | |
| Respiratory tract infection | 38 (35) | 13 (28) | |
| Gastrointestinal problem | 7 (6) | 3 (6) | |
| Genitourinary problem | 3 (3) | 4 (9) | |
| Skin and soft-tissue infection | 6 (5) | 3 (6) | |
| Other | 22 (20) | 13 (28) | |
| Weekend discharge, n (%) | 41 (37) | 14 (30) | .37 |
| Secondary outcomes, n (%) | |||
| AVS missing information | 88 (82) | 36 (77) | .49 |
| Discrepant chartb | 3 (3) | 5 (11) | .06 |
| Complex dosing | 24 (22) | 15 (32) | .18 |
Total sample size: SES: 106 failures and 45 no failure; discrepant chart: 106 failures and 46 no failure; AVS missing information: 108 failures and 47 no failure. APR-DRG, All Patient Refined Diagnosis Related Group; IQR, interquartile range; LOS, length of stay; —, not applicable.
SES was reported as a z score calculated from small census tract data based on the patient’s home address; it reveals the deviation from the mean of the New York State population.31
Fisher’s exact test was used.
Discussion
To our knowledge, this is the first study in which failures in medication management, understanding, and documentation are integrated to describe specific reasons for caregiver medication challenges after pediatric hospital discharge. By analyzing caregiver management and understanding of discharge medications as well as associated medication documentation, we found that an overwhelming majority of caregivers had a discharge medication–related failure and that most documentation lacked key medication information.
Our discharge medication–related failure rate of 70% after inpatient discharge is similar to previously reported rates of caregiver medication administration knowledge after ED discharge. Grover et al10 found that only 38% of caregivers recalled the correct medication dose, frequency, and duration after ED discharge. Our results further reveal domains in which caregivers lack knowledge and report nonadherence after inpatient hospitalization, including when the next dose after discharge is due and medication desired effects and expected side effects. In a study in which the effectiveness of standardized ED discharge teaching was evaluated, Isaacman et al11 determined that accurate parental recall of medication data (name, dose, frequency, and duration) can be improved to >90% with a standardized discharge medication education process. Future studies to evaluate a thorough and standardized discharge medication process in the inpatient unit are warranted.
We found that more than half of caregivers were unaware of expected medication side effects. Knowledge of side effects is not well studied in pediatrics but is highlighted by the Agency for Healthcare Research and Quality as important for discharge planning.5,23 A pediatric ED study in the Kingdom of Saudi Arabia revealed that 47% of subjects recognized possible medication side effects.9 Our study revealed a similar frequency but expands these findings to an American and primarily minority population, filling an understudied research gap in the pediatric literature. Adult patients who recalled having side effects explained were significantly less likely to experience an adverse drug event.24 More research is necessary to elucidate the importance of side-effect counseling during pediatric care transitions.
Additionally, 80% of documentation provided to caregivers lacked important medication information, most often related to duration and when the next dose was due after discharge. An even higher percent lacked key information related to medication desired effects and side effects. Although caregivers frequently lacked knowledge in similar domains, there was no significant association between missing written information and failing the associated survey question. Medication discrepancies between various forms of documentation are common after pediatric discharge,17,18 although our study is 1 of the first to specifically describe the prevalence of medication domains frequently omitted from discharge instructions. This may be due to problems with physician prescription writing (by using free text), transfer of prescriptions to the pharmacy electronically, and/or automatic population of the prescription into the written AVS. Similarly, we report a 25% prevalence of unrounded, difficult-to-administer dosing volumes for pediatric discharge prescriptions, which has only previously been reported in inpatient order entry.16 This finding is critical to future studies for improving electronic prescribing system pediatric dose rounding. Both discharge preparation and medication counseling are dynamic processes that involve multiple individuals and various modalities of education. More research is necessary for evaluating the role of written instructions and complex dosing as part of the entire process to enhance caregiver medication management and understanding.
In our study, a statistically significant association exists by race and/or ethnicity, with Hispanics and Non-Hispanic African Americans having the highest failure rate. Previous studies have revealed similar race-related disparities in areas such as worse asthma control, poorer diabetes management, and increased likelihood of readmission for non-Hispanic African American children, all possibly due to medication understanding.25–27 Minority race and/or ethnicity is a risk factor for caregiver discharge management errors and may be linked to low health literacy.5 In our study of inpatient discharge-medication failures, this finding may be related to low health literacy, cultural differences, or disparities in SES or education. More research is needed to better understand these disparities and identify solutions for improvement.21
Our study is limited by our outcome, which was based on caregiver self-report and recall. Although we confirmed the accuracy of reported medication information by comparing it to the chart, we could not confirm if caregivers were accurately executing instructions. Similarly, we did not direct caregivers on use of written instructions during the survey, so some may have referenced written instructions, which mat have introduced bias against caregivers who were not in direct possession of the documents. The questionnaire we developed is not validated in the literature because this is an understudied area of pediatric research, but it was pilot tested with caregivers in our study and modified. Additionally, available resources limited our results to only English-speaking caregivers. Limited English proficiency has been linked to medication errors,28 and it is likely that our failure rate would be higher if caregivers with limited English proficiency were evaluated. Likewise, we did not directly measure health literacy. Although we know our study took place in a population with low health literacy, and we know low health literacy is a risk factor for making medication errors, we cannot make conclusions about our findings in relation to the rates of caregiver health literacy on pediatric inpatient units. Understanding medication challenges in this population is an important direction for future work.
Our results are limited to a young age range because our hospital medicine services tend to care for children <13 years old; therefore, our results cannot be generalized to teenagers who may be involved in administering their own medications or may face different adherence challenges. Additionally, this study was not powered to detect differences in some of the independent variables we measured; thus, a type II error is possible. Finally, this is a study at a single institution in a primarily underserved minority population, and our findings may not represent the population at other institutions.
Conclusions
Our study provides important insight to caregiver medication challenges after inpatient hospitalization. More than two-thirds of caregivers mismanage and misunderstand discharge medications, particularly related to medication side effects, duration, and start time after hospital discharge. This finding, combined with poor medication documentation at the time of discharge, may place children at risk for medication errors. Future work to optimize the discharge process to support caregiver management and understanding of medications is needed.
Footnotes
Dr Philips conceptualized and designed the study, designed the survey tool, collected data, conducted analyses, drafted the initial manuscript, and reviewed and revised the manuscript; Dr Zhou helped design the study and survey tool, drafted the initial manuscript, and reviewed and revised the manuscript; Dr Rinke conceptualized and designed the study, supervised data collection and analyses, and critically reviewed and revised the manuscript; Drs Lee, Marrese, Nazif, Browne, and Sinnett, Mr Tuckman, Ms Griffith, Ms Kiely, Ms Lutz, and Ms Modi helped design the study and survey tool and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the National Institutes of Health, National Center for Advancing Translational Sciences through Einstein-Montefiore Clinical and Translational Science Awards (grants TL1TR001072 and UL1TR001073). The contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Auger KA, Simon TD, Cooperberg D, et al. Summary of STARNet: Seamless Transitions and (Re)admissions Network. Pediatrics. 2015;135(1):164–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berry JG, Blaine K, Rogers J, et al. A framework of pediatric hospital discharge care informed by legislation, research, and practice. JAMA Pediatr. 2014;168(10):955–962; quiz 965–966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu S, Tyler A, Logsdon T, et al. A quality improvement collaborative to improve the discharge process for hospitalized children. Pediatrics. 2016;138(2):e20143604. [DOI] [PubMed] [Google Scholar]
- 4.Bourgeois FT, Mandl KD, Valim C, Shannon MW. Pediatric adverse drug events in the outpatient setting: an 11-year national analysis. Pediatrics. 2009;124(4). Available at: www.pediatrics.org/cgi/content/full/124/4/e744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Glick AF, Farkas JS, Nicholson J, et al. Parental management of discharge instructions: a systematic review. Pediatrics. 2017;140(2):e20164165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Joint Commission. National patient safety goals effective January 2018. Available at: https://www.jointcommission.org/assets/1/6/NPSG_Chapter_HAP_Jan2018.pdf. Accessed July 18, 2018
- 7.Cua YM, Kripalani S. Medication use in the transition from hospital to home. Ann Acad Med Singapore. 2008;37(2):136–141 [PMC free article] [PubMed] [Google Scholar]
- 8.Yin HS, Dreyer BP, van Schaick L, Foltin GL, Dinglas C, Mendelsohn AL. Randomized controlled trial of a pictogram-based intervention to reduce liquid medication dosing errors and improve adherence among caregivers of young children. Arch Pediatr Adolesc Med. 2008;162(9):814–822 [DOI] [PubMed] [Google Scholar]
- 9.Al-Harthy N, Sudersanadas KM, Al-Mutairi M, et al. Efficacy of patient discharge instructions: a pointer toward caregiver friendly communication methods from pediatric emergency personnel. J Family Community Med. 2016;23(3):155–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grover G, Berkowitz CD, Lewis RJ. Parental recall after a visit to the emergency department. Clin Pediatr (Phila). 1994;33(4):194–201 [DOI] [PubMed] [Google Scholar]
- 11.Isaacman DJ, Purvis K, Gyuro J, Anderson Y, Smith D. Standardized instructions: do they improve communication of discharge information from the emergency department? Pediatrics. 1992;89(6, pt 2):1204–1208 [PubMed] [Google Scholar]
- 12.Kaestli L, Noble S, Combescure C, et al. Drug information leaflets improve parental knowledge of their child’s treatment at paediatric emergency department discharge. Eur J Hosp Pharm Sci Pract. 2016;23(3):151–155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yin HS, Dreyer BP, Moreira HA, et al. Liquid medication dosing errors in children: role of provider counseling strategies. Acad Pediatr. 2014;14(3):262–270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yin HS, Parker RM, Sanders LM, et al. Liquid medication errors and dosing tools: a randomized controlled experiment. Pediatrics. 2016;138(4):e20160357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morecroft CW, Gill A, Caldwell NA, Wood R, Crolla J, Antwi-Boasiako L. Are prescribed doses of medicine for children measurable? Arch Dis Child. 2012;97(5):e18 [Google Scholar]
- 16.Jones AN, Miller JL, Neely S, et al. Prevalence of unrounded medication doses and associated factors among hospitalized pediatric patients. J Pediatr Pharmacol Ther. 2017;22(4):286–292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gattari TB, Krieger LN, Hu HM, Mychaliska KP. Medication discrepancies at pediatric hospital discharge. Hosp Pediatr. 2015;5(8):439–445 [DOI] [PubMed] [Google Scholar]
- 18.Johnson KB, Butta JK, Donohue PK, Glenn DJ, Holtzman NA. Discharging patients with prescriptions instead of medications: sequelae in a teaching hospital. Pediatrics. 1996;97(4):481–485 [PubMed] [Google Scholar]
- 19.Coffey M, Mack L, Streitenberger K, Bishara T, De Faveri L, Matlow A. Prevalence and clinical significance of medication discrepancies at pediatric hospital admission. Acad Pediatr. 2009;9(5):360–365.e1 [DOI] [PubMed] [Google Scholar]
- 20.US Census Bureau. QuickFacts: Bronx County (Bronx Borough), New York. Available at: https://www.census.gov/quickfacts/fact/map/bronxcountybronxboroughnewyork/EDU635216#viewtop. Accessed July 18, 2018
- 21.Yin HS, Johnson M, Mendelsohn AL, Abrams MA, Sanders LM, Dreyer BP. The health literacy of parents in the United States: a nationally representative study. Pediatrics. 2009;124(suppl 3):S289–S298 [DOI] [PubMed] [Google Scholar]
- 22.Johnson KB, Lee CK, Spooner SA, Davison CL, Helmke JS, Weinberg ST. Automated dose-rounding recommendations for pediatric medications. Pediatrics. 2011;128(2). Available at: www.pediatrics.org/cgi/content/full/128/2/e422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agency for Healthcare Research and Quality. Strategy 4: care transitions from hospital to home: IDEAL discharge planning. Available at: www.ahrq.gov/professionals/systems/hospital/engagingfamilies/strategy4/index.html. Accessed October 2, 2018 [DOI] [PubMed]
- 24.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. Adverse drug events occurring following hospital discharge. J Gen Intern Med. 2005;20(4):317–323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mitchell SJ, Bilderback AL, Okelo SO. Racial disparities in asthma morbidity among pediatric patients seeking asthma specialist care. Acad Pediatr. 2016;16(1):64–67 [DOI] [PubMed] [Google Scholar]
- 26.Auslander WF, Thompson S, Dreitzer D, White NH, Santiago JV. Disparity in glycemic control and adherence between African-American and Caucasian youths with diabetes. Family and community contexts. Diabetes Care. 1997;20(10):1569–1575 [DOI] [PubMed] [Google Scholar]
- 27.Parikh K, Berry J, Hall M, et al. Racial and ethnic differences in pediatric readmissions for common chronic conditions. J Pediatr. 2017;186:158–164.e1 [DOI] [PubMed] [Google Scholar]
- 28.Yin HS, Dreyer BP, Ugboaja DC, et al. Unit of measurement used and parent medication dosing errors. Pediatrics. 2014;134(2). Available at: www.pediatrics.org/cgi/content/full/134/2/e354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rinke ML, Moon M, Clark JS, Mudd S, Miller MR. Prescribing errors in a pediatric emergency department. Pediatr Emerg Care. 2008;24(1):1–8 [DOI] [PubMed] [Google Scholar]
- 30.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497 [DOI] [PubMed] [Google Scholar]
- 31.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99–106 [DOI] [PubMed] [Google Scholar]