Abstract
Objective
To determine if preoperative leg pain and low back pain severity affected postoperative outcome.
Method
Prospectively collected Spine-Tango data was analysed for 995 consecutive patients who underwent a primary, single level, lumbar micro-decompression/microdiscectomy at a single tertiary spinal centre.
Result
At 3 months, 72% of patients were satisfied with the outcome of surgery. Pre-operative low back pain was a significant predictor of poor outcome (P < 0.01).
Conclusion
Our study has shown that patients with a low back pain VAS of 6 or more have a significantly greater chance of a poor outcome following primary lumbar microdecompressive/microdiscectomy surgery.
Keywords: Outcome, Lumbar disc herniation, Back pain, Radicular pain, Micro-discectomy
1. Introduction
Lower-limb nerve root pain caused by a lumbar disc herniation is the most frequent indication for spinal surgery. Sixty-thousand such operations are performed in France each year.1 The US has also witnessed a marked increase (2.1 per 1000 Medicare enrollees) in the rates of lumbar discectomies in the past decade.2 However, the literature reports that one in four patients have a suboptimal outcome following surgery,3 suggesting that pre-operative identification of risk factors associated with a poor outcome is paramount for appropriate case selection.
Surgical success depends on achieving pain relief, which improves quality of life.4 Despite many studies on the predictors of outcome5 the effect of the proportion of pain that is radicular (leg) compared to axial (back), has not been studied extensively. Though a few studies4,6, 7, 8 indicate that greater preoperative low back pain is associated with a poor outcome, none have investigated the extent of this relationship and whether the relative intensity of radicular and axial pain can be used to guide patient selection. The aim of this study is to investigate the influence and possible predictive value of the relative intensity of axial and radicular pain on the outcome of lumbar decompressive surgery.
2. Patients and methods
Consecutive patients who underwent a primary single level lumbar micro-decompression/microdiscectomy performed at a single, tertiary level, spinal centre over period of 3 year were included in this study. Written informed consent for data collection was obtained from all patients. Patients with a clinical and confirmed radiological diagnosis of degenerative lumbar spine disorders producing radicular pain (lumbar disc herniations, degenerative stenosis, degenerative spondylolisthesis) were selected for surgery. Patients who underwent fusion surgery, surgery at more than one level, were excluded. Three hundred patients with incomplete datasets were also excluded.
For each case the operating surgeon completed the Spine Society of Europe (SSE) Spine Tango surgery form, which included the diagnosis, clinical data and details of surgery. The Core Outcome Measures Index (COMI) questionnaire was used to assess outcome. The pain questions in the COMI questionnaire recorded the intensity of Low Back Pain Visual Analogue Scale (LBP VAS) and Leg Pain Visual Analogue Scale (LP VAS) separately on a 0–10 numeric VAS scale, with 0 indicating no pain and 10 indicating the worst imaginable pain. Patients completed a (COMI) questionnaire pre-operatively and at 3 months (postal questionnaire). At follow-up the additional COMI questions included the occurrence and nature of any complications that may have risen following the surgery, any reoperations (at the same or different levels), satisfaction with the result of treatment and finally, the global effectiveness of surgery. The COMI score was calculated using standard means.9
Based on the response to the global outcome question, the patients were dichotomised into two outcome groups - good outcome (response 1 – “helped a lot” and 2 – “operation helped”) and poor outcome (response 3 – “operation helped a little”, 4 – “operation did not help” and 5 – “operation made things worse”).
2.1. Surgical technique
All surgeries were performed through a posterior midline incision. A lumbar decompression in the form of a discectomy, sequestrectomy, hemilaminectomy, facet joint resection (partial), partial laminectomy, foraminotomy, or laminotomy of the lumbar spine was performed under magnification, using an operating microscope.
2.2. Statistical analyses
The statistical package for social sciences (“IBM SPSS Version 22.”) and Microsoft Excel 2013 data analysis tool pack was used to analyse the data. Descriptive pre-operative and post-operative data are calculated as mean and ± standard deviations (SD). Categorical variables are expressed as percentages or frequencies.
Univariate regression analysis was performed to determine the significance of the relationship between variables in the data. A multivariate longitudinal regression analysis was used to predict the 3-month post-op COMI score and multivariate logistic regression analysis was used to predict the 3-month outcome category (good or poor). The independent variables that were significantly associated with the outcome (P < 0.05) in the univariate regression analysis were included. Age, gender and comorbidity were first entered, followed by preoperative LP VAS, LBP VAS and the difference between leg pain and low back pain (LP – LBP VAS) scores as potential predictors, using forward conditional selection.
Receiver operating curves (ROC) were used to determine the threshold (maximum area under curve) for preoperative LBP VAS that could be used to predict poor outcome, and therefore serve as a potential screening tool for patient selection. After determining a cut off value of the LBP VAS, we tested the strength of the cut off value by dividing our patient data into two groups around this cut off value (P < 0.01 considered significant).
Two tailed independent t-test were used to compare the mean difference in possible predictor variables (continuous data) between the good and poor outcome groups, and between LBP VAS more or less than 6. These variables included age, gender, LP VAS, LBP VAS, LP – LBP VAS. A paired t-test was used for comparing pre and post-operative data within each outcome group. Chi-squared test and contingency tables were used to determine if the level of intervention had an association with outcome and also if the predominant reason for undergoing surgery (back pain, leg pain or neurological deficit) had any correlation with outcome. A P value < 0.05 was considered as significant.
3. Results
3.1. Patients
1360 patients were enrolled for the study. After exclusion using the criteria described in the methods, our final data set included 995 patients with complete preoperative and follow up records at 3 months. All had undergone single level primary micro-decompressive surgery by 39 senior orthopaedic/neuro-spinal surgeons at a single tertiary centre. The preoperative demographic details of the study participants is presented in Table 1. Seven hundred and eighteen patients (72%) were satisfied or very satisfied (good outcome) with the outcome of surgery while 277 (28%) reported mild satisfaction, dissatisfaction or worsening of symptoms following surgery (poor outcome). A total of 13 patients (1.3%) underwent another operation within 3 months of the first surgery, 6 (0.6%) at the same level and 7 (0.7%) at another level.
Table 1.
Baseline characteristics of the study participants.
| Total | 995 |
|---|---|
| Mean age | 53.69 years; range 17.5–93.3 |
| Gender | Male 587 (59%) |
| Female 448 (41%) | |
| ASA 1(no disturbance) | 326 (32.8%) |
| ASA 2 (mild/moderate) | 333(33.5%) |
| ASA 3(severe) | 283(28.5) |
| ASA 4 (life threatening) | 46((4.6%) |
| ASA 5 (moribund) | 1 (0.1%) |
| Mean preoperative LBP VAS | 6.10; SD 2.94 |
| Mean preoperative LP VAS | 7.58; SD 2.33 |
| Mean LP – LBP VAS | 1.48; SD 2.97 |
| Mean preoperative COMI score | 7.85; SD 1.68 |
| Main problem | |
| Back pain | 170 (17.09%) |
| Leg pain | 526(52.86%) |
| Sensory disturbance | 289 (28.65%) |
| Other | 10 (1.01%) |
| Smoker | 76 (7.64%) |
| Non-smoker | 385(38.69) |
| Unknown | 574(57.69%) |
| Level of intervention | |
| L1-L2 | 19 (1.91%) |
| L2-L3 | 69 (6.94%) |
| L3-L4 | 336 (33.77%) |
| L4-L5 | 441 (44.32%) |
| L5-S1 | 130 (13.07%) |
3.2. Outcome of surgery
The mean reduction to LP VAS, LBP VAS, and COMI score was significant (3.48, P < 0.01; 1.73, P < 0.01; and 2.78, P < 0.01, respectively). In general, patients had more back pain than radicular pain postoperatively. From the multivariate regression model (Table 2) and the independent t tests (Table 3), preoperative LBP VAS, the difference between LP VAS and LBP VAS (LP – LBP VAS) and preoperative COMI score were the most significant predictors of a good or poor outcome (P < 0.01). LP VAS, age, gender and comorbidity were not significant predictors of outcome.
Table 2.
Result of the final step of the multivariate linear regression analysis in predicting the 3 months post- operative COMI score.
| Independent variables | Unstandardized Coefficients |
Standardized Coefficients |
P value | |
|---|---|---|---|---|
| Beta | Std. Error | Beta | ||
| (Constant) | 1.268 | .575 | 0.028 | |
| Gender | -.111 | .184 | -.018 | 0.547 |
| Preoperative LP VAS | -.070 | .052 | -.054 | 0.175 |
| Preoperative COMI | .369 | .072 | .206 | <0.01 |
| Age | .009 | .006 | .043 | 0.167 |
| ASA score | -.034 | .104 | -.010 | 0.741 |
| Preoperative LBP VAS | .183 | .035 | .178 | <0.01 |
| LP – LBP VAS | .188 | .032 | .181 | <0.01 |
Table 3.
Pre-operative mean differences between the good and poor outcome groups.
| Good outcome | Poor outcome | P – value | |
|---|---|---|---|
| Number of patients | 718 (72.16%) | 277 (27.84%) | |
| Age (range) years | 53.75 (17.5–93) | 53.43 (25–86.2) | 0.76 |
| Gender- male | M 368 (51.2%) | M 139 (50.2%) | |
| Gender- female | F 350 (48.8%) | F 138 (49.8%) | |
| Preoperative COMI score | 7.78 (sd± 1.74) | 8.05 (sd± 1.53) | 0.016 |
| Preoperative LBP VAS | 5.79 (sd± 3.05) | 6.91 (sd ± 2.46) | <0.01 |
| Preoperative LP VAS | 7.49 (sd± 2.38) | 7.82 (sd ± 2.19) | 0.037 |
| Preoperative LP – LBP VAS | 1.7 (sd± 3.12) | 0.91 (sd ± 2.45) | <0.01 |
Post-operatively, compared to the good outcome group, the poor outcome group had a significantly higher mean preoperative LBP VAS {6.79 (sd± 2.29) vs 3.43 (sd±2.92)}, LP VAS {6.58 (sd± 2.95) vs 3.14 (sd±3.26)} and COMI score {7.78(sd± 1.61) vs 4.04 (sd±2.78)}. A smaller mean change in the COMI was observed in the poor outcome group compared to the good outcome group {(0.26 (sd± 1.75) vs 3.74 (sd± 2.94)}. The mean LP VAS and LBP VAS were significantly reduced postoperatively in the good outcome group {LP – mean reduction = 4.34 (sd± 3.76), P < 0.01; LBP – mean reduction = 2.35 (sd ±3.71), P < 0.000}. The poor outcome group showed a small but statistically significant reduction in mean LP VAS (mean reduction = 1.24 (sd ± 3.08), P < 0.01, but not in mean LBP VAS (mean reduction = 0.12 (sd ±2.57) P = 0.220).
3.3. LBP VAS as a predictor of outcome
Patients with a poor outcome had greater pre-operative LBP VAS (intensity of back pain) and a smaller LP – LBP VAS compared to the good outcome group (Table 3). Longitudinal multiple regression analysis yielded preoperative LBP as the most important variable (P < 0.01 in predicting the 3 month postoperative COMI after controlling for age, sex, comorbidity and baseline COMI score. In the multivariate model the beta coefficient for the LBP was 0.18 (Table 2). This indicated that, each 1 unit increase in LBP VAS at baseline is expected to increase (worse outcome) the 3 month COMI score by 0.18 (ie: 18%) if other factors are constant.
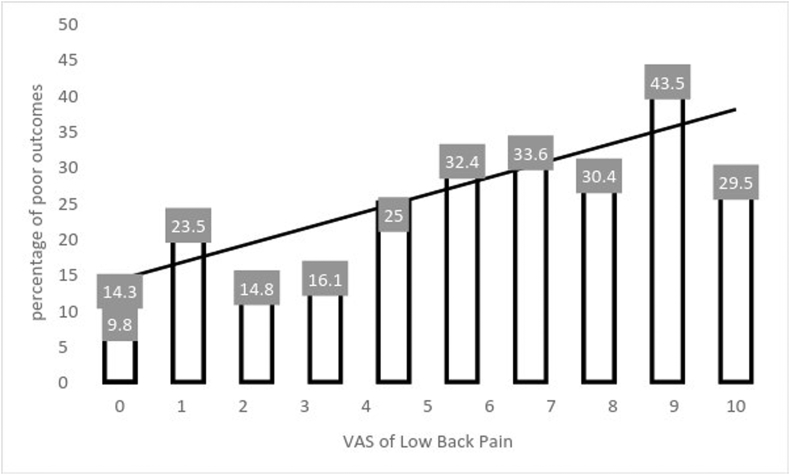
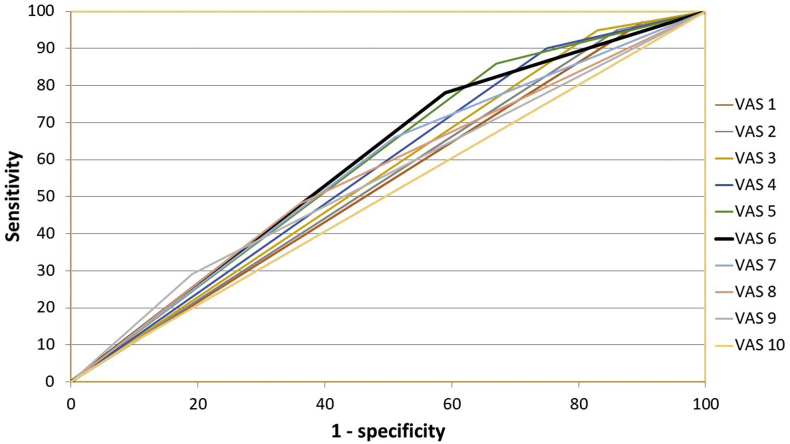
A bar plot of the percentage of poor outcome for each value of preoperative LBP VAS (Fig. 1) showed that the percentage of poor outcomes increased as the LBP VAS increased. A ROC plot of preoperative LBP VAS for predicting poor postoperative outcome, revealed a threshold of 6 for LBP VAS (ie: greatest area under the curve) (Fig. 2). At this threshold, LBP VAS had a 78% sensitivity and a specificity of 41% for predicting a poor outcome. The proportion of poor outcomes in patients with a LBP VAS greater than 6 was nearly double that in those with a LBP VAS less than 6 (34% versus 18%).
Fig. 1.
Bar graph showing percentage of poor outcome for each value of VAS of back pain.
Fig. 2.
Roc curve for the various values of preoperative LBP VAS
Before surgery, patients were required to indicate their main reason for undergoing surgery (from 3 options) – back pain, leg pain or neurological symptoms. 35% of patients who had stated their main problem as back pain had a poor outcome compared to 24% and 32% for those who had declared leg pain and neurological problems respectively as their main complaint. The difference between back pain and the other two (leg pain or neurological symptoms) was statistically significant (P < 0.01).
3.4. LP – LBP VAS as a predictor of outcome
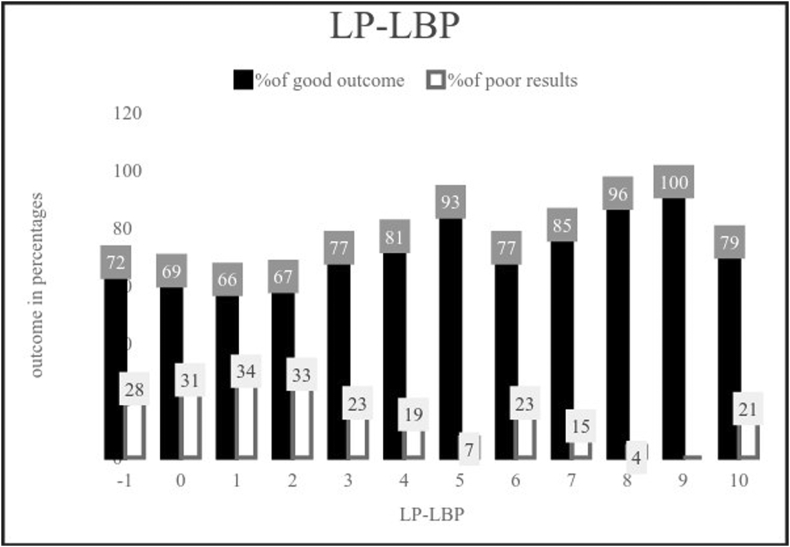
Better outcomes were seen in patients with greater difference between LP VAS and LBP VAS. A plot of LP – LBP VAS against the percentage of good and poor outcomes, revealed that a LP – LBP VAS of more than 3 equated to a good outcome in 77% (or more) of patients (Fig. 3). From the regression model a statistically significant, but weak correlation (r square = 0.03; P < 0.01) between LP – LBP VAS and the improvement in COMI at 3 months was also observed (Table 2). It was also observed that in patients with a LBP VAS less than 6, the LP – LBP VAS was more than 3 (exact value = 3.7), compared to 0.25 in the patients in the group with a LBP VAS more than 6.
Fig. 3.
Bar Graph Showing Percentage of Good and Poor Outcome for Each Value of LP-LBP.
The horizontal line shows that when LP-LBP is more than 3, 77% (or more) consistently have a good outcome.
3.5. Level of compression and outcome
The levels involved in this patient cohort are summarised in Table 1. The most commonly invovled level was L4/5 (n = 441, 44.5%) followed by L3/4 (n = 336, 33.9%). No significant difference was observed in outcomes between the lower lumbar segment procedures. The upper lumbar segment procedures had a significantly higher (P < 0.01) percentage of poor outcomes (62.2%) compared to lower lumbar segment procedures (26.9%).
4. Discussion
In the setting of lumbar disc degenerative disease, it would seem intuitive that surgical relief of stenosis or compression would result in improvement of radicular symptoms. Furthermore, it might seem logical that patients presenting with mainly radicular symptoms would be more likely to have a successful outcome after such surgery than patients who have a greater proportion of axial pain. This current study highlights evidence to support this premise.
We found that 72% of patients reported a good outcome at 3 month follow-up. This compares well with previously published studies.3,7,10,11 A significant reduction in leg pain and COMI score was observed in the early post-operative stage (3 months) for the group as a whole. Greater improvements were seen in leg pain than back pain, and even patients with a poor outcome exhibited a small but significant mean improvement in leg pain (1.24, P < 0.01). Probably unsurprisingly, back pain improvement was not significant in patients with a poor outcome (0.12 P = 0.22). The SPORT trial reported similar outcomes, with greater improvements in leg pain than back pain in patients treated conservatively and surgically.11
Age, gender, comorbidity and preoperative LP VAS were not found to influence outcome. Importantly, it was observed that a pre-operative LBP VAS greater than 6 doubled the risk of a poor outcome. For each unit increase in pre-operative LBP VAS, there was an 18% increase in the 3 month COMI score (ie: worse functional outcome). This relationship between preoperative LBP VAS and poor outcome has been previously identified.6 Studies have reported that a pain VAS is responsive enough to detect the minimal clinically important difference, when used for clinical decision making.12 In calculating the clinical overall score (COS) as a measure of outcome, Graver et al. reported VAS to be the most important factor in determining the success of surgery.13 The difference between leg pain and back pain severity was found to be predictive of poor outcome in this current study (LP – LBP VAS less than 3), and this is in keeping with other published work.6,8,14 Finally, we found that upper lumbar segment involvement seemed to carry a greater risk of poor outcome post-operatively, and this finding is supported by other published studies.14, 15, 16
We acknowledge some limitations in this study. There was no differentiation made between patients with lumbar stenotic disease and those with herniated lumbar discs. Our follow-up period was short (3 months), however it has been suggested that most post-operative improvement happens by 3 months.3,17,18 Furthermore, there is the possibility of clouding results by using a longer follow-up period due to natural ongoing/progressive degenerative changes.19 We feel that using a 3 month follow-up in this current study is reasonable, but certainly acknowledge that longer term follow up work in this area is required to clarify long term outcomes following this type of surgery and the durability of improvements achieved.
5. Conclusion
From the results presented here, we conclude that in patients undergoing a single level lumbar micro-decompression/discectomy, predictors of poor outcome in the early post-operative phase include: (1) a preoperative LBP VAS greater than 6, (2) a LP – LBP VAS less than 3 and (3) upper lumbar segment involvement (L1/2 or L2/3). These factors can be useful in selecting and counseling potential surgical candidates.
Compliance with ethical standards
The study was approved by the ethical committee of the University Of Salford, Manchester.
Disclaimer
The authors declare that no part of this study has been taken from existing published or unpublished materials without due acknowledgement and that all secondary materials used herein has been fully referenced.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contribution to the study
Gagan Sethi, Literature review, Data Collection, Data Analysis, manuscript writing. Ahmed Aljawadi, Data collection & analysis, Drafting and critical revision. Muhammad Choudhry, Operating Surgeon, Data collection. Fischer Ben, Operating Surgeon, Data collection. Hiren Maganlal Divecha, Operating surgeon, Data Collection. John Leach, Operating surgeon, Data Collection. Frances Arnall, Data analysis, Drafting and Critical analysis. Rajat Verma, Operating surgeon, Data analysis, Drafting and Critical analysis. Mohammed Naveed Yasin, Operating surgeon, Data analysis, Drafting and Critical analysis. Saeed Mohammed, Operating surgeon, Data analysis, Drafting and Critical analysis. Irfan Siddique, Operating surgeon, Data analysis, Drafting and Critical analysis.
Footnotes
Institutions. The University of Salford, and Salford Royal NHS Foundation Trust (SRFT).
Contributor Information
G. Sethi, Email: G.Sethi@edu.salford.ac.uk, drgsethi12@gmail.com.
A. Aljawadi, Email: Ahmed.Aljawadi@doctors.net.uk.
B. Fischer, Email: ben.fischer@srft.nhs.uk.
H.M. Divecha, Email: hiren.divecha@doctors.org.uk.
J. Leach, Email: john.leach@srft.nhs.uk.
F. Arnall, Email: F.Arnall@salford.ac.uk.
R. Verma, Email: u3.verma@srft.nhs.uk.
N. Yasin, Email: naveed.yasin@srft.nhs.uk.
S. Mohammad, Email: saeed.mohammad@srft.nhs.uk.
I. Siddique, Email: irfan.siddique@srft.nhs.uk.
References
- 1.Blamoutier A. Surgical discectomy for lumbar disc herniation: surgical techniques. Orthop Traumatol: Surg Res. 2013;99(1):S187–S196. doi: 10.1016/j.otsr.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 2.Weinstein J.N., Lurie J.D., Olson P., Bronner K.K., Fisher E.S., Morgan M.T.S. United States trends and regional variations in lumbar spine surgery: 1992–2003. Spine. 2006;31(23):2707. doi: 10.1097/01.brs.0000248132.15231.fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parker S.L., Mendenhall S.K., Godil S.S. Incidence of low back pain after lumbar discectomy for herniated disc and its effect on patient-reported outcomes. Clin Orthop Relat Res. 2015;473(6):1988–1999. doi: 10.1007/s11999-015-4193-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jansson K.-Å., Nemeth G., Granath F., Jönsson B., Blomqvist P. Health-related quality of life in patients before and after surgery for a herniated lumbar disc. J Bone Jt. Surg. Br vol. 2005;87(7):959–964. doi: 10.1302/0301-620X.87B7.16240. [DOI] [PubMed] [Google Scholar]
- 5.den Boer J.J., Oostendorp R.A., Beems T., Munneke M., Oerlemans M., Evers A.W. A systematic review of bio-psychosocial risk factors for an unfavourable outcome after lumbar disc surgery. Eur Spine J. 2006;15(5):527–536. doi: 10.1007/s00586-005-0910-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kleinstueck F., Fekete T., Jeszenszky D. The outcome of decompression surgery for lumbar herniated disc is influenced by the level of concomitant preoperative low back pain. Eur Spine J. 2011;20(7):1166–1173. doi: 10.1007/s00586-010-1670-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Junge A., Dvorak J., Ahrens S. Predictors of bad and good outcomes of lumbar disc surgery. A prospective clinical study with recommendations for screening to avoid bad outcomes. Spine. 1995;20(4):460–468. doi: 10.1097/00007632-199502001-00009. [DOI] [PubMed] [Google Scholar]
- 8.Soriano J.C., Revuelta M.S., Fuente M.F., Díaz I.C., Ureña P.M., Meneses R.D. Predictors of outcome after decompressive lumbar surgery and instrumented posterolateral fusion. Eur Spine J. 2010;19(11):1841–1848. doi: 10.1007/s00586-010-1284-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mannion A.F., Elfering A., Staerkle R. Outcome assessment in low back pain: how low can you go? Eur Spine J. 2005;14(10):1014–1026. doi: 10.1007/s00586-005-0911-9. [DOI] [PubMed] [Google Scholar]
- 10.Atlas S.J., Keller R.B., Wu Y.A., Deyo R.A., Singer D.E. Long-term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the Maine lumbar spine study. Spine. 2005;30(8):927–935. doi: 10.1097/01.brs.0000158954.68522.2a. [DOI] [PubMed] [Google Scholar]
- 11.Pearson A.M., Blood E.A., Frymoyer J.W. SPORT lumbar intervertebral disk herniation and back pain: does treatment, location, or morphology matter? Spine. 2008;33(4):428. doi: 10.1097/BRS.0b013e31816469de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hägg O., Fritzell P., Nordwall A. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12(1):12–20. doi: 10.1007/s00586-002-0464-0. [DOI] [PubMed] [Google Scholar]
- 13.Graver V., Haaland A., MAGNáS B., Loeb M. Seven-year clinical follow-up after lumbar disc surgery: results and predictors of outcome. Br J Neurosurg. 1999;13(2):178–184. doi: 10.1080/02688699943952. [DOI] [PubMed] [Google Scholar]
- 14.Dewing C.B., Provencher M.T., Riffenburgh R.H., Kerr S., Manos R.E. The outcomes of lumbar microdiscectomy in a young, active population: correlation by herniation type and level. Spine. 2008;33(1):33–38. doi: 10.1097/BRS.0b013e31815e3a42. [DOI] [PubMed] [Google Scholar]
- 15.Sanderson S.P., Houten J., Errico T., Forshaw D., Bauman J., Cooper P.R. The unique characteristics of “upper” lumbar disc herniations. Neurosurgery. 2004;55(2):385–389. doi: 10.1227/01.neu.0000129548.14898.9b. [DOI] [PubMed] [Google Scholar]
- 16.Albert T.J., Balderston R.A., Heller J.G. Upper lumbar disc herniations. J Spinal Disord. 1993;6(4):351–359. doi: 10.1097/00002517-199306040-00009. [DOI] [PubMed] [Google Scholar]
- 17.Mannion A., Porchet F., Kleinstück F. The quality of spine surgery from the patient's perspective: part 2. Minimal clinically important difference for improvement and deterioration as measured with the core outcome measures index. Eur Spine J. 2009;18(3):374–379. doi: 10.1007/s00586-009-0931-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Häkkinen A., Kautiainen H., Järvenpää S., Arkela-Kautiainen M., Ylinen J. Changes in the total Oswestry Index and its ten items in females and males pre-and post-surgery for lumbar disc herniation: a 1-year follow-up. Eur Spine J. 2007;16(3):347–352. doi: 10.1007/s00586-006-0187-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peul W.C., Van Houwelingen H.C., van den Hout W.B. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007;356(22):2245–2256. doi: 10.1056/NEJMoa064039. [DOI] [PubMed] [Google Scholar]