Abstract
Background
Patients affected by coxarthrosis may be treated surgically with total hip arthroplasty (THA). During the surgical intervention, the hip joint capsule can be completely removed, performing a capsulectomy. Otherwise it's possible to perform a capsulotomy, which allows for capsular conservation. Since there is no scientific evidence demonstrating the superiority of one method over the other, the choice whether to remove or conserve the capsule is at the surgeon's discretion and both procedures are actually accepted.
The purpose of our study is to evaluate the differences in functional activities and proprioception in patients who underwent THA and capsulotomy with capsular conservation versus patients who underwent THA with capsulectomy.
Methods
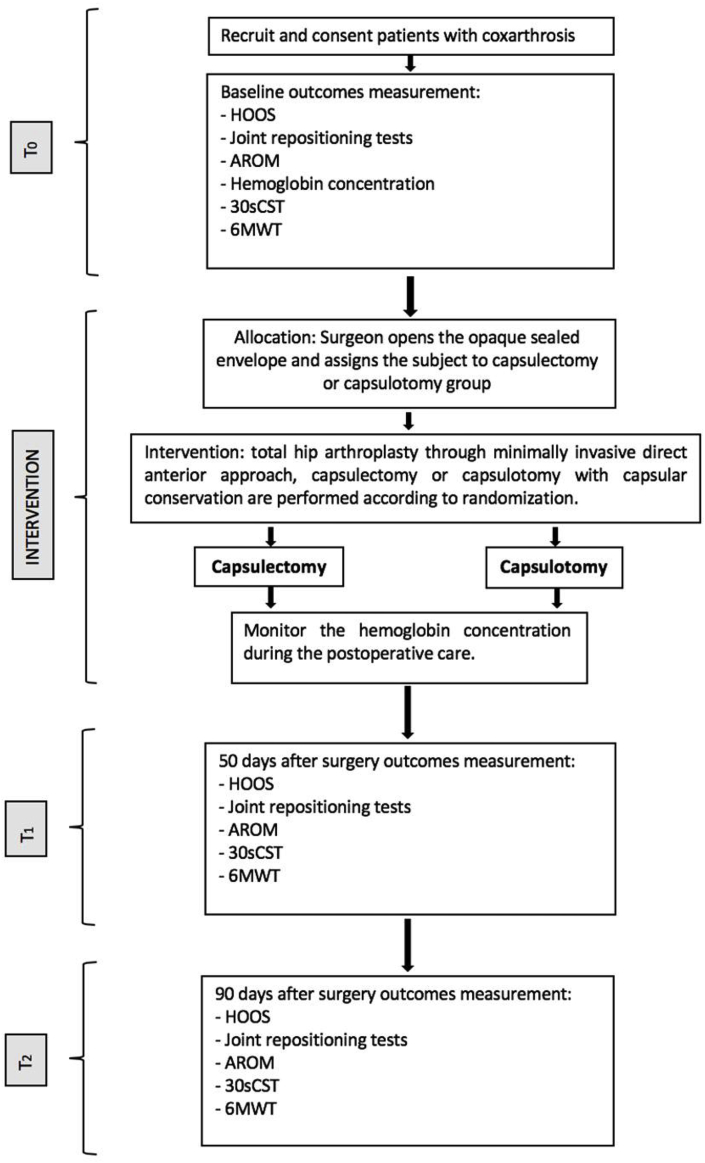
In order to compare the two surgical techniques of capsulotomy with capsular conservation and capsulectomy, we created a randomized, controlled, double-blind, single-centre, non-pharmacological, interventional, superiority, parallel-group trial. The primary outcome of our study is evaluated using the HOOS scale (Hip disability and Osteoarthritis Outcome Score). Secondary outcomes are: the proprioceptive sensitivity, the postoperative bleeding, the surgical time, the active range of motion, and the ability to walk, sit and stand. The proprioception study is carried out through active and passive repositioning tests. THA is performed through the minimally invasive direct anterior approach. The evaluation tests are carried out in the 15 days preceding the intervention (T0), at 50-day post-operative (T1), and finally at three months after surgery (T2).
Discussion
Considering that the hip joint capsule is innervated by proprioceptive nerve endings, while the psuedocapsule that replaces the native capsule following a THA with capsulectomy doesn't have any active neurophysiological role, we hypothesize that capsulotomy with capsular conservation at the time of primary THA may lead to better proprioception and therefore better functional recovery.
Trial registration
ClinicalTrials.gov identifier: NCT02749058. Date of registration: 04/21/2016.
Keywords: Capsulotomy, Capsulectomy, Proprioception, Total hip arthroplasty, Minimally-invasive approach
1. Background
In total hip arthroplasty surgery (THA), the hip joint capsule needs to be approached in order to reach the intra-articular plane. There are two different techniques of capsular approach: the first one is capsulectomy and the second one is capsulotomy, followed by capsular repair at the end of the articular replacement procedure. Both preserving and excising the capsule are accepted methods and the choice whether to repair the capsule or not is at the surgeons’ discretion, since studies have not demonstrated the superiority of one technique over the other yet.1
The hip joint capsule has a neurophysiological role2, 3, 4, 5 and the presence of proprioceptive nerve endings in both healthy patients and those affected by coxarthrosis has been demonstrated.6
Proprioception, literally the “sense of self” (from Latin proprius, meaning individual, and capio, to take or grasp), is the group of sensory modalities that allow us to know the positions of our limbs in space and to detect and assess the magnitudes of movements and forces without vision.7
Performing a capsulectomy during primary arthroplasty, a pseudocapsule will replace the native capsule. Instead of the physiological capsule, the pseudocapsule does not have any active neurophysiological role. In fact, the presence of proprioceptive nerve endings has never been demonstrated in the pseudocapsule of patients who underwent primary THA with capsulectomy7
In light of this evidence, we hypothesize that capsulotomy with anatomical repair at the time of primary THA may lead to a better proprioception, and therefore to a better functional recovery, since nerve endings are preserved.
However, capsulotomy with capsule repair may result in an increased postoperative pain, and in a reduction of the articular range of motion (ROM). This could occur due to a number of reasons. At first, capsule sparing approach could result in a longer operative time as well as the reconstructed capsule built over the prosthesis could be an obstacle to movement.
Moreover, preserving the capsule with its nociceptors could result in increased postoperative pain.1
Concerning the aforementioned considerations, the aim of this paper is to create a study protocol in order to compare the two surgical techniques and highlighting a possible superiority of capsulotomy with capsular repair in terms of functional recovery and proprioceptive sensibility.
2. Methods
2.1. Design
This is a controlled, randomized, monocentric, interventional, double-blinded study of superiority, with parallel groups. For the single patient, the study has a duration of 105 days, starting 15 days before surgery and ending 90 days after this (see Table 1) .
Table 1.
Study periods.
| STUDY PERIOD |
||||
|---|---|---|---|---|
| Enrolment and Baseline Assessments | Allocation and Intervention | 45 days follow up | 90 days follow up | |
| TIMEPOINT |
T0 |
Tintervention |
T1 |
T2 |
| ENROLMENT: | ||||
| Eligibility screen | X | |||
| Informed consent | X | |||
| Allocationa | X | |||
| INTERVENTION: | ||||
| THA with Capsulectomy or Capsulotomy | X | |||
| ASSESSMENTS: | ||||
| HOOS | X | X | X | |
| Joint repositioning tests | X | X | X | |
| Hemoglobin concentration | X | Xb | ||
| Surgical time | X | |||
| 30sCST | X | X | X | |
| 6MWT | X | X | X | |
Allocation is performed the day of the intervention, 30 minutes before surgery.
Hemoglobin concentration is tested during the 15 days of postoperative care.
This study began after receiving the permission by the ethic committee in March 2016, and will go on until the required number of subjects for each of the two groups is reached. The required sample size is calculated to be 94 patients.
The study was approved by the Ethics Committee in March 2016 and is registered with the Clinical Trials Registry, clinicaltrials.gov identifier: NCT02749058. Reporting of the study will adhere to the Consolidated Standards of Reporting Trials (CONSORT) guidelines. Participants will be randomized into either a “capsulectomy” group or a “capsulotomy” group. The SPIRIT checklist for this study protocol can be accessed as Additional file.
2.2. Inclusion/exclusion criteria
We recruited patients with a surgical indication of primary hip arthroplasty. Our inclusion criteria are elective unilateral primary hip arthroplasty via direct anterior approach (the direct anterior approach is used in order to standardize the surgical technique and because it is a tissue-sparing technique); age ≥ 18; signature of the informed consent.
Exclusion criteria we have adopted are documented peripheral neuropathies, documented central nervous system and neuromuscular diseases; presence of other joint prosthesis in the lower limbs, revision hip arthroplasty, symptomatic osteoarthritis of other joints in the lower limbs or the spine, body mass index (BMI) > 35. Indeed, the aforementioned conditions could influence hip proprioception and consequently they could have interfered with the execution of the clinical study.
The whole sample of patients resulted homogenous considering both the surgical indications and the potential co-morbidities, as well as the stage of osteoarthritis.
2.3. Withdrawal and termination criteria
Withdrawal from the study is possible at any time without giving reasons and investigators may determine whether it is unsafe for the subject to continue in the study. There aren't conditions that allow a temporary treatment discontinuation. Any decision about to abandon the project will be permanent.
2.4. Randomization
Offsite randomization procedures ensure random and concealed allocation of participants. An outside researcher electronically randomizes participants to either “capsulectomy group” or “capsulotomy” group.
An allocation concealed approach with the opening of opaque sealed envelopes during surgical time by the appointed surgeon is adopted.
2.5. Study intervention
The intervention is total hip arthroplasty surgery through the minimally invasive direct anterior approach.1According to randomization, patients undergo a capsulectomy, or a capsulotomy with capsular repair at the end of the procedure.
The direct anterior approach is a technique which follows a surgical path of intermuscular and internervous planes, therefore reducing the risk of damage to periarticular structures such as muscles, nerves and tendons. The hip joint is approached in the intermuscular plane between the tensor fascia lata and sartorius/rectus femoris.1,8
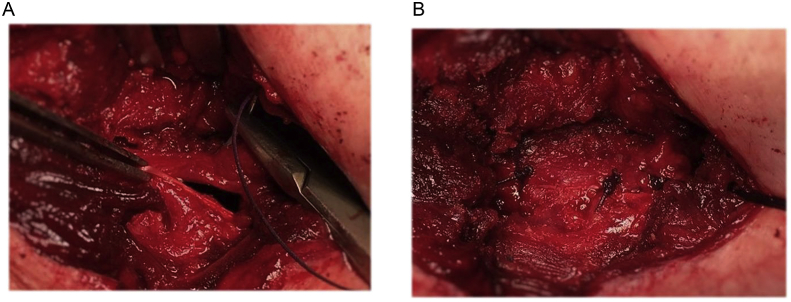
According to the randomization, the capsule could be cut and conserved, or partially removed. In both cases, the capsule must be incised following the ileocapsularis muscle edge from distal to proximal. Proximally, the incision ends at the anterior edge of the acetabulum. Distally, the incision runs along the infero-medial insertion of the capsule, then laterally following the intertrochanteric line along the vastus lateralis fibres. Thus, a triangular flap is detached laterally over the fibres of the gluteus minimus in the direction of the tensor fasciae latae. In case of capsule-sparing procedure, the flap should be ensured with a suture in order to ease the access to the intra-articular space and to preserve it during all steps of the joint replacement procedure.1 Otherwise, in the capsulectomy group, the triangular flap is completely removed. As the joint capsule is opened and conserved – in case of capsulotomy – or removd in case of capsulectomy, the procedure of joint replacement can be performed. At the end of the arthroplasty procedure, if the capsule has been conserved, this is then reconstructed over the prosthetic joint through a suture of the triangular capsular flap with few resorbable stiches. Finally, a drainage is placed and the surgery wound is closed (see Fig. 1).9
Fig. 1.
a,b: capsule reconstruction in a patient belonging to capsulotomy group.
In this study, all surgery procedures are carried out by two surgeons, who are also the investigators.1
2.6. Outcome measures
We compared the two groups in terms of functional activities, proprioception and surgical parameters. Primary outcome of this study is the Hip disability and Osteoarthtitis Outcome Score (HOOS)10; secondary outcomes are: proprioception, surgical time, blood loss, ability to walk, sit and stand, active range of motion (AROM). Subjects undergo assessment tests about functional activities and proprioception. These tests will be performed 15 days before the operation (T0), at 50 days (T1), and at three months after the operation (T2).
2.7. Primary outcomes
The outcome evaluation scale chosen for the primary endpoint is the Hip disability and Osteoarthtitis Outcome Score (HOOS), that is a validated scale that analyses symptoms, pain, activities of daily living (ADL), sport and recreational activities and quality of life (QoL).10The clinically relevant difference at T1, as stated in previous studies, is 9.1.11We will also evaluate pain, ADL, sport activity, and QoL subscales that we believe are the most important to underline the difference in proprioception that can be found maintaining or removing the articular capsule.11
2.8. Secondary outcomes
The maximal active articular ROM (AROM) was measured manually through a goniometer.
To measure flexion, the subject was asked, from a supine position, to maximally flex the hip, twice while also maintaining a flexed knee, and once with an extended knee. Should he not be able to completely extend the knee, the subject was asked to extend it as much as possible.
The subject always had to lift his heel from the table during the execution of movements.
To measure abduction, the subject was positioned supine and was asked to abduct the limb as much as possible without extrarotating the hip. To facilitate the movement and in order to calculate the degree of abduction, a graduated plank was placed under the patient.
To measure extrarotation, the subject was settled in upright position and is asked to extrarotate the hip while keeping the pelvis still. The subject is placed with the foot to be examined on a rotating platform, while the other foot is placed on a fixed support of the same height. On the rotating platform, extrarotation ROM are depicted. Furthermore, the subject was given a support to maintain balance and was asked to concentrate on distributing the weight equally on both legs and to keep his trunk as straight as possible.
The AROM was evaluated as the difference in measured values in the pre-op session and in both post-op sessions, and the difference of these in the two groups at the same time.
For all the performed movements, the best performance was taken into account.
2.9. Proprioception
In order to evaluate proprioception, the difference in degrees between a reference angle and the angle reproduced by the subject in active and passive joint reposition test was measured.
The reference angles were chosen according to the maximal ROM that has been previously calculated. From the best performance, the angles at 80% and 50% are taken, and for each of these two values the subject will carry out two trials, resulting in four active and four passive repetitions.
Concerning flexion, the angles at 80% and 50% from the ROM with extended knee are taken, since the repositioning trial will be carried out with the extended knee, even though this does not represent the maximal ROM.
Since the receptors present in the articular capsule are more sensible to maximal degrees of movement an 80% angle was chosen, however we did not want to choose an excessively high ROM that would have caused pain in the subject. The 50% angle, on the other side, was chosen because the identification of a movement reaching about half of the maximal ROM is more difficult to identify for the patient, and because choosing a smaller angle would have implied technical difficulties as very small angles would have resulted, which would have been difficult to measure (e.g. the actual movement of extrarotating a hip by 10° is so small that it would be difficult to measure).
In the active joint reposition test, the subject has to move his leg until he reaches a predetermined position. In flexion, the subject has to stop once he touches a rubber band positioned at the required height to perform the necessary extent of movement; in abduction and extra-rotation, the subject stops once he touches a weight placed at the required distance. This position is maintained for three seconds, after which the subject will return to his neutral position. After three seconds, the subject has to perform the same movement without the previously present reference points, so this time he will have to stop the movement autonomously, once he feels to have reached the previous position.
In the passive joint reposition test, the operator who moves the subject's leg and stop at certain predetermined degree, keeping that position for three seconds. The operator then moves the leg back to the neutral position, maintaining it for three seconds. Afterwards, the operator will again move the leg and will stop once the subject feels to have reached the previous position and tells the operator to stop the movement.
It is important that the operator tries to maintain the same grip throughout the entire movement and also in the following trials, in order to provide the patient with as few tactile references as possible. The operator has to try and keep a velocity of movement of about 10°/seconds.12
As for ROM measurement, flexion and abduction are tested with the subject supine, while extrarotation is tested with the subject in upright position.
Movements tested this way are hip flexion, abduction, adduction, external rotation and internal rotation.
The surgical time is measured as the difference between the beginning and ending time of surgery in the two groups.
Blood loss is calculated as the decrease in haemoglobin percentage, will be estimated considering basal values at pre-op and the values at 15 days post-operatively.
2.10. Walking
Walking was evaluated through the six Minute Walk Test (6MWT), analysing the difference in distance, measured in meters, and the subject's endurance.13,14
The aim of the test is to measure the distance that the subject is able to cover in 6 minutes of time. It evaluates the functional status of the patient, estimating its capacity to exercise, but considering the subject in the precise moment in which the test is executed, since this test is influenced by many variables, such as tiredness, physical pain, and the use of inappropriate shoes that alter the result.15
Before starting the test, precise instructions were given to the patient in order to highlight that the purpose is not to walk at maximal velocity, but to cover the maximal distance. It is a self-based test, in which the patient regulates the velocity and decides to stop if necessary.16
During the test, the subject should be able to use the walking aids he normally uses.
The circuit used measures 15 m in length and is delimitated by two cones, it is even and does not present obstacles. Even though the required length between the two cones is of 30 or 20 m, we do not feel that this biased the result in any way, since all the trials executed for every subject have been carried out on the same path, so no subject has been favoured over the other.
Before and after the trial the subject is handed out the BORG Rating of Perceived Exertion (RPE 6-20) scale, which evaluates the global sensation of fatigue in a deconditioned subject, such as patients with OA that may reduce the activity due to pain or functional limitation16. It is important to explain to the subject that the parameter which is being measured is the sensation of fatigue, and not hip pain. The subject needs to read all the words together with the examiner, and decide in which word he allocates himself and then indicate the corresponding number. Using this scale we are both able to evaluate if the patient improves the covered distance, and it's globally ability to better endure exertion.16
2.11. Sit-to-stand ability
To evaluate sit-to-stand ability, the 30 seconds Chair Stand Test (30sCST) was used. It evaluates leg strength during that functional activity.17 In this test, we count how many times the patient will be able to stand from a 44cm-chair in 30 seconds, and only the movements with a right execution (with a complete hip and knee extension, and to complete sit) are considered.
We chose this test over other test that allow to evaluate the time needed to carry out a predetermined amount of movements, such as the 5 Times Sit-To-Stand test, as we felt that the 30sCST allowed to evaluate a wider variety of functional levels, with a scoring system that, for the population tested by us, started from zero, for those who could not stand without using their hands, to 15 for women and 17 for men, indicating more athletic individuals.
2.12. Evaluation of T0, intervention, T1 and T2
2.12.1. T0
At T0 the subject needs to undergo instrumental (axial hip XR, pelvis XR, chest XR, ECG), and haematochemical examination (haemochrome) required for all interventions, in addition to examination by the anaesthesiologist.
Furthermore, an orthopaedic examination is required, carried out by the same orthopaedic surgeon that will successively operate the patient; during this examination, the patient is asked to participate in the study, and if he meets all the requirements and accepts to participate in the study, he may sign the informed consent.
During the physical examination of the hip, the following parameters are evaluated: leg length, ROM, and possible positivity for flexion adduction internal rotation (FADDIR), flexion abduction external rotation (FABER), log roll and Trendelenburg tests.
We may now proceed to the analysis in the physiotherapy lab, where the patient is handed out the HOOS scale. After completing the latter, six markers are placed on the subject on the following anatomical landmarks: right anterior superior iliac spine (ASIS), left ASIS, trochanter, lateral femoral epicondyle, lateral malleolus, head of the second metatarsus.
First, the maximal ROM in flexion is evaluated, first with the knee in flexion and then with an extended knee. Successively, the passive and active repositioning trials are carried out. The same is done for the evaluation of abduction movement. For the evaluation of extrarotation, which is carried out in an upright position, three additional markers are placed, namely on the right posterior superior iliac spine (PSIS), the left PSIS (posterior superior Iliac spine) and C7.
After having measured the maximal ROM and having carried out all repositioning trials, the patient will do the 6MWT and the 30sCST test (see Fig.2).
Fig. 2.
Flow chart of the trial protocol.
Legend: HOOS: Hip disability and Osteoarthtitis Outcome Score; AROM: Active Range Of Motion; 30sCST: 30 seconds Chair Stand Test; 6MWT: six Minutes Walk Test.
2.12.2. Intervention
On the day of admission, haematochemical exams are done (haemochrome).
On the day of the operation, total hip arthroplasty via anterior mini-invasive (AMIS-technique) is carried out. Immediately after surgery, the patient will receive an axial XR of the hip for control.
The first day after the operation, haematochemical exams are done again (haemochrome, C-Reactive Protein, electrolytes). The drainage is kept in place while the patient is instructed on how to carry out isometric exercises. If possible, the patient is positioned in a sitting position.
The second day after the operation, the drainage is removed and a haemostatic stocking is worn by the patient to avoid thrombus formation, furthermore, the patient will walk short distances with auxiliary devices.
On the fourth post-operative day, haematochemical exams are done.
After hospitalization in the Orthopedics department, patients are discharged and addressed to a rehabilitation structure, where they will stay about 15 days, during which they will undergo a rehabilitation therapy to recover the ROM, muscle trophism and will train to walk and climb stairs.
2.12.3. T1
At 50 days post-operatively, the subject will undergo a control orthopaedic examination, during which the axial XR of the hip that the patient must have done in the previous days, will also be controlled.
As for the T0, the patients will again be examined in the physiotherapy lab, completing the HOOS, measuring the ROM and carrying out the active and passive repositioning tests as well as completing the 6MWT and the 30sCST.
2.12.4. T2
At 90 days post-operatively, the subject will again undergo a control orthopaedic examination and tested as well as for T0 and T1.
2.13. Experimental setting
Evaluation of proprioception required the development of an appropriate setting. For each movement a different set of tools was necessary.
For flexion analysis, a table with two demarcations was used. The first – more cranial demarcation – was placed in correspondence of the marker on the greater trochanter, while the second demarcation was used as a reference to position two tripods. The latter are placed at the sides of the examination table and are inclined towards its head. Furthermore, on the tripods there is a graduated notch displaying, with a 5° interval, degrees from 15° to 60°.
To study active repositioning, a thick, transparent hollow tube was spanned between the tripods in order for the patient to easily feel it once he touches it.
For abduction analysis, two tables were placed adjacent to each other, and a plank reporting abduction degrees (from 0° to 50°) was placed on top of them. The patient was positioned with the femoral head's projection at the level of the abduction ray's origin.
For extrarotation analysis, a custom-made device has been used. A graduated circular platform that can rotate both clockwise and counter-clockwise has been mounted on a wooden plank. Next to it, a fixed wooden support of the same height of the previously mentioned platform has been placed. On the former goes the limb to be examined, while on the latter goes the other limb.
2.14. Data acquisition
Data have been acquired at the Laboratory for Human Movement Analysis of the Physiotherapy, Neuroscience department of our hospital.
Data acquisition has been achieved through BTS Bioengineer software for movement analysis.
The optoelectronic system SMART DX 7000 (BTS SpA, Italy) has been used. It consists of seven video cameras that acquire three-dimensional coordinates of the markers that have been placed on the subject's anatomical landmarks. The camera's sampling frequency is of 500 H, and these are positioned in the lab in order to be able to frame the entire movement and warrant visibility of every marker by at least three cameras. The markers, passive and spherical in shape, reflect the infrared radiation, and the reflection is in turn read as a luminescent dot.
With the Biomech Motion Analysis System software, which is linked to the optoelectronic system SMART DX 7000, it is possible to record the three-dimensional position of the markers in every moment, allowing for movement analysis thanks to the marker's movement in space.
Data acquired in this way and relative to movement kinematics are the three-dimensional coordinates in every instant at the centre of the marker.
The marker's coordinates' trajectories have been elaborated in a first instance by the software SMARTTRACK (BTS SpA, Italia), which allowed for marker tracking, namely the calculation of their trajectory. This passage is fundamental for the following data elaboration.
Finally, in order to elaborate data, a protocol was created using the SMARTAnalyzer (BTS SpA, Italia) software, which allowed to assess a calculation scheme generating necessary data for a complete analysis.
2.15. Analysis protocol
Once data has been recorded with the Biomech Motion Analysis System software, previously designed tracking protocols have been used. Protocols were different for the right or the left hip, for flexion, abduction or extrarotation.
The tracking operation represents the link between two successive frames one with the other to identify the temporal evolution of the markers, hence of the body as a whole.
Once the movement has been reconstructed, we move to the analysis of the repositioning error.
A specific protocol for each movement has been created, which allowed to calculate the difference in degrees between the reference position and the reproduced position.
For flexion movement, the angle formed between the thigh vector (e.g. the vector that extends from the marker on the trochanter up to the marker on the lateral epicondyle of the femur) and the surrounding environment, used as a point of reference, has been used. Since the objective was only that of evaluating the error on a sagittal plane, the projection on the latter was considered.
To determine the angle of the thigh vector, the angle between the projected thigh vector and the X-axis in space was measured. In addition, to achieve a cleaner movement, small oscillations of 6Hz have been corrected. At this point, two stable periods have been chosen from the obtained movement graph, one for the reference movement and one for the reproduced movement. A stable period is defined as a time-frame of one second in which the position of the limb is as static as possible.
From the above mentioned two stable periods the mean of the angle has been calculated. Moreover, the difference between the stable period of the repositioning and the stable period of the reference angle has been evaluated. The resulting numerical value represents the relative error and provides information about the direction of the error.
For abduction movement, the same protocol was used, but this time the axis of reference in space is the Z-axis.
Finally, for extrarotation, the angle considered was between the foot vector (e.g. the vector extending between the lateral malleolus and the head of the second metatarsus) and the Z-axis in space. Since in rotation the executed movements were very small, the correction of oscillation was carried out at a frequency of 4Hz, which proved to be much more sensible.
2.16. Sample size calculation
The sample size, estimated based on the difference between groups equal to the MCID of the primary outcome at 50 days postop, must be of 43 subjects for each group. We will increase this value by 10% to face drop out, the total number of subjects analysed will be 94 (47 each for each group). We are planning a study of a continuous response variable from independent control and experimental subjects, with one control per experimental subject. In previous studies, response within each subject group was normally distributed with a standard deviation of 14.8. If the true difference between the experimental and control means is 9.1 (MCID of the HOOS, our primary outcome), we will need to study 43 experimental subjects and 43 control subjects to be able to reject the null hypothesis that the population means of the experimental and control groups are equal with BETA error probability of 0.8 (power of 80%). The Type I error probability associated with this test of this null hypothesis is 0.05.18 At this value, we add 10% of subjects to hedge against potential drop out, obtaining a sample size of 94 subjects, 47 for each group. Standard deviation was elaborated from a recent study on the same topic.19 We assume that the standard deviation of principal outcome is the same in each group.
2.17. Statistical analysis
Statistical data will be analysed Per-Protocol, so we won't consider data from drop-out subjects. Demographic data and outcomes will be analysed with descriptive statistics. Continuous variables (HOOS, 6MWT, 30sCST, degrees of active and passive joint reposition, AROM, surgical time) will be summed up with mean, standard deviation, minimal value, maximal value, and median. Frequency and percentage of subjects in each category will be given for categorical data. Two groups outcomes will be compared using the Analysis of Variance (ANOVA). T-test for paired data will be used to compare changes from baseline for each outcome in each group. T-test for independent data will be used to verify difference between the two groups for each variable at a given time.
2.18. Data collection and management
All data are collected in case report forms for each patient. All information obtained in this study are preserved by our Department of Orthopedics and Traumatology and by our Laboratory of Analysis and Rehabilitation of Motor Function.
2.19. Trial quality assurance and control
It is the responsibility of the investigator to maintain adequate and accurate case report forms (CRFs). All CRFs must be completed in their entirety in a neat, legible manner to ensure accurate interpretation of data. According to the ICH/Good Clinical Practice, the monitoring team must check the Case Report Form entries against the source documents.
2.20. Trial status
We are actively recruiting at the time of submission. Patient recruitment started on April 2016 and the study is scheduled for completion in October 2019.
3. Discussion
Nowadays the proprioceptive role of the joint capsule remains still unclear. Some authors suggest that joint receptors themselves do not bear primary responsibility for our proprioceptive acuity.20 In fact, joint afferents appear to respond primarily at extremes of the joint's angular excursion, showing fewer degrees of response throughout the entire physiological range of joint movement. This sensitive power is provided by high mechanical thresholds mechanoreceptors known as Ruffini organs.20 Otherwise, the evidence of sensory function of the joint capsule is provided by studies stating that anesthesia of the interphalangeal joint attenuates its proprioception and, on the other hand intra-articular fluid expansion improve the one, suggesting a role of joint afferents in proprioception. Supporting this evidence, it has been noticed that intraneural microstimulation of a single joint afferent in conscious human subjects can be perceived as a pressure over the joint or as a small movement, suggesting a strong synaptic coupling to higher order sensory neurons in the joints afferents.21 Concerning the human hip capsule, several anatomic studies have demonstrated its complex innervation according to specific capsular regions. In particular, anteromedial innervation is determined by the articular branches of the obturator nerve. The anterior hip joint capsule is innervated by sensory articular branches from the femoral nerve. The posteromedial region is innervated by articular branches from the sciatic nerve. The posterolateral region is innervated by articular branches of the superior gluteal nerve.2
Furthermore, it has been found that the hip capsule shows a quite homogeneous innervation, with a higher nerve fibers concentration in the superior part of the capsule.22
Given the aforementioned considerations, since THA requires the capsule incision and possibly its removal, the understanding of the overall regenerative ability of the fibers is crucial. Particularly, it has been noticed that in case of capsule removal a pseudocapsule will form over time to replace the original capsule. Syed et al.7 analysed 20 full-thickness pseudocapsule specimen, excised via the original approach, from patients who had to undergo revision total hip replacement surgery. To evaluate the presence of mechanoreceptors, an immunohistochemical approach was chosen, using monoclonal antibodies against S-100 protein, which is expressed by nerve fibers, free nerve endings, and sensory corpuscles including periaxonal cells. The results show no mechanoreceptors detected in any of the 20 specimens analysed. The pseudocapsule turned out to be a crude fibrous envelope showing some areas of hyalinization with occasional histiocytes. Sparingly, free nerve endings were observed in some samples, mainly in the deeper layers.7
Currently, during total hip arthroplasty surgery, whether the articular capsule is removed (capsulectomy) or incised and later sutured (capsulotomy) is entirely dependent on the surgeon's preference. However, to this day scientific literature does not provide the means to properly justify choosing either technique, and consequently the surgeon's decision is based on his personal experience. Surgeons in favor of capsular conservation suggest that capsule may exert a prophylactic effect on post-operative dislocation and preservation of proprioceptive sensibility, while the ones in favor of capsulectomy suggest that capsular preservation may result in pain persistence after joint replacement. In order to compare these two assumptions, a well-designed superiority trial with an appropriate statistical power is necessary.
Considering the small number of studies in the literature, the purpose of this study is to create a protocol which aims to find answers on the issue capsulotomy vs capsulectomy. To evaluate the potential importance of capsular conservation we built a randomized, interventional, double-blind trial that evaluates the neurophysiological function of the capsule, the proprioception and the implications that it brings in terms of functional outcomes.
From our analysis of the literature, we set the following pivots on which the study protocol is based on: the presence of proprioceptive nerve endings in the hip joint capsule, which has been demonstrated in healthy subjects as well as in subjects affected by hip osteoarthritis; the formation of pseudocapsule without any proprioceptive nerve endings following the capsulectomy; the direct anterior approach for THA as a muscle and nerve sparing technique which is crucial for the surgery, since any additional damage to the hip joint and musculature would result in confounding factors for functional outcomes.
4. Conclusion
Whereas the pseudocapsule formed after excision of the capsule will not have any active neurophysiological role, we hypothesize that capsulotomy with anatomical repair at the time of primary THA may lead to better proprioception and therefore better functional recovery. For that reason, the aim of our study is to create a protocol able to compare the two surgical techniques in order to state a possible superiority of capsulotomy with capsular repair in terms of functional recovery and proprioceptive sensibility.
Ethics approval and consent to participate
This study protocol was approved by the Ethics Committee of our hospital and its reference number is CE:28/INT/2016; therefore it was conducted in accordance with the principles laid down by the 18th World Medical Assembly (Helsinki, 1964) and all applicable amendments laid down by the World Medical Assemblies, and the International Council for Harmonisation (ICH) guidelines for Good Clinical Practice. All participants will complete informed consent to participate.
List of abbreviations
THA: Total Hip Arthroplasty; HOOS: Hip disability and Osteoarthritis Outcome Score; ROM: Range Of Motion; CONSORT: Consolidated Standards Of Reporting Trials; BMI: Body Mass Index; AROM: Active Rangeof Motion; QoL: Quality Of Life; 6MWT: 6 Minutes Walk Test; 30sCST: 30 seconds Chair Stand Test; FADDIR: Flexion Adduction Internal Rotation; FABER: Flexion Abduction External Rotation; ASIS: Anterior Superior Iliac Spine; PSIS: Posterior Superior Iliac Spine; ANOVA: Analisis Of Variance; CRFs: Case Report Forms; ICH: International Council for Harmonisation.
Consent for publication
Not applicable.
Availability of data and materials
No data to publish yet.
Competing interests
The authors declare that they have no competing interests.
Funding
No funding has been and will be received for the present trial.
Acknowledgments
We would like to thank the Department of Orthopedics and Traumatology, San Raffaele Hospital; the Laboratory of Analysis and Rehabilitation of Motor Function, San Raffaele Hospital; and the Department of Anatomical Pathology, San Raffaele Hospital.
References
- 1.Keggi K.J. Anterior approach to total hip replacement: surgical technique and clinical results of our first one thousand cases using non-cemented prostheses. Yale J Biol Med. 1993;66(3) 243- [PMC free article] [PubMed] [Google Scholar]
- 2.Birnbaum K. The sensory innervation of the hip joint--an anatomical study. Surg Radiol Anat. 1997;19(6):371–375. doi: 10.1007/BF01628504. Hewitt JD. The mechanical properties of the human capsule ligaments. J Arthroplasty. 2002;17(1):82-9. [DOI] [PubMed] [Google Scholar]
- 3.Hewitt J.D. The mechanical properties of the human capsule ligaments. J Arthroplast. 2002;17(1):82–89. doi: 10.1054/arth.2002.27674. Martin HD. The function of the hip capsular ligaments: A quantitative report. Arthroscopy. 2008;24(2):188-95. [DOI] [PubMed] [Google Scholar]
- 4.Martin H.D. The function of the hip capsular ligaments: a quantitative report. Arthroscopy. 2008;24(2):188–195. doi: 10.1016/j.arthro.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 5.Alzaharani A., Bali K. The innervation of the human acetabular labrum and hip joint: an anatomic study. BMC Muscoskelet Disord. 2014 doi: 10.1186/1471-2474-15-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moraes M.R., Cavalcante M.L. The characteristics of the mechanoreceptors of the hip with arthrosis. J Orthop Surg Res. 2011 doi: 10.1186/1749-799X-6-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Syed S.N. Assessing regeneration of mechanoreceptors in human hip pseudocapsule after primary total hip arthroplast. JOTR. 2014;18:1. [Google Scholar]
- 8.Matta J.M. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res. 2005;441:115–124. doi: 10.1097/01.blo.0000194309.70518.cb. [DOI] [PubMed] [Google Scholar]
- 9.Masonis J. Safe and accurate: learning the direct anterior total hip arthroplasty. Orthopedics. 2008;31(Suppl 12):2. [PubMed] [Google Scholar]
- 10.Nilsdotter A.K. Hip disability and osteoarthritis outcome score (HOOS) - validity and responsiveness in total hip replacement. BMC Muscoskelet Disord. 2003;30:4–10. doi: 10.1186/1471-2474-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berliner J.L. Preoperative patient-reported outcome measures predict clinically meaningful improvement in function after THA. Clin Orthop Relat Res. 2016;474(2):321–329. doi: 10.1007/s11999-015-4350-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suarez T. Comparison in joint-position sense and muscle coactivation between anterior cruciate ligament-deficient and healty individuals. J Sport Rehabil. 2016;25(1):64–69. doi: 10.1123/jsr.2014-0267. [DOI] [PubMed] [Google Scholar]
- 13.Perera S. Change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54(5):743–749. doi: 10.1111/j.1532-5415.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- 14.Bennell K. Measures of physical performance assessments: self-paced walk test (SPWT), stair climb test (SCT), six-minute walk test (6MWT), chair stand test (CST), timed up & go (TUG), sock test, lift and carry test (LCT), and car task. Arthritis Care Res. 2011;63(Suppl 11):350–370. doi: 10.1002/acr.20538. [DOI] [PubMed] [Google Scholar]
- 15.ATS Statement Guidelines for the 6 minutes walk test. Am J Respir Crit Care Med. 2002;166(1):111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 16.Lazzeri M. Edra Editore; 2014. Il ricondizionamento all’esercizio fisico nel paziente con patologia respiratoria: dalla valutazione al trattamento. [Google Scholar]
- 17.Kennedy D.M. Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC Muscoskelet Disord. 2005;28 doi: 10.1186/1471-2474-6-3. 6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dupont W.D. Power and sample size calculations for studies involving linear regression. Contr Clin Trials. 1998;19:587–601. doi: 10.1016/s0197-2456(98)00037-3. [DOI] [PubMed] [Google Scholar]
- 19.Barker K.L. Recovery of function following hip resurfacing arthroplasty: a randomized controlled trial comparing an accelerated versus standard physiotherapy rehabilitation programme. Clin Rehabil. 2013;27(9):771–784. doi: 10.1177/0269215513478437. [DOI] [PubMed] [Google Scholar]
- 20.Ferrell W.R., Gandevia S.C., Mccloskey D.I. The role of joint receptors in human kinaesthesia when intramuscular receptors cannot contribute. J Physiol. 1987;386:63–71. doi: 10.1113/jphysiol.1987.sp016522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Macefield V.G. 2005. Proprioception: Role of Joint Receptors Proprioception: Roles of Muscle Receptors; pp. 3315–3318. [Google Scholar]
- 22.Haversath M., Hanke J., Landgraeber S. The distribution of nociceptive innervation in the painful hip. Bone Joint Lett J. 2013;95-B(6):770–776. doi: 10.1302/0301-620X.95B6.30262. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data to publish yet.