Abstract
Introduction
Cartilage regeneration have been attracted attentions because of the poor ability of cartilage tissues to regenerate. Three-dimensional (3D) culture of chondrocytes is considered to be advantageous for cartilage regeneration. Although it is plausible that maturation of the constructs before transplantation positively affects the chondrogenesis, matured constructs after cultures for longer periods do not necessarily result in effective cartilage regeneration. In this study, we compared different types of culture media including growth factors which are clinically available. We prepared differentiation medium containing insulin-like growth factor-1 (IGF-1), proliferation medium containing fibroblast growth factor-2 (FGF-2) and insulin, and combination of them, and compared their efficacies on chondrogenesis when used in 3D culture of engineered cartilage constructs.
Methods
Cartilage constructs were fabricated by auricular chondrocytes and atelocollagen, and they were 3D-cultured with four types of media: control medium, differentiation medium, proliferation medium, and combination medium. After 3 weeks of culture, the constructs were analyzed for cell number, gene and protein expressions and mechanical properties. The constructs were also transplanted into nude mice. After 8 weeks, the degree of cartilage regeneration was evaluated. Constructs manufactured with canine auricular chondrocytes were subjected to autologous transplantation into beagles and examined for cartilage regeneration.
Results
During 3D culture, remarkably high gene expression of type II collagen was detected in the construct cultured with the differentiation medium whereas cell apoptosis were suppressed in the proliferation medium. When transplanted into nude mice, the constructs 3D-cultured in the proliferation medium produced abundant cartilage matrices. In autologous implantation model, the construct cultured in the proliferation medium again showed better chondrogenesis than those in other media.
Conclusions
The present study indicates that 3D culture with the proliferation medium maintains the cell viability to potentiate the subsequent cartilage regeneration. Here, we propose that not only differentiation but also high cell viability accompanied by proliferation factors should be taken into account to improve cartilage regeneration.
Keywords: Cartilage regeneration, Three-dimensional culture, Culture medium
Highlights
-
•
Differentiation mediun induced maturation of cartilageous constructs in 3D culure.
-
•
Proliferation medium used in 3D culure induced better chondrogenesis in vivo.
-
•
Proliferation medium prevented chondrocytes from apoptosis.
1. Introduction
Over the past several decades, cartilage regeneration techniques have been intensively studied, because cartilage tissues seldom regenerate. Since the report by Brittberg et al., in 1995, autologous chondrocyte implantation (ACI) has been applied for the treatment of articular cartilage defects [[1], [2], [3]]. However, there was a concern regarding dedifferentiation of applied chondrocytes because they would readily undergo dedifferentiation during monolayer culture [4,5].
To date, some studies have revealed that chondrocytes cultured in a three-dimensional (3D) environment with scaffolds composed of several materials such as agarose gels, collagen gels, alginate beads and hyaluronic acid, or in a scaffold free conditions are able to maintain or regain their characteristics as chondrocytes [[6], [7], [8], [9], [10], [11]]. In addition, 3D culture improves maturation of engineered cartilage after transplantation into animals [12,13]. Based on this idea, regenerative cartilage constructs composed of autologous chondrocytes and atelocollagen hydrogel were applied in clinical researches [[14], [15], [16], [17]].
Culture conditions of regenerative cartilage largely affect cartilage formation after transplantation [12,13,[18], [19], [20], [21], [22], [23]]. Culture media is one of the factors which affects the cartilage regeneration. Moretti et al. compared differentiating medium and proliferating medium used in pre-culture, and concluded differentiation medium containing transforming growth factor-β (TGF-β), insulin, and ascorbic acid was better for the cartilage regeneration after transplantation [19]. Culture period is another factor affecting the chondrogenesis. Many of the studies concluded that appropriate culture period (i.e. 1–3 weeks) improved chondrogenesis, while too long culture resulted in worse results in spite of the better maturation in vitro [13,20,21]. These results suggested that in vitro maturation does not necessarily promote chondrogenesis after transplantation.
Considering clinical application of the culture method, it is quite important to use agents which have been approved for clinical use. Although TGF-β is often used for chondrogenic culture [19,20,24,25], it has not been approved for clinical use. Alternatively, insulin-like growth factor-1 (IGF-1), recombinant form of which is used for the treatment of growth failure, is also known to induce chondrogenesis as TGF-β [26]. In 3D environment, IGF-1 induce matrix synthesis in explant culture of cartilage [27,28] and a scaffold free 3D culture of chondrocytes using bioreactor [29], and to promote survival of chondrocytes in alginate suspension culture [30]. On the other hand, effects of IGF-1 used in 3D preculture on cartilage generation after transplantation have not been fully defined.
The effects of IGF-1 in monolayer preculture on chondrocytes have been reported by several groups. Shakibaei M et al. reported IGF-1 preserve chondrogenic potential of human chondrocytes in monolayer culture [31]. IGF-1 was also shown to induce cell proliferation and production of collagen and glycosaminoglycan [32]. On the contrary, Mounts T et al. showed that rabbit auricular chondrocytes cultured with fibroblast growth factor-2 (FGF-2), which induce proliferation of chondrocytes, was better than those with IGF-1 in generating cartilaginous tissue by aggregate cultures [33]. This report raised a question whether 3D preculture using differentiating medium containing IGF-1 or that with proliferation medium is better for cartilage generation after transplantation.
Our group have screened clinically-available growth factors for their effects on proliferation of auricular chondrocytes, and found that combination of FGF-2 and insulin or IGF-1 was found to be best for the expansion of auricular chondrocytes in monolayer culture [34].
In the present study, we compared the efficacy of differentiation medium containing IGF-1, proliferation medium containing FGF-2 and insulin defined by our group, and combination of them used in 3D culture on the maturation of engineered cartilage constructs in vitro and in vivo.
2. Materials and methods
2.1. Materials and antibodies
Dulbecco's Modified Eagle's Medium/Nutrient Mixture F-12 Ham (DMEM/F12), human serum, penicillin-streptomycin solution, and trypsin–EDTA solution were purchased from Sigma Chemical Co. (MO, USA), IGF-I was from Astellas Pharma Inc (Tokyo, Japan), FGF-2 was from Kaken Pharmaceutical Co, Ltd. (Tokyo, Japan), and insulin was from Novo Nordisk Pharma Ltd. (Tokyo, Japan). One percent atelocollagen was purchased from Kawaken Fine Chemicals Co., Ltd. (Tokyo, Japan), 3% atelocollagen from Koken Co., Ltd. (Tokyo, Japan), poly-L lactic acid (PLLA) scaffolds from GC R&D Dept. (Tokyo, Japan), collagenase, type I from Clostridium histolyticum from Worthington Biochemical Corporation, collagenase from C. histolyticum and anti-collagen antibody (type I and II) from LSL CO., LTD, TdT-mediated dUTP nick end labeling kit (TUNEL) from TAKARA Bio Inc. (Tokyo, Japan), anti-proliferating cell nuclear antigen antibody (PCNA) from Abcam® plc (Tokyo, Japan). Biotinylated secondary antibody, Vectastain Elite ABC Kit, and DAB Peroxidase Substrate Kit were all obtained from Vector Laboratories (Burlingame, CA).
2.2. Isolation and culture of human auricular chondrocytes
The ethics committee of the University of Tokyo Hospital approved all procedures in the present study (ethics permission #622). Remnant auricular cartilages were obtained from microtia patients during reconstruction surgeries of ears under informed consent. Auricular chondrocytes were isolated and cultured as previously described [35]. Briefly, cartilages were cut into small pieces and incubated in 0.3% collagenase in DMEM supplemented with penicillin and streptomycin at 37 °C for 16 h. After the incubation, the solution containing cells was passed through a 70-μm nylon cell strainer (BD Falcon, Bedford, MA), centrifuged at 430 g for 5 min, and washed twice with DMEM supplemented with penicillin and streptomycin. Auricular chondrocytes were cultured in DMEM/F12 supplemented with 5% human serum, FGF-2 (100 ng/mL), and insulin (5 μg/mL), and cells of passage 1 (P1) were collected for the fabrication of constructs. Their viability was confirmed by a NucleoCounter™ device (Chemometec); only cells with more than 96% viability were used in this study.
2.3. Fabrication of constructs and transplantation in nude mice
For the fabrication of constructs, P1 human auricular chondrocytes were suspended in 0.8% atelocollagen gel (Kawaken) and then incubated for gelation at 37 °C in 5% CO2 for 2 h. The cells were embedded at three concentrations: 1 × 106 cells/100 μL (High), 1 × 105 cells/100 μL (Middle), and 1 × 104 cells/100 μL (Low). In 3D culture, 4 types of media were employed: control medium consisting of DMEM/F12 without any additives; differentiation medium consisting of DMEM/F12 supplemented with IGF-I (1 μg/mL); proliferation medium consisting of DMEM/F12 supplemented with 5% human serum, FGF-2 (100 ng/mL), and insulin (5 μg/mL); and combination medium consisting of DMEM/F12 containing all the factors (IGF-I, human serum, FGF-2, and insulin). The constructs were cultured in 10 mL of each type of medium, and the medium was fully exchanged twice a week.
To investigate cell proliferation, 36 constructs were fabricated for 3 cell densities (High, Middle, and Low), 4 kinds of media (control, differentiation, proliferation, and combination), and 3 culture periods (1, 2, and 3 weeks) for the 3D culture group, and 3 more constructs at each cell density were prepared for the direct group; in total, 39 constructs were manufactured at the beginning of a series of experiments (direct and 3D culture groups, n = 3). After each culture period, the constructs were weighed and digested with 0.3% collagenase solution (Wako) at 37 °C for 1 h. Then the number of cells was counted using a hemocytometer with trypan blue staining.
For transplantation experiments, 5 constructs at a cell density of 1 × 106 cells/100 μL (High) were prepared: one construct was subcutaneously transplanted into the back of a 6-week-old male BALB/c nu/nu mouse (Nisseizai, Tokyo, Japan) immediately after the fabrication of the construct (direct group, n = 3), and the other 4 were 3D-cultured in each medium for 3 weeks and then implanted following the same procedure as the direct group (3D culture groups, n = 3). Each construct was independently transplanted into an individual mouse for 8 weeks.
2.4. Fabrication of constructs with PLLA and transplantation into beagles
Canine auricular chondrocytes were isolated from the ear cartilage of a beagle by digesting with 0.6% solution of type I collagenase (Worthington) at 37 °C for 18 h. P0 cells were used without passaging because the amount of autologous serum for the media was not enough for 3 weeks of 3D culture. The cells were suspended in 1% atelocollagen gel (1:2 mixture of 3% atelocollagen gel and DMEM/F12), and applied to a porous PLLA scaffold, which had successfully supported chondrogenesis in beagles [36], to sustain the size and shape of a construct under the thick canine skin. Each 10 × 10 × 5 mm3 PLLA scaffold held 2.5 × 106 cells/500 μL and was incubated at 37 °C in 5% CO2 for 2 h to complete gelation. The engineered constructs were then divided into the direct group and 3D culture groups. The constructs were 3D-cultured in 50 mL of each type of medium, and the medium was fully exchanged twice a week. With time differences due to the presence or absence of 3D culture, they were autologously transplanted into subcutaneous space in the back of the same beagle under general anesthesia by halothane (Takeda Pharmaceutical Co. Ltd., Osaka, Japan). Eight weeks after transplantation, the constructs were excised from the implantation site under general anesthesia, and the animal was euthanized by intravenous injection of potassium chloride after the excision of the 3D cultured constructs. One beagle was used in a series of experiments (direct and 3D culture groups, n = 3).
2.5. Histological and immunohistochemical staining
A harvested sample was cut in half; one half underwent biochemical analyses (described below), and the other half was fixed with 4% paraformaldehyde, embedded in paraffin, and cut into 5 μm sections for histological analyses. The sections were stained with toluidine blue (TB) to detect proteoglycan and with hematoxylin and eosin (HE) to observe cell morphology. To examine type I and II collagen, PCNA, and apoptotic cells, immunohistochemical staining was employed according to the manufacturer's instructions. After activating the antigens and blocking non-specific binding, incubation with primary antibodies (Rabbit polyclonal anti-type I collagen, 1:6000 dilution; rabbit polyclonal anti-type II collagen, 1:200 dilution; and rabbit polyclonal anti-PCNA, 1:6000 dilution) was performed overnight at 4 °C. The sections were then incubated with biotinylated secondary antibodies diluted 1:200 for 30 min at room temperature. The visualization of positive reactions was conducted using a Vectastain Elite ABC kit and DAB Peroxidase Substrate Kit following the manufacturer's instructions. Finally, they were counterstained with hematoxylin for type I and II collagen and with methyl green for TUNEL and PCNA. Positive ratios of TUNEL and PCNA were defined by counting the number of positive cells out of total cells in randomly selected five fields under a microscope (× 20 magnification); numerical values were calculated by averaging the cell numbers.
2.6. Biochemical analyses and measurement of mechanical strength
One half of a harvested sample was cut into tiny pieces with scissors and dissolved in 10 mg/mL pepsin and 0.05 M acetic acid at 4 °C for 48 h. Then, 1 mg/mL pancreatic elastase and 10 × TBS were added to each sample, and they were incubated at 4 °C overnight. The samples were centrifuged at 12,000 g for 15 min, and the supernatant was subjected to examinations for type I and II collagen by ELISA (Chondrex, Redmond, WA, USA) and glycosaminoglycan (GAG) by Alcian blue binding assay (Wieslab AB, Lund, Sweden) according to the manufacturer's instructions. Mechanical strength was measured in terms of Young's modulus with a Venustron tactile sensor (Axiom, Fukushima, Japan) as previously described [37].
2.7. RNA isolation and real time RT-PCR
A collected sample was dissected into small pieces and total RNA of cells in the construct was isolated by ISOGEN (Nippon Gene Co., Ltd, Tokyo, Japan) according to the manufacturer's instructions. RNA was reverse-transcribed with PrimeScript™ reagent Kit (TAKARA Bio Inc., Tokyo, Japan), and gene expression was detected by real time qPCR using Fast SYBR® Green Master Mix with ABI Real-Time PCR System (Applied BioSystems, CA, USA). Sequences of primers used for RT-PCR were as follows: 5′-ATTCCAGTTCGAGTATGGCG-3′ and 5′-CGACAGTGACGCTGTAGGTG-3′ for alpha-1 type I collagen (COL1A1), 5′-TTCAGCTATGGAGATGACAATC-3′ and 5′-AGAGTCCTAGAGTGACTGAG-3′ for alpha-1 type II collagen (COL2A1); 5′-ATGATGACCATGGCGTGTTCATAA-3′ and 5′-AAGGAAAAGGACTCAAATTCTGTTG-3′ for caspase-3; 5′-TCCTACAAATCTCGCGGGAAT-3′ and 5-GCATTTCTCGGAGCCTCTCA-3′ for matrix metalloproteinase-13 (MMP-13); 5′-GAAGGTGAAGGTCGGAGTCA-3′ and 5′-GAAGATGGTGATGGGATTTC-3′ for glyceraldehyde-3-phosphate dehydrogenase (GAPDH). All the primers were confirmed to be specific to only the human gene, and transcript levels were normalized to that of GAPDH.
2.8. Statistics
Statistical evaluation was performed using JMP Pro software version 12 software (SAS Institute Japan Ltd.). Data were expressed as mean ± standard deviation. Statistical significance was evaluated using Dunnett's test. A value of p < 0.05 was considered to indicate statistical significance.
3. Results
3.1. Characteristics of engineered constructs 3D-cultured with different types of media
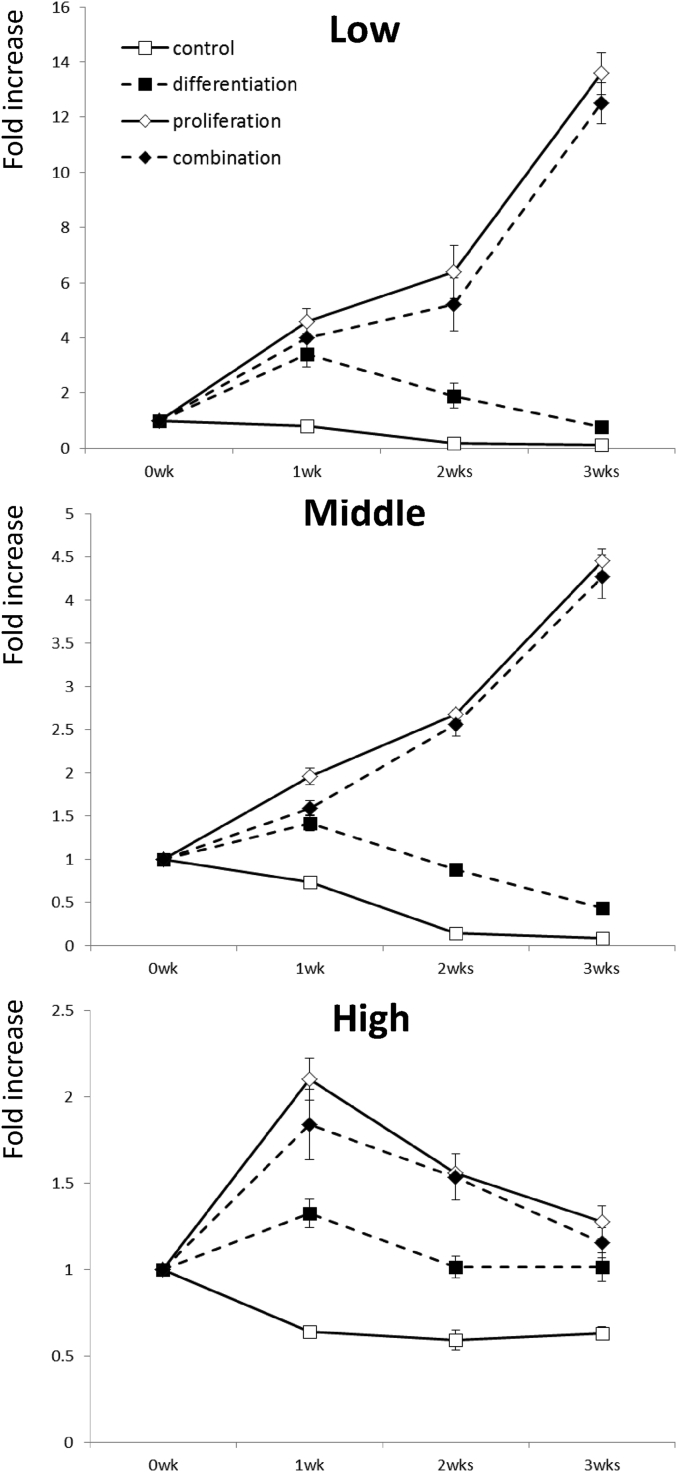
Firstly, to confirm the effects of different type of media on the cell proliferation in constructs, cell numbers in the constructs were counted at different time points during 3D culture. At the low and middle cell densities, the cell number increased in a time-dependent manner in proliferation and combination media for 3 weeks indicating the mitogenic effects of proliferation medium on chondrocytes, while it gradually decreased in control and differentiation media after 1 week (Fig. 1 Low and Middle). On the other hand, at the high cell density, the cell number increased rapidly, reached its peak at 2 weeks, and then turned to decline in proliferation medium and combination medium. Cell number was almost unchanged in differentiation medium, and the cells constantly decreased in number from the beginning in control medium (Fig. 1 High). As a result, cell numbers were similar in constructs cultured in proliferation, differentiation and combination media at high cell density.
Fig. 1.
Number of chondrocytes in engineered constructs during 3D culture. P1 human auricular chondrocytes were mixed with atelocollagen at the densities of 105 cells/mL (Low), 106 cells/mL (Middle), and 107 cells/mL (High) to fabricate constructs. The number of cells in the constructs at 1, 2, and 3 weeks were calculated.
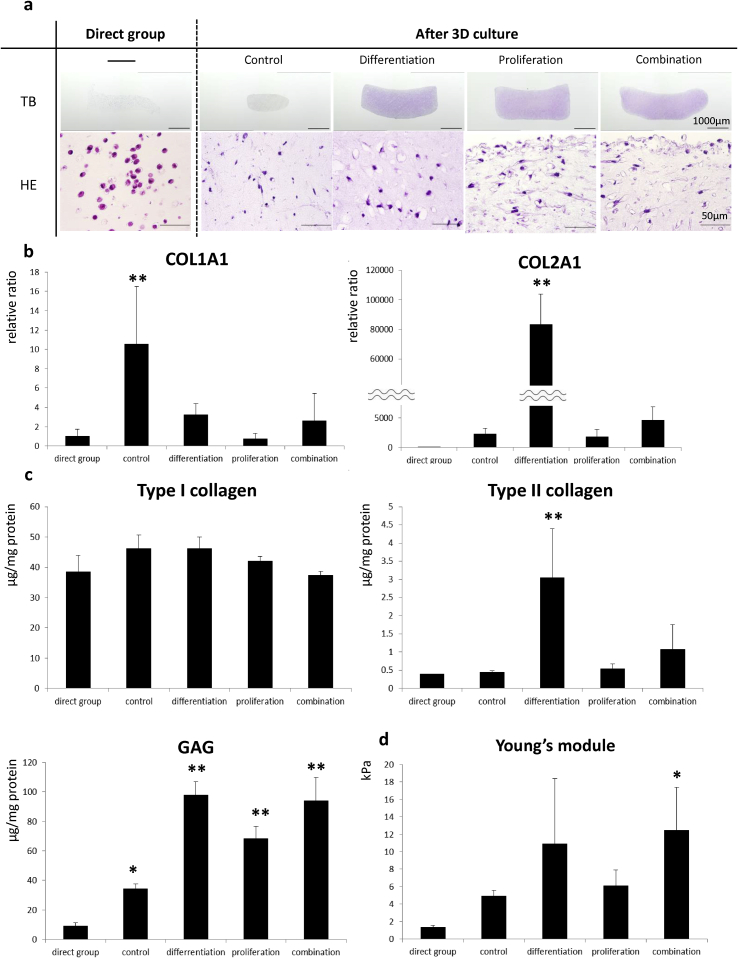
To evaluate the effects of 3D culture on cell differentiation and tissue maturation, constructs of high cell density with or without preculture in different media for 3 weeks were examined histologically. Toluidine blue (TB) staining showed slight but uniform metachromasia over the entire sections, indicating the immature glycosaminoglycan production in all the 3D culture groups except the control group (Fig. 2a TB). Hematoxylin and eosin (HE) staining showed that spindle-shaped, fibroblast-like cells were observed for the most part in the construct with control medium, whereas chondrocytes in lacunae were abundantly detected in that with differentiation medium. In the constructs with proliferation and combination media, both types of cells were scattered over the specimens (Fig. 2a HE).
Fig. 2.
Histological, biochemical, and biomechanical analyses of engineered constructs in vitro. Engineered constructs were analyzed just after fabrication or 3-weeks culture in control, differentiation, proliferation or combination media. (a): Histological findings of the constructs. (TB) Toluidine blue staining. Scale bars = 1 mm. (HE) Hematoxylin and eosin staining. Scale bars = 50 μm. (b): Gene expression of alpha-1 type I collagen (COL1A1) and alpha-1 type II collagen (COL2A1) determined by real-time RT-PCR. Data are expressed as mean ± standard deviation. Statistical significance was evaluated using Dunnett's test. **p < 0.01 vs. the direct group. (c): Matrix accumulation of the constructs. Protein synthesis of type I and II collagen and GAG accumulation were examined by ELISA and Alcian blue binding assay, respectively. Statistical significance was evaluated using Dunnett's test. **p < 0.01, *p < 0.05 vs. the direct group. (d): Young's modulus of the constructs. Young's modulus was measured with a Venustron tactile sensor. Data are expressed as mean ± standard deviation. Statistical significance was evaluated using Dunnett's test. *p < 0.05 vs. the direct group.
Gene expression levels of collagens were determined to examine effects of the media on chondrocyte differentiation during 3D culture. COL1A1, which is a marker of chondrocyte dedifferentiation, was expressed higher in control medium than in the other media. COL2A1 was expressed significantly higher only in the differentiation group relative to the direct group, confirming the chondrogenic activity of IGF-1 (Fig. 2b). Biochemical measurements revealed that only differentiation medium promoted the accumulation of both type II collagen and GAG whereas proliferation and combination media enhanced only GAG production (Fig. 2c). Similarly to the GAG measurement, the elasticity was increased in combination group, and showed tendency to increase in differentiation group, suggesting that the stiffness of constructs would depend on the GAG accumulation, but not on type I or type II collagen (Fig. 2d).
3.2. Chondrogenesis of engineered constructs after transplantation
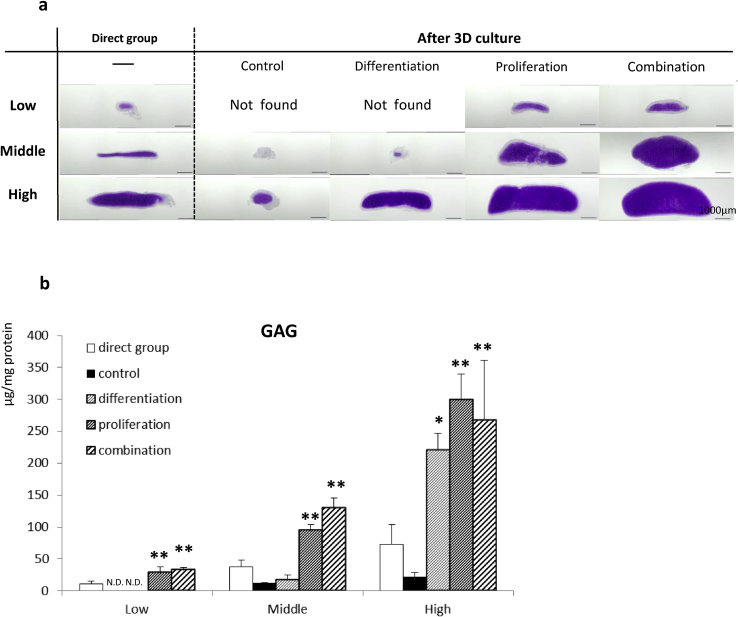
To analyze the effects of different types of media during 3D culture on following cartilage regeneration in vivo, engineered constructs were transplanted into nude mice. Without 3D culture, chondrogenesis was detected regardless of the cell density, and the volume of the regenerated cartilage and GAG content increased steadily, depending on the cell density (Fig. 3a and b). By 3D culture in control medium, chondrogenesis was obviously suppressed in constructs with all the cell densities; notably, the transplanted construct with low cell density disappeared. In differentiation medium, cartilage was regenerated and matured with abundant ECM in the construct with the high cell density; however, with the low and middle densities, the constructs barely sustained their size and shape or produced cartilage matrices. In proliferation and combination media, chondrogenesis was improved in the constructs with all the cell densities, exhibiting the excellent cartilage formation in both histological and biochemical examinations; in particular, GAG production in the proliferation and combination group was significantly higher than that in the direct group at all the cell densities (Fig. 3a and b).
Fig. 3.
Chondrogenesis of engineered constructs in vivo (nude mice). The constructs with or without 3D culture were transplanted subcutaneously into the back of BALB/c nu/nu and evaluated histologically and biochemically after 8 weeks. (a): Toluidine blue staining. Scale bars = 1 mm. (b): GAG accumulation examined by Alcian blue binding assay. Data are expressed as mean ± standard deviation. Statistical significance was evaluated using Dunnett's test. **p < 0.01, *p < 0.05 vs. the direct group.
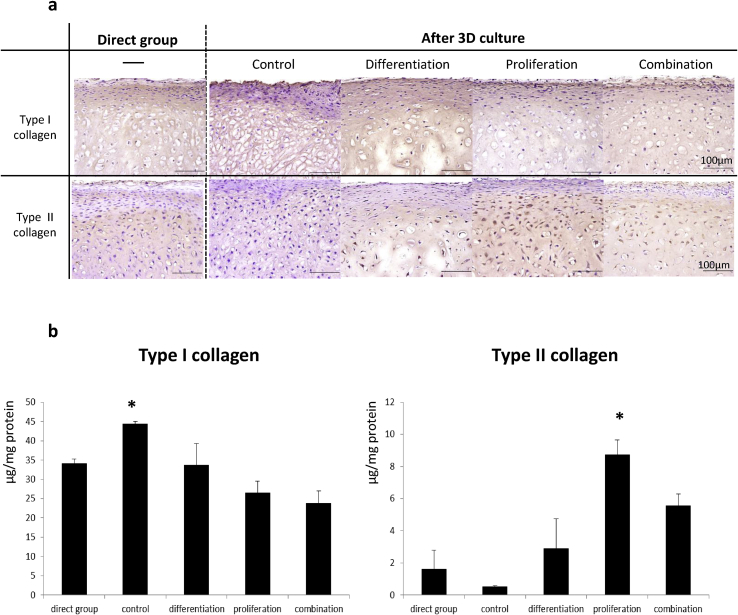
The characteristics of engineered constructs after transplantation were examined in detail by evaluating the accumulation and localization of type I and II collagen. The results of immunohistochemical staining revealed the deposition of dense type II collagen from the surface to deep inside the construct only in the proliferation group. On the other hand, sparse localization of type I collagen was observed only near the surface in all the groups (Fig. 4a). The accumulation of type I and II collagen was quantified by ELISA, and the result supported the immunohistochemical findings. There was a statistically significant difference in collagen II accumulation between the proliferation group and the direct group (Fig. 4b).
Fig. 4.
Immunohistochemical analysis of engineered constructs in vivo. Localization and content of type I and II collagen in the constructs were examined 8 weeks after transplantation into nude mice. (a): Immunostaining for type I and II collagen. Scale bars = 100 μm (b): Protein synthesis of type I and II collagen, examined by ELISA. Data are expressed as mean ± standard deviation. Statistical significance was evaluated using Dunnett's test. *p < 0.05 vs. direct group.
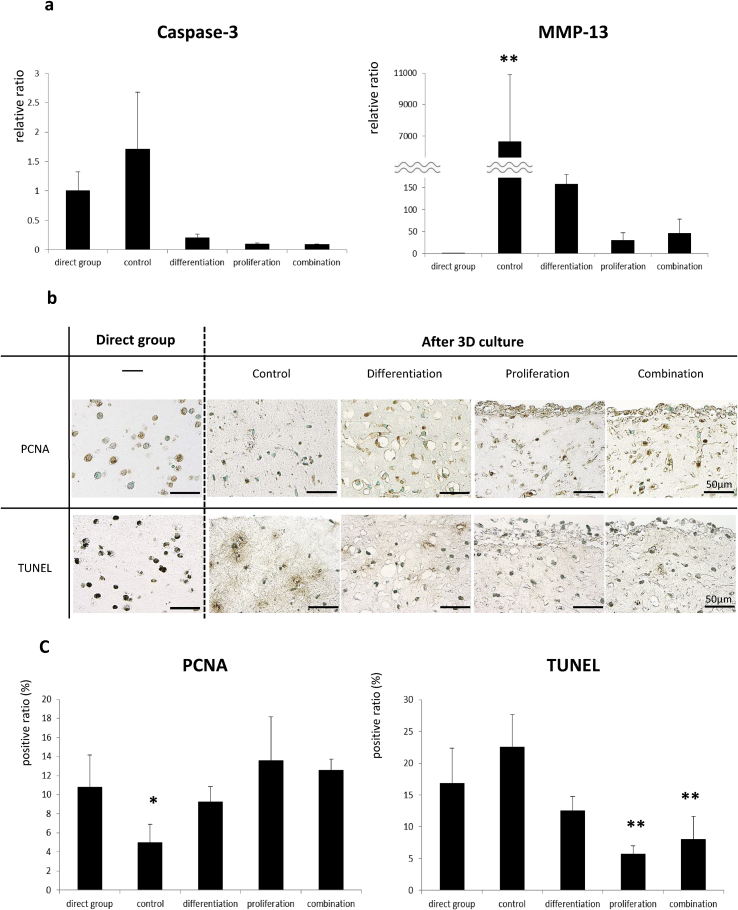
To elucidate why constructs that had been 3D-cultured in proliferation medium showed the robust cartilage regeneration after transplantation, we examined properties of the constructs before transplantation. First, we explored gene expression levels of catabolic and apoptotic factors. The expression of matrix metalloproteinase 13 (MMP-13), a catabolic factor of cartilage, was enormously higher in control group than in the other groups. In the differentiation group, expression of MMP13 is higher than proliferation and combination groups (Fig. 5a). Caspase-3, which plays an essential role in apoptosis and likely has a negative effect on chondrogenesis, tended to be highly expressed in the constructs without 3D culture or any stimulating factors during 3D culture (Fig. 5a). In addition, immunohistochemical and biochemical analyses showed that apoptosis frequently occurred in control and differentiation media (Fig. 5b and c TUNEL) whereas PCNA expression was not significantly different among groups except the control group (Fig. 5b and c PCNA). From these results, it is suggested that proliferation medium promoted cartilage regeneration by suppressing apoptosis of chondrocytes.
Fig. 5.
Biochemical examination and immunohistochemical analysis of catabolic factors and cell apoptosis in engineered constructs in vitro. Expression of catabolic factors and cell apoptosis in the constructs with or without 3D culture were examined. (a): Gene expression of MMP-13 and caspase-3. Data are expressed as mean ± standard deviation. Statistical significance was evaluated using Dunnett's test. **p < 0.01 vs. the direct group. (b): Immunostaining for PCNA and TUNEL. Scale bars = 50 μm. (c): Positive ratios of PCNA and TUNEL were counted under a microscope (positive cells out of total cells,×20 magnification, average of 5 fields). Data are expressed as mean ± standard deviation. Statistical significance was evaluated using Dunnett's test. **p < 0.01, *p < 0.05 vs. the direct group.
3.3. Autologous transplantation of engineered constructs after 3D culture
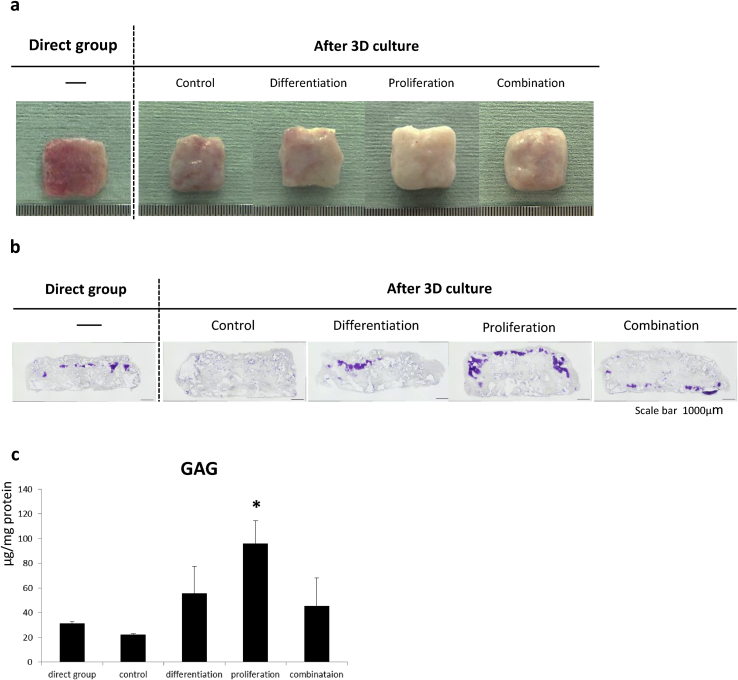
Considering clinical application of regenerative cartilage, autologous transplantation to immunocompetent host is a possible case. We investigated the effects of 3D culture in the beagle autologous transplantation model. In the proliferation group, the engineered construct appeared glossy and white after transplantation. By contrast, the surface of harvested construct in the direct or other 3D culture groups were rough and tinged with red to a greater or lesser extent (Fig. 6a). Certainly, the most extensive metachromasia was observed by TB staining, although positive areas of TB staining were limited to the superficial regions of the constructs (Fig. 6b). A statistically significant increase in GAG accumulation were detected in the proliferation group (Fig. 6c).
Fig. 6.
Chondrogenesis of engineered constructs in vivo (beagle). The constructs were fabricated with P0 canine auricular chondrocytes, atelocollagen (Koken), and PLLA scaffolds, and then transplanted subcutaneously into the back of beagles. Eight weeks after transplantation, the constructs were evaluated histologically and biochemically. (a): Morphological features of the constructs. Scale on the ruler = 500 μm. (b): Toluidine blue staining. Scale bars = 1 mm. (c): GAG accumulation examined by Alcian blue binding assay. Data are expressed as mean ± standard deviation. Statistical significance was evaluated using Dunnett's test. *p < 0.05 vs. the direct group.
4. Discussion
Several studies have reported that 3D culture of chondrocytes promotes cartilage regeneration after transplantation. Because dedifferentiated chondrocytes recover their original properties (redifferentiation) when cultured with scaffolds, it seems plausible that maturation of engineered constructs during 3D culture prior to transplantation determined the degree of subsequent cartilage regeneration. Moretti et al. [19] compared their differentiation medium containing TGF-β1, insulin, and l-ascorbic acid with proliferation medium consisting of TGF-β1, FGF-2, and PDGF in 3D culture. They concluded that only their differentiation medium elicited efficient chondrogenic development of engineered cartilage.
On the other hand, the present study showed that the proliferation medium used in 3D culture of constructs affect more positively on the cartilage regeneration after transplantation than the differentiation medium (Fig. 3, Fig. 4). The differentiation medium certainly contributed to the efficient maturation of an engineered construct during 3D culture, indicated by cartilage lacunae and abundant cartilage matrices consisting of GAG and type II collagen (Fig. 2). Although 3D culture with the differentiation medium was highly effective for redifferentiation and enhancement of stiffness in vitro, the expression of type II collagen was relatively low in vivo afterwards. On the other hand, in the proliferation medium, there was abundant deposition of type II collagen as well as GAG accumulation after transplantation despite the low degree of differentiation and stiffness during 3D culture. Cartilage constructs cultured in proliferation medium also showed better GAG accumulation in the beagle autologous transplantation model (Fig. 6c). However, areas positive for TB staining were limited to the superficial regions even in the proliferation group (Fig. 6b). This insufficient cartilage formation may partly be due to the choice of scaffold. There are few reports for the combination of scaffold and canine auricular chondrocytes for cartilage regeneration, in which cells loaded to polymer-based scaffold showed limited cartilage formation [36,38,39]. To confirm the advantages of the proliferation medium in this model, appropriate choice of scaffold must be established.
Considering the mechanism by which proliferation medium promote cartilage regeneration, it is possible that increased cell number directly affected the matrix deposition. This hypothesis may be partly true in the setting of low or middle cell concentration in which cell number was largely different between proliferation group and differentiation group (Fig. 1). On the other hand, at high cell concentration, the cell number at the end of preculture was quite similar between both groups, suggesting that there were other factors which caused the difference in chondrogenesis between those groups (Fig. 1). As shown in Fig. 5, proliferation medium contributed the reduction of MMP13, albeit not significantly, and apoptosis of chondrocytes. MMP13 is involved in the pathogenesis of osteoarthritis by degrading cartilage tissues [40]. Apoptosis of chondrocytes not only decreases the number of cells which otherwise are able to contribute to matrix production, but also induces inflammatory reaction. Dead cells induce inflammation by stimulating phagocytes through the secretion of endogenous inflammatory materials called damage-associated molecular patterns (DAMPs) [[41], [42], [43]] and high-mobility group box 1 protein (HMGB1) [44,45]. It is possible that the proliferation medium promotes cartilage regeneration by maintaining cell viability. To test this hypothesis, the effects of prevention of apoptosis on cartilage regeneration must be examined. In addition, contribution of other factors on the promotion of chondrogenesis by proliferation medium must be considered. For example, an immature engineered construct allows chondrocytes to proliferate and soluble chondrogenic factors to penetrate inside.
This contradiction between a previous report and the present study might arise from the differences in cell source (articular cartilage and auricular cartilage), scaffolds (nonwoven meshes of hyaluronic acid and atelocollagen) or culture media. IGF-1 is reported to be as a potent chondrogenic factor as TGF-β [26]. These 2 factors may promote chondrogenesis of mesenchymal stem cells independently, while crosstalk of these factors was suggested by other reports [26,46]. In addition, the effects of IGF-1 and TGF-β on chondrocytes are affected differently by several factors such as condition of cells or environmental oxygen saturation [29,47].
The results obtained by the present study raised a question on the hypothesis that 3D preculture promotes cartilage regeneration via maturation of constructs. One of the other hypotheses is that the sensitivity of encapsulated chondrocytes against chondrogenic stimuli was increased through 3D culture. The chondrocytes that fell into a susceptible state in a 3D environment would easily undergo redifferentiation stimulated by the host tissues with growth factors [48,49], matrix signals [[50], [51], [52]], or host-donor cellular interactions [53,54] and eventually promote cartilage regeneration after transplantation. If this hypothesis is true, chondrogenesis after transplantation of 3D-cultured constructs will be largely affected by transplanted sites. The results of this study, in which constructs were transplanted subcutaneously, may not be applicable for the treatment of defects in articular cartilages.
Recognizing the contradiction between the previous studies in which primary emphasis was devoted to differentiation and our present study that places high importance on proliferation, further studies are needed to investigate the changes in engineered cartilage constructs during 3D culture in more detail and to determine the most suitable 3D culture condition. To attain this objective, we should refine not only the 3D culture method but also the materials such as gel or scaffolds and culture techniques, which will all lead to the improvement of cartilage regeneration.
5. Conclusions
In this study, we found that cartilage regeneration was largely affected by the composition of 3D culture media. We conclude that it is important to maintain high cell viability, rather than promote chondrogenesis during 3D culture, because the viability of 3D-cultured chondrocytes would be a key factor that determines the sensitivity to chondrogenic stimuli and the cartilage-forming potential in subsequent transplantation.
Declaration of Competing Interest
Atsuhiko Hikita and Yukiyo Asawa: Affiliation with an endowed chair from FUJISOFT INCORPORATED.
Acknowledgements
This study was supported in part by Research Center Network for Realization of Regenerative Medicine from Japan Science and Technology Agency (JST) and Japan Agency for Medical Research and Development (AMED).
Footnotes
Peer review under responsibility of the Japanese Society for Regenerative Medicine.
References
- 1.Brittberg M., Lindahl A., Nilsson A., Ohlsson C., Isaksson O., Peterson L. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med. 1994;331(14):889–895. doi: 10.1056/NEJM199410063311401. [DOI] [PubMed] [Google Scholar]
- 2.Pareek A., Carey J.L., Reardon P.J., Peterson L., Stuart M.J., Krych A.J. Long-Term outcomes after autologous chondrocyte implantation: a systematic review at mean follow-up of 11.4 years. Cartilage. 2016;7(4):298–308. doi: 10.1177/1947603516630786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DiBartola A.C., Wright B.M., Magnussen R.A., Flanigan D.C. Clinical outcomes after autologous chondrocyte implantation in adolescents' knees: a systematic review. Arthroscopy. 2016;32(9):1905–1916. doi: 10.1016/j.arthro.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 4.von der Mark K., Gauss V., von der Mark H., Müller P. Relationship between cell shape and type of collagen synthesised as chondrocytes lose their cartilage phenotype in culture. Nature. 1977;267(5611):531–532. doi: 10.1038/267531a0. [DOI] [PubMed] [Google Scholar]
- 5.Darling E.M., Athanasiou K.A. Rapid phenotypic changes in passaged articular chondrocyte subpopulations. J Orthop Res. 2005;23(2):425–432. doi: 10.1016/j.orthres.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Benya P.D., Shaffer J.D. Dedifferentiated chondrocytes reexpress the differentiated collagen phenotype when cultured in agarose gels. Cell. 1982;30(1):215–224. doi: 10.1016/0092-8674(82)90027-7. [DOI] [PubMed] [Google Scholar]
- 7.Kimura T., Yasui N., Ohsawa S., Ono K. Chondrocytes embedded in collagen gels maintain cartilage phenotype during long-term cultures. Clin Orthop Relat Res. 1984;(186):231–239. [PubMed] [Google Scholar]
- 8.Bonaventure J., Kadhom N., Cohen-Solal L., Ng K.H., Bourguignon J., Lasselin C. Reexpression of cartilage-specific genes by dedifferentiated human articular chondrocytes cultured in alginate beads. Exp Cell Res. 1994;212(1):97–104. doi: 10.1006/excr.1994.1123. [DOI] [PubMed] [Google Scholar]
- 9.Girotto D., Urbani S., Brun P., Renier D., Barbucci R., Abatangelo G. Tissue-specific gene expression in chondrocytes grown on three-dimensional hyaluronic acid scaffolds. Biomaterials. 2003;24(19):3265–3275. doi: 10.1016/s0142-9612(03)00160-1. [DOI] [PubMed] [Google Scholar]
- 10.Uchio Y., Ochi M., Matsusaki M., Kurioka H., Katsube K. Human chondrocyte proliferation and matrix synthesis cultured in Atelocollagen gel. J Biomed Mater Res. 2000;50(2):138–143. doi: 10.1002/(sici)1097-4636(200005)50:2<138::aid-jbm7>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 11.Chiu L.L.Y., Weber J.F., Waldman S.D. Engineering of scaffold-free tri-layered auricular tissues for external ear reconstruction. Laryngoscope. 2019;129(8):E272–E283. doi: 10.1002/lary.27823. [DOI] [PubMed] [Google Scholar]
- 12.Ball S.T., Goomer R.S., Ostrander R.V., Tontz W.L., Williams S.K., Amiel D. Preincubation of tissue engineered constructs enhances donor cell retention. Clin Orthop Relat Res. 2004;420:276–285. doi: 10.1097/00003086-200403000-00039. [DOI] [PubMed] [Google Scholar]
- 13.Deponti D., Di Giancamillo A., Mangiavini L., Pozzi A., Fraschini G., Sosio C. Fibrin-based model for cartilage regeneration: tissue maturation from in vitro to in vivo. Tissue Eng A. 2012;18(11–12):1109–1122. doi: 10.1089/ten.TEA.2011.0272. [DOI] [PubMed] [Google Scholar]
- 14.Ochi M., Uchio Y., Tobita M., Kuriwaka M. Current concepts in tissue engineering technique for repair of cartilage defect. Artif Organs. 2001;25(3):172–179. doi: 10.1046/j.1525-1594.2001.025003172.x. [DOI] [PubMed] [Google Scholar]
- 15.Ochi M., Uchio Y., Kawasaki K., Wakitani S., Iwasa J. Transplantation of cartilage-like tissue made by tissue engineering in the treatment of cartilage defects of the knee. J Bone Jt Surg Br. 2002;84(4):571–578. doi: 10.1302/0301-620x.84b4.11947. [DOI] [PubMed] [Google Scholar]
- 16.Tohyama H., Yasuda K., Minami A., Majima T., Iwasaki N., Muneta T. Atelocollagen-associated autologous chondrocyte implantation for the repair of chondral defects of the knee: a prospective multicenter clinical trial in Japan. J Orthop Sci. 2009;14(5):579–588. doi: 10.1007/s00776-009-1384-1. [DOI] [PubMed] [Google Scholar]
- 17.Adachi N., Ochi M., Deie M., Nakamae A., Kamei G., Uchio Y. Implantation of tissue-engineered cartilage-like tissue for the treatment for full-thickness cartilage defects of the knee. Knee Surg Sport Traumatol Arthrosc. 2014;22(6):1241–1248. doi: 10.1007/s00167-013-2521-0. [DOI] [PubMed] [Google Scholar]
- 18.Katsube K., Ochi M., Uchio Y., Maniwa S., Matsusaki M., Tobita M. Repair of articular cartilage defects with cultured chondrocytes in Atelocollagen gel. Comparison with cultured chondrocytes in suspension. Arch Orthop Trauma Surg. 2000;120(3–4):121–127. doi: 10.1007/pl00021232. [DOI] [PubMed] [Google Scholar]
- 19.Moretti M., Wendt D., Dickinson S.C., Sims T.J., Hollander A.P., Kelly D.J. Effects of in vitro preculture on in vivo development of human engineered cartilage in an ectopic model. Tissue Eng. 2005;11(9–10):1421–1428. doi: 10.1089/ten.2005.11.1421. [DOI] [PubMed] [Google Scholar]
- 20.Miot S., Brehm W., Dickinson S., Sims T., Wixmerten A., Longinotti C. Influence of in vitro maturation of engineered cartilage on the outcome of osteochondral repair in a goat model. Eur Cells Mater. 2012;23:222–236. doi: 10.22203/ecm.v023a17. [DOI] [PubMed] [Google Scholar]
- 21.Bichara D.A., Pomerantseva I., Zhao X., Zhou L., Kulig K.M., Tseng A. Successful creation of tissue-engineered autologous auricular cartilage in an immunocompetent large animal model. Tissue Eng A. 2014;20(1–2):303–312. doi: 10.1089/ten.TEA.2013.0150. [DOI] [PubMed] [Google Scholar]
- 22.Liu Y., Li D., Yin Z., Luo X., Liu W., Zhang W. Prolonged in vitro precultivation alleviates post-implantation inflammation and promotes stable subcutaneous cartilage formation in a goat model. Biomed Mater. 2016;12(1) doi: 10.1088/1748-605X/12/1/015006. [DOI] [PubMed] [Google Scholar]
- 23.Pomerantseva I., Bichara D.A., Tseng A., Cronce M.J., Cervantes T.M., Kimura A.M. Ear-shaped stable Auricular cartilage engineered from extensively expanded chondrocytes in an immunocompetent experimental animal model. Tissue Eng A. 2016;22(3–4):197–207. doi: 10.1089/ten.tea.2015.0173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jakob M., Démarteau O., Schäfer D., Hintermann B., Dick W., Heberer M. Specific growth factors during the expansion and redifferentiation of adult human articular chondrocytes enhance chondrogenesis and cartilaginous tissue formation in vitro. J Cell Biochem. 2001;81(2):368–377. doi: 10.1002/1097-4644(20010501)81:2<368::aid-jcb1051>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 25.Chaipinyo K., Oakes B.W., van Damme M.P. Effects of growth factors on cell proliferation and matrix synthesis of low-density, primary bovine chondrocytes cultured in collagen I gels. J Orthop Res. 2002;20(5):1070–1078. doi: 10.1016/S0736-0266(02)00025-6. [DOI] [PubMed] [Google Scholar]
- 26.Longobardi L., O'Rear L., Aakula S., Johnstone B., Shimer K., Chytil A. Effect of IGF-I in the chondrogenesis of bone marrow mesenchymal stem cells in the presence or absence of TGF-beta signaling. J Bone Miner Res. 2006;21(4):626–636. doi: 10.1359/jbmr.051213. [DOI] [PubMed] [Google Scholar]
- 27.McQuillan D.J., Handley C.J., Campbell M.A., Bolis S., Milway V.E., Herington A.C. Stimulation of proteoglycan biosynthesis by serum and insulin-like growth factor-I in cultured bovine articular cartilage. Biochem J. 1986;240(2):423–430. doi: 10.1042/bj2400423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tyler J.A. Insulin-like growth factor 1 can decrease degradation and promote synthesis of proteoglycan in cartilage exposed to cytokines. Biochem J. 1989;260(2):543–548. doi: 10.1042/bj2600543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rosa R.G., Joazeiro P.P., Bianco J., Kunz M., Weber J.F., Waldman S.D. Growth factor stimulation improves the structure and properties of scaffold-free engineered auricular cartilage constructs. PLoS One. 2014;9(8) doi: 10.1371/journal.pone.0105170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Loeser R.F., Shanker G. Autocrine stimulation by insulin-like growth factor 1 and insulin-like growth factor 2 mediates chondrocyte survival in vitro. Arthritis Rheum. 2000;43(7):1552–1559. doi: 10.1002/1529-0131(200007)43:7<1552::AID-ANR20>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 31.Shakibaei M., Seifarth C., John T., Rahmanzadeh M., Mobasheri A. Igf-I extends the chondrogenic potential of human articular chondrocytes in vitro: molecular association between Sox9 and Erk1/2. Biochem Pharmacol. 2006;72(11):1382–1395. doi: 10.1016/j.bcp.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 32.Guenther H.L., Guenther H.E., Froesch E.R., Fleisch H. Effect of insulin-like growth factor on collagen and glycosaminoglycan synthesis by rabbit articular chondrocytes in culture. Experientia. 1982;38(8):979–981. doi: 10.1007/BF01953688. [DOI] [PubMed] [Google Scholar]
- 33.Mounts T., Ginley N., Schluchter M., Dennis J.E. Optimization of the expansion and differentiation of rabbit chondrocytes in vitro. Cartilage. 2012;3(2):181–187. doi: 10.1177/1947603511420999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Takahashi T., Ogasawara T., Kishimoto J., Liu G., Asato H., Nakatsuka T. Synergistic effects of FGF-2 with insulin or IGF-I on the proliferation of human auricular chondrocytes. Cell Transplant. 2005;14(9):683–693. doi: 10.3727/000000005783982675. [DOI] [PubMed] [Google Scholar]
- 35.Asawa Y., Ogasawara T., Takahashi T., Yamaoka H., Nishizawa S., Matsudaira K. Aptitude of auricular and nasoseptal chondrocytes cultured under a monolayer or three-dimensional condition for cartilage tissue engineering. Tissue Eng A. 2009;15(5):1109–1118. doi: 10.1089/ten.tea.2007.0218. [DOI] [PubMed] [Google Scholar]
- 36.Asawa Y., Sakamoto T., Komura M., Watanabe M., Nishizawa S., Takazawa Y. Early stage foreign body reaction against biodegradable polymer scaffolds affects tissue regeneration during the autologous transplantation of tissue-engineered cartilage in the canine model. Cell Transplant. 2012;21(7):1431–1442. doi: 10.3727/096368912X640574. [DOI] [PubMed] [Google Scholar]
- 37.Yamaoka H., Asato H., Ogasawara T., Nishizawa S., Takahashi T., Nakatsuka T. Cartilage tissue engineering using human auricular chondrocytes embedded in different hydrogel materials. J Biomed Mater Res A. 2006;78(1):1–11. doi: 10.1002/jbm.a.30655. [DOI] [PubMed] [Google Scholar]
- 38.Morotomi T., Wada M., Uehara M., Enjo M., Isogai N. Effect of local environment, fibrin, and basic fibroblast growth factor incorporation on a canine autologous model of bioengineered cartilage tissue. Cells Tissues Organs. 2012;196(5):398–410. doi: 10.1159/000336029. [DOI] [PubMed] [Google Scholar]
- 39.Enjo M., Terada S., Uehara M., Itani Y., Isogai N. Usefulness of polyglycolic acid-polypropylene composite scaffolds for three-dimensional cartilage regeneration in a large-animal autograft model. Plast Reconstr Surg. 2013;131(3) doi: 10.1097/PRS.0b013e31827c6dd8. 335e-42e. [DOI] [PubMed] [Google Scholar]
- 40.Li H., Wang D., Yuan Y., Min J. New insights on the MMP-13 regulatory network in the pathogenesis of early osteoarthritis. Arthritis Res Ther. 2017;19(1):248. doi: 10.1186/s13075-017-1454-2. Epub 2017/11/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Seong S.Y., Matzinger P. Hydrophobicity: an ancient damage-associated molecular pattern that initiates innate immune responses. Nat Rev Immunol. 2004;4(6):469–478. doi: 10.1038/nri1372. [DOI] [PubMed] [Google Scholar]
- 42.Kono H., Rock K.L. How dying cells alert the immune system to danger. Nat Rev Immunol. 2008;8(4):279–289. doi: 10.1038/nri2215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Krysko D.V., Agostinis P., Krysko O., Garg A.D., Bachert C., Lambrecht B.N. Emerging role of damage-associated molecular patterns derived from mitochondria in inflammation. Trends Immunol. 2011;32(4):157–164. doi: 10.1016/j.it.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 44.Andersson U., Wang H., Palmblad K., Aveberger A.C., Bloom O., Erlandsson-Harris H. High mobility group 1 protein (HMG-1) stimulates proinflammatory cytokine synthesis in human monocytes. J Exp Med. 2000;192(4):565–570. doi: 10.1084/jem.192.4.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Klune J.R., Dhupar R., Cardinal J., Billiar T.R., Tsung A. HMGB1: endogenous danger signaling. Mol Med. 2008;14(7–8):476–484. doi: 10.2119/2008-00034.Klune. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Horita M., Nishida K., Hasei J., Furumatsu T., Sakurai M., Onodera Y. Involvement of ADAM12 in chondrocyte differentiation by regulation of TGF-β1-induced IGF-1 and RUNX-2 expressions. Calcif Tissue Int. 2019;105(1):97–106. doi: 10.1007/s00223-019-00549-6. [DOI] [PubMed] [Google Scholar]
- 47.Jonitz A., Lochner K., Tischer T., Hansmann D., Bader R. TGF-β1 and IGF-1 influence the re-differentiation capacity of human chondrocytes in 3D pellet cultures in relation to different oxygen concentrations. Int J Mol Med. 2012;30(3):666–672. doi: 10.3892/ijmm.2012.1042. [DOI] [PubMed] [Google Scholar]
- 48.Goldring M.B., Tsuchimochi K., Ijiri K. The control of chondrogenesis. J Cell Biochem. 2006;97(1):33–44. doi: 10.1002/jcb.20652. [DOI] [PubMed] [Google Scholar]
- 49.Wuelling M., Vortkamp A. Chondrocyte proliferation and differentiation. Endocr Dev. 2011;21:1–11. doi: 10.1159/000328081. [DOI] [PubMed] [Google Scholar]
- 50.Kozhemyakina E., Lassar A.B., Zelzer E. A pathway to bone: signaling molecules and transcription factors involved in chondrocyte development and maturation. Development. 2015;142(5):817–831. doi: 10.1242/dev.105536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li J., Dong S. The signaling pathways involved in chondrocyte differentiation and hypertrophic differentiation. Stem Cell Int. 2016;2016:2470351. doi: 10.1155/2016/2470351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lefebvre V., Dvir-Ginzberg M. SOX9 and the many facets of its regulation in the chondrocyte lineage. Connect Tissue Res. 2017;58(1):2–14. doi: 10.1080/03008207.2016.1183667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tavella S., Raffo P., Tacchetti C., Cancedda R., Castagnola P. N-CAM and N-cadherin expression during in vitro chondrogenesis. Exp Cell Res. 1994;215(2):354–362. doi: 10.1006/excr.1994.1352. [DOI] [PubMed] [Google Scholar]
- 54.Cao B., Li Z., Peng R., Ding J. Effects of cell-cell contact and oxygen tension on chondrogenic differentiation of stem cells. Biomaterials. 2015;64:21–32. doi: 10.1016/j.biomaterials.2015.06.018. [DOI] [PubMed] [Google Scholar]