Abstract
Background
Nonalcoholic fatty-liver disease (NAFLD) is the most common cause of chronic liver disease worldwide. Although NAFLD has been studied extensively, potential risk factors for NAFLD among chronic hepatitis B (CHB) patients and their comparison with healthy individuals have remained understudied in Iran. As such, we examined the association between HBV infection and the development of NAFLD in two groups.
Methods
A case–control study was done on 376 CHB patients and 447 healthy subjects randomly selected from Birjand, South Khorasan province, Iran. We used logistic regression to estimate adjusted ORs with 95% CIs for incidence of NAFLD. Potential risk factors for NAFLD were evaluated while adjusting for age, sex, marital status, and educational level. Also, χ2 was used to compare demographic characteristics between the two groups.
Results
A total of 373 CHB patients (mean age 40.1±12.9 years) versus 447 individuals in the control group (mean age 39.8±13.9 years) were included in this study (p=0.337). Liver characteristics were found to be significantly different in CHB and healthy groups (p<0.05). According to the results obtained from logistic regression, the adjusted OR (95% CI) for NAFLD incidence of comparing HBsAg-positive to HBsAg-negative participants was 0.62 (0.45–0.84).
Conclusion
The results suggested that HBsAg seropositivity was associated with lower risk of developing NAFLD. This study also revealed that mild cases of fatty liver in carriers of hepatitis B are more common than in healthy subjects. However, moderate and severe cases of this condition are more common in healthy people than in hepatitis B carriers.
Keywords: NAFLD, metabolic syndrome, liver diseases, hepatitis B
Introduction
Viral hepatitis ie, inflammation of the liver caused by specific viruses, such as hepatitis B (HBV), targets the liver cells and can result in death, mostly due to cirrhosis and hepatocellular carcinoma.1 In 2015, 887,000 persons died from these complications, as reported by the World Health Organization.2 This potentially harmful liver disease is more common in developing countries, such as Iran, although its endemicity in Iran is low among Middle East countries. Sociocultural and economic status are two major factors influencing the prevalence of HBV.3 Nonalcoholic fatty liver disease (NAFLD), which refers to hepatic steatosis not associated with significant alcohol intake, is the most prevalent chronic liver disease worldwide.4 NAFLD ranges from simple steatosis to steatosis plus necroinflammation with or without fibrosis.5,6
Several studies have revealed that steatosis (such as NAFLD) and chronic viral hepatitis (including chronic HBV [CHB]) have a synergistic effect on aggravating liver injury through oxidative damage, so their coincidence could promote hepatic fibrosis and hepatocellular carcinoma.7,9 On the other hand, according to various previous studies, NAFLD is strongly associated with obesity, type 2 diabetes, and metabolic syndrome,10,12 especially when in combination with CHB.13,16 There have been several investigations reporting the prevalence of NAFLD in the general population,11,17,18 but no comprehensive study conducted on both CHB patients and healthy people in order to make a comparison.
Methods
In this case–control study, from all confirmed CHB patients who were under observation at all hepatitis clinics located in Birjand, South Khorasan, Iran in 2013–2014, 376 persons were included after signing written consent for participation. In the current study, CHB was defined as being HBsAg-positive for >6 months. A total of 447 healthy persons from another Birjand study3 were also selected (equal sex-distribution ratio). Experienced technicians performed blood sampling and data collection. Venous blood (8 mL) was collected from each subject. Specimens were stored at −30°C until collection of all the samples. Detection of the HBV core antibody (BioELISA anti-HBc; Biokit, Barcelona, Spain) in the serum samples was done using a commercially available kit. Subjects whose results for this detection were negative were considered healthy, so our healthy samples were selected randomly from this collection.
These two groups had been stratified for age and sex. In another Birjand study, two teams composed of well-educated health-care workers invited people to undergo serologic tests for HBV after explaining the aims and scopes of the research and the necessity for awareness about HBV and liver-function status to prevent irreversible poor outcomes. Afterward, a questionnaire consisting of demographic data (ie, age, sex, level of education, history of FLD and its grade if known) was completed for each volunteer. Then, 5 mL whole blood was taken from each person and referred to a laboratory to determine aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels. Among the healthy subjects from that study, 447 were selected by table of random numbers.
Inclusion criteria for both groups were full agreement for participation and negative history of treatment for FLD. People who were diabetic (on treatment or not) and those who had a history of steroid, phenytoin, or tetracycline consumption (as these can induce fatty liver) were excluded. Laboratory investigations for diabetes were applied for all participants in both groups where confirmed diabetic patients were excluded. Serologic tests for HBV (ie, HBsAg, HBcAb, and HBsAb) were applied for control-group individuals to ensure absence of hepatitis. Additionally, serologic testing with ELISA for hepatitis C and HIV was done for all participants. Individuals coinfected with hepatitis C or HIV and those consuming alcohol regularly were also excluded.
An expert sonologist performed all liver sonography to detect evidence of fatty-liver changes. All participants in both groups underwent these tests. Fatty liver was categorized into three principal classes: mild, moderate, and severe. In mild fatty-liver subjects, liver echo was raised in contrast to kidney-cortex echo; in moderate fatty-liver cases, portal vein echogenic branches were absent; and finally for the severe form of fatty liver, detection was made based on loss of definition of the diaphragm.18
Ethical Considerations
The study was approved by the ethics and scientific committees of Birjand University of Medical Sciences (registration Ir.bums.REC.1394.379). This work was conducted in accordance with the Declaration of Helsinki (2013). Written informed consent was obtained from all participants, and data sheets were coded to ensure confidentiality.
Statistical Analyses
Descriptive statistics are used to summarize the characteristics of the study participants according to the presence of HBsAg in the two groups. Incidence rate in each group was calculated as the number of cases divided by persons at follow‐up. We used multiple logistic regression to determine risk factors associated with NAFLD, and χ2 was also used to determine relationships between demographic and clinical characteristics. Mann–Whitney U tests were applied to compare ALT and AST levels between CHB and healthy groups. We estimated adjusted ORs with 95% CI for incidence of NAFLD. We also performed adjustment for age and sex, as well as for marital status and educational level. All statistical tests and analyses were done in SPSS version 21. All p-values were two‐tailed and p<0.05 was considered statistically significant.
Results
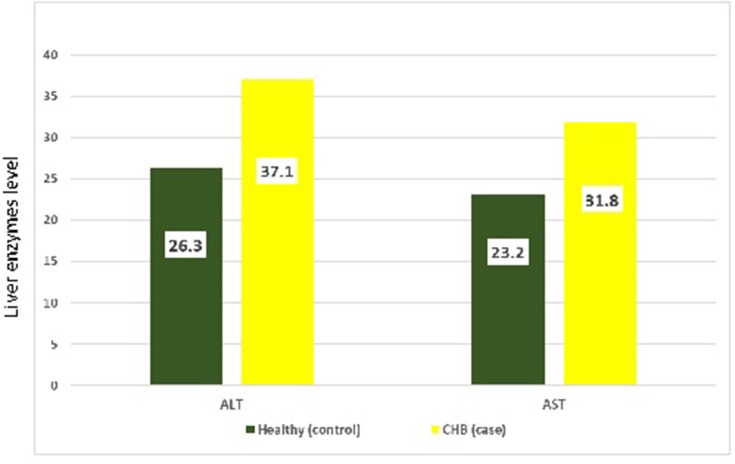
A total of 373 patients in the CHB group (mean age 41.1± 12.9 years) participated in the study and 447 subjects in the control group (mean age 39.8±13.9 years; p=0.34). Most study participants were 31–49 years of age. Mean ALT and AST levels for CHB (case) and healthy (control) groups are presented in Figure 1. Frequency distribution of demographic characteristics among the groups is reported in Table 1. Homogeneity of sex and age was observed in the both groups (p>0.05). Participants in both groups were mostly educated at least up to high school, and the majority of participants were married (79.6% and 85.9% in CHB and healthy groups, respectively). Means ± SD of ALT were 37.1±36.8 and 37.1±36.8) andof AST 31.8±26.9 and 23.2±23.1 in the CHB and control groups, respectively. A significant difference was observed on Mann–Whitney U test (p<0.001). Figure 1 shows the mean ALT and AST levels for the CHB (case) and healthy (control) groups. Demographic data for each group are listed in Table 1. Table 2 compares liver status in the CHB and healthy groups.
Figure 1.
Mean levels of ALT and AST between CHB and healthy groups.
Abbreviations: CHB, chronic hepatitis B; AST, aspartate aminotransferase; ALT, alanine aminotransferase.
Table 1.
Frequency Distribution For CHB And Healthy Groups
| Variable | Healthy (447) | CHB (376) | p-value | |
|---|---|---|---|---|
| Age (years) | 30 and less | 136 (30.4%) | 90 (24.1%) | 0.11 |
| 31–49 | 199 (44.5%) | 190 (50.4%) | ||
| 50 and more | 112 (25.1%) | 96 (25.5%) | ||
| Sex | Male | 233 (52.1%) | 187 (49.6%) | 0.47 |
| Female | 214 (47.9%) | 189 (50.4%) | ||
| Education | Illiterate | 33 (7.7%) | 67 (18%) | 0.03 |
| Elementary | 74 (17.3%) | 80 (21.3%) | ||
| Intermediate | 35 (8.2%) | 27 (6.6%) | ||
| High school | 147 (34.4%) | 135 (36.1%) | ||
| Academic | 138 (32.3%) | 67 (18%) | ||
| Marital status | Single | 84 (18.8%) | 43 (11.4%) | 0.005 |
| Married | 356 (79.6%) | 325 (87.3%) | ||
| Divorced or widowed | 7 (1.6%) | 8 (1.4%) |
Notes: Data presented as n (%). Bold values indicate significance.
In multiple logistic regression analyses (Table 3), an association between NAFLD incidence and HBsAg was consistently observed to be higher across prespecified subgroups (age 30–50 vs <30 years), with corresponding ORs of 5.64 (95% CI 3.5–9.1) and 8.5 (95% CI 5.01–14.41) obtained for subjects aged >50 years. We did not observe any significantly higher risk in terms of sex (OR=1.14, 95% CI 0.97–1.81). On the other hand, the correlation of NAFLD incidence was significantly stronger in married subjects against single cases (OR 1.68, 95% CI 1.09–2.60; p<0.05). HBsAg‐positive subjects had lower NAFLD incidence. In models adjusted for age, sex, and marital status, comparison subjects with positive HBsAg to those with negative HBsAg gave an OR (95% CI) for NAFLD incidence of 0.62 (0.455–0.845). The association between HBV infection and NAFLD incidence persisted, denoting that the association is mediated by metabolic parameters up to a certain level.
Table 3.
Results Of Multiple Logistic Regression For NAFLD
| Variable | OR | 95% CI | Wald | p-value | |
|---|---|---|---|---|---|
| Age (years) | 30 and less | 1 | — | — | — |
| 31–49 | 5.649 | 3.50–9.1 | 50.69 | <0.001 | |
| 50 and more | 8.505 | 5.01–14.41 | 63.24 | <0.001 | |
| Sex | Male | 1 | — | — | — |
| Female | 1.14 | 0.975–1.812 | 3.246 | 0.072 | |
| Marital status | Single | 1 | — | — | —– |
| Married | 1.68 | 1.09–2.60 | 5.50 | 0.019 | |
| HBsAg | Negative | 1 | — | — | —– |
| Positive | 0.62 | 0.455–0.8450 | 9.162 | 0.002 |
Note: Bold values indicate statistical significance.
Discussion
HBV infection, which can result in hepatocellular carcinoma and cirrhosis, is now a major cause of chronic liver disease worldwide.19 Meanwhile, NAFLD, which includes steatosis with or without necroinflammation, has emerged as another major and common cause of liver injury in the general population. As it can result in hepatocellular carcinoma, cirrhosis, and liver failure,9 it is one of the most targeted liver disorders for prevention and treatment. Researchers have concluded that host factors including metabolic syndrome provide conditions for developing fatty liver and steatohepatitis in patients with CHB,16 and liver fibrosis may be more frequent in this situation.20 Others have concluded that fatty liver in combination with HBV infection can induce and aggravate liver damage.21
In this regard, as with other researchers, such as Rastogi et al7 and Alavian et al,10 we decided to focus on the prevalence of NAFLD in CHB patients and investigate different parameters, such as age, sex, and marital status and their possible correlation with this situation. Further, we aimed to assess the presence of fatty liver across a healthy population (HBsAg-negative) and evaluate whether HBsAg positivity would be a risk factor for developing NAFLD. In this study, fatty liver was classified into three main categories; mild, moderate, and severe, as with some previous reports.18
In this large-sample case–control study of people in Birjand, HBV infection was significantly correlated with a lower risk of NAFLD occurrence. Notably, this association remained significant even after adjustment for possible confounders. To the best of the authors’ knowledge, this research is the first case–control study to indicate an inverse relationship between HBV infection and NAFLD incidence as a metabolic syndrome in Iran. Previous researchers have surveyed a dependence between HBV infection and NAFLD, with inconsistent results. Some studies have stated that the outbreak of fatty liver established using ultrasound was comparable between healthy controls and HBV-infected patients.22–25 Also, a cross-sectional study suggested that chronic HBV infection was significantly associated with a lower risk of fatty liver.26 Further, a large survey in Taiwan showed an inverse association between FLD and HBV infection.27
In the current study, we found a significant relationship between fatty liver and HBV infection (p=0.002). Specifically, the risk of developing fatty liver in HBsAg-positive individuals was 38% lower than for healthy subjects. This finding suggests that chronic HBV infection was inversely associated with fatty liver. This finding is consistent with the findings of previously published studies.11,28,29 In contrast to all studies mentioned and our study, Lin et al and Kuo et al concluded that interactions of HBV infection and NAFLD is not conclusive yet.25,30 The opposite dependence between HBV infection and incident NAFLD persisted even after adjustment for possible confounders, such as age, sex, and marital status, implying that HBV may play a protective role in the progress of NAFLD. The mechanism by which HBV affects steatosis is not well known. Several studies have suggested an inverse relationship between HBV infection and lipid profile, such as cholesterol, triglycerides, LDL-C, and HDL-C.31,32
The other finding in this study was a significant rise in hepatic fatty liver (mild) in HBV carriers compared to healthy subjects. In contrast, moderate (grade 2) and severe (grade 3) hepatic fatty liver was found to be higher in healthy subjects than among HBV carriers. This can be attributed to the early detection of fatty liver in the early stages of HBV carriers in their ultrasound examinations and periodic checkups. However, healthy subjects may refer less oftrn for periodic checkups or their condition might be diagnosed at a higher stage of fatty liver. According to the results of Table 1, frequency distributions of age and sex among CHB and healthy groups were homogeneous (p>0.05). However, frequency distributions of educational levels and marital status were different for the two groups (p<0.05).
Further, according to the results obtained from Table 2, fatty-liver status in the CHB and healthy groups was significantly different, such that the prevalence of fatty liver in the control group was higher than the CHB group (44.3% versus 36.8%). Table 3 indicates that several factors, such as age and marital status, have a significant influence on developing FLD. The odds of NAFLD among individuals aged >50 years and 31–49 years were 8.505 and 5.649 times those of 30-year-old adults and younger. Also, the risk of NAFLD was 68% greater in married people than the risk in their single counterparts (p=0.019). Possible reasons for this difference should be evaluated in future. Results obtained for age were compatible with some others, indicating that age, ethnicity, and endocrine disorders (eg, hypothyroidism, hypogonadism, and polycystic ovarian syndrome) are associated with NAFLD.5,6,23,33
Table 2.
Frequency Distribution Of Status Of Liver In CHB And Healthy Groups
| Variable | Healthy (447) | CHB (376) | p-value | |
|---|---|---|---|---|
| Presence of fatty liver | Yes | 198 (44.3%) | 138 (36.8%) | 0.03 |
| No | 249 (55.7%) | 238 (63.2%) | ||
| Grade of fatty liver | No | 249 (55.7%) | 238 (63.2%) | <0.001 |
| Mild | 15 (3.4%) | 29 (7.8%) | ||
| Moderate | 177 (39.6%) | 106 (28.5%) | ||
| Severe | 6 (1.3%) | 2 (0.5%) |
Notes: Data presented as n (%). Bold values indicate statistical significance.
Among studies conducted within Iran, Moghaddasifar et al found hypertension, high serum ALT, metabolic syndrome, advanced age, diabetes, male sex, and hypertriglyceridemia were determinants of NAFLD. They also reported high incidence of this disease in Iran.6 Alavian et al found strong relationships between NAFLD and sex, occupation, cigarette smoking, and family history of liver diseases, as well as hemoglobin, AST, ALT, triglyceride, and bilirubin levels.10 Our study did not find sex to be a significant risk factor for NAFLD, but we found older individuals (>30 and especially >50 years) to be at significantly higher risk of developing this disorder (p<0.05). Additionally, we found educational status to be a strong risk factor for developing NAFLD, with more highly educated individuals being at significantly greater risk than illiterate subjects (p<0.05). We also observed significantly higher levels of AST and ALT when NAFLD coincided with CHB.
Conclusion
HBV infection appears to be associated with lower rates of NAFLD in this Iranian population. This study suggests that cases with mild fatty liver are more common in HBV carriers than healthy subjects, while cases with moderate and severe liver fatty liver are more common in healthy subjects than HBV carriers in this area. This can be due to the early diagnosis of fatty liver in HBV patients in their periodic tests. Therefore, it is recommended that fatty-liver checkups be done in individuals with risk factors to prevent them developing advanced fatty liver. Finally, additional research is required to better understand the mechanisms involved in the development of NAFLD in HBV patients.
Disclosure
The authors declare that no financial or any other conflicts of interest are associated with this work.
References
- 1.Ziaee M, Sharifzadeh G, Namaee MH, Fereidouni M. Prevalence of HIV and hepatitis B, C, D infections and their associated risk factors among prisoners in Southern Khorasan Province, Iran. Iran J Public Health. 2014;43(2):229. [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Viral hepatitis surveillance—United States, 2009. Atlanta: Centers for Disease Control and Prevention. 2012:1–71. Available from: https://www.cdc.gov/hepatitis/statistics/2015surveillance/pdfs/2015HepSurveillanceRpt.pdf Accessed September20, 2019.
- 3.Ziaee M, Ebrahimzadeh A, Azarkar Z, Namaei M, Saburi A. Seroprevalence and risk factors for hepatitis B in an adult population: the first report from Birjand, South Khorasan, Iran. Hepat Mon. 2016;16(9):e36452. doi: 10.5812/hepatmon.36452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Milić S, Lulić D, Štimac D. Non-alcoholic fatty liver disease and obesity: biochemical, metabolic and clinical presentations. World J Gastroenterol. 2014;20(28):9330–9337. doi: 10.3748/wjg.v20.i28.9330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Osmani F, Hajizadeh E, Mansoori P. Use of smoothing methods for estimating the coefficients of time dependent rate models in survival analysis and its application in psoriasis disease. Iran J Epidemiol. 2016;12(3):36–46. [Google Scholar]
- 6.Moghaddasifar I, Lankarani KB, Moosazadeh M, et al. Prevalence of non-alcoholic fatty liver disease and its related factors in Iran. Int J Organ Transplant Med. 2016;7(3):149–160. [PMC free article] [PubMed] [Google Scholar]
- 7.Rastogi A, Sakhuja P, Kumar A, et al. Steatosis in chronic hepatitis B: prevalence and correlation with biochemical, histologic, viral, and metabolic parameters. Indian J Pathol Microbiol. 2011;54(3):454–459. doi: 10.4103/0377-4929.85074 [DOI] [PubMed] [Google Scholar]
- 8.Powell EE, Jonsson JR, Clouston AD. Steatosis: co-factor in other liver diseases. Hepatology. 2005;42:5–13. doi: 10.1002/hep.20750 [DOI] [PubMed] [Google Scholar]
- 9.Chen Y, Fan C, Chen Y, et al. Effect of hepatic steatosis on the progression of chronic hepatitis B: a prospective cohort and in vitro study. Oncotarget. 2017;8(35):58601–58610. doi: 10.18632/oncotarget.17380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alavian SM, Ramezani M, Bazzaz A, et al. Frequency of fatty liver and some of its risk factors in asymptomatic carriers of HBV attending the Tehran blood transfusion organization hepatitis clinic. Iran J Endocrinol Metab. 2008;10(2):99–106. [Google Scholar]
- 11.Wong VW-S, Wong GL-H, Chu WC-W, et al. Hepatitis B virus infection and fatty liver in the general population. J Hepatol. 2012;56(3):533–540. doi: 10.1016/j.jhep.2011.09.013 [DOI] [PubMed] [Google Scholar]
- 12.Tsochatzis E, Papatheodoridis G, Manesis E, Chrysanthos N, Kafiri G, Archimandritis A. Hepatic steatosis in chronic hepatitis B develops due to host metabolic factors: a comparative approach with genotype 1 chronic hepatitis C. Dig Liver Dis. 2007;39(10):936–942. doi: 10.1016/j.dld.2007.07.151 [DOI] [PubMed] [Google Scholar]
- 13.Gordon A, McLean CA, Pedersen JS, Bailey MJ, Roberts SK. Hepatic steatosis in chronic hepatitis B and C: predictors, distribution and effect on fibrosis. J Hepatol. 2005;43:38–44. doi: 10.1016/j.jhep.2005.01.031 [DOI] [PubMed] [Google Scholar]
- 14.Altlparmak E, Koklu S, Yalinkilic M. Viral and host causes of fatty liver in chronic hepatitis B. World J Gastroenterol. 2005;11:3056–3059. doi: 10.3748/wjg.v11.i20.3056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomopoulos KC, Arvaniti V, Tsamantas AC, et al. Prevalence of liver steatosis in patients with chronic hepatitis B: a study of associated factors and of relationship with fibrosis. Eur J Gastroenterol Hepatol. 2006;18:233–237. doi: 10.1097/00042737-200603000-00002 [DOI] [PubMed] [Google Scholar]
- 16.Bondini S, Kallman J, Wheeler A, et al. Impact of non-alcoholic fatty liver disease on chronic hepatitis B. Liver Int. 2007;27:607. doi: 10.1111/j.1478-3231.2007.01482.x [DOI] [PubMed] [Google Scholar]
- 17.Amarapurkar D, Kamani P, Patel N, et al. Prevalence of non-alcoholic fatty liver disease: population based study. Ann Hepatol. 2007;6(3):161–163. [PubMed] [Google Scholar]
- 18.Azarkar G, Zeinali T, Sharifzadeh G, Abedi F, Hajihosseini M, Ziaee M. Prevalence of non-alcoholic fatty liver and its related factors in Birjand, during year 2015. Mod Care J. 2016;13(4):e58829. doi: 10.5812/mcj [DOI] [Google Scholar]
- 19.Ziaee M, Javanmard D, Sharifzadeh G, Namaei M, Azarkar G. Genotyping and mutation pattern in the overlapping MHR region of HBV isolates in Southern Khorasan, Eastern Iran. Hepat Mon. 2016;16(10):e37806. doi: 10.5812/hepatmon [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shi JP, Xun YH, Su YX, et al. Metabolic syndrome and severity of fibrosis in patients with chronic viral hepatitis B infection or non-alcoholic fatty liver disease. Afr J Microbiol Res. 2011;5(5):481–485. [Google Scholar]
- 21.Lin YC, Hsiao ST, Chen JD. Sonographic fatty liver and hepatitis B virus carrier status: synergistic effect on liver damage in Taiwanese adults. World J Gastroenterol. 2007;13(12):1805–1810. doi: 10.3748/wjg.v13.i12.1805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Machado MV, Cortez-Pinto H. Non-alcoholic fatty liver disease: what the clinician needs to know. World J Gastroenterol. 2014;20:12956–12980. doi: 10.3748/wjg.v20.i36.12956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Osmani F, Hajizadeh E, Rasekhi A. Association between multiple recurrent events with multivariate modeling: a retrospective cohort study. J Res Health Sci. 2018;18(4). [PMC free article] [PubMed] [Google Scholar]
- 24.Bedogni G, Nobili V, Tiribelli C. Epidemiology of fatty liver: an update. World J Gastroenterol. 2014;20:9050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lin C, Huang X, Liu H, Wang Y. Interactions of hepatitis B virus infection with nonalcoholic fatty liver disease: possible mechanisms and clinical impact. Dig Dis Sci. 2015;60(12):3513–3524. doi: 10.1007/s10620-015-3772-z [DOI] [PubMed] [Google Scholar]
- 26.Wang CC, Tseng TC, Kao JH. Hepatitis B virus infection and metabolic syndrome: fact or fiction? J Gastroenterol Hepatol. 2015;30:14–20. doi: 10.1111/jgh.12700 [DOI] [PubMed] [Google Scholar]
- 27.Wang CC, Hsu CS, Liu CJ, Kao JH, Chen DS. Association of chronic hepatitis B virus infection with insulin resistance and hepatic steatosis. J Gastroenterol Hepatol. 2008;23:779–782. doi: 10.1111/j.1440-1746.2007.05216.x [DOI] [PubMed] [Google Scholar]
- 28.Cheng YL, Wang YJ, Kao WY, et al. Inverse association between hepatitis B virus infection and fatty liver disease: a large-scale study in populations seeking for check-up. PLoS One. 2013;8:e72049. doi: 10.1371/journal.pone.0072049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chiang CH, Yang HI, Jen CL, et al. Association between obesity, hypertriglyceridemia and low hepatitis B viral load. Int J Obes (Lond). 2013;37:410–415. doi: 10.1038/ijo.2012.63 [DOI] [PubMed] [Google Scholar]
- 30.Chen JY, Wang JH, Lin CY, et al. Lower prevalence of hypercholesterolemia and hyperglyceridemia found in subjects with seropositivity for both hepatitis B and C strains independently. J Gastroenterol Hepatol. 2010;25. doi: 10.1111/j.1440-1746.2010.06300.x [DOI] [PubMed] [Google Scholar]
- 31.Razi B, Alizadeh S, Omidkhoda A, Imani D, Rezaei R. Association of chronic hepatitis B infection with metabolic syndrome and its components: meta‐analysis of observational studies. Diabetes Metab Syndr. 2017;11(Suppl 2):S939–S947. doi: 10.1016/j.dsx.2017.07.020 [DOI] [PubMed] [Google Scholar]
- 32.Kuo YH, Kee KM, Wang JH, et al. Association between chronic viral hepatitis and metabolic syndrome in southern Taiwan: a large population‐based study of 180 359 participants. Aliment Pharmacol Ther. 2018;48:993–1002. doi: 10.1111/apt.14960 [DOI] [PubMed] [Google Scholar]
- 33.Joo EJ, Chang Y, Yeom JS, Ryu S. Hepatitis B virus infection and decreased risk of nonalcoholic fatty liver disease: a cohort study. Hepatology. 2017;65(3):828. doi: 10.1002/hep.28917 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Centers for Disease Control and Prevention. Viral hepatitis surveillance—United States, 2009. Atlanta: Centers for Disease Control and Prevention. 2012:1–71. Available from: https://www.cdc.gov/hepatitis/statistics/2015surveillance/pdfs/2015HepSurveillanceRpt.pdf Accessed September20, 2019.