Abstract
Background
ABO blood groups have been suggested to have a high correlation with cardiovascular diseases (CVDs). It has also been postulated that platelet indices, including mean platelet volume (MPV) and platelet distribution width (PDW), are very important in the development and progression of CVDs. However, despite these common associations with CVDs, as far as we know, there are no studies investigating platelet indices in ABO blood groups. Thus, the aim of this study was to investigate whether platelet indices are associated with ABO blood groups.
Methods
The study included 301 healthy volunteers (99 women and 202 men; mean age: 32.59 ± 7.52 years) whose blood groups were determined by the gel column method using agglutination techniques. Platelet indices were studied by an automated blood counter.
Results
No considerable differences in age, gender, or Rh factors were observed among ABO blood groups. MPV was detected to be considerably lower in O and A blood group subjects than in AB and B blood group subjects. Similarly, PDW was significantly lower in O and A blood group subjects than in B blood group subjects. Additionally, MPV in the O blood group subjects was significantly lower than in the non‐O blood group subjects.
Conclusions
Because MPV and PDW are used as markers of CVDs, individuals with O and A blood groups in this study may be considered to have a lower risk of CVDs than AB and B blood group subjects. However, prospective cohort studies involving a greater number of volunteers are needed to elucidate these relationships.
Keywords: ABO blood groups, cardiovascular diseases, mean platelet volume, platelet distribution width, platelet indices
1. INTRODUCTION
Some red blood cells have A and/or B antigens on their surface, and blood groups are identified according these antigen types. If the red blood cells have no A or B antigens, the blood type is called the O blood group. Many studies have investigated whether there is any relationship between ABO blood groups and cardiovascular diseases (CVDs).1, 2, 3, 4 Non‐O blood groups—in particular, the A blood group—were found to be associated with ischemic heart disease and atherosclerotic CVD.4, 5 Many different studies have declared that non‐O blood groups have increased von Willebrand factor and coagulation factor VIII levels, and these increased levels could lead to cardiac and thromboembolic diseases.6, 7 Thromboembolic disorders can lead to ischemic heart disease, stroke, and systemic organ failure. These pathologies negatively affect life quality and may lead to mortality. Studies have also reported that non‐O blood group individuals had higher total cholesterol and low‐density lipoprotein cholesterol levels8 and cholesterol absorption rates9 than did O blood group individuals, leading to atherosclerotic plaque progression and an increased risk of coronary artery disease (CAD) and myocardial infarction (MI).5
Platelet indices, including mean platelet volume (MPV) and platelet distribution width (PDW), are potential biomarkers of CVDs.10 These different markers give information about platelet sizes and platelet functions.11, 12 During activation, the platelet size tends to increase, and the platelets become hemostatically more active than small platelets.12, 13 MPV, usually used to measure the platelet size, is an important biomarker of platelet activation and function.12 In previous studies, increased MPV was demonstrated in patients with thromboembolic and atherosclerotic CAD.14, 15, 16 The PDW measures the variability in platelet size.17, 18 Although MPV is currently the most widely used indicator of platelet activation, PDW has previously been used as a marker of platelet activation.18 A high PDW indicates that the platelets are more variable in volume and more reactive than normal.17
The studies mentioned above have shown that both ABO blood groups and platelet indices are associated with ischemic, atherosclerotic, and thromboembolic CVDs. However, as far as we know from the literature, no studies have clarified the relationship between ABO blood groups and platelet indices. For this reason, we sought to express the relationship between ABO blood groups and platelet indices in a healthy adult population.
2. MATERIALS AND METHODS
2.1. Subjects
This study included 301 healthy volunteers (99 women and 202 men; mean age: 32.59 ± 7.52 years; body mass index [BMI]: 24.01 ± 1.69 kg/m2) who applied to the Cardiology Outpatient Clinic of Harran University medical faculty, with atypical chest pain, and who were referred to the Internal Medicine Polyclinic of Yuzuncu Yıl University medical faculty, because of dyspeptic complaints.
The clinical risk factors, smoking status, and other demographic data of all the participants were recorded from hospital registries. The subjects who had malign hematological disorders, were using of anticoagulants or oral contraceptives, or had a history of thromboembolic events, hypertension, diabetes mellitus, hyperlipidemia, chronic respiratory insufficiency, liver and renal disease, CAD, or cerebrovascular disease were not included in the research. Participants were not smoking or drinking and were not taking vitamin therapy.
Written informed consent was obtained from all participants whose blood groups had been worked before, and the study protocol was approved by the Local Ethics Committee of Harran University.
2.2. Blood collection and platelet indices measurement
Venous blood samples were collected from each participant after at least 8 hours of overnight fasting. The blood samples were taken in tubes containing ethylenediaminetetraacetic acid. To prevent in vitro platelet activation, all the measurements were performed immediately after the blood collection. Platelet count (PLT), MPV, PDW, and plateletcrit (PCT) were studied by an auto‐analyzer (Abbott Cell‐Dyn Ruby Hematology Analyzer, USA). Blood groups were determined by the gel column blood typing method using agglutination techniques.
2.3. Statistical analysis
Statistical analyses were conducted with SPSS for Windows version 23.0 software (IBM SPSS Inc, Chicago, IL, USA). The Shapiro‐Wilk test was used to evaluate the normal distribution of the data, and all the data were found to be normally distributed. Numerical variables were presented as mean ± standard deviation, and categorical variables were stated as number (n) and percentage (%). A two‐sample comparison of numerical variables was conducted by an unpaired Student's t test, and multiple comparisons of numerical variables were conducted by analysis of variance (two‐way ANOVA, Bonferroni's post hoc test). The chi‐square test was also used to compare categorical variables. The confidence interval was accepted as 95% throughout the analyses. A two‐tailed P value of <0.05 was considered statistically significant.
3. RESULTS
The demographic characteristics of the enrolled subjects are summarized in Table 1. There were no significant differences with respect to age, gender, BMI, or Rh factors among ABO blood group subjects (P > 0.05 for each).
Table 1.
Comparison of demographic data among ABO blood group subjects
| ABO blood group phenotypes | ANOVA P | ||||
|---|---|---|---|---|---|
| A (n = 87) | B (n = 72) | AB (n = 61) | O (n = 81) | ||
| Age (y) | 31.83 ± 7.33 | 31.6 ± 27.40 | 33.97 ± 7.10 | 33.22 ± 8.05 | 0.196 |
| Gender (female) | 25 (28.7%) | 24 (33.3%) | 25 (41.0%) | 25 (30.9%) | 0.449 |
| BMI (kg/m2) | 24.24 ± 1.59 | 24.20 ± 1.83 | 23.79 ± 1.71 | 23.78 ± 1.69 | 0.173 |
| Rh factor (Rh +) | 44 (50.6%) | 42 (58.3%) | 34 (55.7%) | 36 (44.4%) | 0.332 |
The comparison of alterations in platelet indices among ABO blood group subjects is presented in Table 2 and in Figures 1 and 2. MPV was found to be significantly lower in both O and A blood group subjects than in B and AB blood group subjects (P < 0.05 for each). Additionally, PDW was detected to be considerably lower in O and A blood group subjects than in B blood group subjects (P < 0.006 and P < 0.019, respectively). However, no considerable differences with respect to PLT and PCT among ABO blood group subjects were detected (P > 0.05 for each).
Table 2.
Comparison of platelet indices among ABO blood group subjects
| ABO blood group phenotypes | ANOVA P | ||||
|---|---|---|---|---|---|
| A (n = 87) | B (n = 72) | AB (n = 61) | O (n = 81) | ||
| PLT (×103/µL) | 267.7 ± 61.4 | 265.4 ± 58.4 | 262.6 ± 58.5 | 275.0 ± 50.3 | 0.606 |
| PCT (%) | 0.198 ± 0.041 | 0.209 ± 0.043 | 0.211 ± 0.052 | 0.202 ± 0.042 | 0.209 |
| MPV (fL) | 7.498 ± 0.919a | 7.916 ± 1.243 | 8.031 ± 1.491 | 7.376 ± 1.023b | 0.001 |
| PDW (fL) | 19.22 ± 1.20c | 19.66 ± 1.05 | 19.37 ± 1.21 | 19.13 ± 1.18d | 0.033 |
Values are mean ± SD.
MPV, mean platelet volume; PCT, plateletcrit; PDW, platelet distribution width; PLT, platelet count.
P < 0.05 compared with AB and B blood groups
P < 0.05 compared with AB and B blood groups
P < 0.05 compared with B blood groups
P < 0.05 compared with B blood groups
Figure 1.
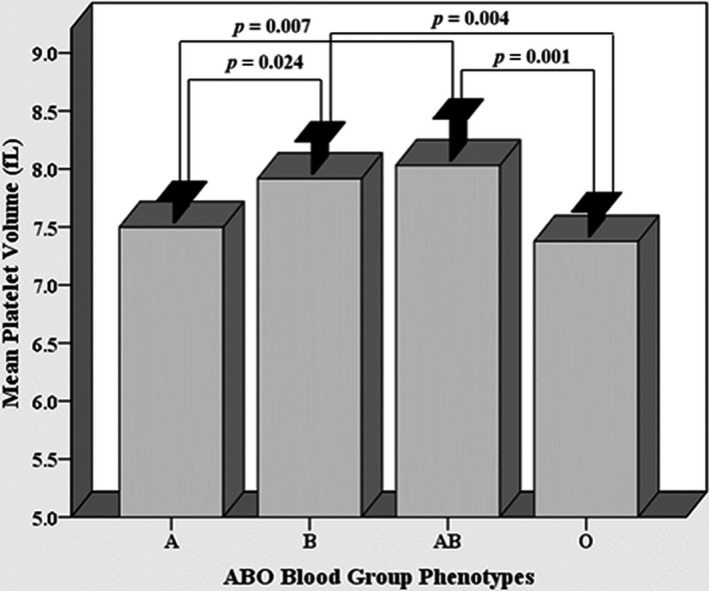
Comparison of mean platelet volume among ABO blood group subjects
Figure 2.
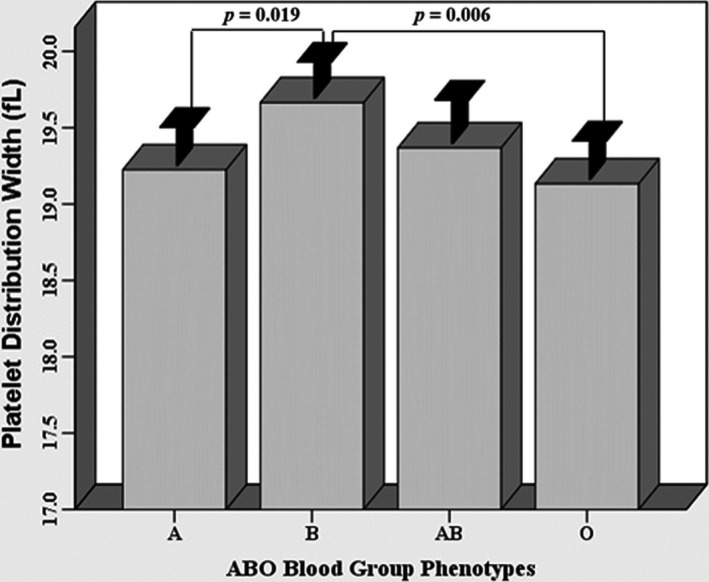
Comparison of platelet distribution width among ABO blood group subjects
The platelet indices of O blood group subjects and non‐O blood groups are compared in Table 3 and Figure 3. MPV values were found to be considerably lower in O blood group subjects than in non‐O blood group subjects (P = 0.008). However, there were no significant differences between O blood group subjects and non‐O blood group subjects in terms of PLT, PCT, or PDW (P > 0.05).
Table 3.
Comparison of platelet indices between O blood group subjects and non‐O blood group subjects
| ABO blood group phenotypes | P Values | ||
|---|---|---|---|
| Non‐O (n = 220) | O (n = 81) | ||
| PLT (×103/µL) | 265.5 ± 59.3 | 275.0 ± 50.3 | 0.204 |
| PCT (%) | 0.205 ± 0.045 | 0.202 ± 0.042 | 0.499 |
| MPV (fL) | 7.783 ± 1.215 | 7.376 ± 1.023 | 0.008 |
| PDW (fL) | 19.41 ± 1.15 | 19.13 ± 1.18 | 0.067 |
Values are mean ± SD.
MPV, mean platelet volume; PCT, plateletcrit; PDW, platelet distribution width; PLT, platelet count.
Figure 3.
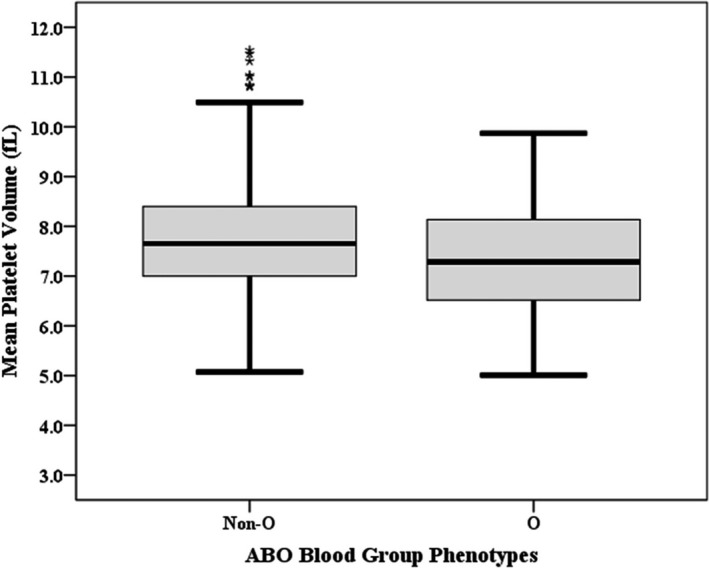
Comparison of mean MPV between O blood group subjects and non‐O blood group subjects
4. DISCUSSION
Although there is a confirmed association between ABO blood groups and CVDs1, 2, 3, 4 and between platelet indices and thromboembolic and atherosclerotic CVD,11, 14, 15, 16 to the best of our knowledge, there is no study that addresses the relationship between platelet indices and CVDs in healthy adults. Hence, we aimed to investigate whether MPV and PDW, two important indicators of platelet activity, had relationships with ABO blood groups in healthy adult subjects.
Studies have elucidated that non‐O blood group subjects have a higher coronary heart disease risk19 and increased atherosclerotic cardiovascular mortality20 compared with O blood group subjects. It has also been detected that there is a lower incidence of coronary heart disease in O blood group subjects as compared with A blood group subjects in Western countries.2, 21 Similarly, some authors have argued that there is a high correlation between MPV and CVDs.11, 15, 22 Besides, this biomarker could be an early predictive factor for cardiac diseases and could give information for prognosis of the pathology.16, 23, 24 Also, Cetin et al found a relationship between MPV and thrombolysis failure in patients with ST‐segment elevation MI.25 In relation to these studies, we found that O blood group subjects have considerably decreased MPV levels than do B and AB blood group subjects (P = 0.004 and P = 0.001, respectively). Moreover, in this study, MPV levels in O blood group subjects were significantly lower than MPV levels in non‐O blood group subjects (P = 0.008). However, several other studies have reported that there is no relationship between MPV and CAD.11, 26 Similarly, Karabuva et al presented that ABO blood groups were not associated with the presence of atherosclerotic CAD.27
Many researchers investigated the association between blood groups and skin diseases. Shahkar et al28 demonstrated no relationship between ABO groups and presence of the pemphigus vulgaris. Similarly, no relationship was observed between ABO groups and Behçet's disease.29 Beckman et al30 stated that A‐factor of ABO blood groups was found increased in the patients with psoriasis. Xie et al31 declared that non‐O blood group was associated with decreased risk of skin cancers. Beside this, there was a significant relationship between non‐O blood groups and non‐melanoma cancers.31
A systematic review and meta‐analysis study conducted by Chen et al4 indicates that risk factors for CAD are high in both A blood group subjects and non‐O blood group subjects. In addition, other studies have suggested that the A blood group is an independent risk factor for coronary atherosclerosis and ischemic CVD.2, 32, 33 In contrast to previous studies, MPV, a useful prognostic marker in patients with CAD and venous thrombosis, was found to be significantly lower in A blood group subjects than in B and AB blood group subjects (P = 0.024 and P = 0.007, respectively).
We also observed that PDW, an indicator of prothrombotic status,34 was significantly higher in B blood group subjects than in A and O blood group subjects (P = 0.019 and P = 0.006, respectively). In accordance with our study, many investigations have shown that PDW was significantly higher in subjects with CAD and thrombolysis failure.25, 35, 36, 37 However, other studies have reported that there is no relationship between PDW and the extent of CAD.11, 18
5. CONCLUSIONS
Although a few studies have not found any relationship between platelet indices and CVDs, the vast majority of investigations have stated that platelet indices are important prognostic markers in CVDs. Hence, we argued in this study that AB and B blood group subjects may have a higher risk of CVDs than do O and A blood group subjects. However, prospective cohort studies involving more volunteers are needed to clarify the relationship between ABO blood groups and CVDs.
Celik H, Duzenli U, Aslan M, et al. The relationship between platelet indices and ABO blood groups in healthy adults. J Clin Lab Anal. 2019;33:e22720 10.1002/jcla.22720
REFERENCES
- 1. Zhou S. Is ABO blood group truly a risk factor for thrombosis and adverse outcomes? World J Cardiol. 2014;26:985‐992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gong P, Luo SH, Li XL, et al. Relation of ABO blood groups to the severity of coronary atherosclerosis: an Gensini score assessment. Atherosclerosis. 2014;237:748‐753. [DOI] [PubMed] [Google Scholar]
- 3. Sujirachato K, Worasuwannarak W, Srisont S, et al. ABO blood group and coronary atherosclerosis in Thais at Ramathibodi Hospital. Siriraj Med J. 2015;67:53‐59. [Google Scholar]
- 4. Chen Z, Yang S‐H, Xu H, et al. ABO blood group system and the coronary artery disease: an updated systematic review and meta‐analysis. Sci Rep. 2016;6:23250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Huang X, Zou Y, Li L, et al. Relation of ABO blood groups to the plaque characteristic of coronary atherosclerosis. Biomed Res Int. 2017;2017:1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schleef M, Strobel E, Dick A, et al. Relationship between ABO and secretor genotype with plasma levels of factor VIII and von Willebrand factor in thrombosis patients and control individuals. Br J Haematol. 2005;128:100‐107. [DOI] [PubMed] [Google Scholar]
- 7. Ohira T, Cushman M, Tsai MY, et al. ABO blood group, other risk factors and incidence of venous thromboembolism: the longitudinal investigation of thromboembolism etiology (LITE). J Thromb Haemost. 2007;5:1455‐1461. [DOI] [PubMed] [Google Scholar]
- 8. Chen Y, Chen C, Ke X, et al. Analysis of circulating cholesterol levels as a mediator of an association between ABO blood group and coronary heart disease. Circ Cardiovasc Genet. 2014;7:43‐48. [DOI] [PubMed] [Google Scholar]
- 9. Silbernagel G, Chapman MJ, Genser B, et al. High intestinal cholesterol absorption is associated with cardiovascular disease and risk alleles in ABCG8 and ABO: evidence from the LURIC and YFS cohorts and from a meta‐analysis. J Am Coll Cardiol. 2013;62:291‐299. [DOI] [PubMed] [Google Scholar]
- 10. Mirzaie AZ, Abolhasani M, Ahmadinejad B, et al. Platelet count and MPV, routinely measured but ignored parameters used in conjunction with the diagnosis of acute coronary syndrome: single study center in Iranian population, 2010. Med J Islam Repub Iran. 2012;26:17‐21. [PMC free article] [PubMed] [Google Scholar]
- 11. Turk U, Tengiz I, Ozpelit E, et al. The relationship between platelet indices and clinical features of coronary artery disease. Kardiol Pol. 2013;71:1129‐1134. [DOI] [PubMed] [Google Scholar]
- 12. Gasparyan AY, Ayvazyan L, Mikhailidis DP, et al. Mean platelet volume: a link between thrombosis and inflammation? Send to Curr Pharm Des. 2011;17:47‐58. [DOI] [PubMed] [Google Scholar]
- 13. Farah R, Samra N. Mean platelets volume and neutrophil to lymphocyte ratio as predictors of stroke. J Clin Lab Anal. 2018;32:e22189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kucur SK, Gozukara I, Aksoy A, et al. How medical treatment affects mean platelet volume as a cardiovascular risk marker in polycystic ovary syndrome? Blood Coagul Fibrinolysis. 2015;26:862‐865. [DOI] [PubMed] [Google Scholar]
- 15. Sansanayudh N, Anothaisintawee T, Muntham D, et al. Mean platelet volume and coronary artery disease: a systematic review and meta‐analysis. Int J Cardiol. 2014;175:433‐440. [DOI] [PubMed] [Google Scholar]
- 16. Chu SG, Becker RC, Berger PB, et al. Mean platelet volume as a predictor of cardiovascular risk: a systematic review and meta‐analysis. J Thromb Haemost. 2010;8:148‐156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vagdatli E, Gounari E, Lazaridou E, et al. Platelet distribution width: a simple, practical and specific marker of activation of coagulation. Hippokratia. 2010;14:28‐32. [PMC free article] [PubMed] [Google Scholar]
- 18. De Luca G, Venegoni L, Iorio S, et al. Platelet distribution width and the extent of coronary artery disease: results from a large prospective study. Platelets. 2010;21:508‐514. [DOI] [PubMed] [Google Scholar]
- 19. He M, Wolpin B, Rexrode K, et al. ABO blood group and risk of coronary heart disease in two prospective cohort studies. Arterioscler Thromb Vasc Biol. 2012;32:2314‐2320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Etemadi A, Kamangar F, Islami F, et al. Mortality and cancer in relation to ABO blood group phenotypes in the Golestan Cohort Study. BMC Med. 2015;13:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Franchini M, Mengoli C, Capuzzo E, et al. Correlation between ABO blood group, and conventional hematological and metabolic parameters in blood donors. Semin Thromb Hemost. 2016;42:75‐86. [DOI] [PubMed] [Google Scholar]
- 22. Tsiara S, Elisaf M, Jagroop IA, et al. Platelets as predictors of vascular risk: is there a practical index of platelet activity? Clin Appl Thromb Hemost. 2003;9:177‐190. [DOI] [PubMed] [Google Scholar]
- 23. Vizioli L, Muscari S, Muscari A. The relationship of mean platelet volume with the risk and prognosis of cardiovascular diseases. Int J Clin Pract. 2009;63:1509‐1515. [DOI] [PubMed] [Google Scholar]
- 24. Taskesen T, Sekhon H, Wroblewski I, et al. Usefulness of mean platelet volume to predict significant coronary artery disease in patients with non–ST‐elevation acute coronary syndromes. Am J Cardiol. 2017;119:192‐196. [DOI] [PubMed] [Google Scholar]
- 25. Cetin M, Bakirci EM, Baysal E, et al. Increased platelet distribution width is associated with ST‐segment elevation myocardial infarction and thrombolysis failure. Angiology. 2014;65:737‐743. [DOI] [PubMed] [Google Scholar]
- 26. De Luca G, Santagostino M, Secco GG, et al. Mean platelet volume and the extent of coronary artery disease: results from a large prospective study. Atherosclerosis. 2009;206:292‐297. [DOI] [PubMed] [Google Scholar]
- 27. Karabuva S, Carević V, Radić M, et al. The association of ABO blood groups with extent of coronary atherosclerosis in Croatian patients suffering from chronic coronary artery disease. Biochem Med (Zagreb). 2013;23:351‐359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shahkar H, Fallahzadeh MK, Namazi MR. ABO blood groups and pemphigus vulgaris: no relationship. Acta Dermatovenerol Alp Pannonica Adriat. 2010;19:49‐51. [PubMed] [Google Scholar]
- 29. Ozyurt K, Ozturk P, Gul M, et al. ABO blood groups, Rhesus factor, and Behçet's disease. Acta Dermatovenerol Alp Pannonica Adriat. 2013;22:63‐64. [PubMed] [Google Scholar]
- 30. Beckman L, Bronnestam R, Cedergren B, et al. HL‐A antigens, blood groups, serum groups and red cell enzyme types in psoriasis. Hum Hered. 1974;24:496‐506. [DOI] [PubMed] [Google Scholar]
- 31. Xie J, Qureshi AA, Li Y, et al. ABO blood group and incidence of skin cancer. PLoS ONE. 2010;5:e11972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ba DM, Sow MS, Diack A, et al. Cardiovascular disease and ABO blood‐groups in Africans. are blood‐group a individuals at higher risk of ischemic disease?: a pilot study. Egypt Heart J. 2017;69:229‐234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wang Y, Zhou B‐Y, Zhu C‐G, et al. Distribution of ABO blood groups and coronary artery calcium. Heart Lung Circ. 2017;26:593‐598. [DOI] [PubMed] [Google Scholar]
- 34. Jindal S, Gupta S, Gupta R, et al. Platelet indices in diabetes mellitus: indicators of diabetic microvascular complications. Hematology. 2011;16:86‐89. [DOI] [PubMed] [Google Scholar]
- 35. Vatankulu MA, Sonmez O, Ertas G, et al. A new parameter predicting chronic total occlusion of coronary arteries: platelet distribution width. Angiology. 2014;65:60‐64. [DOI] [PubMed] [Google Scholar]
- 36. Khandekar MM, Khurana AS, Deshmukh SD, et al. Platelet volume indices in patients with coronary artery disease and acute myocardial infarction: an Indian scenario. J Clin Pathol. 2006;59:146‐149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cetin MS, Ozcan Cetin EH, Akdi A, et al. Platelet distribution width and plateletcrit: novel biomarkers of ST elevation myocardial infarction in young patients. Kardiol Pol. 2017;75:1005‐1012. [DOI] [PubMed] [Google Scholar]


