Abstract
INTRODUCTION:
The effectiveness of high-frequency oscillatory ventilation (HFOV) in the pediatric hematopoietic cell transplant patient has not been established. We sought to identify current practice patterns of HFOV, investigate parameters during HFOV and their association with mortality, and compare the use of HFOV to conventional mechanical ventilation in severe pediatric ARDS.
METHODS:
This is a retrospective analysis of a multi-center database of pediatric and young adult allogeneic hematopoietic cell transplant subjects requiring invasive mechanical ventilation for critical illness from 2009 through 2014. Twelve United States pediatric centers contributed data. Continuous variables were compared using a Wilcoxon rank-sum test or a Kruskal-Wallis analysis. For categorical variables, univariate analysis with logistic regression was performed.
RESULTS:
The database contains 222 patients, of which 85 subjects were managed with HFOV. Of this HFOV cohort, the overall pediatric ICU survival was 23.5% (n = 20). HFOV survivors were transitioned to HFOV at a lower oxygenation index than nonsurvivors (25.6, interquartile range 21.1–36.8, vs 37.2, interquartile range 26.5–52.2, P = .046). Survivors were transitioned to HFOV earlier in the course of mechanical ventilation, (day 0 vs day 2, P = .002). No subject survived who was transitioned to HFOV after 1 week of invasive mechanical ventilation. We compared subjects with severe pediatric ARDS treated only with conventional mechanical ventilation versus early HFOV (within 2 d of invasive mechanical ventilation) versus late HFOV. There was a trend toward difference in survival (conventional mechanical ventilation 24%, early HFOV 30%, and late HFOV 9%, P = .08).
CONCLUSIONS:
In this large database of pediatric allogeneic hematopoietic cell transplant subjects who had acute respiratory failure requiring invasive mechanical ventilation for critical illness with severe pediatric ARDS, early use of HFOV was associated with improved survival compared to late implementation of HFOV, and the subjects had outcomes similar to those treated only with conventional mechanical ventilation.
Keywords: hematopoietic stem cell transplantation, critical care, respiratory insufficiency, artificial respiration, high frequency ventilation, mortality, respiratory distress syndrome, adult
Introduction
The pediatric allogeneic hematopoetic cell transplant patient admitted to the pediatric ICU has a high mortality risk. While outcomes for these patients have improved,1 respiratory failure and mechanical ventilation continue to be associated with high mortality.2–5 These patients are at high risk of severe pulmonary complications when respiratory failure develops.6–8 Immunodeficiency is a risk factor for the development of pediatric ARDS and related mortality. The vast majority of pediatric hematopoietic cell transplant patients intubated for respiratory failure develop pediatric ARDS within the first week of ventilation.9
High-frequency oscillatory ventilation (HFOV) is a common rescue modality utilized in pediatric ARDS. Data supporting its use in pediatric ARDS demonstrate an improvement in oxygenation.10–14 However, emerging data question the effect of HFOV on meaningful outcomes. Some studies have suggested that HFOV use may be associated with a higher mortality and a longer duration of ventilation even when severity of illness markers are incorporated into the analyses.15,16 In the adult population, HFOV use has been found to not improve survival. One trial was stopped early due to a higher mortality rate, increased sedation and neuromuscular blockade, and more vasoactive agents in the HFOV group. In pediatrics, unfortunately, the available data do not allow for an evidence-based application of HFOV in the management of pediatric ARDS. Furthermore, the effectiveness of HFOV in unique and highly vulnerable populations, such as pediatric hematopoietic cell transplant patients, has not been established.
We sought to establish current practice patterns of HFOV in the pediatric allogeneic hematopoietic cell transplant patient, investigate parameters during HFOV and their association with mortality, and compare HFOV use to conventional mechanical ventilation in patients with severe pediatric ARDS.
QUICK LOOK.
Current knowledge
Although high-frequency oscillatory ventilation (HFOV) is commonly used in pediatric ARDS, the effectiveness of this modality remains unclear. Many studies suggest an improvement in oxygenation, yet other studies suggest its use may be associated with higher mortality and longer duration of ventilation. The currently available data do not allow for an evidence-based application of HFOV. Furthermore, the application of HFOV in the pediatric hematopoietic cell transplant patient has not been established.
What this paper contributes to our knowledge
In pediatric and young adults after hematopoietic cell transplant with severe pediatric ARDS, those who survived had continued improvement in oxygenation throughout an HFOV course. Also, earlier use of HFOV was associated with improved survival compared to those who were transitioned later in the course of mechanical ventilation. Late transition to HFOV, especially after 7 d of mechanical ventilation, should be done with caution.
Methods
This is a secondary analysis of a retrospective multi-center database. Twelve centers contributed up to 25 of their most recent, consecutive, pediatric allogeneic hematopoietic cell transplant patients who had acute respiratory failure requiring invasive mechanical ventilation. All indications for allogeneic hematopoietic cell transplant were included. Subjects were included if they were between the ages of 1 month and 21 y. Autologous transplant patients were excluded. Patients who were admitted prior to January 1, 2009, were also excluded from the study to ensure the data would be as relevant to current practice as possible. Institutional review board approval was obtained at each individual center prior to the start of data collection.
The study was performed at the following institutions: Riley Hospital for Children at Indiana University School of Medicine; Joseph M Sanzari Children's Hospital at Hackensack University Medical Center; Medical College of Wisconsin, Children's Hospital of Wisconsin; Children's Hospital of Philadelphia University of Pennsylvania Perelman School of Medicine; University of Minnesota, Masonic Children's Hospital; Weil Cornell Medical College, New York Presbyterian Hospital; Dana-Farber Cancer Institute; Children's Hospital of Los Angeles; University of Washington and Seattle Children's Hospital; Duke Children's Hospital; Nationwide Children's Hospital; and Penn State Children's Hospital.
A total of 222 patients were included in the original database, of which 85 subjects received HFOV at some point during their course of mechanical ventilation. These patients served as the subjects for the description of HFOV utilization in this population as well as for the comparison of survivors to nonsurvivors. We collected the following data points: demographics, transplant variables, length of pediatric ICU stay, duration of mechanical ventilation, duration of HFOV, use of vasoactive agents during the course of mechanical ventilation, use of renal replacement therapy during the course of mechanical ventilation, use of inhaled nitric oxide, respiratory infections, and survival. Respiratory parameters, settings, and arterial blood gas data were collected every 6 h for the day before, the day of, and day after transition to HFOV. Oxygenation index (OI) was calculated as (FIO2 × ¯Paw/PaO2) × 100, where ¯Paw indicates mean airway pressure. Oxygen saturation index was calculated as (FIO2 × ¯Paw/PaO2) × 100 if the pulse oximeter saturation was ≤ 97%.17
All but 2 of the subjects had severe pediatric ARDS as defined using the OI or oxygen saturation index criteria established by the Pediatric Acute Lung Injury and Consensus Conference (PALICC); to assess the value of timing of HFOV, subjects were categorized into 3 groups: subjects managed only with conventional mechanical ventilation, subjects placed on HFOV early in the course of mechanical ventilation, and subjects transitioned to HFOV late in the mechanical ventilation course. Early HFOV was defined a priori as being transitioned to HFOV by day 2 of mechanical ventilation, with the day of intubation being day 0.
Statistical Analysis
Continuous variables are presented as medians with interquartile ranges (IQRs) and were compared with a Wilcoxon rank-sum test or a Kruskal-Wallis analysis. A Dunn test was run to conduct a pairwise comparison for variables that were statistically significant on a Kruskal-Wallis analysis when comparing the 3 groups of conventional mechanical ventilation, early HFOV, and late HFOV. Categorical variables are presented as frequencies or percentages and were compared with chi-square analysis or a Fisher exact test where appropriate.
Results
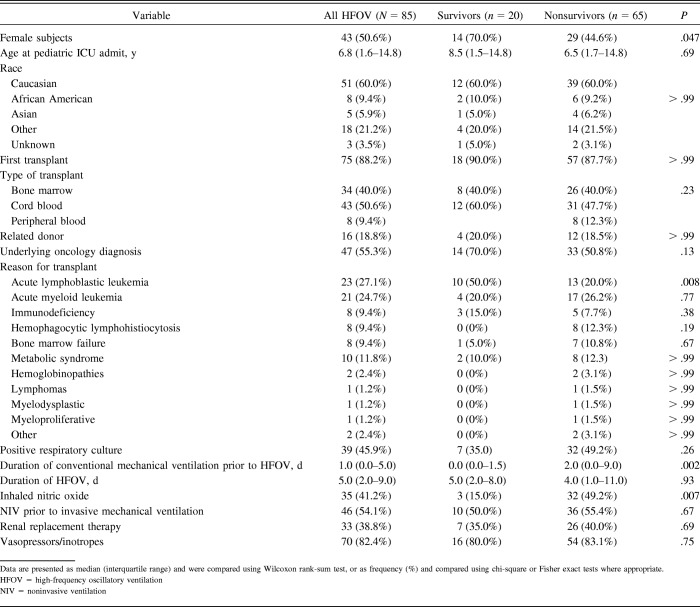
There were 85 pediatric hematopoietic cell transplant subjects transitioned to HFOV. Of these 85 subjects, only 20 subjects survived to pediatric ICU discharge for an overall survival rate of 23.5%. At 180 d after pediatric ICU discharge, only 14 of the 20 subjects were still alive, rendering a 180-d survival rate of 16.5% for the whole HFOV cohort. Demographics and those categorized by survival are displayed in Table 1. Of note, survivors were more likely to be female (P = .047). Interestingly, there was a predominance of acute lymphoblastic leukemia in the group that survived compared to those who died (50% vs 20%, P = .008). Of the 20 surviving subjects, 10 had acute lymphoblastic leukemia as the indication for transplant. While not reaching statistical significance, it is of note that none of the subjects with hemophagocytic lymphohistiocytosis survived a course of HFOV. There were no differences in any of the other underlying diagnoses between survivors and nonsurvivors. When underlying diagnoses were categorized as oncologic or non-oncologic, there was also no difference between survivors and nonsurvivors (P = .13).
Table 1.
Demographics Assess by Survival Status to Pediatric ICU Discharge
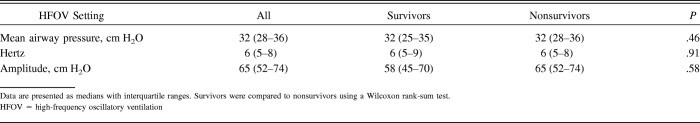
The initial HFOV settings can be found in Table 2. The median change in ¯Paw between the 6 h prior to HFOV initiation and the implementation of HFOV was an increase of 10.5 cm H2O, and this was not different between survivors and nonsurvivors.
Table 2.
Starting Settings on HFOV Compared by Survival Status
Subjects who survived were transitioned to HFOV at a lower OI (25.6, IQR 21.1–36.8 vs 37.2, IQR 26.5–52.2, P = .046). The median OI at 6 h and 24 h of HFOV for both survivors and nonsurvivors decreased. The median OI at 48 h for the survivors was lower than that for nonsurvivors (P = .02). Additionally, the median OI for nonsurvivors was almost the same at 24 h, 48 h, and at discontinuation of HFOV (Table 3).
Table 3.
Oxygenation Index and Oxygen Saturation Index Over Time Assessed by Pediatric ICU Survival Status
Survivors were transitioned to HFOV earlier in the course of mechanical ventilation. Their median day of transition from conventional mechanical ventilation to HFOV was 0 d (IQR 0–1.5) versus 2 d (IQR 0–9) for nonsurvivors, P = .002. Table 4 illustrates common critical care interventions by survival status. Seventeen of the 20 survivors were transitioned by day 2 of invasive mechanical ventilation. Those transitioned to HFOV early had a higher survival than those transitioned late (32.7% [n = 17] vs 9.1% [n = 3], P = .02). No subjects who were transitioned to HFOV after 1 week of conventional mechanical ventilation survived.
Table 4.
Comparison of Common Critical Care Interventions and Duration of Ventilation by Survivor Status
There was no difference between survivors and nonsurvivors in the need for vasoactive agents or renal replacement therapy. Nonsurvivors were more likely to have been placed on inhaled nitric oxide (P = .007) (Table 4). The institutional effect for this population was also examined, and no institutional effect on mortality was found (P = .41). In addition, no statistical difference in the application of early or late HFOV by the institution was seen (P = .06).
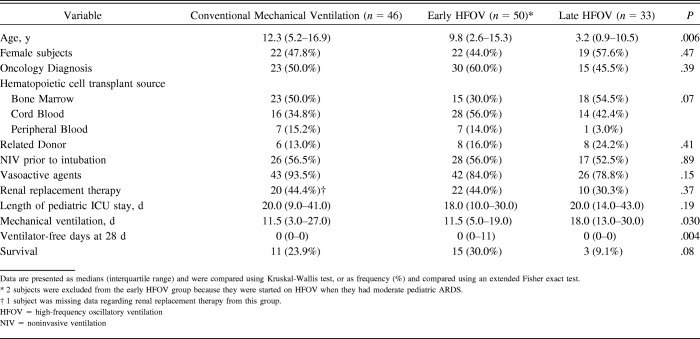
Conventional Mechanical Ventilation Versus Early HFOV Versus Late HFOV in Subjects With Severe Pediatric ARDS
Of the 129 subjects included in this comparative analysis, 50 were in the early HFOV group, 33 were in the late HFOV group, and 46 were in the conventional mechanical ventilation group. The conventional mechanical ventilation group represents the cohort that had severe pediatric ARDS according to the PALICC definition and did not transition to HFOV. Two subjects were excluded from the early HFOV group because they had only moderate pediatric ARDS at time of conversion to HFOV. Both of these subjects survived. There was a difference in age among these groups (P = .006). On pairwise testing, those ventilated with only conventional mechanical ventilation were older than those in the late HFOV group (P = .003), but there was no statistical difference with early HFOV. There was no difference in gender, oncology diagnosis, source of hematopoietic cell transplant, or related donor status between the 3 groups (Table 5).
Table 5.
Comparison of Demographic and Critical Care Variables Stratified by Mechanical Ventilation Practice
There was a trend toward a lower survival rate in the late HFOV group (P = .08), with the early HFOV group having the highest rate of survival at 30.0% (Table 5). The duration of mechanical ventilation was different between groups (P = .03), but on pairwise testing there was no difference in the total duration of mechanical ventilation between the conventional mechanical ventilation and early HFOV groups. Those ventilated with late HFOV had a longer duration of mechanical ventilation compared to the early HFOV group (P = .039). Ventilator-free days at 28 d was examined. The distribution of ventilator-free days was statistically different; however, the median number of ventilator-free days for all groups was 0 (Table 5). Interestingly, in the late HFOV group, every subject had 0 ventilator-free days. In the conventional mechanical ventilation group, 83% of subjects (n = 39) had 0 ventilator-free days, and in the early HFOV group, 72% of subjects (n = 36) had 0 ventilator-free days. On pairwise analysis, ventilator-free days for the conventional mechanical ventilation was not statistically different from ventilator-free days for the early HFOV group, but ventilator-free days for the early HFOV group was different from that of the late HFOV group (P = .002). The use of noninvasive ventilation prior to intubation was similar (P = .51). Vasoactive medication use was common in all groups and was not statistically different (P = .15). The use of renal replacement therapy was also not different among groups (P = .37).
Discussion
Our study has 3 significant findings. The first is that subjects who were transitioned to HFOV earlier in the course of invasive mechanical ventilation had improved survival when compared to subjects transitioned to HFOV late in their course of mechanical ventilation. Second, those who survived continued to have improvement in their oxygenation; those who died had a plateau in the improvement of their OI at 48 h. The last finding in this cohort is that the outcomes were not statistically different when comparing subjects with severe pediatric ARDS who were managed with conventional mechanical ventilation alone to those who were transitioned early to HFOV.
HFOV has been a longstanding tool in the treatment of pediatric ARDS. After HFOV demonstrated a decrease in the risk of chronic lung disease in premature babies, HFOV gained interest for use in pediatric ARDS.18 Arnold et al11 found promising results with the application of HFOV in ARDS, illustrating improved oxygenation and decreased need for supplemental O2 at 30 d. However, there was no difference in the duration of mechanical ventilation or survival. Multiple studies have shown that HFOV can improve oxygenation.12–14,19–21 Despite this improvement in oxygenation, studies have not confirmed a mortality difference. Like our study, however, Arnold et al19 found in a heterogeneous population that an improvement in OI discriminated between survivors and nonsurvivors, and Yehya et al22 found the same in immunocompromised subjects.
When comparing subjects on HFOV, most had an improvement in oxygenation, but those who survived had a more dramatic and sustained OI improvement. In this high-acuity cohort, continued oxygenation improvement was associated with survival. It is likely that the continued improvement in oxygenation represents recoverable lung injury, whereas subjects who experienced a plateau in their OI improvement may have had unrecoverable lung damage. While the nonsurvivors did have a lower OI at 48 h and at the conclusion of HFOV, it was not a clinically notable improvement. The median OI at both points remained consistent with oxygenation criteria for severe pediatric ARDS. A greater use of inhaled nitric oxide was seen in the nonsurvivor population. This likely reflects the severity of lung disease in nonsurvivors. Potentially this rescue intervention was applied more often in this group due to the lack of sustained improvement in oxygenation.
With this demonstration of improvement in oxygenation, the critical care community has sought to find the best way to apply this modality. The improvement in oxygenation is encouraging, but the lack of clinically relevant positive changes in outcomes continues to be a source of frustration. In this cohort, early application of HFOV (ie, within the first 2 d of invasive mechanical ventilation) was associated with improved survival compared to late application of HFOV. This is in line with suggestions from previously published literature.12,13 Perhaps this early approach with HFOV allows for earlier, more aggressive lung recruitment. However, this directly contradicts more recent literature that questions the current approach to HFOV, suggesting that it is associated with worse mortality and longer duration of mechanical ventilation in the general pediatric population.15,16 In the study by Bateman et al,15 ventilator-free days were lower in the early HFOV cohort as compared to those who were managed with only conventional mechanical ventilation or with late HFOV. This study's cohort is unique from the general pediatric population in that they were at higher risk for a variety of lung diseases, including severe infections, diffuse alveolar hemorrhage, idiopathic pulmonary syndrome, lung graft-versus-host disease, and bronchiolitis obliterans.6,8,23 The recoverability of each of these diseases is variable. Additionally, these patients have generally been exposed to previous lung-toxic drugs and infections, which placed them at risk to be admitted to the pediatric ICU with existing lung disease. Therefore, the findings from studies of the general pediatric population may not be applicable to our unique and highly vulnerable patient population.
To begin to understand the effectiveness of HFOV compared to conventional mechanical ventilation, we isolated subjects with severe pediatric ARDS, as defined by PALICC guidelines, treated with conventional mechanical ventilation alone and compared them to the early and late HFOV groups. In this analysis, we found data that contradict previously published data by Bateman et al.15 In this secondary analysis of the RESTORE database, they found that those treated with early HFOV had a longer duration of mechanical ventilation. In our specialized cohort, this was not the case. Those treated with early HFOV had the same duration of mechanical ventilation as those with severe pediatric ARDS treated with conventional mechanical ventilation alone. Additionally, the early HFOV group had the highest survival at 30%, although this did not meet statistical significance. Isolating those treated with HFOV later in the course of mechanical ventilation, we found this group to have both a higher mortality and a longer duration of mechanical ventilation.
Our study does have limitations that are inherent to all retrospective analyses. We were limited by the availability of the data, particularly blood gas data, to calculate OI for every subject at each time point. We hoped to negate some of this limitation by collecting OI at multiple time points to obtain a more complete picture of the degree of oxygenation failure in this population. Additionally, the study is limited by a diverse approach to both transitioning and utilization of HFOV. Because this study was retrospective, subjects were transitioned to HFOV at the discretion of the clinical care team. Despite these limitations, this study is strengthened by the large cohort of subjects from multiple centers, which improves the generalizability and the frequency of ventilator and blood gas data collected throughout the study.
Conclusion
In pediatric allogeneic hematopoietic cell transplant subjects, those treated with HFOV had a lower overall pediatric ICU survival at 23.5% compared to the reported survival rates of 40–50% of those receiving all types of mechanical ventilation.5,24,25 However, this is more likely a reflection of the severity of lung injury than of the modality itself. Furthermore, there is a suggestion that early application of HFOV may be of benefit. A prospective study is necessary to answer the questions about the timing of HFOV and the overall benefit of this modality. While it is clear that a prospective trial is warranted to make firm recommendations, our data suggest that the late use of HFOV in this population, especially after 7 d of conventional mechanical ventilation, should be undertaken with caution.
Footnotes
The authors have disclosed no conflicts of interest.
A version of this paper was presented at the American Thoracic Society conference, held May 19–24, 2017, in Washington, D.C.
References
- 1. Tamburro RF, Barfield RC, Shaffer ML, Rajasekaran S, Woodard P, Morrison RR, et al. Changes in outcomes (1996-2004) for pediatric oncology and hematopoietic stem cell transplant patients requiring invasive mechanical ventilation. Pediatr Crit Care Med 2008;9(3):270–277. [DOI] [PubMed] [Google Scholar]
- 2. van Gestel JP, Bierings MB, Dauger S, Dalle JH, Pavlicek P, Sedlacek P, et al. Outcome of invasive mechanical ventilation after pediatric allogeneic hematopoietic SCT: results from a prospective, multicenter registry. Bone Marrow Transplant 2014;49(10):1287–1292. [DOI] [PubMed] [Google Scholar]
- 3. Wermke M, Schiemanck S, Hoffken G, Ehninger G, Bornhauser M, Illmer T. Respiratory failure in patients undergoing allogeneic hematopoietic SCT: a randomized trial on early non-invasive ventilation based on standard care hematology wards. Bone Marrow Transplant 2012;47(4):574–580. [DOI] [PubMed] [Google Scholar]
- 4. Kaya Z, Weiner DJ, Yilmaz D, Rowan J, Goyal RK. Lung function, pulmonary complications, and mortality after allogeneic blood and marrow transplantation in children. Biol Blood Marrow Transplant 2009;15(7):817–826. [DOI] [PubMed] [Google Scholar]
- 5. Duncan CN, Lehmann LE, Cheifetz IM, Greathouse K, Haight AE, Hall MW, et al. Clinical outcomes of children receiving intensive cardiopulmonary support during hematopoietic stem cell transplant. Pediatr Crit Care Med 2013;14(3):261–267. [DOI] [PubMed] [Google Scholar]
- 6. Cerveri I, Zoia MC, Fulgoni P, Corsico A, Casali L, Tinelli C, et al. Late pulmonary sequelae after childhood bone marrow transplantation. Thorax 1999;54(2):131–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Leneveu H, Bremont F, Rubie H, Peyroulet MC, Broue A, Suc A, et al. Respiratory function in children undergoing bone marrow transplantation. Pediatr Pulmonol 1999;28(1):31–38. [DOI] [PubMed] [Google Scholar]
- 8. Griese M, Rampf U, Hofmann D, Fuhrer M, Reinhardt D, Bender-Gotze C. Pulmonary complications after bone marrow transplantation in children: twenty-four years of experience in a single pediatric center. Pediatr Pulmonol 2000;30(5):393–401. [DOI] [PubMed] [Google Scholar]
- 9. Rowan CM, Smith LS, Loomis A, McArthur J, Gertz SJ, Fitzgerald JC, et al. Pediatric acute respiratory distress syndrome in pediatric allogeneic hematopoietic stem cell transplants: a multicenter study. Pediatr Crit Care Med 2017;18(4):304–309. [DOI] [PubMed] [Google Scholar]
- 10. Rosenberg RB, Broner CW, Peters KJ, Anglin DL. High-frequency ventilation for acute pediatric respiratory failure. Chest 1993;104(4):1216–1221. [DOI] [PubMed] [Google Scholar]
- 11. Arnold JH, Hanson JH, Toro-Figuero LO, Gutiérrez J, Berens RJ, Anglin DL. Prospective, randomized comparison of high-frequency oscillatory ventilation and conventional mechanical ventilation in pediatric respiratory failure. Crit Care Med 1994;22(10):1530–1539. [PubMed] [Google Scholar]
- 12. Brogan TV, Bratton SL, Meyer RJ, O'Rourke PP, Jardine DS. Nonpulmonary organ failure and outcome in children treated with high-frequency oscillatory ventilation. J Crit Care 2000;15(1):5–11. [DOI] [PubMed] [Google Scholar]
- 13. Slee-Wijffels FY, van der Vaart KR, Twisk JW, Markhorst DG, Plötz FB. High-frequency oscillatory ventilation in children: a single-center experience of 53 cases. Crit Care 2005;9(3):R274–R279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ben Jaballah N, Khaldi A, Mnif K, Bouziri A, Belhadj S, Hamdi A, et al. High-frequency oscillatory ventilation in pediatric patients with acute respiratory failure. Pediatr Crit Care Med 2006;7(4):362–367. [DOI] [PubMed] [Google Scholar]
- 15. Bateman ST, Borasino S, Asaro LA, Cheifetz IM, Diane S, Wypij D, et al. Early high-frequency oscillatory ventilation in pediatric acute respiratory failure: a propensity score analysis. Am J Respir Crit Care Med 2016;193(5):495–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gupta P, Green JW, Tang X, Gall CM, Gossett JM, Rice TB, et al. Comparison of high-frequency oscillatory ventilation and conventional mechanical ventilation in pediatric respiratory failure. JAMA Pediatr 2014;168(3):243–249. [DOI] [PubMed] [Google Scholar]
- 17. Thomas NJ, Shaffer ML, Willson DF, Shih MC, Curley MA. Defining acute lung disease in children with the oxygenation saturation index. Pediatr Crit Care Med 2010;11(1):12–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Randomized study of high-frequency oscillatory ventilation in infants with severe respiratory distress syndrome. HiFO Study Group. J Pediatr 1993;122(4):609–619. [DOI] [PubMed] [Google Scholar]
- 19. Arnold JH, Anas NG, Luckett P, Cheifetz IM, Reyes G, Newth CJ, et al. High-frequency oscillatory ventilation in pediatric respiratory failure: a multicenter experience. Crit Care Med 2000;28(12):3913–3919. [DOI] [PubMed] [Google Scholar]
- 20. Fioretto JR, Batista KA, Carpi MF, Bonatto RC, Moraes MA, Ricchetti SM, et al. High-frequency oscillatory ventilation associated with inhaled nitric oxide compared to pressure-controlled assist/control ventilation and inhaled nitric oxide in children: randomized, non-blinded, crossover study. Pediatr Pulmonol 2011;46(8):809–816. [DOI] [PubMed] [Google Scholar]
- 21. Yehya N, Topjian AA, Lin R, Berg RA, Thomas NJ, Friess SH. High frequency oscillation and airway pressure release ventilation in pediatric respiratory failure. Pediatr Pulmonol 2014;49(7):707–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yehya N, Topjian AA, Thomas NJ, Friess SH. Improved oxygenation 24 hours after transition to airway pressure release ventilation or high-frequency oscillatory ventilation accurately discriminates survival in immunocompromised pediatric patients with acute respiratory distress syndrome. Pediatr Crit Care Med 2014;15(4):e147–e156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rowan CM, Baloglu O, McArthur J. Non-infectious pulmonary complications of hematopoietic stem cell transplantation. Journal of Pediatric Critical Care 2014;3(3):133–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rowan CM, Gertz SJ, McArthur J, Fitzgerald JC, Nitu ME, Loomis A, et al. Invasive mechanical ventilation and mortality in pediatric hematopoietic stem cell transplantation: a multicenter study. Pediatr Crit Care Med 2016;17(4):294–302. [DOI] [PubMed] [Google Scholar]
- 25. Chima RS, Daniels RC, Kim MO, Li D, Wheeler DS, Davies SM, et al. Improved outcomes for stem cell transplant recipients requiring pediatric intensive care. Pediatr Crit Care Med 2012;13(6):e336–e342. [DOI] [PubMed] [Google Scholar]