Abstract
Purpose
Despite increasing evidence for the effectiveness of off-the-shelf and rehabilitation-specific active video games (AVGs) and virtual reality (VR) systems for rehabilitation, clinical uptake remains poor. A better match between VR/AVG system capabilities and client/therapist needs, through improved end-user involvement (UI) in VR/AVG implementation research, may increase uptake of this technology. The purpose of this paper is to review four case examples from the authors’ collective experience of including end users in VR/AVG research to identify common benefits, challenges and lessons learned.
Design/methodology/approach
The authors apply knowledge and lessons learned from the four cases to make recommendations for subsequent user-engaged research design and methods, including evaluation of the impact of end UI.
Findings
A better match between VR/AVG system capabilities and client/therapist needs leads to improved end UI in all stages of VR/AVG implementation research. There are common benefits of increasing buy-in and soliciting early on the knowledge and skills of therapists as well as input from the ultimate end users: people participating in rehabilitation. Most settings have the challenges of balancing the technology requirements with the needs and goals of the practice setting and of the end users.
Research limitations/implications
Increasing end UI in VR/AVG implementation research may address issues related to poor clinical uptake. In the VR/AVG context, end users can be therapists, clients or technology developers/engineers. This paper presented four case scenarios describing the implementation of different VR/AVG systems and involving a variety of populations, end users and settings.
Originality/value
The set of recommendations for subsequent user-engaged research design and methods span the process of development, research and implementation. The authors hope that these recommendations will foster collaborations across disciplines, encourage researchers and therapists to adopt VR/AVGs more readily, and lead to efficacious and effective treatment approaches for rehabilitation clients.
Keywords: Virtual reality, Rehabilitation, Disability, Implementation science, Knowledge translation, Video games
Introduction
Virtual reality and active video game (VR/AVG) systems are becoming increasingly popular treatment modalities in rehabilitation (Laver et al., 2017), with evidence building to support skill acquisition in a variety of populations (Darekar et al., 2015). Given the diversity of VR/AVG system options, occupational and physical therapists (OTs and PTs) who provide VR-based therapy must engage in complex clinical decision making about the selection of appropriate systems and games that are congruent with their clients’ abilities and treatment goals (Glegg et al., 2014). A recent survey of VR/AVG use and knowledge needs of PTs and OTs practicing in Canada found that 46 percent had used VR/AVG at least once, but only 12 percent reported current use, primarily of Nintendo Wii/WiiFIT systems (Levac et al., 2017). Further, 70 percent of those surveyed wanted more educational resources to help them become familiar with using AVGs in clinical practice. Therapists who would like to integrate VR/AVGs clinically shoulder much of the decision-making burden to ensure a “just-right-fit” for their clients. However, lack of knowledge about VR/AVG system selection, implementation in practice and outcome assessment were common barriers to using VR/AVGs identified by survey participants (Levac et al., 2017).
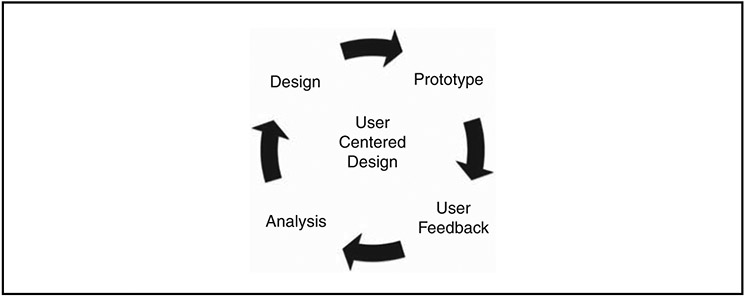
Knowledge translation (KT) refers to the process of moving evidence into action to improve the healthcare system and the health outcomes it facilitates for clients (Graham et al., 2007). KT interventions aim to enhance knowledge or skills to target the barriers and facilitators of change to promote the uptake of evidence (Graham et al., 2007; Scott et al., 2012). Ideally, both researchers and knowledge users (otherwise known as end users) are involved throughout the KT process. A few frameworks exist that describe varying levels of end-user involvement (UI). The “Knowledge to Action” framework developed by Graham et al. (2006) explicitly describes end UI during the “Action Cycle” portion of the KT process. However, the framework falls short of providing direct recommendations about involving users in the “Knowledge Creation funnel” phase. The User Centered Design Cycle (Figure 1) is another framework more commonly used in technology and VR development (Lange et al., 2010; Proffitt and Lange, 2013). This Cycle is also less than explicit about when and how end users are involved in the process, leaving this decision making to the researchers. Research on UI in software and technology development has demonstrated that nearly 68 percent of studies reported positive outcomes at some point in the process (Bano and Zowghi, 2015). However, the nature of UI varies tremendously; the “team” of researchers is generally not diverse in expertise, and healthcare practitioners are oftentimes not involved at all (Bano and Zowghi, 2015).
Figure 1.
The User Centered Design Cycle as applied in VR and AVG development for rehabilitation
Integrated KT, the process of involving end users within an interdisciplinary team (Gagliardi et al., 2015), is one method to ensure that the expertise and perspectives of the end users are incorporated. An interdisciplinary team can include OTs, PTs, physicians, other allied health professionals, clients and caregivers. In addition, specific to technology-based integration is the inclusion of industry partners, such as VR/AVG developers and software engineers. This integrated KT approach can be utilized for research evaluating both adoption of commercially available VR/AVG systems as well as the development, testing and implementation of rehabilitation-specific systems.
Effective and appropriate design for the end user can promote adherence, improved function and clinical effectiveness (McDonagh and Thomas, 2013). Conversely, poor compatibility with therapists’ usage preferences and with clients’ abilities and interests and low perceived therapeutic value can hinder adoption (Glegg et al., 2013; McDonagh and Thomas, 2013). For example, although commercial AVG systems present engaging graphics and a great variety of games, they do not allow for necessary control over software parameters to support adequate activity grading for clients with a range of cognitive and physical impairments (Lange et al., 2009). For example, in contract to rehabilitation-specific systems, non-customized AVG systems have limited task difficulty and modification options. This reality can have a significant impact on therapists’ adoption of the technology and can influence client motivation to participate in the repetitive interventions required for motor learning (Glegg et al., 2017; Levac et al., 2016). We propose that a strong match to user needs and goals is essential to support evidence-based, state-of-the-art technologies in delivering optimal therapy outcomes.
Therefore, the purpose of this paper is threefold. First, we will outline four case examples in which we were more and less successful in involving therapist and client end users in VR/AVG implementation research. We then describe the benefits to this process, the challenges faced and the lessons learned. Finally, we provide a set of recommendations for UI in the process of KT for VR/AVGs in rehabilitation clinical practice.
Case examples
Case 1: pitfalls of end users as research participants instead of research colleagues
The acquisition of a rehabilitation-specific, engineer-built VR system – GestureTek Health’s Interactive Rehabilitation Exercise System (IREX) – by two stroke rehabilitation hospitals was the impetus for this research. To use the IREX, patients stand in front of a green screen and view their image integrated in the virtual environment where they can interact with virtual objects using full body movements. At the time of this research, the IREX was the first and most well-studied motion-capture-based gaming technology in rehabilitation. However, it was not being used in these two clinical contexts. To address this underuse issue, and to situate IREX use in a theoretical framework of relevance to stroke rehabilitation, we undertook a KT intervention with the goal of increasing therapist knowledge about how to use the IREX to promote motor learning in adults undergoing inpatient rehabilitation for acute stroke. A secondary goal was to promote increased use of the IREX following the study intervention.
We developed online KT modules introducing therapists to the IREX, reviewing relevant motor learning strategies, and explaining how to use the IREX to promote motor learning principles. We also provided in-person individual and group training in IREX use. In total, 11 therapists volunteered to participate in the study and delivered a total of 107 VR-based sessions to 34 clients with stroke. On the assessing determinants of prospective uptake of virtual reality (ADOPT-VR) instrument, therapists improved their scores on the perceived behavioral control, self-efficacy and facilitating conditions scales, but intention to use VR did not change, with no decrease in the frequency of perceived barriers to VR use (Levac et al., 2016b, a). In addition, using validated self-report and observer-rated instruments, therapists improved knowledge about motor learning but no changes in clinical reasoning, use of motor learning strategies or IREX use were observed (Levac et al., 2016b, a). Therapists reported that clients were motivated to use the IREX, but that too many environmental barriers existed for strong clinical implementation of this particular system (Levac et al., 2016a, b).
Subsequent to the study, we recognized several flaws in our study design. In particular, the intended end users (therapists) were not involved in developing the study procedures, identifying knowledge that would be beneficial to support IREX use or development of any of the KT resources. The study also did not address the practical barriers that were present from before study onset. In particular, logistical factors related to IREX acquisition were a significant issue, including its location far away from the regular therapy room, the fact that it required a 1:1 therapist/client ratio, and its many software issues. Although therapists reported that clients were motivated and engaged with the IREX, the also expressed frustration due to perceived mismatches between games and client therapeutic goals. This experience illustrated that when end users are not involved at the beginning of the research process to make decisions about what they would like to learn and how they would like to learn it, and when their needs are not considered in technology integration, well-designed KT interventions can improve knowledge and attitudes but have unfortunate little impact on actual use. As such, targeting both knowledge needs and environmental barriers is important, and should be supported by involving both end users and the administrators who are in practical, decision-making roles in the research design.
Case 2: a student train-the-trainer model for knowledge translation
The Rapael SmartGlove (Neofect, Inc.) is a novel technology for hand and wrist rehabilitation. The SmartGlove consists of a wearable, flexible “glove” that contains a gyroscope and accelerometer to track movement wrist, hand and fingers. The SmartGlove is paired (via Bluetooth) with a touch-screen computer that displays interactive games and movement assessment results. The SmartGlove has been tested in a small study (Shin et al., 2016) and showed promising findings, particularly for those who have experienced a stroke. The company offers a home version for rent by clients and families. The system is touted as being easy to learn and requires minimal training (by both clients and therapists). However, the company only has training materials in beta versions and reached out for input on the materials.
At the University of Missouri, the Department of Occupational Therapy provides a no-fee, student-run clinic called TigerOT Clinic. This site served as a prime location for developing and testing training materials for KT relative to the Rapael SmartGlove. Furthermore, the end users (OT students) were involved in the design of the training materials as well as being the receivers of the training. The train-the-trainer approach to clinical education and program implementation is based in public health and community-based programs. It has been successfully utilized in occupational therapy education to develop clinical skills in graduate-level students (Doyle et al., 2008).
Two OT students learned how to use the Rapael SmartGlove using provided manuals and internet resources from Neofect, Inc. Based on a draft model of a competency assessment, the two OT students created a competency assessment for clinical SmartGlove use. This version was revised several times through iterative clinical testing. The two OT students became the trainers for the SmartGlove. The trainers trained five OT students in the clinical use of the Rapael glove for a client being treated in the TigerOT Clinic. The competency assessment was administered before training, after the training and after five weeks of using the SmartGlove in the TigerOT clinic with the client. At the end of the five weeks, a usability scale was also administered to both the OT student and the client that used the SmartGlove.
OT students had an average competency rating pre-training of 1.3/5 (not at all competent) and moved to an average of 4.8/5 (very competent) both post-training and post-intervention. Further, the OT students rated their clinical decision-making skills relative to the SmartGlove low pre-training and very high after training and after the intervention period. The OT students rated the device 4.4/5 (fairly usable) on the usability scale and the clients rated the device 4/5 on the usability scale. The two trainers reported that they felt very successful in delivering the training and stated that the competency checklist helped to guide the training sessions with OT students. The OT students reported that they felt very comfortable during the training sessions and found it to be more meaningful coming from peers rather than from a company salesperson or a faculty researcher. Thus, a train-the-trainer approach to KT in VR and technology is feasible and potentially effective. A larger study over a longer period of time is currently in progress.
The use of a train-the-trainer model is feasible as an initial step for KT into clinical practice. The two trainers used an iterative process to design a competency assessment that then guided their approach to training. The involvement of the OT students and feedback from the clinic clients further enhanced the process of KT.
Case 3: end-user engagement in the evaluation of technology implementation efforts
The Functional Engagement in Assisted Therapy through Therapy Robotics (FEATHERS) system is a rehabilitation-specific system that integrates adapted commercially available AVG technology (PlayStation2) and mainstream gaming applications from a social media platform (Facebook) using custom-designed computer software (Glegg et al., 2016). The system was designed for use with adults and adolescents with hemiparesis as the result of conditions, such as cerebral palsy, stroke and acquired brain injury (Shirzad et al., 2015). System design requires participants to engage in bimanual upper limb movements in order to interact with the games, while affording them tremendous variety in game selection, and the potential for interaction with peers and their therapist through the social media platform (Glegg et al., 2016). FEATHERS was designed by engineering researchers and computer scientists through a partnership with industry, and in collaboration with community therapists. Clients, families and therapists were engaged as participants in the early design phases of the project to contribute input on the design of the system to meet their needs (Shirzad et al., 2015). Usability testing with clients followed, which led to the refinement of the technology prior to the launch of a clinical trial to evaluate its effectiveness and feasibility as a home-based treatment tool (Glegg et al., 2016).
During this implementation phase, the multi-disciplinary research team included mechanical and biomedical engineers, computer scientists, OTs, a kinesiologist and a PT/knowledge broker. In addition to conducting the clinical trial, the team gathered qualitative data from three adolescent and seven adult participants about their experiences engaging in FEATHERS-based home therapy, and conducted a debriefing session with 12 research team members and community collaborators to share lessons learned (Valdes et al., 2018). Key findings of these engagement methods included the identification of advantages of the FEATHERS system, including the variety of games, the option for participants of communicating with the team through various channels, and the technology’s perceived therapeutic benefit by some participants. Also identified were challenges associated with the technology itself (e.g. lack of ability to grade challenge or monitor compensatory movements and accessibility), the communication processes in place to support clients/families and therapists in implementing and evaluating the intervention (e.g. accessing technical support and methods of reporting client progress), and the need for additional training (Valdes et al., 2018). Each of these areas were pertinent to both the clients and the treating therapists.
While having research team members with clinical backgrounds as part of the research team was extremely valuable, additional input from the therapists implementing the technology as part of the research process, as well as from the study participants, was necessary to gather a comprehensive understanding of the range of barriers to the technology’s clinical implementation. A balance of perspectives, and a decision-making process that values each of them in motivating action, can help to guide the refinement of VR/AVG design, as well as anticipate and plan for the mitigation of barriers to the technology’s successful implementation.
Case 4: knowledge and research outcomes from an interdisciplinary research team and iterative end-user involvement
Following the release of the Nintendo Wii in 2006 and Nintendo WiiFit in 2007, a series of studies were undertaken with therapists and client populations with the aim of identifying the benefits, challenges and appropriate implementation of these technologies in the clinical setting. The research team (PT, OT, psychologist, stroke survivor, computer scientist, biomedical and mechanical engineers) explored the usability of the Nintendo Wii/WiiFit and PlayStation2 EyeToy in the clinical setting through focus groups and structured mixed methods observational research with therapists and people with neurological impairments. Findings demonstrated that although commercial AVGs can motivate people to move, a need for more control over the game features and tasks existed, in order to use the technologies within the clinical setting (Lange et al., 2009). The findings from this and subsequent research (Flynn and Lange, 2010) were incorporated into a two-day workshop series that was presented at national and international conferences, universities and rehabilitation hospitals and clinics across the USA. These workshops provided researchers, developers, therapists and potential end users with the basic information they needed to begin to use and/or develop/design game-based technologies for exercise and rehabilitation. These workshops were well-received by therapists and researchers.
Since then, we addressed the challenge using user-centered iterative design principles to create low cost home-based video game systems for motor and cognitive assessment and rehabilitation for people with stroke, acquired brain injury, spinal cord injury and for older adults at risk of falls. The key advantage of designing these games was to provide the therapist and/or client with the ability to alter elements of game play in order to tailor treatment tasks for individual users and expand the use of these tasks to a wider range of level of ability. The use of games for rehabilitation must maintain the goals of existing therapies, whilst improving motivation to perform therapeutic exercise programs. Through our structured clinical observations, focus groups and user testing with input from clients and therapists at more than ten sites, we developed and adapted a suite of low-cost game-based rehabilitation tools targeted at improving balance and cognitive rehabilitation (Lange et al., 2010, 2011, 2012; Proffitt and Lange, 2013). The activities within the systems included cognitive tasks and structured static and dynamic balance tasks. The usability of these technologies were evaluated through a series of usability tests at clinical sites run by researchers (observational mixed-methods design), the development of a user manual, and feedback gathered following trialing of the system at clinical sites (user testing, observations and interviews). The VR systems were also evaluated during a six-week individualized home-based exercise program for three people with stroke who had different levels of function (Proffitt and Lange, 2015). The VR system is currently being used in a modified form as an intervention in a multi-center randomized controlled trial for people with brain injury (Krch et al., 2016). The modifications were made because therapists at two sites reported difficulties setting up the individualized programs because there were too many options and it was overwhelming at times.
Therapists are keen to try new technologies but it is important that the right technology is chosen and that therapists are provided with the training and knowledge to adequately implement the intervention in the clinical setting. Commercial systems have a place if they are carefully considered, however, a greater scope exists for the implementation of customizable systems within the clinical setting. Through our work with therapists, we found that therapists want options and control; however, feedback also indicated at times that there was too much control and too many options that could become overwhelming. There is a need to balance what users want with the capacity of the end users and need for training, time to familiarize and learn a new system, set-up time, etc. (difference between plug and play vs needing training to effectively use the system) (Table I).
Table I.
Summary of cases including type of VR/AVG types of end users and outcomes
| Case | Target population | Treatment setting |
Type of VR/AVG | End users involved | Outcomes |
|---|---|---|---|---|---|
| 1 | Individuals with stroke | Inpatient stroke rehabilitation | Gesturetek IREX | PT, OT | Improved self-reported knowledge and attitudes No change in intention to use VR No change in VR use |
| 2 | Pro-bono clinic clients (uninsured/underinsured) | Pro-bono student-run outpatient clinic | Rapael SmartGlove | OT students | Successful training Student reported high levels of competence Target population reported good usability of system |
| 3 | Adolescents and adults with hemiparesis | Home-based rehabilitation | Adapted PlayStation2 controllers interfaced with existing games on social media platform | PT, OT, participants with hemiparesis | Perceived therapeutic benefit by target population Additional training necessary Awareness of communication preferences of end users during implementation |
| 4 | Individuals with stroke, brain injury, amputations, older adults at risk for falls | Outpatient clinic, hospital, home | Commercially available games, customized software paired with Microsoft Kinect® | PT, OT, individuals with disabilities (target population) | Support for use in the clinical setting Training workshops well-received by therapists and other end users |
Benefits and challenges
Table II summarizes the benefits and challenges faced in each of the cases. Taking these reflections one step further, we present lessons learned from our experiences to inform therapists and researchers interested in developing and implementing VR systems for rehabilitation.
Table II.
Summary of factors supporting success, challenges/barriers to implementation and lessons learned
| Case | Factors supporting success | Factors that are challenges/barriers | Lessons learned |
|---|---|---|---|
| 1 | Motivated end users Motivated clients |
Mismatch between technology requirements and setting needs Practical barriers not addressed |
Involve end users in selection of most relevant VR systems Design study with barriers and practical issues in mind Involve end users in goal setting relative to use of VR, then focus knowledge translation there |
| 2 | Students chose learning outcomes Train-the-trainer model removes “authority figure” |
Initial training time intensive Sustainability | Involving students can further enhance knowledge translation |
| 3 | Range of perspectives from end users were incorporated in all phases of research process | Balancing multiple perspectives against feasibility of technology refinement/integration Time required for additional training for therapists and clients |
Generating knowledge from multiple perspective is necessary Multiple perspectives can help mitigate current and future barriers to implementation |
| 4 | Commercially available systems accessible and affordable for clinic use Buy-in from end users Involving end users from the beginning and throughout the research process |
Evaluating and ensuring the technology is appropriate for the end user Balancing what end users want against how the system will be used Balancing what end users want with level of complexity of system |
Commercial systems should be utilized strategically Match the “right” technology to the “right” setting Too much control/choices in a system can be overwhelming for therapists |
Recommendations
Based on our lessons learned from the four cases, we present a series of recommendations for researchers and therapists who plan to develop and use VR/AVGs for rehabilitation. These recommendations build on the past nearly three decades of research in VR and video games for rehabilitation (Fluet and Deutsch, 2013; Laver et al., 2017; Rizzo and Kim, 2005; Wilson et al., 1997). As we move research out of laboratory settings and into clinics, homes and community-based settings, the recommendations we provide below are framed in a rich history of development and research. These recommendations can be modified for different practice settings and disciplines:
Recommendation 1: involve end users early in, and throughout the development, research and implementation processes (i.e. from conceptualization and design to implementation and evaluation). For example, leverage clinical expertise and client experience to co-develop system design, user-tailored operational manuals and clinical training resources that will facilitate capacity building for end users (Lange et al., 2009; Rizzo and Kim, 2005).
Recommendation 2: conduct a barriers assessment for implementation that engages all stakeholder groups (e.g. therapists, clients, healthcare administrators, etc.). This step will help to identify practical strategies that target the most significant barriers from different stakeholder perspectives, as a means of promoting success (Rizzo and Kim, 2005; Wilson et al., 1997).
Recommendation 3: understand health professionals’ clinical reasoning processes as a means of informing the features and functionality of VR systems that support game groupings and the ability to grade the degree of task challenge. This will help “match” the technology and the setting (including the demands of the therapist) (Laver et al., 2017).
Recommendation 4: consider a train-the-trainer model when working with a target population that is resistant to change or authority. Trainers must develop rapport with end user groups to maximize buy-in and eventual implementation (Doyle et al., 2008).
Recommendation 5: identify champions or mentors in implementation settings to support engagement, training and troubleshooting. Ongoing linkages to the technology developers and researchers may support uptake, and allow for continued knowledge exchange that could inform improvements of the system (Fluet and Deutsch, 2013).
Conclusion
Increasing end UI in VR/AVG implementation research may address issues related to poor clinical uptake. In the VR/AVG context, end users can be therapists, clients or technology developers/engineers. This paper presented four case scenarios describing the implementation of different VR/AVG systems and involving a variety of populations, end users and settings. We illustrate that a better match between VR/AVG system capabilities and client/therapist needs leads to improved end UI in all stages of VR/AVG implementation research. We identified common benefits of increasing buy-in and soliciting early on the knowledge and skills of therapists as well as input from the ultimate end users: people participating in rehabilitation. We discussed challenges of balancing the technology requirements with the needs and goals of the practice setting and of the end users. Our set of recommendations for subsequent user-engaged research design and methods span the process of development, research and implementation. We hope that these recommendations will foster collaborations across disciplines, encourage researchers and therapists to adopt VR/AVGs more readily, and lead to efficacious and effective treatment approaches for rehabilitation clients.
Contributor Information
Rachel Proffitt, Department of Occupational Therapy, School of Health Professions, University of Missouri, Columbia, Missouri, USA..
Stephanie Glegg, Department of Therapy, Sunny Hill Health Centre for Children, Vancouver, Canada..
Danielle Levac, Department of Physical Therapy, Movement and Rehabilitation Sciences, Northeastern University, Boston, Massachusetts, USA..
Belinda Lange, College of Nursing and Health Sciences, Flinders University, Adelaide, Australia..
References
- Bano M and Zowghi D (2015), “A systematic review on the relationship between user involvement and system success”, Information and Software Technology, Vol. 58, February, pp. 148–69. [Google Scholar]
- Darekar A, McFadyen BJ, Lamontagne A and Fung J (2015), “Efficacy of virtual reality-based intervention on balance and mobility disorders post-stroke: a scoping review”, Journal of Neuroengineering and Rehabilitation, Vol. 12 No. 1, pp. 46–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyle S, Gallagher J, Bell M, Rochford C and Roynane S (2008), “Establishing a ‘train the trainer’ education model for clinical skills development”, Nursing Older People, Vol. 20 No. 5, pp. 34–7. [DOI] [PubMed] [Google Scholar]
- Fluet GG and Deutsch JE (2013), “Virtual reality for sensorimotor rehabilitation post-stroke: the promise and current state of the field”, Current Physical Medicine and Rehabilitation Reports, Vol. 1 No. 1, pp. 9–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn SM and Lange BS (2010), “Games for rehabilitation: the voice of the players”, International Conference Disability, Virtual Reality & Associated Technologies, August, pp. 185–94. [Google Scholar]
- Gagliardi AR, Berta W, Kothari A, Boyko J and Urquhart R (2015), “Integrated knowledge translation (IKT) in health care: a scoping review”, Implementation Science, Vol. 11 No. 1, pp. 38–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glegg SM, Tatla SK and Holsti L (2014), “The GestureTek virtual reality system in rehabilitation: a scoping review”, Disability and Rehabilitation: Assistive Technology, Vol. 9 No. 2, pp. 89–111. [DOI] [PubMed] [Google Scholar]
- Glegg SM, Hung CT, Valdes BA, Kim BD and Van der Loos HF (2016), “Kinecting the moves: the kinematic potential of rehabilitation-specific gaming to inform the treatment of hemiparesis”, International Journal of Child Health and Human Development, Vol. 9 No. 3, pp. 351–60. [Google Scholar]
- Glegg SM, Holsti L, Velikonja D, Ansley B, Brum C and Sartor D (2013), “Factors influencing therapists’ adoption of virtual reality for brain injury rehabilitation”, Cyberpsychology, Behavior, and Social Networking, Vol. 16 No. 5, pp. 385–401. [DOI] [PubMed] [Google Scholar]
- Glegg SM, Holsti L, Stanton S, Hanna S, Velikonja D, Ansley B, Sartor D and Brum C (2017), “Evaluating change in virtual reality adoption for brain injury rehabilitation following knowledge translation”, Disability and Rehabilitation: Assistive Technology, Vol. 12 No. 3, pp. 217–26. [DOI] [PubMed] [Google Scholar]
- Graham ID and Tetroe J and KT Theories Research Group (2007), “Some theoretical underpinnings of knowledge translation”, Academic Emergency Medicine, Vol. 14 No. 11, pp. 936–41. [DOI] [PubMed] [Google Scholar]
- Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W and Robinson N (2006), “Lost in knowledge translation: time for a map?”, Journal of Continuing Education in the Health Professions, Vol. 26 No. 1, pp. 13–24. [DOI] [PubMed] [Google Scholar]
- Krch D, Ward I, Lange B, Kesten AG, Cording CM, Frank LE, Mejia M, Chervin K, König S, Chang CY and Rizzo A (2016), “A systematic delivery for multisensory balance impairment using virtual reality in TBI”, Archives of Physical Medicine and Rehabilitation, Vol. 97 No. 10, pp. e139–e40. [Google Scholar]
- Lange B, Flynn S and Rizzo A (2009), “Initial usability assessment of off-the-shelf video game consoles for clinical game-based motor rehabilitation”, Physical Therapy Reviews, Vol. 14 No. 5, pp. 355–63. [Google Scholar]
- Lange B, Flynn S, Proffitt R, Chang CY and Rizzo AS (2010), “Development of an interactive game-based rehabilitation tool for dynamic balance training”, Topics in Stroke Rehabilitation, Vol. 17 No. 5, pp. 345–52. [DOI] [PubMed] [Google Scholar]
- Lange B, Flynn S, Chang CY, Liang W, Si Y, Nanavati C and Chieng CL (2011), “Development of an interactive stepping game to reduce falls in older adults”, International Journal on Disability and Human Development, Vol. 10 No. 4, pp. 331–5. [Google Scholar]
- Lange B, Koenig S, Chang CY, McConnell E, Suma E, Bolas M and Rizzo A (2012), “Designing informed game-based rehabilitation tasks leveraging advances in virtual reality”, Disability and Rehabilitation, Vol. 34 No. 22, pp. 1863–70. [DOI] [PubMed] [Google Scholar]
- Laver KE, Lange B, George S, Deutsch JE, Saposnik G and Crotty M (2017), “Virtual reality for stroke rehabilitation”, Cochrane Database of Systematic Reviews, No. 11, pp. e1–e183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levac D, Glegg S, Colquhoun H, Miller P and Noubary F (2017), “Virtual reality and active videogame-based practice, learning needs, and preferences: a cross-Canada survey of physical therapists and occupational therapists”, Games for Health Journal, Vol. 6 No. 4, pp. 217–28. [DOI] [PubMed] [Google Scholar]
- Levac D, Glegg SM, Sveistrup H, Colquhoun H, Miller PA, Finestone H, DePaul V, Harris JE and Velikonja D (2016a), “A knowledge translation intervention to enhance clinical application of a virtual reality system in stroke rehabilitation”, BMC Health Services Research, Vol. 16 No. 1, pp. 557–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levac DE, Glegg SM, Sveistrup H, Colquhoun H, Miller P, Finestone H, DePaul V, Harris JE and Velikonja D (2016b), “Promoting therapists’ use of motor learning strategies within virtual reality-based stroke rehabilitation”, PloS One, Vol. 11 No. 12, pp. 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonagh D and Thomas J (2013), “Innovating alongside designers”, The Australasian Medical Journal, Vol. 6 No. 1, pp. 29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proffitt R and Lange B (2013), “User centered design and development of a game for exercise in older adults”, International Journal of Technology, Knowledge, & Society, Vol. 8 No. 5, pp. 95–112. [Google Scholar]
- Proffitt R and Lange B (2015), “Feasibility of a customized, in-home, game-based stroke exercise program using the Microsoft Kinect® Sensor”, International Journal of Telerehabilitation, Vol. 7 No. 2, pp. 23–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizzo AS and Kim GJ (2005), “A SWOT analysis of the field of virtual reality rehabilitation and therapy”, Presence: Teleoperators & Virtual Environments, Vol. 14 No. 2, pp. 119–46. [Google Scholar]
- Scott SD, Albrecht L, O’Leary K, Ball GD, Hartling L, Hofmeyer A, Jones CA, Klassen TP, Burns KK, Newton AS and Thompson D (2012), “Systematic review of knowledge translation strategies in the allied health professions”, Implementation Science, Vol. 7 No. 1, pp. 70–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin JH, Kim MY, Lee JY, Jeon YJ, Kim S, Lee S, Seo B and Choi Y (2016), “Effects of virtual reality-based rehabilitation on distal upper extremity function and health-related quality of life: a single-blinded, randomized controlled trial”, Journal of Neuroengineering and Rehabilitation, Vol. 13 No. 1, pp. 17–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirzad N, Valdes BA, Hung CT, Law M, Hay J and Van der Loos HF (2015), “FEATHERS, a bimanual upper limb rehabilitation platform: a case study of a user-centered approach in rehabilitation device design”, Proceedings of the 20th International Conference on Engineering Design, pp. e1–e10. [Google Scholar]
- Valdes BA, Glegg SM, Lambert-Shirzad N, Schneider AN, Marr J, Bernard R, Lohse K, Hoens AM and Van der Loos HF (2018), “Home-based rehabilitation gaming for hemiparesis: challenges and lessons learned”, Games for Health, Vol. 7 No. 3, pp. 197–207. [DOI] [PubMed] [Google Scholar]
- Wilson PN, Foreman N and Stanton D (1997), “Virtual reality, disability and rehabilitation”, Disability and Rehabilitation. Vol. 19 No. 6, pp. 213–20. [DOI] [PubMed] [Google Scholar]