Background:
Postoperative pain management in orthopaedic surgery accounts for a substantial portion of opioid medications prescribed in the United States. Understanding prescribing habits and patient utilization of these medications following a surgical procedure is critical to establishing appropriate prescribing protocols that effectively control pain while minimizing unused opioid distribution. We evaluated prescribing habits and patient utilization following elective orthopaedic surgical procedures to identify ways of improving postoperative opioid-prescribing practices.
Methods:
We performed a review of prescribing data of 1,199 procedures and gathered telephone survey results from 557 patients to determine the number of opioid pills prescribed postoperatively and the number of unused pills. The data were collected from adult patients who underwent 1 of the 5 most common elective orthopaedic procedures at our institution in fiscal year 2015: total hip arthroplasty, total knee arthroplasty, endoscopic carpal tunnel release, arthroscopic rotator cuff repair, or lumbar decompression. We converted all dosages to opioid equivalents of oxycodone 5 mg and performed analyses of prescribing patterns, patient utilization, and patient disposal of unused opioids.
Results:
Prescribing patterns following the 5 orthopaedic procedures showed wide variation. The median numbers of oxycodone 5-mg equivalent opioid pills prescribed upon discharge were 90 pills (range, 20 to 330 pills) for total hip arthroplasty, 90 pills (range, 10 to 200 pills) for total knee arthroplasty, 20 pills (range, 0 to 168 pills) for endoscopic carpal tunnel release, 80 pills (range, 18 to 100 pills) for arthroscopic rotator cuff repair, and 80 pills (range, 10 to 270 pills) for lumbar decompression. Thirty-seven percent of patients overall requested and received at least 1 refill. The mean number of total pills prescribed (and standard deviation) including refills was 113.6 ± 75.7 for total hip arthroplasty, 176.4 ± 108.0 for total knee arthroplasty, 24.3 ± 29.0 for carpal tunnel release, 98.2 ± 59.6 for rotator cuff repair, and 107.4 ± 64.4 for lumbar decompression. Participants reported unused opioid medication in 61% of cases. During the study year, >43,000 unused opioid pills were prescribed. Forty-one percent of patients reported appropriate disposal of unused opioid pills.
Conclusions:
Prescribing patterns vary widely, and a large amount of opioid medications remains unused following elective orthopaedic surgical procedures. Effective prescribing protocols are needed to limit this source of potential abuse and opioid diversion within the community.
Prescription opioid use in the United States has increased markedly over the past 3 decades1. In 1986, Portenoy and Foley demonstrated effective pain management with chronic prescription opioid use2,3. Following a period of increased research on opioid effectiveness bolstered by pharmaceutical marketing efforts, in 1996, the American Pain Society adopted the phrase “pain as the fifth vital sign.”4,5 Additional initiatives by the Veterans Health Administration and the Joint Commission (formerly known as the Joint Commission on Accreditation of Healthcare Organizations) ushered in the paradigm shift in providers treating chronic pain with prescription opioid medication4-7. The ramifications of increased opioid prescribing appeared soon after when, in 2008, drug overdoses surpassed automobile collisions as the leading cause of accidental death in the United States8. In 2015, opioids were involved in 33,091 deaths, the highest number in a year to date7. Almost half of these deaths involved a prescription opioid8. The remaining deaths resulted from heroin use, and approximately 70% of heroin users cite use of a prescribed opioid as the inciting cause of their addiction9.
Federal and state government agencies have instituted multiple programs to regulate and track opioid-prescribing practices10,11. One important goal of these programs is to reduce the excess amount of opioid medications prescribed to patients, as illicit diversion of these medications may be a substantial contributor to opioid-related abuse11.
The burden of postoperative musculoskeletal pain is substantial, and appropriate use of opioid medication in its treatment remains a goal for practitioners12-14. Recent studies in the orthopaedic literature have highlighted that substantial variation and overprescribing occur after surgical procedures15-18. For example, Kim et al. showed that patients undergoing an upper-extremity surgical procedure used only 34% of the opioid medications prescribed18.
Orthopaedic surgeons are the third-highest group of opioid prescribers among physicians, accounting for almost 8% of all opioid prescriptions in the United States6. The orthopaedic literature has presented trends and risk factors associated with opioid use following surgical procedures19-24. Recent studies have highlighted a pattern of patients receiving excess opioid medication after undergoing orthopaedic surgery; however, to our knowledge, there have been few data to suggest an optimal supply of pain medication postoperatively18,25,26. We are aware of no comprehensive guide to inform surgeons on typical opioid consumption following common orthopaedic procedures.
The purpose of this study was to determine how much postoperative pain medication was being prescribed, how much of the medication was being taken, and the minimal number of opioid pills optimally needed to treat postoperative pain following 5 common elective orthopaedic procedures.
Materials and Methods
Study Design
Internal review board approval was obtained prior to the initiation of the study. We obtained prescribing data from the electronic medical records of all patients undergoing the 5 most commonly performed elective orthopaedic procedures at our institution in fiscal year (FY) 2015: total hip arthroplasty, total knee arthroplasty, endoscopic carpal tunnel release, arthroscopic rotator cuff repair, and lumbar spine decompression (laminectomy, facetectomy, and foraminotomy with or without arthrodesis).
Our data set included patients treated by 15 fellowship-trained orthopaedic surgeons.
We included all adult (≥18 years of age), English-speaking patients who were followed postoperatively for a minimum of 90 days and for whom postoperative prescription data were available. We excluded trauma cases and any patients who underwent a revision procedure for any reason. Also excluded were patients who underwent simultaneous bilateral procedures. For patients who underwent staged bilateral procedures, we included both procedures. Patients who continued to require prescription opioid medication for postoperative pain control for >90 days postoperatively were excluded from our aggregate calculations. These patients were removed from aggregate calculations based on established expectations for postoperative opioid independence and our department’s protocol for involving chronic pain specialists in opioid management for those requiring continued opioid prescriptions at 90 days postoperatively20,27.
Using the prescribing data recorded in the electronic medical records, we recorded the number, dosage, and formulation of opioid medication prescribed upon discharge from our facility. Detailed refill data were also recorded to calculate the entire duration and amount of postoperative opioid therapy. Using opioid equianalgesic charts, we converted dosages to an oxycodone 5-mg standard to better assess the number of pills prescribed28,29. We also noted whether or not the patient had been taking opioids in the 30-day period prior to the surgical procedure.
For the second portion of the study, we conducted telephone interviews of patients who met our inclusion criteria and had undergone the surgical procedure in the second half of FY2015 to obtain information with regard to opioid utilization and pain management satisfaction. We contacted eligible patients using telephone numbers recorded in the electronic medical record and classified respondents as “could not be reached” if we were unable to reach a respondent after 5 telephone attempts. The data were captured using a uniform telephone survey and were modeled using an equation derived by Hill et al. in a report on opioid prescribing following general surgical procedures30. We asked patients how much of their opioid medication was remaining after they completed recovery and assigned “% remaining” estimations based on their responses. Patients who had a full prescription remaining were assigned 100% remaining. Patients who had more than half but not a full prescription remaining were assigned 75% remaining. Patients who had less than half but not an empty prescription remaining were assigned 25% remaining. Patients who had no pills remaining were assigned 0% remaining30. We multiplied these percentages by the number of pills last prescribed to determine the excess number of pills.
We additionally queried patients on methods of disposal of unconsumed pills. We offered 4 choices to account for their excess pills: (1) had appropriately disposed of the pills; (2) still had excess pills; (3) did not know what happened to the pills; and (4) other. If patients reported that they still had remaining pills, we instructed them on appropriate disposal methods using the U.S. Food and Drug Administration (FDA) official recommendations for opioid disposal31.
Statistical Methods
We assessed age for distribution and association with the respective procedure using the Student t test. Categorical variables (sex, race, preoperative opioid use) were evaluated using the chi-square test and are presented using counts and percentages.
After calculating summary statistics of the prescribing data, we calculated the number of pills prescribed on discharge, the overall number of pills prescribed, and the overall number of pills taken using the percentage remaining data from the telephone surveys. Distributions of the total number of pills taken per procedure were plotted, facilitating an analysis of prescribing numbers, refill rates, and projected excess pill numbers. Additional outcome measures including refill rates, the number of unconsumed pills, and satisfaction scores were adjusted for the main covariates (age, sex, preoperative opioid use).
We conducted a subanalysis of survey responses regarding postoperative satisfaction with pain control by surgical procedure by performing multivariate logistic regression with relevant covariates. We also performed an adjusted multivariate logistic regression on patients who continued to take opioid medication longer than 90 days postoperatively to identify any association with the procedure and preoperative opioid use.
Finally, we performed a multivariate adjusted linear regression to determine which exposures proved to be significant, which was defined as p < 0.05, in their association with the total number of postoperative opioid pills prescribed.
Results
Prescribing Data
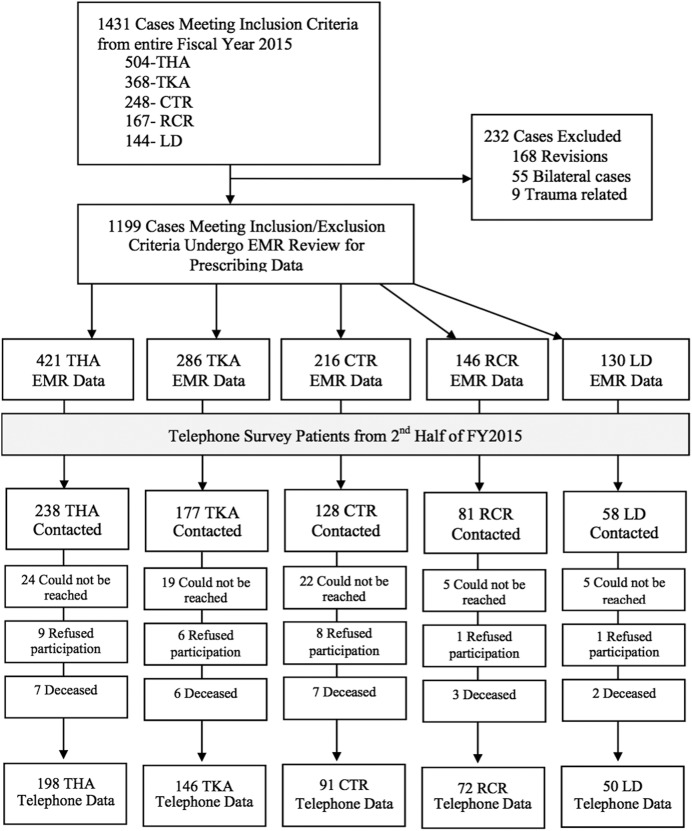
In our study, 1,199 procedures on 1,159 distinct patients met the inclusion and exclusion criteria for review of prescription data following an orthopaedic surgical procedure. The number of cases for each elective procedure was 421 for total hip arthroplasty, 286 for total knee arthroplasty, 216 for endoscopic carpal tunnel release, 146 for arthroscopic rotator cuff repair, and 130 for lumbar decompression (Fig. 1). Forty-seven patients were then excluded from primary analysis for postoperative opioid use that continued for >90 days postoperatively.
Fig. 1.
Study flow diagram demonstrating inclusion in prescribing data review, inclusion in telephone survey, attrition from lack of telephone contact, and exclusion at each stage of the study. THA = total hip arthroplasty, TKA = total knee arthroplasty, CTR = endoscopic carpal tunnel release, RCR = arthroscopic rotator cuff repair, LD = lumbar decompression (with or without arthrodesis), EMR = electronic medical record, and FY = fiscal year.
For the patient’s initial discharge prescription, providers prescribed opioid pills (oxycodone 5-mg equivalent) at a median of 90 pills (range, 20 to 330 pills) following total hip arthroplasty, a median of 90 pills (range, 10 to 200 pills) following total knee arthroplasty, a median of 20 pills (range, 0 to 168 pills) following endoscopic carpal tunnel release, a median of 80 pills (range, 18 to 100 pills) following arthroscopic rotator cuff repair, and a median of 80 pills (range, 10 to 270 pills) following lumbar decompression.
Thirty-seven percent of patients overall requested and received at least 1 refill prescription within the initial 90-day postoperative period (Table I).
TABLE I.
Summary of Patient Demographic Characteristics and Opioid Prescriptions from Electronic Medical Record Data*
| Characteristics | Total Hip Arthroplasty (N = 421) | Total Knee Arthroplasty (N = 286) | Endoscopic Carpal Tunnel Release (N = 216) | Arthroscopic Rotator Cuff Repair (N = 146) | Lumbar Decompression (with or without Arthrodesis) (N = 130) | P Value† |
| Age‡ (yr) | 65.2 ± 10.7 | 65.7 ± 9.9 | 59.6 ± 14.5 | 60.6 ± 9.7 | 65.6 ± 12.1 | 0.301 |
| Male sex§ | 203 (48%) | 125 (44%) | 90 (42%) | 100 (68%) | 68 (52%) | 0.004 |
| White race§ | 416 (99%) | 284 (99%) | 212 (98%) | 141 (97%) | 128 (98%) | 0.243 |
| Cases with preoperative opioid use§ | 79 (19%) | 49 (17%) | 32 (15%) | 25 (17%) | 26 (20%) | 0.717 |
| Cases with postoperative opioid use >90 days§ | 19 (5%) | 21 (7%) | 1 (0.5%) | 4 (3%) | 2 (2%) | 0.001 |
| Opioid pills prescribed upon discharge | <0.001 | |||||
| Mean‡ | 78.9 ± 35.8 | 82.8 ± 25.1 | 20.3 ± 17.9 | 74.6 ± 27.9 | 81.6 ± 37.5 | |
| Median | 90 | 90 | 20 | 80 | 80 | |
| Range | 20 to 330 | 10 to 200 | 0 to 168 | 18 to 100 | 10 to 270 | |
| Cases with postoperative opioid refills§ | 167 (40%) | 193 (67%) | 18 (8%) | 47 (32%) | 48 (37%) | <0.001 |
| Total opioid pills prescribed including refills‡# | 113.6 ± 75.7 | 176.4 ± 108.0 | 24.3 ± 29.0 | 98.2 ± 59.6 | 107.4 ± 64.4 | <0.001 |
Summary statistics of 1,199 elective orthopaedic procedures in FY2015 obtained from prescribing data in hospital records. Bilateral procedures and cases requiring revisions excluded. Pills are listed in oxycodone 5-mg equivalents.
These p values were determined by a Student t test for continuous characteristics (age, total opioid pills) and a chi-square test for categorical characteristics (sex, race, cases) by surgical category and refer to the comparison between surgery types.
The values are given as the mean and the standard deviation.
The values are given as the number of cases, with the percentage in parentheses.
This category does not include patients using chronic postoperative opioids.
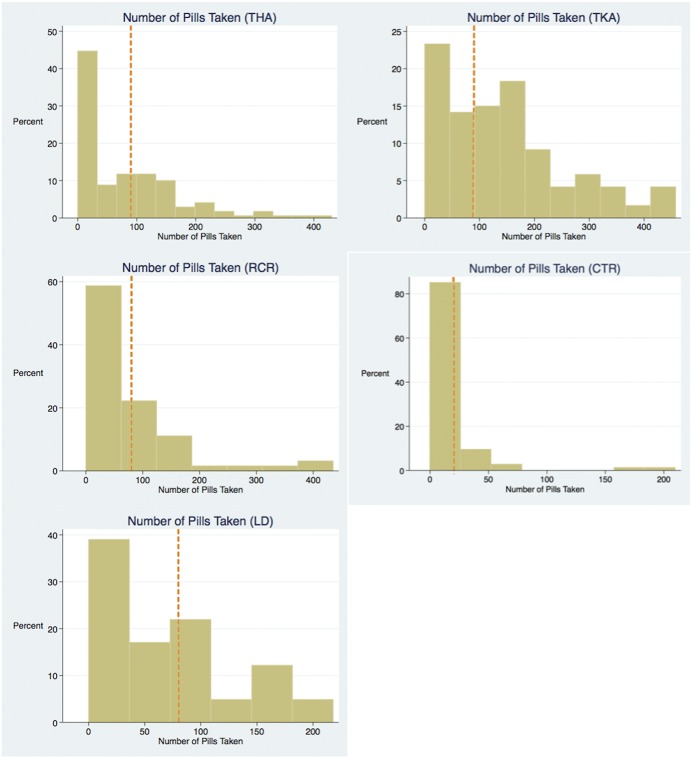
The mean number of opioid pills prescribed (and standard deviation) including refills was 113.6 ± 75.7 (range, 30 to 560) for patients undergoing total hip arthroplasty, 176.4 ± 108.0 (range, 10 to 480) for patients undergoing total knee arthroplasty, 24.3 ± 29.0 (range, 0 to 220) for patients undergoing endoscopic carpal tunnel release, 98.2 ± 59.6 (range, 30 to 435) for patients undergoing arthroscopic rotator cuff repair, and 107.4 ± 64.4 (range, 14 to 364) for patients undergoing lumbar decompression (Fig. 2).
Fig. 2.
Box plots of median (middle line in box) and interquartile range (box) of total number of opioid pills prescribed (blue) and total pills taken (red) following orthopaedic procedures in FY2015. The whiskers indicate the range. All pills are shown as an oxycodone 5-mg equivalent. THA = total hip arthroplasty, TKA = total knee arthroplasty, RCR = arthroscopic rotator cuff repair, CTR = endoscopic carpal tunnel release, and LD = lumbar decompression (with or without arthrodesis).
Survey Results
From the second half of FY2015, 682 patients were eligible to be included in the telephone survey portion of the study, and 557 patients participated in the survey questions. Of the 125 nonparticipants, 75 could not be reached, 25 did not wish to participate, and 25 had died (Fig. 1). At 17.6%, survey participants had a lower recorded percentage of preoperative opioid use (p = 0.039) compared with nonparticipants at 24.0%; there were no other documented differences between the populations.
Using the respondents’ answers to the question regarding the amount of opioid prescription remaining, we were able to calculate the sum of all opioids prescribed (first prescription and refills) and to subtract the excess pills reported (the percentage remaining multiplied by the final prescription number), giving us the amount of medication taken. The mean total number of opioid pills taken was 80.8 ± 83.8 pills for patients undergoing total hip arthroplasty, 146.9 ± 116.4 pills for patients undergoing total knee arthroplasty, 15.9 ± 32.0 pills for patients undergoing endoscopic carpal tunnel release, 79.8 ± 88.8 pills for patients undergoing arthroscopic rotator cuff repair, and 70.7 ± 62.0 pills for patients undergoing lumbar decompression (Table II).
TABLE II.
Opioid Utilization Data from Postoperative Telephone Survey*
| Characteristics | Total Hip Arthroplasty (N = 238) | Total Knee Arthroplasty (N = 177) | Endoscopic Carpal Tunnel Release (N = 128) | Arthroscopic Rotator Cuff Repair (N = 81) | Lumbar Decompression (with or without Arthrodesis) (N = 58) |
| No. patients surveyed | 198 | 146 | 91 | 72 | 50 |
| Declined survey, could not be reached, or had died† | 40 (17%) | 31 (18%) | 37 (29%) | 9 (11%) | 8 (14%) |
| Opioid pills prescribed‡ | 110.9 ± 75.5 | 167.3 ± 108.0 | 26.8 ± 29.1 | 103.9 ± 59.6 | 103.7 ± 64.4 |
| Pills taken‡§ | 80.8 ± 83.8 | 146.9 ± 116.4 | 15.9 ± 32.0 | 79.8 ± 88.8 | 70.7 ± 62.0 |
| Pills remaining‡§ | 31.9 ± 29.4 | 28.9 ± 31.7 | 11.2 ± 11.1 | 25.5 ± 24.6 | 29.3 ± 37.1 |
| Satisfaction with postoperative pain control# | 4.6 | 4.5 | 4.8 | 4.5 | 4.3 |
| Appropriate disposal** of unused pills† | 74 (37%) | 59 (40%) | 41 (45%) | 32 (44%) | 21 (42%) |
These were telephone survey respondents who underwent an orthopaedic surgical procedure during FY2015. All pills were adjusted to oxycodone 5-mg equivalents.
The values are given as the number of patients, with the percentage in parentheses.
The values are given as the mean and the standard deviation.
This category does not include patients who had chronic postoperative opioids.
The values are given as the mean score based on a Likert scale of 1 to 5.
The disposal was in accordance with the FDA recommendations.
Participants reported having unused opioid medication in 61% (340 of 557) of the cases. The mean number of unconsumed pills was 31.9 pills for patients undergoing total hip arthroplasty, 28.9 pills for patients undergoing total knee arthroplasty, 11.2 pills for patients undergoing endoscopic carpal tunnel release, 25.5 pills for patients undergoing arthroscopic rotator cuff repair, and 29.3 pills for patients undergoing lumbar decompression (Table II). Applying these mean unconsumed amounts to the overall number of patients undergoing these procedures at our institution in a single fiscal year results in an estimated 43,216 unused pills.
Patient satisfaction with postoperative pain control was generally high for all 5 procedures as they all registered a >83% overall satisfaction rate (defined by measures of 4 “somewhat satisfied” or 5 “very satisfied” on a 5-point Likert scale) (Fig. 3). Satisfaction was highest for endoscopic carpal tunnel release (mean, 4.8 of 5) and lowest for lumbar decompression (mean, 4.3 of 5). Logistic regression of postoperative satisfaction demonstrated a significant increase in satisfaction associated with patients who were >75 years of age compared with a reference group of patients who were <55 years of age (odds ratio [OR], 2.70; p = 0.011). Preoperative opioid use was not associated with satisfaction (OR, 1.00; p = 0.986).
Fig. 3.
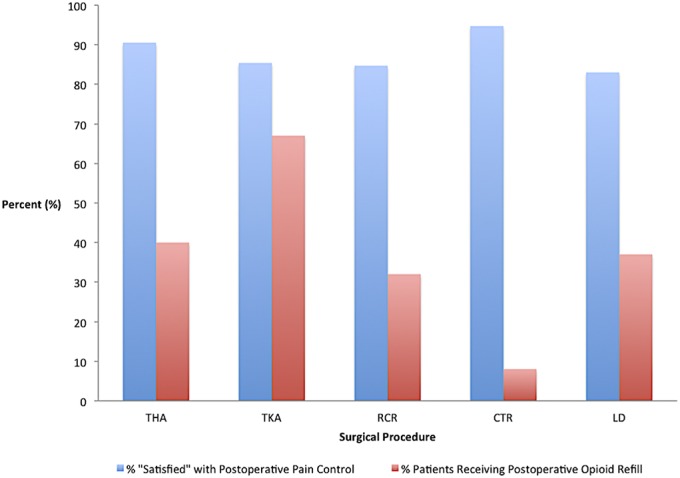
Bar graph of rates for postoperative opioid refill prescriptions (red) and patient satisfaction with postoperative pain control (blue) as denoted by a response of “satisfied” or “very satisfied” on telephone survey. TKA = total hip arthroplasty, THA = total knee arthroplasty, RCR = arthroscopic rotator cuff repair, CTR = endoscopic carpal tunnel release, and LD = lumbar decompression (with or without arthrodesis).
When asked about unused opioid disposal, 41% of patients stated that they had appropriately disposed of excess pills, 15% stated that they still had the excess pills, 8% said that they did not know what happened to the excess pills, and 36% said “other” (Fig. 4).
Fig. 4.
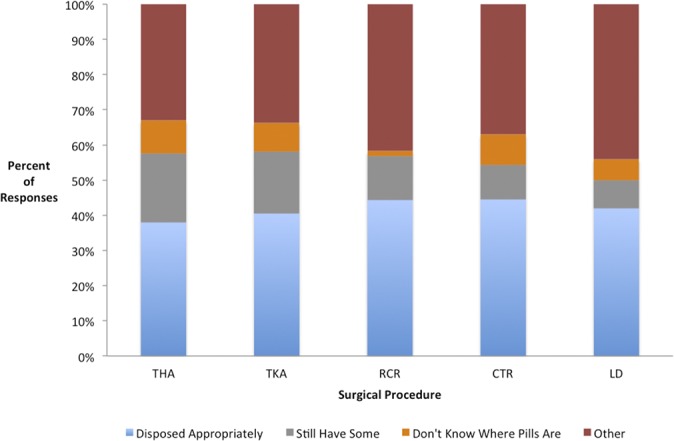
Stacked bar graph showing how patients disposed of unused opioid pills (by procedure). Less than half of respondents reported appropriate disposal of unused pills in every surgical procedure. Blue denotes appropriate disposal (per the FDA), gray denotes patients who still have remaining pills, orange denotes patients who reported not knowing where the unused pills were, and red denotes “other.” THA = total hip arthroplasty, TKA = total knee arthroplasty, RCR = arthroscopic rotator cuff repair, CTR = endoscopic carpal tunnel release, and LD = lumbar decompression (with or without arthrodesis).
Chronic Postoperative Opioid Use
Forty-seven patients continued to use opioid medications chronically for more than 90 days postoperatively (confirmed by an opioid prescription in the electronic medical record dated postoperative day 91 or later). Twenty-seven of these patients had been taking opioids preoperatively. As the remaining 20 patients had not been using opioid medications preoperatively, this implies that postoperative pain control contributed to chronic opioid use in approximately 2.0% (20 of 988 of the patients who were not taking opioids preoperatively and postoperatively) of our patients who were opioid-naïve preoperatively but became chronic opioid users postoperatively.
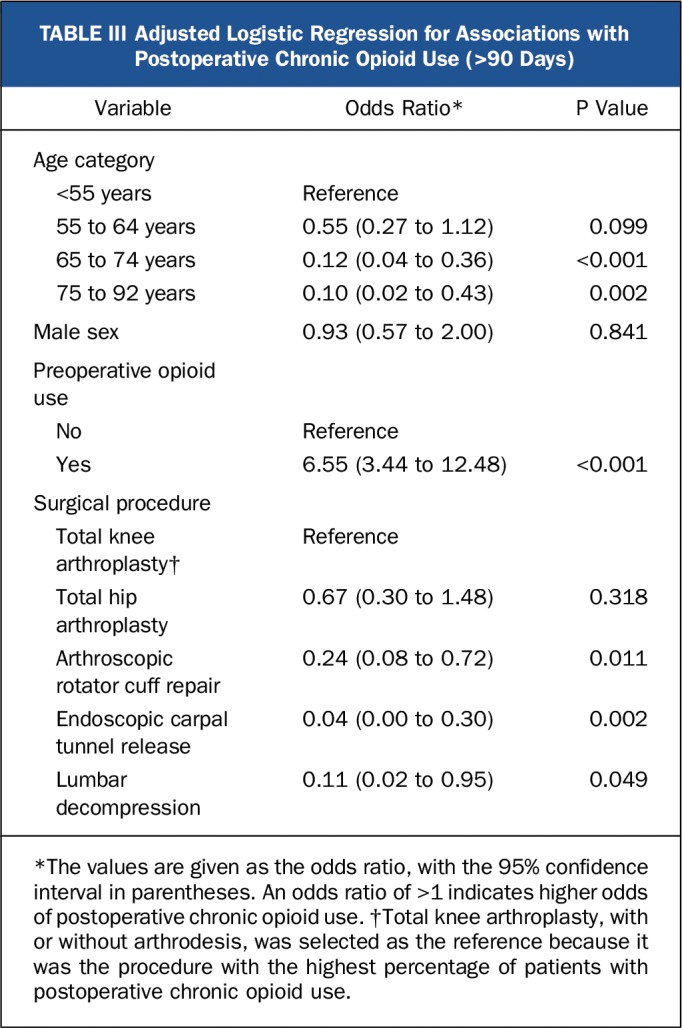
Multivariate logistic regression, adjusted for age, showed a significant association of increased risk of chronic postoperative opioid use in patients who were taking opioids preoperatively (OR, 6.55; p < 0.001). A significantly lower risk of chronic postoperative use was associated with older age when patients who were 65 to 74 years of age were compared with patients who were <55 years of age (OR, 0.12; p < 0.001) and patients who were 75 to 92 years of age were compared with patients who were <55 years of age (OR, 0.10; p = 0.002). Additionally, patients undergoing total knee arthroplasty had significant association of increased chronic postoperative use compared with patients undergoing rotator cuff repair, carpal tunnel release, or lumbar decompression (Table III).
TABLE III.
Adjusted Logistic Regression for Associations with Postoperative Chronic Opioid Use (>90 Days)
Discussion
In an evaluation of the 5 most common elective orthopaedic procedures performed at our institution, we found that postoperative opioid-prescribing patterns varied widely among procedures and tended to provide patients with an excess of pills approximately 60% of the time. Our findings show that, during FY2015, an excess of approximately 43,000 opioid pills were prescribed following the 5 most common elective orthopaedic procedures at our institution. Patients who had undergone total knee arthroplasty had the highest mean number of postoperative opioid pills at 176.4 (including refills), and patients who had undergone total hip arthroplasty had the largest mean number of remaining pills at 31.9 per patient. The widest range in total pills prescribed was among patients who had undergone total hip arthroplasty, ranging from 30 to 560 postoperatively.
A limitation of our study was the broad scope that we applied to capture prescribing and utilization trends in elective procedures. There are meaningful differences within surgical procedures and the preoperative status of individual patients that we did not assess in this study. Previous studies have demonstrated that patients who undergo upper-extremity, soft-tissue procedures tend to use less opioid pain medication than those who undergo osseous procedures18,32. We did not stratify for incorporation of additional osseous procedures (for example, subacromial decompression) in the patients who had undergone arthroscopic rotator cuff repair. Similarly, we did not evaluate surgical intensity or surgical approach, and we made the broad assumption that cases within the same primary Current Procedural Terminology (CPT) code were generally the same.
Another limitation was our reliance on patient recall in capturing excess medication counts. Although we focused our surveys on patients who had undergone a surgical procedure between March and September 2015, it is still reasonable to expect some recall error from patients attempting to remember the events from as long as 14 months prior. Finally, our patient population tended to be fairly homogenous with regard to patient race and ethnicity, which could have limited the generalizability of our findings.
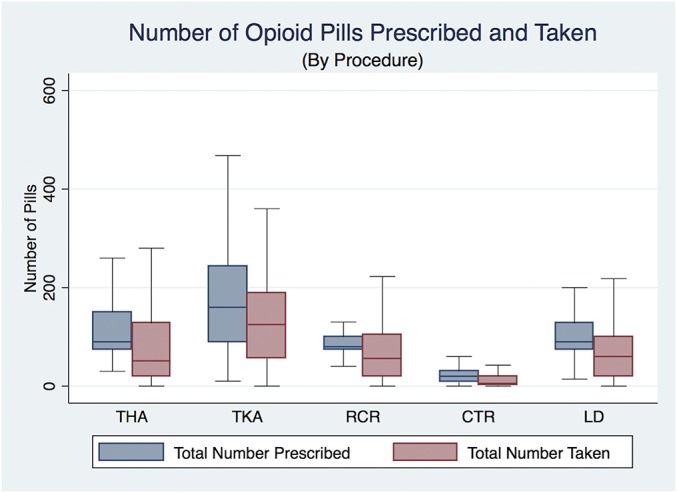
One trend that emerged from our data was a detectable bimodal distribution of postoperative opioid consumption. Approximately half of the patients for each given procedure utilized a fraction of their initial prescription, and the other half of patients used their full initial prescription or received refills for additional medication (Fig. 5). Some of this variation in use may be due to the intensity of the procedure (in the case of a shoulder arthroscopy or a spine surgical procedure)18,33. In the case of patients undergoing total hip arthroplasty or total knee arthroplasty, other explanations as to why certain patients require less (or more) pain medication for similar procedures warrant further investigation.
Fig. 5.
Histograms by procedure showing the distribution of opioid pills taken. The orange, dashed vertical line indicates the median value of the initial postoperative prescription. Note that, for each procedure except total knee arthroplasty (TKA), approximately half of the patients took fewer than the median initial number prescribed. THA = total hip arthroplasty, RCR = arthroscopic rotator cuff repair, CTR = endoscopic carpal tunnel release, and LD = lumbar decompression (with or without arthrodesis).
We did not find a correlation between preoperative opioid use and decreased satisfaction with postoperative pain control. This finding is not generally supported by most current studies that demonstrate preoperative use of opioids portends worse outcomes following a surgical procedure23,34,35. One explanation for the absence of correlation may be our overall high satisfaction rates. With a range of 84% to 95% satisfaction in postoperative pain management among the 5 procedures, we had a small sample size of dissatisfied patients in which to detect an association. This finding may strike at a foundation of the current opioid abuse crisis: the high number of opioids prescribed may promote greater patient satisfaction while simultaneously fueling the problems of excess opioid use and increased risk of opioid diversion.
Our study appears to be unique with regard to the number of cases captured, the number of patients surveyed, and the breadth of procedural categories. To our knowledge, this study is also the first to quantify the volume of excess opioid pills distributed by an orthopaedic surgery department following common elective procedures. Our determination that an excess of 43,000 opioid pills were prescribed in the course of 1 year highlights the magnitude of the contribution of orthopaedic surgery to the ongoing epidemic of opioid abuse and diversion. Additionally, Cicero et al. demonstrated that white patients living in nonurban areas who previously abused prescription opioid medications represent the majority of new heroin users in the United States36. Indeed, the setting of our institution in a rural New England community with a predominantly white patient base serves as a microcosm for the exponential rise in heroin abuse.
The findings in this study may be a useful guide to postoperative opioid protocols by establishing a standard number of opioid pills following elective orthopaedic procedures. By prescribing an amount slightly below the recorded median value in this study (for example, prescribing 70 opioid pills upon discharge for total hip arthroplasty), providers could potentially meet the pain control demands of more than half of their patients while lowering the amount of excess medication prescribed.
Multiple authors have proposed ways to approach stratifying potential pain control issues following an orthopaedic surgical procedure based on characteristics of the surgical procedure and the patient risk factors for chronic opioid use25,32. We believe that better prescribing protocols should be developed following orthopaedic procedures to curb overprescribing and the detrimental impact that it can have on the community.
Footnotes
Investigation performed at the Dartmouth Hitchcock Medical Center, Lebanon, New Hampshire
A commentary by Nicholas A. Bedard, MD, Rafael J. Sierra, MD, and Tad Mabry, MD, is linked to the online version of this article at jbjs.org.
Disclosure: One author (B.J.K.) received partial funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) of the National Institutes of Health; funds were used to pay for partial salary support. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJS/E612).
References
- 1.Centers for Disease Control and Prevention. Understanding the epidemic. 2016. https://www.cdc.gov/drugoverdose/epidemic/. Accessed 2017 Nov 13.
- 2.Portenoy RK. Continuous infusion of opioid drugs in the treatment of cancer pain: guidelines for use. J Pain Symptom Manage. 1986. Fall;1(4):223-8. [DOI] [PubMed] [Google Scholar]
- 3.Portenoy RK, Foley KM. Chronic use of opioid analgesics in non-malignant pain: report of 38 cases. Pain. 1986. May;25(2):171-86. [DOI] [PubMed] [Google Scholar]
- 4.Morris BJ, Mir HR. The opioid epidemic: impact on orthopaedic surgery. J Am Acad Orthop Surg. 2015. May;23(5):267-71. [DOI] [PubMed] [Google Scholar]
- 5.Department of Veterans Affairs. Pain as the 5th vital sign toolkit. 2000. Octoberhttps://www.va.gov/PAINMANAGEMENT/docs/Pain_As_the_5th_Vital_Sign_Toolkit.pdf. Accessed 2017 Nov 9.
- 6.Volkow ND, McLellan TA, Cotto JH, Karithanom M, Weiss SR. Characteristics of opioid prescriptions in 2009. JAMA. 2011. April 6;305(13):1299-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The Joint Commission. Pain standards for 2001. 2001. December 18 https://www.jointcommission.org/assets/1/6/2001_Pain_Standards.pdf. Accessed 2017 Dec 12.
- 8.Centers for Disease Control and Prevention. Opioid overdose. 2016. https://www.cdc.gov/drugoverdose/index.html. Accessed 2017 Nov 13.
- 9.Jones CM, Logan J, Gladden RM, Bohm MK. Vital signs: demographic and substance use trends among heroin users—United States. 2002-2013. MMWR Morb Mortal Wkly Rep. 2015. July 10;64(26):719-25. [PMC free article] [PubMed] [Google Scholar]
- 10.The 190th General Court of the Commonwealth of Massachusetts. Bill H.4056: an act relative to substance use, treatment, education and prevention. 2016. https://malegislature.gov/Bills/189/House/H4056. Accessed 2017 Nov 7. [Google Scholar]
- 11.HHS.gov. HHS takes strong steps to address opioid-drug related overdose, death and dependence. 2015. March 26 https://wayback.archive-it.org/3926/20170128023910/https://www.hhs.gov/about/news/2015/03/26/hhs-takes-strong-steps-to-address-opioid-drug-related-overdose-death-and-dependence.html. Accessed 2017 Nov 7.
- 12.Trescot AM, Helm S, Hansen H, Benyamin R, Glaser SE, Adlaka R, Patel S, Manchikanti L. Opioids in the management of chronic non-cancer pain: an update of American Society of the Interventional Pain Physicians’ (ASIPP) guidelines. Pain Physician. 2008. March;11(2)(Suppl):S5-62. [PubMed] [Google Scholar]
- 13.Larochelle MR, Zhang F, Ross-Degnan D, Wharam JF. Trends in opioid prescribing and co-prescribing of sedative hypnotics for acute and chronic musculoskeletal pain: 2001-2010. Pharmacoepidemiol Drug Saf. 2015. August;24(8):885-92. Epub 2015 Apr 22. [DOI] [PubMed] [Google Scholar]
- 14.Bedson J, Chen Y, Hayward RA, Ashworth J, Walters K, Dunn KM, Jordan KP. Trends in long-term opioid prescribing in primary care patients with musculoskeletal conditions: an observational database study. Pain. 2016. July;157(7):1525-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mathiesen O, Dahl B, Thomsen BA, Kitter B, Sonne N, Dahl JB, Kehlet H. A comprehensive multimodal pain treatment reduces opioid consumption after multilevel spine surgery. Eur Spine J. 2013. September;22(9):2089-96. Epub 2013 May 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roberts M, Brodribb W, Mitchell G. Reducing the pain: a systematic review of postdischarge analgesia following elective orthopedic surgery. Pain Med. 2012. May;13(5):711-27. Epub 2012 Apr 11. [DOI] [PubMed] [Google Scholar]
- 17.O’Neill DF, Webb Thomas C. Less is more: limiting narcotic prescription quantities for common orthopedic procedures. Phys Sportsmed. 2014. November;42(4):100-5. [DOI] [PubMed] [Google Scholar]
- 18.Kim N, Matzon JLMD, Abboudi J, Jones C, Kirkpatrick W, Leinberry CF, Liss FE, Lutsky KF, Wang ML, Maltenfort M, Ilyas AM. A prospective evaluation of opioid utilization after upper-extremity surgical procedures: identifying consumption patterns and determining prescribing guidelines. J Bone Joint Surg Am. 2016. October 19;98(20):e89. [DOI] [PubMed] [Google Scholar]
- 19.Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014. February 11;348:g1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Devin CJ, Lee DS, Armaghani SJ, Bible J, Shau DN, Martin PR, Ehrenfeld JM. Approach to pain management in chronic opioid users undergoing orthopaedic surgery. J Am Acad Orthop Surg. 2014. October;22(10):614-22. [DOI] [PubMed] [Google Scholar]
- 21.Goesling J, Moser SE, Zaidi B, Hassett AL, Hilliard P, Hallstrom B, Clauw DJ, Brummett CM. Trends and predictors of opioid use after total knee and total hip arthroplasty. Pain. 2016. June;157(6):1259-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kidner CLP, Mayer TGMD, Gatchel RJPA. Higher opioid doses predict poorer functional outcome in patients with chronic disabling occupational musculoskeletal disorders. J Bone Joint Surg Am. 2009. April;91(4):919-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morris BJ, Sciascia AD, Jacobs CA, Edwards TB. Preoperative opioid use associated with worse outcomes after anatomic shoulder arthroplasty. J Shoulder Elbow Surg. 2016. April;25(4):619-23. Epub 2015 Dec 2. [DOI] [PubMed] [Google Scholar]
- 24.Nota SP, Spit SA, Voskuyl T, Bot AG, Hageman MG, Ring D. Opioid use, satisfaction, and pain intensity after orthopedic surgery. Psychosomatics. 2015. Sep-Oct;56(5):479-85. Epub 2014 Sep 6. [DOI] [PubMed] [Google Scholar]
- 25.O’Neil JT, Wang ML, Kim N, Maltenfort M, Ilyas AM. Prospective evaluation of opioid consumption after distal radius fracture repair surgery. Am J Orthop (Belle Mead NJ). 2017. Jan-Feb;46(1):E35-40. [PubMed] [Google Scholar]
- 26.Kumar K, Gulotta LV, Dines JS, Allen AA, Cheng J, Fields KG, YaDeau JT, Wu CL. Unused opioid pills after outpatient shoulder surgeries given current perioperative prescribing habits. Am J Sports Med. 2017. March;45(3):636-41. Epub 2017 Feb 9. [DOI] [PubMed] [Google Scholar]
- 27.Helmerhorst GTTMD, Vranceanu AMP, Vrahas M, Smith M, Ring D. Risk factors for continued opioid use one to two months after surgery for musculoskeletal trauma. J Bone Joint Surg Am. 2014. March 19;96(6):495-9. [DOI] [PubMed] [Google Scholar]
- 28.Center for Disease Control and Prevention. Opioid morphine equivalent conversion factors. 2015. March https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Opioid-Morphine-EQ-Conversion-Factors-March-2015.pdf. Accessed 2017 Nov 7.
- 29.UNC Health Care Guideline. Opiate equianalgesic dosing chart. 2009. December https://www.med.unc.edu/aging/fellowship/current/curriculum/palliative-care/UNC%20Equianalgesic%20Card%20-Dec2009.pdf/. Accessed 2017 Nov 17.
- 30.Hill MV, McMahon ML, Stucke RS, Barth RJ., Jr Wide variation and excessive dosage of opioid prescriptions for common general surgical procedures. Ann Surg. 2017. April;265(4):709-14. [DOI] [PubMed] [Google Scholar]
- 31.U.S. Food and Drug Administration. Disposal of unused medicines: what you should know. 2017. October 20 https://www.fda.gov/Drugs/ResourcesForYou/Consumers/BuyingUsingMedicineSafely/EnsuringSafeUseofMedicine/SafeDisposalofMedicines/ucm186187.htm. Accessed 2017 Nov 7. [Google Scholar]
- 32.Kelley BP, Shauver MJ, Chung KC. Management of acute postoperative pain in hand surgery: a systematic review. J Hand Surg Am. 2015. August;40(8):1610-9, 1619.e1. [DOI] [PubMed] [Google Scholar]
- 33.Mirza SK, Deyo RA, Heagerty PJ, Konodi MA, Lee LA, Turner JA, Goodkin R. Development of an index to characterize the “invasiveness” of spine surgery: validation by comparison to blood loss and operative time. Spine (Phila Pa 1976). 2008. November 15;33(24):2651-61; discussion 2662. [DOI] [PubMed] [Google Scholar]
- 34.Zywiel MGMD, Stroh DABS, Lee SYMD, Bonutti PMMD, Mont MAMD. Chronic opioid use prior to total knee arthroplasty. J Bone Joint Surg Am. 2011. November 2;93(21):1988-93. [DOI] [PubMed] [Google Scholar]
- 35.Ben-Ari A, Chansky H, Rozet I. Preoperative opioid use is associated with early revision after total knee arthroplasty: a study of male patients treated in the Veterans Affairs system. J Bone Joint Surg Am. 2017. January 4;99(1):1-9. [DOI] [PubMed] [Google Scholar]
- 36.Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry. 2014. July 1;71(7):821-6. [DOI] [PubMed] [Google Scholar]