Supplemental Digital Content is available in the text.
Abstract
The Ventrain is a small, manually operated, single-use, inspiratory flow-adjustable ventilation device that generates positive pressure during inspiration and, through a Bernoulli effect within the device, active suction during expiration. It was designed to provide emergency ventilation during airway obstruction via narrow-bore cannulae. The device has been used successfully in elective procedures lasting >1 hour. It remains to be seen if its theoretical advantages in “can’t intubate, can’t oxygenate” (CICO) scenarios translate to reliable clinical benefit and allow inclusion in future airway algorithms. We advocate for regular simulation training and the detailed reporting of clinical experience with this encouraging new tool.
Pulmonary ventilation via narrow-bore catheters or cannulae is challenging due to the high resistance to gas flow. Traditionally, jet ventilation is required to inject gas under pressure, but the lack of sufficient bidirectional flow demands a patent upper airway to ensure effective passive expiration and to avoid barotrauma and hemodynamic collapse. The Ventrain (Ventinova Medical B.V., Eindhoven, the Netherlands) combines high-pressure source lung ventilation with active aspiration of gas during expiration. The device, which provides manual flow-controlled ventilation, originated in the Netherlands from industrial injectors used on automated assembly lines and underwent testing in bench studies as well as in animals. Although initially intended for ventilation via needle cricothyrotomy in the emergency “can’t intubate, can’t oxygenate” (CICO) situation, to date, the Ventrain has been used mainly in the operating room during elective airway surgery. It is currently approved for emergency use within the European Union, the United States, Australia, and New Zealand. In this article, we describe the structure and function of this interesting tool and briefly speculate on whether it might have a future role in difficult airway algorithms.
DESCRIPTION
The Ventrain is a small, manually operated, single-use, inspiratory flow-adjustable ventilation device driven from a high-pressure oxygen source. It generates positive pressure during inspiration and, through a Bernoulli effect within the device, active suction during expiration. It was designed to provide ventilation through a narrow-bore catheter in emergencies where conventional ventilation via mask, supraglottic airway, or tracheal tube fails.1 There are 2 connections: an inlet tube (length, 213 ± 20 cm; internal diameter, 3.0–4.5 mm) and a short sidearm (length, 20 ± 1 cm; internal diameter, 5.20 ± 0.15 mm) that connects via a male Luer Lock to the airway catheter/cannula. The dimensions of the internal channels are not available. A Luer Lock connection on the sidearm allows intermittent measurement of end-tidal CO2 concentration and can provide a continuous nonquantitative capnograph. Oxygen should be supplied from a pressure-compensated flowmeter or pressure-regulated cylinder to maintain stable flows and avoid problematic backpressure seen with anesthesia machines.2 Internally, the inlet channel narrows to a diameter of 0.7 mm before directly splitting into a T shape (Figure 1). Gas is diverted either along the inspiratory/expiratory sidearm to the airway or along the exhaust channel to an opening on the upper surface. Acceleration of oxygen flow across the inlet constriction generates subatmospheric pressure over the sidearm, resulting in active suctioning during expiration. A bypass channel runs internally from the proximal inspiratory/expiratory limb, just below the T junction, to open on the lower surface. The internal dead space volume is 5 mL.
Figure 1.
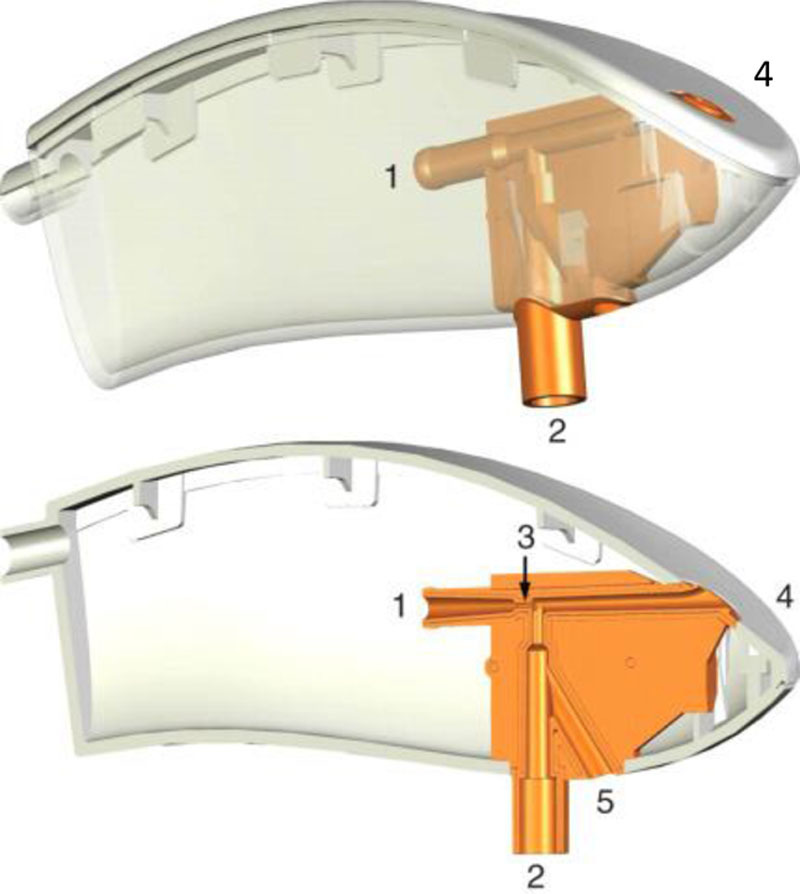
Internal structure of the Ventrain device. 1, Conical oxygen inlet channel. 2, Inspiratory/expiratory channel connecting to the sidearm. 3, Constriction (0.7 mm) producing downstream subatmospheric pressure. 4, Exhaust channel opening. 5. Bypass channel acting as on/off switch used to equilibrate lung volume. Reproduced with permission from Hamaekers et al.1
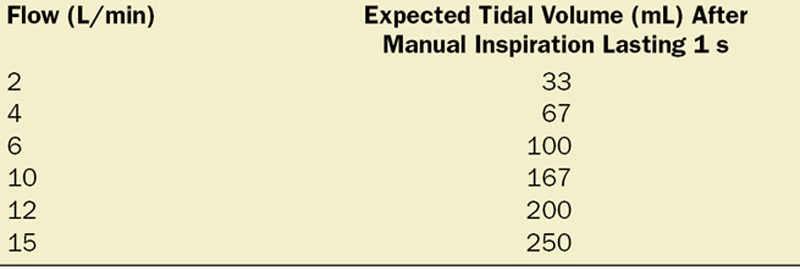
Figure 2 describes the 3 operational phases: inspiration, expiration, and equilibration (see also Supplemental Digital Content, Video, http://links.lww.com/AACR/A283, which demonstrates use of the Ventrain in the skills laboratory). During inspiration, the upper and lower openings are occluded by the thumb and index fingers, respectively. In laboratory studies conducted on a model of airway occlusion, a driving pressure of 2.3 bar was observed at flows of 15 L/min.1 Insufflation pressure proximal to the airway catheter was measured at 138 cm H2O. However, in pigs with a closed airway, peak airway pressure was limited at 30–35 cm H2O.4 Tidal volume depends on oxygen flow rate, inspiratory time, and the impedance to airflow of the airway catheter and respiratory system. When pulmonary compliance and airway resistance (components of impedance) are normal, insufflation lasting 1 second produces tidal volumes of approximately 250 mL (flow, 15 L/min). The manufacturer provides a guide to flow and tidal volume as illustrated in the Table. Respiratory frequency is determined by the duration of the manual inspiratory/expiratory cycle.
Figure 2.
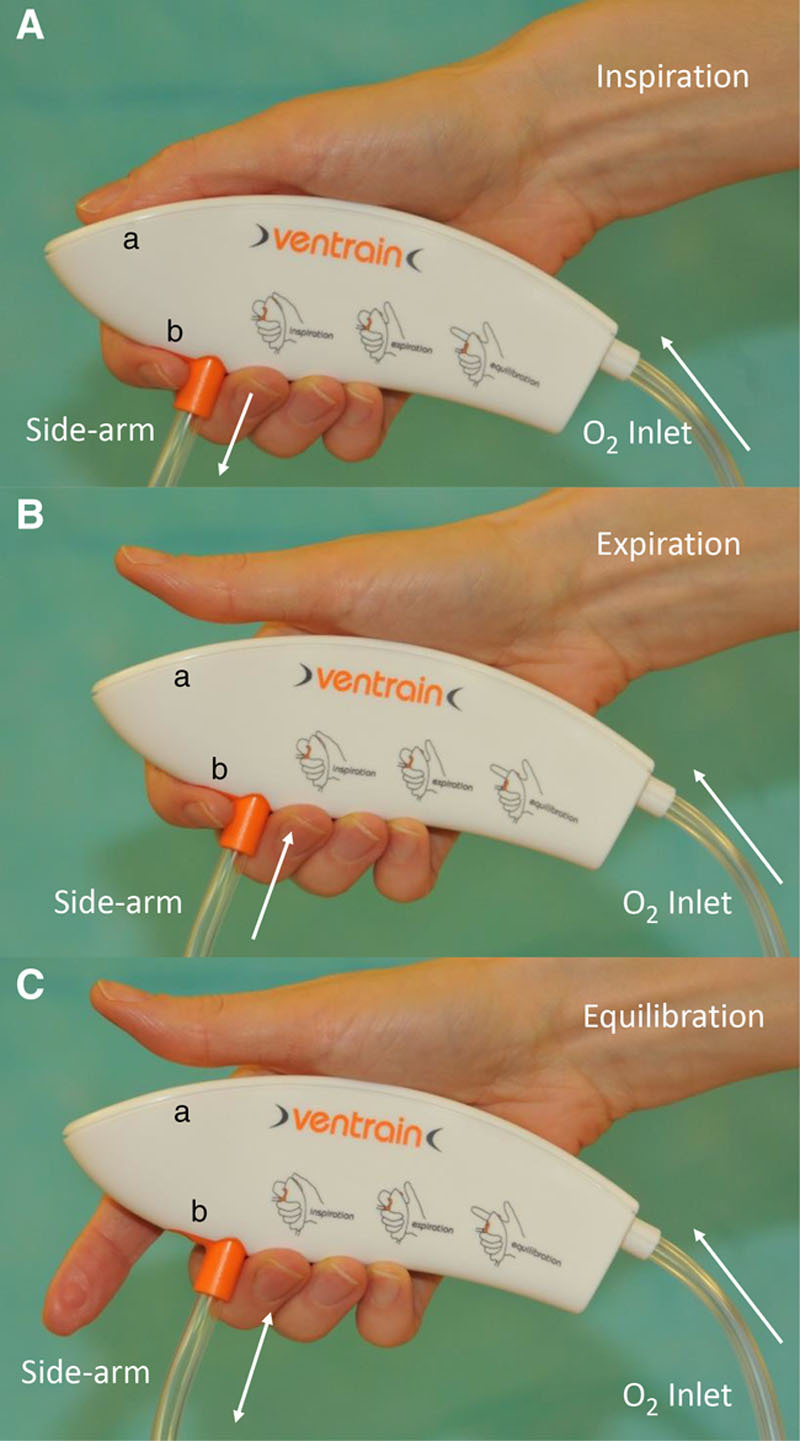
Operation of the Ventrain device. A, Inspiration. The exhaust aperture (a) and bypass aperture (b) are occluded with the thumb and index fingers, respectively. Oxygen flow accelerates under high proximal driving pressure across a narrow constriction and is diverted along the inspiratory channel, via the sidearm to the airway. B, Expiration. The exhaust aperture (a) is opened by lifting the thumb while maintaining the bypass aperture (b) closed. Subatmospheric pressure downstream from the inlet constriction results in active aspiration of gas from the lungs, which is entrained with the fresh oxygen flow via the exhaust. C, Equilibration. Opening both apertures allows fresh oxygen to escape via the exhaust. Gas flow via the bypass channel, to or from the lungs, allows lung volume to equilibrate to near functional residual capacity. This equilibration phase should last 5 s after every 5–10 respiratory cycles. Reproduced with permission from Morrison et al.3
Table.
Approximate Tidal Volumes (mL) Expected After Manual Inspiration Lasting 1 s, With a Given Flow
During expiration, the upper exhaust aperture is opened by lifting the thumb, while maintaining the lower aperture closed. Gas from the lungs is entrained with fresh oxygen via the exhaust port. Minimum pressures of −97 cm H2O have been measured in the sidearm when the airway is totally occluded. An inspiratory/expiratory ratio of 1/1 results in similar inspiratory and expiratory tidal volumes. Clinical monitoring of chest wall excursions during ventilation is essential.
During equilibration, both apertures are open allowing lung volume to stabilize near functional residual capacity, while fresh oxygen escapes via the exhaust. This avoids inadvertent hyperinflation or excessive suctioning on the lungs and should be performed every 5–10 breaths. The manufacturers recommend the Ventrain be used as a temporizing measure for a maximum of 20 minutes.
DISCUSSION
Clinical experience with the Ventrain is accumulating. The device has already been used in patients with airway obstruction for periods ≥60 minutes by experienced anesthesiologists in an elective setting. Both transtracheal cannulae5,6 (sometimes preemptively placed for airway rescue) and exchange catheters3 have been used for ventilation. Use in pediatric anesthesia has also been described.7,8 Although originally intended for narrow-bore transtracheal ventilation in a CICO situation, experience in this area is limited.9 Many hospitals now include this device in their difficult airway cart, even if it has not yet been incorporated into official guidelines on difficult airway management. The rarity of a CICO event (1:12,500 general anesthetics10) and ethical constraints mitigate against randomized controlled trials for this indication. To further our knowledge, therefore, it is essential that anesthesiologists report their experiences by publishing their cases or entering details in registries such as the Airway App.11
In pigs, the Ventrain outperforms traditional transtracheal jet ventilation (TTJV) during partial and complete airway obstruction.4 The most successful reports with the Ventrain have been in the operating room during elective use for obstructive airway pathology, but as Noppens12 pointed out, premature use of the device by inexperienced anesthesiologists in unselected patients may have a negative impact on its future applications.
Even if this promising technology can be endorsed for elective use, a future role in CICO scenarios is more contentious. In this setting, needle cricothyrotomy remains an option for restoring oxygenation in many airway algorithms (eg, American Society of Anesthesiologists, Difficult Airway Society, Canadian Airway Focus Group). The 2015 Difficult Airway Society guidelines for managing unanticipated difficult intubation in adults favor surgical cricothyrotomy as the final step in an airway crisis; however, the use of needle cricothyrotomy by experienced, trained personnel is acknowledged. The arguments for preferring surgical emergency front of neck access (FONA) with a scalpel/bougie/tube technique are compelling: it is a relatively straightforward, standardized procedure; it uses simple, easily accessible equipment; and it allows conventional ventilation with capnometry via a cuffed tracheal tube. Moreover, a number of national anesthesia databases (Denmark, the United Kingdom, the United States, and Canada) confirm better success rates with a surgical approach. In the 4th National Audit Project, needle cricothyrotomy failed in approximately 60% of cases, and scalpel techniques were almost universally successful, although the procedures were performed by surgeons. For many anesthesiologists, however, the psychological barrier of making an incision and performing a cricothyrotomy, especially in an obese neck, remains a considerable hurdle and may delay timely rescue. Interestingly, in a survey of attitudes to emergency FONA, only ≈10% of responding Canadian anesthesiologists opted for open surgical or scalpel/bougie cricothyrotomy as their first choice approach.13 Furthermore, Timmermann et al14 have questioned abandoning narrow-bore cricothyrotomy, emphasizing the role of human factors in determining the preferred approach for emergency FONA. Instead, this group advocated continued training in both techniques.
Much of the morbidity associated with narrow-bore cricothyrotomy relates to TTJV. This is fraught with problems, even in experienced hands, and can easily lead to barotrauma. In a meta-analysis of elective as well as emergency CICO and emergency non-CICO cases, Duggan et al15 concluded that complications occurred 6–7 times more frequently with emergency CICO (51% of the 90 cases reported). Barotrauma was 4–5 times more likely with emergency CICO. The Ventrain’s unique technology, however, associated with lower peak inspiratory pressures and the possibility of capnography monitoring, may make ventilation with the device inherently safer than with TTJV. Nevertheless, a major concern with both techniques is the need for a correctly placed airway cannula. Kinking, malpositioning, and dislodgement are all known complications. Furthermore, during a crisis, cognitive and motor skills become impaired, and this may have a detrimental effect on the manual operation of the Ventrain. Anesthesiologists should therefore undergo regular skills training in transtracheal cannulation and operation of the device if the full benefits of this potentially life-saving technology are to be realized.
Needle cricothyrotomy is the recommended FONA technique in 1- to 8-year-old children (Difficult Airway Society guidelines). Although CICO is a rare event in this age group, critical upper airway obstruction may arise from respiratory infection or anaphylaxis. In these situations, needle cricothyrotomy with an appropriately sized cannula and adjusted Ventrain flow rate may be indicated.
In summary, the Ventrain has many theoretical advantages over TTJV. The device has a role to play in elective airway management, but it remains unclear whether clinical benefits will arise in the CICO scenario and allow inclusion in airway algorithms. We advocate regular simulation training with this technique. Furthermore, to better define its future place in anesthetic practice, anesthesiologists are encouraged to report details of their clinical experiences.
DISCLOSURES
Name: Stuart Morrison, MBChB, FFARCSI.
Contribution: This author helped prepare and revise the manuscript, and prepare the supplemental digital content (video).
Name: Sophie Aerts, MD.
Contribution: This author helped prepare, edit, and revise the manuscript.
Name: Vera Saldien, MD.
Contribution: This author helped prepare, edit, and revise the manuscript, and prepare the supplemental digital content (video).
This manuscript was handled by: BobbieJean Sweitzer, MD, FACP.
GLOSSARY
- CICO =
- can’t intubate, can’t oxygenate
- FONA =
- front of neck access
- TTJV =
- transtracheal jet ventilation
Funding: None.
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal’s website.
REFERENCES
- 1.Hamaekers AE, Borg PA, Enk D. Ventrain: an ejector ventilator for emergency use. Br J Anaesth. 2012;108:1017–1021. [DOI] [PubMed] [Google Scholar]
- 2.Schmidt AR, Ruetzler K, Haas T, Schmitz A, Weiss M. Impact of oxygen sources on performance of the Ventrain(®) ventilation device in an in vitro set-up. Acta Anaesthesiol Scand. 2016;60:241–249. [DOI] [PubMed] [Google Scholar]
- 3.Morrison S, Aerts S, Van Rompaey D, Vanderveken O. Failed awake intubation for critical airway obstruction rescued with the Ventrain device and an Arndt exchange catheter: a case report. A A Pract. 2019;13:23–26. [DOI] [PubMed] [Google Scholar]
- 4.Paxian M, Preussler NP, Reinz T, Schlueter A, Gottschall R. Transtracheal ventilation with a novel ejector-based device (Ventrain) in open, partly obstructed, or totally closed upper airways in pigs. Br J Anaesth. 2015;115:308–316. [DOI] [PubMed] [Google Scholar]
- 5.Fearnley RA, Badiger S, Oakley RJ, Ahmad I. Elective use of the Ventrain for upper airway obstruction during high-frequency jet ventilation. J Clin Anesth. 2016;33:233–235. [DOI] [PubMed] [Google Scholar]
- 6.Onwochei DN, El-Boghdadly K, Ahmad I. Two-stage technique used to manage severe upper airway obstruction and avoid surgical tracheostomy: a case report. A A Pract. 2018;10:118–120. [DOI] [PubMed] [Google Scholar]
- 7.Escribá Alepuz FJ, Alonso García J, Cuchillo Sastriques JV, Alcalá E, Argente Navarro P. Emergency ventilation of infant subglottic stenosis through small-gauge lumen using the Ventrain: a case report. A A Pract. 2018;10:136–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Willemsen MG, Noppens R, Mulder AL, Enk D. Ventilation with the Ventrain through a small lumen catheter in the failed paediatric airway: two case reports. Br J Anaesth. 2014;112:946–947. [DOI] [PubMed] [Google Scholar]
- 9.Heuveling DA, Mahieu HF, Jongsma-van Netten HG, Gerling V. Transtracheal use of the Cricath cannula in combination with the Ventrain device for prevention of hypoxic arrest due to severe upper airway obstruction: a case report. A A Pract. 2018;11:344–347. [DOI] [PubMed] [Google Scholar]
- 10.Kheterpal S, Martin L, Shanks AM, Tremper KK. Prediction and outcomes of impossible mask ventilation: a review of 50,000 anesthetics. Anesthesiology. 2009;110:891–897. [DOI] [PubMed] [Google Scholar]
- 11.Duggan LV, Lockhart SL, Cook TM, O’Sullivan EP, Dare T, Baker PA. The airway app: exploring the role of smartphone technology to capture emergency front-of-neck airway experiences internationally. Anaesthesia. 2018;73:703–710. [DOI] [PubMed] [Google Scholar]
- 12.Noppens RR. Ventilation through a ‘straw’: the final answer in a totally closed upper airway? Br J Anaesth. 2015;115:168–170. [DOI] [PubMed] [Google Scholar]
- 13.Wong DT, Mehta A, Tam AD, Yau B, Wong J. A survey of Canadian anesthesiologists’ preferences in difficult intubation and “cannot intubate, cannot ventilate” situations. Can J Anaesth. 2014;61:717–726. [DOI] [PubMed] [Google Scholar]
- 14.Timmermann A, Chrimes N, Hagberg CA. Need to consider human factors when determining first-line technique for emergency front-of-neck access. Br J Anaesth. 2016;117:5–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duggan LV, Ballantyne Scott B, Law JA, Morris IR, Murphy MF, Griesdale DE. Transtracheal jet ventilation in the ‘can’t intubate can’t oxygenate’ emergency: a systematic review. Br J Anaesth. 2016;117suppl 1i28–i38. [DOI] [PubMed] [Google Scholar]


