Background:
Women are underrepresented as applicants to and trainees of orthopaedic surgery residencies. Factors that attract women to or deter them from orthopaedic surgery have been previously published; however, there has been no analysis of the programs that train high percentages of female residents and the factors that differentiate them from programs that have low percentages of women. The purpose of this study was to identify and compare these factors between programs with high and low percentages of female residents.
Methods:
Information on each orthopaedic surgery residency program listed in the American Medical Association (AMA) Fellowship and Residency Electronic Interactive Database (FREIDA) was collected utilizing residency program web sites, an online survey distributed to residency program coordinators, and a follow-up telephone survey. These included data on resident and faculty demographic characteristics and residency program curriculum structure. The prevalence of factors in programs with the highest percentages of female residents was compared with those with lower percentages.
Results:
Data were obtained from 143 (97.3%) of 147 programs, with 3,406 residents identified. Only 485 residents (14.2%) were female. Programs with more female residents had more female faculty members per program (p = 0.001), a higher percentage of faculty who were female (p < 0.001), more female associate professors (p < 0.001), more women in leadership positions (p < 0.001), and a higher prevalence of women’s sports medicine programs (p = 0.03); were more commonly listed in the Top 40 for National Institutes of Health (NIH) funding (p = 0.03) and U.S. News & World Report rankings (p = 0.02); and were more likely to offer a research year (p = 0.045).
Conclusions:
There are greater percentages of female residents at orthopaedic residency programs with more female faculty members, more women in leadership positions, a women’s sports medicine program, and the option to do a research year. Departmental and national leaders may consider these factors when efforts are undertaken to enhance the recruitment of female applicants and improve female interest in orthopaedic surgery as a specialty.
There is a well-documented disparity of women applying for and training in orthopaedic residencies. This disparity ensues even though women comprise approximately 50% of medical school matriculates1. Previous studies have discussed factors that motivate women to pursue a career in orthopaedic surgery or deter them from doing so2-4. However, the data regarding the distribution of women among orthopaedic residency programs in the United States are limited5,6.
Residency programs select applicants on the basis of performance during orthopaedic rotations, class rank, United States Medical Licensing Examination (USMLE) Step 1 and 2 scores, interview performance, and letters of recommendation7, and applicants generally rank residency programs on the basis of a variety of factors including academic reputation, lifestyle, and geography8-10. It has been shown that female applicants weigh their personal interactions on interview days and a program’s proximity to family and friends more heavily when determining their rank list, while eliminating programs based on their perceived sex biases more readily than their male counterparts9. Although these issues have been explored, the factors that draw women to certain orthopaedic residency programs have yet to be fully understood8,9.
Van Heest et al. demonstrated that only a small proportion of orthopaedic residencies train most of the female residents and that a majority of orthopaedic residency programs have percentages of female trainees well below the national average of 14%5,6. The purpose of this study was to determine what factors are present in the programs that have the highest percentage of female residents and to compare the prevalence of these factors in the programs with lower percentages of women. The identification of these factors may allow for targeted recruitment efforts for women and the expansion of a diverse resident pool.
Materials and Methods
This study met exemption criteria as determined by our hospital’s institutional review board. The American Medical Association (AMA) Fellowship and Residency Electronic Interactive Database (FREIDA) was used to identify all allopathic orthopaedic surgery residency programs during the 2016 to 2017 academic year. To ensure comprehensive data collection, information on each program was collected using a 3-tiered approach: searching residency program web sites, reviewing online surveys distributed to residency program coordinators at all identified programs, and following up with telephone surveys of program coordinators who had not returned the online survey after a total of 3 reminders. All data compiled from program web sites were cross-referenced with data obtained from the e-mail or telephone surveys, and, if conflicts were noted, it was assumed that the information from program coordinators would be more current and accurate and, thus, that information was used in the analysis.
Data collected from the residency program web sites consisted of resident and faculty demographic characteristics and program curriculum structure. Resident and faculty demographic data included the total number of residents and faculty members as well as the female complement of each, the number of full female professors, the number of female associate professors, the number of women in leadership positions (section chief, residency program director, fellowship program director), and the presence of a female chairperson. Program curriculum data included the existence of a mandatory or optional research year, establishment of a women’s sports medicine program, description of a formal maternity leave policy and whether the leave was paid, and the affiliation of the residency with a university. A women’s sports medicine program is a formal facility or organization that is dedicated to the multidisciplinary treatment of active women and is typically associated with a department of orthopaedic surgery. The online and telephone surveys distributed to residency program coordinators included 17 questions about the program recapitulating and confirming the information found online. Finally, publicly available information was used to determine if programs were affiliated with one of the top-40 National Institutes of Health (NIH)-funded medical school-based orthopaedic residency programs11 or were affiliated with a top-40 orthopaedic hospital in the 2016 to 2017 U.S. News & World Report rankings12. The information obtained highlights 9 factors (Table I) that have been referenced as possibly impacting female medical student interest in orthopaedic surgery3,5,13-17. The number of factors present in each program was totaled.
TABLE I.
Analysis of Program-Specific Factors
| Top Quartile | Other Quartiles | P Value | |
| No. of programs | 35 | 108 | — |
| Total no. of residents | 939 | 2,467 | — |
| Total no. of female residents | 228 | 257 | — |
| No. of residents per program* | 26.8 ± 9.4 | 22.8 ± 9.8 | 0.036† |
| Range of female residents in programs | 20.0% to 42.1% | 0% to 19.4% | — |
| Total no. of faculty | 1,140 | 3,121 | — |
| Total no. of female faculty‡ | 145 | 251 | — |
| Female faculty | 12.7% | 8.0% | <0.001† |
| Female faculty per program* | 4.1 ± 2.8 | 2.3 ± 2.8 | 0.001† |
| Female full professors per program* | 0.36 ± 0.73 | 0.24 ± 0.63 | 0.40 |
| Female associate professors per program* | 2.9 ± 2.5 | 1.5 ± 1.6 | <0.001† |
| Women in leadership positions per program*‡ | 0.94 ± 1.1 | 0.33 ± 0.64 | <0.001† |
| No. of female chairpersons‡ | 0 | 0 | 1.00 |
| Programs with women’s sports medicine program‡ | 21.4% | 6.5% | 0.03† |
| Female part-time surgeons per program* | 0.14 ± 0.47 | 0.21 ± 0.51 | 0.55 |
| Programs with a research year‡ | 31.4% | 14.8% | 0.045† |
| Programs in top-40 NIH funding‡ | 42.9% | 23.1% | 0.03† |
| Programs in top-40 U.S. News & World Report rankings‡ | 37.1% | 15.7% | 0.02† |
| Programs with a defined maternity leave policy‡ | 78.6% | 91.7% | 0.18 |
| Programs noting paid maternity leave time | 91.7% | 78.3% | 0.43 |
| University-affiliated programs‡ | 93.3% | 89.4% | 1.00 |
| Program-specific factors per program* | 3.5 ± 1.8 | 2.5 ± 1.6 | <0.001† |
The values are given as the mean number and the standard deviation.
Significant.
This category was identified as 1 of the 9 program-specific factors.
Programs were then stratified on the basis of their percentage of female residents. The total number of women within a program, including those in a research year, were included and programs were plotted on a box plot (Fig. 1). Quartiles of programs based on the percentage of female residents were determined, and to highlight programs that have the highest percentages of female residents, the programs in the top (fourth) quartile were selected. Data were then compared between the top quartile and the other (combined first through third) quartiles.
Fig. 1.
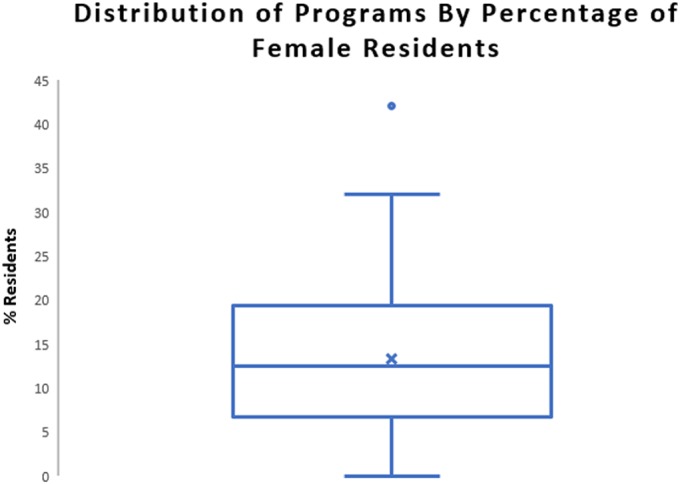
Box plot showing the 25th and 75th quartiles (top and bottom of the box), mean (x), median (central line), and outliers (•) of the distribution of orthopaedic residency programs based on their percentage of female residents. The whiskers indicate the minimum value of the first quartile and the maximum value of the fourth quartile, excluding any outliers.
Continuous data were analyzed with independent t tests, and categorical data were analyzed with 2 × 2 contingency tables and Fisher exact tests. For all statistical tests, significance was set at p < 0.05.
Results
Data were obtained from 97.3% (143 of 147) allopathic, non-military, orthopaedic surgery residency programs within the United States. The 4 excluded programs had no usable information on their web sites and coordinators did not return multiple phone calls or respond to the e-mail survey.
A total of 485 female residents (14.2%) were identified in a pool of 3,406 orthopaedic residents. The percentage of female residents in each program was calculated and the results are summarized in Figure 1. Fourteen programs (9.8%) had no female residents. The top quartile of programs had a ≥20% complement of female residents and no program had >42.1% female residents. Almost all programs were affiliated with a teaching university, and there was no difference (p = 1.00) between the top quartile (93.3%) and the other quartiles (89.4%) in their proportion of university-affiliated programs.
The academic faculty affiliated with all residency programs totaled 4,261, with 1,140 (32.6 per program) in the top quartile and 3,121 (28.9 per program) in the other quartiles. There was no difference in the mean size of the faculty per program (p = 0.35). The mean complement of female faculty in programs within the top quartile was 12.7%, a proportion that was 59% higher than the 8.0% of women on staff in the other quartiles (p < 0.001). Each program in the top quartile had almost double the mean number of female faculty members (mean and standard deviation, 4.1 ± 2.8) compared with the other quartiles (2.3 ± 2.8) (p = 0.001). Although the difference in the mean number of female professors per program was no different between the top quartile and the other quartiles, the mean number of female associate professors in each program in the top quartile (2.9 ± 2.5) was almost twice that in the other quartiles (1.5 ± 1.6) (p < 0.001). In the top quartile, there was only 1 program (5.7%) that did not have a female attending physician, and 22 programs in the other quartiles (20.4%) had no female attending physician (p = 0.02).
Programs in the top quartile had nearly triple the mean number of women in leadership positions (0.94 ± 1.1) than those in the other quartiles (0.33 ± 0.64) (p < 0.001). Of the 143 programs analyzed, there was no female chairperson.
Women’s sports medicine programs were found more commonly in the top quartile programs (21.4% compared with 6.5%; p = 0.03). Top quartile programs were more commonly ranked in the top-40 programs for NIH funding (42.9% compared with 23.1%; p = 0.03) and on U.S. News & World Report rankings (37.1% compared with 15.7%; p = 0.02). Furthermore, programs in the top quartile were more than twice as likely to offer or have a separate track for a year of research as part of the residency training (31.4% compared with 14.8%; p = 0.045).
There were no significant differences in the proportions of programs defining their policy on maternity leave either on their web site or internally (78.6% compared with 91.7%; p = 0.18) or offering paid leave time (91.7% compared with 78.3%; p = 0.43).
Overall, programs in the top quartile had a mean of 1 more of the 9 factors that have been identified as possibly impacting female medical student interest in orthopaedic surgery (3.5 ± 1.8 compared with 2.5 ± 1.6; p < 0.001).
Discussion
An increasing focus has been placed on the lack of diversity within orthopaedic surgery residencies and the specialty itself. The makeup of residents in orthopaedics has consistently been unbalanced, with women currently comprising only 14% of all orthopaedic residents, the lowest of any surgical specialty5,18. Although several studies have postulated why the specialty itself is not attractive to many female medical students, citing reasons such as work hours and physical demands15, others have negated this rationale given that specialties with high percentages of women (e.g., obstetrics and gynecology19) or those with increasing percentages of women (e.g., other surgical subspecialties and general surgery5) similarly require long work hours and uncontrolled lifestyles20. Others claim that there is an inherent lack of early exposure of women to science, technology, engineering, and mathematics (STEM) fields and have partnered with programs such as the Perry Initiative to expose women to these fields as early as in middle school3,17. Several studies have described the important role of early exposure in attracting applicants to orthopaedics13,21 and this is especially true for women22,23, but little has been published about the specific factors of orthopaedic residency programs that may influence female enrollment. Some have even directly called for the identification of program-specific factors that attract women6. Our investigation was designed with the thought that an increase in female recruitment into orthopaedics can be facilitated by having a better understanding of the factors present in residency programs with higher percentages of women.
Why does sex diversity in the orthopaedic workforce matter? First, 51% of the patient population in the United States is women24. Also, women often have higher rates of orthopaedic surgical interventions than men, even with elective procedures being offered to and utilized by women at markedly lower rates25. These data suggest that women will make up a substantial component of surgeons’ practices. In addition, patients often prefer to be treated by physicians of the same sex26-28, and we are ultimately doing a disservice to our patients by having an uneven distribution of male and female orthopaedic surgeons4. Increasing the number of women in orthopaedic training will help to prepare a culturally competent workforce29, as male trainees can learn to interact more effectively with female patients by training in a system with a variety of viewpoints and backgrounds. Aside from sex-focused patient care, poor recruitment efforts may result in the best and brightest medical students choosing not to apply to orthopaedics, which may slow the progress of orthopaedic surgery15,30.
The presence of female leadership and effective female mentors has been previously noted as impactful on the sex composition of orthopaedic residency programs. Hill et al. described how female orthopaedic residents had been positively influenced to become interested in orthopaedics because of mentors of the same sex or ethnicity more so than their male counterparts2. Despite the importance of having female mentors, O’Connor described their limited availability3, and Day et al. calculated that the field of orthopaedics has the lowest percentage of female faculty (13%) of any medical specialty and that only 3.8% of full professors are women31. Jagsi et al. attempted to determine a relationship between the presence of female chairpersons or female faculty in specific programs and the application of women to these programs, but they were unable to draw meaningful conclusions because of the limited number of female chairpersons and faculty32. Their data also suggested that female applicants were not necessarily matching into programs that already had higher numbers of women. In 2010, Nguyen et al. also attempted to find an association between the sex composition of faculty and residents, but with their limited survey, they were also unable to do so33. To our knowledge, the present study is the first to determine that there are greater proportions and numbers of female faculty, more female associate professors, and higher numbers of women in leadership positions at orthopaedic residency programs with greater proportions of female residents.
Many women perceive there to be sex biases in orthopaedics among faculty and male residents4. To dispel these perceptions, some advocate for the greater allocation of resources to residency programs to encourage female medical students to apply34. One such method is by expanding the number of residents to allow for accommodations such as maternity leave34. We were unable to find a difference in the presence of maternity leave policies between programs with high percentages of female residents and other residency programs. However, there is profound variability in the presence of and the types of policies within orthopaedic residencies for maternity leave35, so a true relationship between the number of female residents and the presence of a maternity leave policy may be difficult to interpret.
Having residency programs demonstrate that they are dedicating resources to the orthopaedic care of female patients may be critical in adjusting the perception of the specialty. Female medical students readily eliminate programs from their rank lists based on perceived sex biases9, so programmatic efforts such as the development of a women’s sports medicine program can go a long way to demonstrating advocacy for women and eliminating bias. Only 10% of residencies have affiliations with such programs, but a greater percentage of programs with high percentages of women have these established relationships. It is unknown how much the presence of a women’s sports medicine program is promoted during interviews and on program web sites, but we utilized their presence as a surrogate for residency programs that have publicly dedicated efforts to the orthopaedic care of women. Perhaps increased public exposure of these unique programs can attract female applicants already interested in orthopaedics and change the perception of orthopaedic residencies by promoting that orthopaedic surgeons are dedicated to the egalitarian treatment of all patients.
This study had several limitations. There are likely many more applicant and program-related factors than are detailed in this report that have associations with the prevalence of female residents in specific orthopaedic surgery training programs. For example, the experiences of female applicants on interview days have been shown to influence their willingness to rank a program. Women are less likely to rank programs when they are asked biased interview questions on issues such as their marital status and family planning36. In addition, quality of life and lifestyle issues have been cited as possible reasons deterring many women from pursuing a career in orthopaedics2, although one would imagine that there may be differences in the quality of life of residents at different programs. Furthermore, the geographic preferences of an applicant or the proximity to a spouse may play a role in attracting women to specific programs. Our study was not able to account for these possibilities. We also understand the potential for detection bias in the acquisition of the data from various sources. Finally, our study was cross-sectional in that we only included residents currently in training. Meaningful fluctuations in percentages of female residents may be possible at programs from year to year as resident class sizes are small and therefore small changes are magnified. However, the percentage of female orthopaedic residents has not drastically changed in recent years5 and the majority of the programs that have previously been defined as having more female residents6 are the same as those highlighted in more recent studies5 and our study.
Despite these limitations, our study design is validated by the thorough inclusion of all residents at almost every orthopaedic residency program in the United States. Other recent investigations into this topic showed similar percentages of female orthopaedic residents to our current study (14.8% compared with 14.2%)18. Coincidentally, the threshold for programs having percentages of female residents “above the national average” in the studies by Van Heest et al.5,6 was identical to the lower limit of our top quartile (20%), and despite our threshold representing the mean female complement of the 5 years of residency classes currently in training, about 75% of the residency programs were the same in our top quartile as in those studies.
The identification of factors present in orthopaedic residency programs with high percentages of women may allow for other residencies to model themselves after such programs to increase the diversity of their training program. However, some factors may be more easily correctable than others. For instance, it likely requires fewer resources and less time to hire a female faculty member than to increase research funding from the NIH. Efforts by a program to improve the diversity of their trainees must stem from the department chair. Chairpersons who outwardly recognize the sex disparity and heighten the “level of consciousness of the faculty” can effect an increase in the number of women who are selected for interviews and subsequently match into their program37.
In summary, the purpose of this study was to determine what factors are present in orthopaedic residency programs that have the highest percentage of female residents and to compare these factors with the programs with lower percentages of female residents. The programs with the most female residents (i.e., top quartile) were found to have greater numbers and percentages of female faculty and women in leadership positions, suggesting greater availability of same-sex mentors for female applicants. In addition, programs in the top quartile had greater percentages of residencies with women’s sports medicine programs, perhaps demonstrating an increased focus on female patients and a reduced bias toward women within the training program itself. Finally, a greater proportion of programs in the top quartile had dedicated research years, top-40 NIH funding, and top-40 U.S. News & World Report rankings, which may indicate greater focuses on academic productivity. These findings highlight specific factors on which residency programs can improve to enhance their recruitment of female applicants, and these data can potentially be extrapolated to a national level to improve interest in orthopaedics as a specialty.
Footnotes
Investigation performed at the Department of Orthopaedic Surgery, The Warren Alpert School of Medicine at Brown University, Providence, Rhode Island; the Department of Orthopaedic Surgery, Drexel University College of Medicine, Philadelphia, Pennsylvania; and the Department of Orthopaedic Surgery, Tulane University School of Medicine, New Orleans, Louisiana
Disclosure: There was no source of external funding for this study. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJS/E759).
References
- 1.Association of American Medical Colleges. Table A-1: U.S. medical school applications and matriculants by school, state of legal residence, and sex,2016-2017., 2016-2017 2016. https://www.aamc.org/download/321442/data/factstablea1.pdf. Accessed 2018 Feb 6. [Google Scholar]
- 2.Hill JF, Yule A, Zurakowski D, Day CS. Residents’ perceptions of sex diversity in orthopaedic surgery. J Bone Joint Surg Am. 2013. October 2;95(19):e1441-6. [DOI] [PubMed] [Google Scholar]
- 3.O’Connor MI. Medical school experiences shape women students’ interest in orthopaedic surgery. Clin Orthop Relat Res. 2016. September;474(9):1967-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lewis VO, Scherl SA, O’Connor MI. Women in orthopaedics—way behind the number curve. J Bone Joint Surg Am. 2012. March 7;94(5):e30. [DOI] [PubMed] [Google Scholar]
- 5.Van Heest AE, Fishman F, Agel J. A. 5-year update on the uneven distribution of women in orthopaedic surgery residency training programs in the United States. J Bone Joint Surg Am. 2016. August 3;98(15):e64. [DOI] [PubMed] [Google Scholar]
- 6.Van Heest AE, Agel J. The uneven distribution of women in orthopaedic surgery resident training programs in the United States. J Bone Joint Surg Am. 2012. January 18;94(2):e9. [DOI] [PubMed] [Google Scholar]
- 7.Egol KA, Collins J, Zuckerman JD. Success in orthopaedic training: resident selection and predictors of quality performance. J Am Acad Orthop Surg. 2011. February;19(2):72-80. [DOI] [PubMed] [Google Scholar]
- 8.Sanfilippo JA, Sharkey PF, Parvizi J. Criteria used by medical students to rank orthopedic surgery residency programs. Am J Orthop (Belle Mead NJ). 2006. November;35(11):512-4. [PubMed] [Google Scholar]
- 9.Huntington WP, Haines N, Patt JC. What factors influence applicants’ rankings of orthopaedic surgery residency programs in the National Resident Matching Program? Clin Orthop Relat Res. 2014. September;472(9):2859-66. Epub 2014 Jun 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Resident Matching Program. Results of the 2015 NRMP applicant survey. 2015. September http://www.nrmp.org/wp-content/uploads/2015/09/Applicant-Survey-Report-2015.pdf. Accessed 2018 Feb 6.
- 11.Blue Ridge Institute for Medical Research. Ranking tables of NIH funding to US medical schools. 2014. November 12 http://www.brimr.org/NIH_Awards/2014/NIH_Awards_2014.htm. Accessed 2018 Feb 6.
- 12.U.S. News & World Report. Best hospitals for orthopedics. 2016. http://health.usnews.com/best-hospitals/rankings/orthopedics. Accessed 2018 Feb 6.
- 13.London DA, Calfee RP, Boyer MI. Impact of a musculoskeletal clerkship on orthopedic surgery applicant diversity. Am J Orthop (Belle Mead NJ). 2016. Sep-Oct;45(6):E347-51. [PubMed] [Google Scholar]
- 14.Templeton K, Wood VJ, Haynes R. Women and minorities in orthopaedic residency programs. J Am Acad Orthop Surg. 2007;15(Suppl 1):S37-41. [DOI] [PubMed] [Google Scholar]
- 15.Blakemore LC, Hall JM, Biermann JS. Women in surgical residency training programs. J Bone Joint Surg Am. 2003. December;85(12):2477-80. [DOI] [PubMed] [Google Scholar]
- 16.Rohde RS, Wolf JM, Adams JE. Where are the women in orthopaedic surgery? Clin Orthop Relat Res. 2016. September;474(9):1950-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lattanza LL, Meszaros-Dearolf L, O’Connor MI, Ladd A, Bucha A, Trauth-Nare A, Buckley JM. The Perry Initiative’s medical student outreach program recruits women into orthopaedic residency. Clin Orthop Relat Res. 2016. September;474(9):1962-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brotherton SE, Etzel SI. Graduate medical education, 2015-2016. JAMA. 2016. December 6;316(21):2291-310. [DOI] [PubMed] [Google Scholar]
- 19.Baldwin K, Namdari S, Bowers A, Keenan MA, Levin LS, Ahn J. Factors affecting interest in orthopedics among female medical students: a prospective analysis. Orthopedics. 2011. December 6;34(12):e919-32. [DOI] [PubMed] [Google Scholar]
- 20.Dorsey ER, Jarjoura D, Rutecki GW. The influence of controllable lifestyle and sex on the specialty choices of graduating U.S. medical students, 1996-2003. Acad Med. 2005. September;80(9):791-6. [DOI] [PubMed] [Google Scholar]
- 21.Rao RD, Khatib ON, Agarwal A. Factors motivating medical students in selecting a career specialty: relevance for a robust orthopaedic pipeline. J Am Acad Orthop Surg. 2017. July;25(7):527-35. [DOI] [PubMed] [Google Scholar]
- 22.Bernstein J, Dicaprio MR, Mehta S. The relationship between required medical school instruction in musculoskeletal medicine and application rates to orthopaedic surgery residency programs. J Bone Joint Surg Am. 2004. October;86(10):2335-8. [DOI] [PubMed] [Google Scholar]
- 23.Mason BS, Ross W, Ortega G, Chambers MC, Parks ML. Can a strategic pipeline initiative increase the number of women and underrepresented minorities in orthopaedic surgery? Clin Orthop Relat Res. 2016. September;474(9):1979-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.United States Census Bureau. QuickFacts: United States. 2017. https://www.census.gov/quickfacts/fact/table/US/PST045216. Accessed 2018 Feb 6.
- 25.Borkhoff CM, Hawker GA, Wright JG. Patient gender affects the referral and recommendation for total joint arthroplasty. Clin Orthop Relat Res. 2011. July;469(7):1829-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oberlin DT, Vo AX, Bachrach L, Flury SC. The gender divide: the impact of surgeon gender on surgical practice patterns in urology. J Urol. 2016. November;196(5):1522-6. Epub 2016 May 10. [DOI] [PubMed] [Google Scholar]
- 27.Schmittdiel J, Grumbach K, Selby JV, Quesenberry CP., Jr Effect of physician and patient gender concordance on patient satisfaction and preventive care practices. J Gen Intern Med. 2000. November;15(11):761-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Derose KP, Hays RD, McCaffrey DF, Baker DW. Does physician gender affect satisfaction of men and women visiting the emergency department? J Gen Intern Med. 2001. April;16(4):218-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cohen JJ, Gabriel BA, Terrell C. The case for diversity in the health care workforce. Health Aff (Millwood). 2002. Sep-Oct;21(5):90-102. [DOI] [PubMed] [Google Scholar]
- 30.Gebhardt MC. Improving diversity in orthopaedic residency programs. J Am Acad Orthop Surg. 2007;15(Suppl 1):S49-50. [DOI] [PubMed] [Google Scholar]
- 31.Day CS, Lage DE, Ahn CS. Diversity based on race, ethnicity, and sex between academic orthopaedic surgery and other specialties: a comparative study. J Bone Joint Surg Am. 2010. October 6;92(13):2328-35. [DOI] [PubMed] [Google Scholar]
- 32.Jagsi R, Griffith KA, DeCastro RA, Ubel P. Sex, role models, and specialty choices among graduates of US medical schools in 2006-2008. J Am Coll Surg. 2014. March;218(3):345-52. Epub 2013 Nov 20. [DOI] [PubMed] [Google Scholar]
- 33.Nguyen L, Amin NH, Vail TP, Pietrobon R, Shah A. Editorial: a paucity of women among residents, faculty, and chairpersons in orthopaedic surgery. Clin Orthop Relat Res. 2010. July;468(7):1746-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hariri S, York SC, O’Connor MI, Parsley BS, McCarthy JC. Career plans of current orthopaedic residents with a focus on sex-based and generational differences. J Bone Joint Surg Am. 2011. March 2;93(5):e16. [DOI] [PubMed] [Google Scholar]
- 35.Weiss J, Teuscher D. What provisions do orthopaedic programs make for maternity, paternity, and adoption leave? Clin Orthop Relat Res. 2016. September;474(9):1945-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hern HG, Jr, Alter HJ, Wills CP, Snoey ER, Simon BC. How prevalent are potentially illegal questions during residency interviews? Acad Med. 2013. August;88(8):1116-21. [DOI] [PubMed] [Google Scholar]
- 37.Thomas CL. African Americans and women in orthopaedic residency. The Johns Hopkins experience. Clin Orthop Relat Res. 1999. May;362:65-71. [PubMed] [Google Scholar]


