Abstract
BACKGROUND
In women with obesity, excess gestational weight gain (≥270 g/week) occurs in 2 out of 3 pregnancies and contributes to metabolic impairments in both mother and baby. To improve obstetrical care, objectively assessed information on energy balance is urgently needed. The objective of this study was to characterize determinants of gestational weight gain in women with obesity.
METHODS
This was a prospective, observational study of pregnant women with obesity. The primary outcome was energy intake calculated by the energy intake-balance method. Energy expenditure was measured by doubly labeled water and whole-room indirect calorimetry and body composition as a 3-compartment model by air displacement plethysmography and isotope dilution in early (13–16 weeks) and late (35–37 weeks) pregnancy.
RESULTS
In pregnant women with obesity (n = 54), recommended weight gain (n = 8, 15%) during the second and third trimesters was achieved when energy intake was 125 ± 52 kcal/d less than energy expenditure. In contrast, women with excess weight gain (67%) consumed 186 ± 29 kcal/d more than they expended (P < 0.001). Energy balance affected maternal adiposity (recommended: –2.5 ± 0.8 kg fat mass; excess: +2.2 ± 0.5; inadequate: –4.5 ± 0.5; P < 0.001) but not fetal growth. Weight gain was not related to demographics, activity, metabolic biomarkers, or diet quality. We estimated that energy intake requirements for recommended weight gain during the second and third trimesters were not increased as compared with energy requirements early in pregnancy (34 ± 53 kcal/d, P = 0.83).
CONCLUSION
We here provide what we believe are the first evidence-based recommendations for energy intake in pregnant women with obesity. Contrary to current recommendations, energy intake should not exceed energy expenditure.
TRIAL REGISTRATION
ClinicalTrials.gov, NCT01954342.
FUNDING
This study was funded by the National Institutes of Health (R01DK099175) and the Clinical Research Cores at Pennington Biomedical Research Center (U54GM104940 and P30DK072476).
Keywords: Metabolism, Reproductive Biology
Keywords: Clinical practice, Obesity, Obstetrics/gynecology
Introduction
According to the 2009 Institute of Medicine guidelines, women entering pregnancy with obesity should limit total weight gain to 5–9 kg (1). Despite these recommendations, excess gestational weight gain occurs in 2 out of every 3 pregnancies among women with obesity (2, 3), increasing the risks of obesity and type 2 diabetes mellitus in both the mother and baby (4, 5). Thus, for women with obesity, effective weight gain management in pregnancy is an unmet need in clinical practice.
Lifestyle modification therapy is considered the first line strategy for controlling gestational weight gain. To date, more than 6300 patients who are overweight or obese have participated in effectiveness trials evaluating lifestyle interventions, including LIMIT (6), DALI (7, 8), UPBEAT (9), RADIEL (10), and LIFE-Moms (11). Only half of these studies report a significant reduction in the incidence of excess gestational weight gain (7, 11). Overall, reductions in total weight gain were modest and averaged 0.5 kg (6–11). Very few studies demonstrated downstream improvements in maternal and infant outcomes at birth (6, 8, 11). The low efficacy of lifestyle intervention trials is generally attributed to poor patient adherence, yet we and others (6, 8–11) hypothesize that most interventions are of insufficient intensity. Consequently, they produce only small perturbations in energy balance (intake minus expenditure) and therefore small changes in weight gain.
The Institute of Medicine recommends that all pregnant women increase energy intake by 340–450 kcal/d during the second and third trimesters (1). Such recommendations for dietary energy intake (1, 12, 13) were based on studies in pregnant women without obesity (14–16). In recognition of the different needs for the patient with obesity, the American College of Obstetricians and Gynecologists states that pregnant women with obesity may need fewer extra calories, but does not provide specific guidance (12). Studies of gestational weight gain in women with obesity attempt to inform clinical guidance for energy intake, diet quality, and physical activity but employ subjective self-reported assessments, which are prone to recall bias (17, 18). Energy intake recommendations for pregnant women with obesity are therefore either extrapolated from women without obesity or based on subjective measures, but not based on appropriate evidence.
To improve clinical guidance for obstetrical care, we obtained objective assessments to characterize the physiological and behavioral determinants of gestational weight gain in women with obesity.
Results
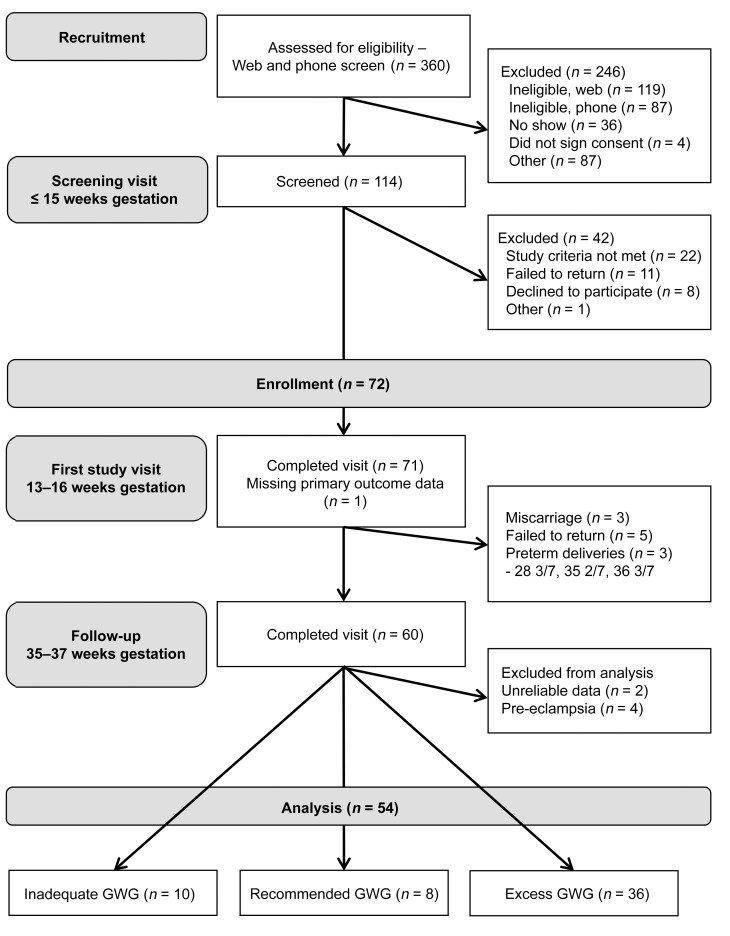
Of the 72 women enrolled, 60 completed the late pregnancy assessment and 54 had complete data to analyze the primary outcome, energy intake (Figure 1). Women who did not have complete data were more likely to be African American, were heavier (111.2 kg vs. 96.1 kg, 41.0 kg/m2 vs. 35.8 kg/m2), and had higher HbA1c values (5.6% vs. 5.4%) as compared with those included in this study. Throughout the second and third trimesters, the mean rate of weight gain of the study population was 369 ± 29 grams per week (range –50 to +796 g/week), resulting in 7.8 ± 0.6 kg total weight gain.
Figure 1. Participant throughput.
Seventy-two women were enrolled, 60 completed the late pregnancy assessment, and 54 satisfied the criteria for inclusion in the statistical analysis.
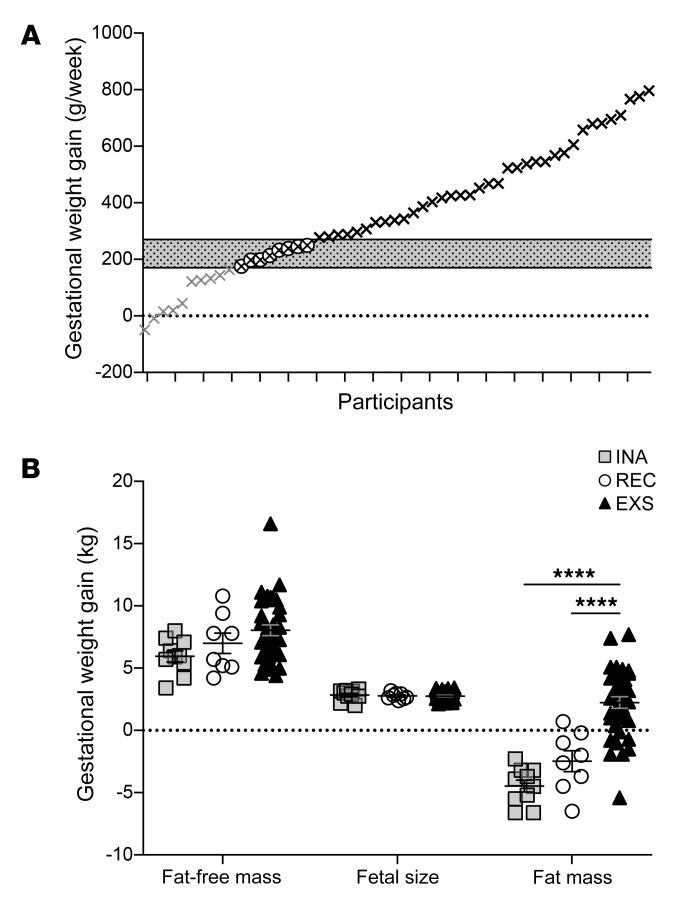
Applying the 2009 Institute of Medicine guidelines for gestational weight gain in women with obesity, 8 women (15%) gained weight as recommended (REC), 36 women (67%) gained excess weight (EXS), and 10 (19%) had inadequate (INA) weight gain (Figure 2A). The groups did not differ by demographic characteristics (Table 1), but the INA group had more severe obesity (P = 0.002, Table 1) and was more insulin resistant compared with the EXS group (P = 0.008, Supplemental Table 1; supplemental material available online with this article; https://doi.org/10.1172/JCI130341DS1). In a sensitivity analysis, we excluded the 2 most obese patients (BMI: 57.1, 46.0, both INA group). The differences in obesity and insulin resistance early in pregnancy disappeared, whereas primary outcomes were unchanged. Pregnancy outcomes, delivery outcomes, and infant size at birth were not different among the weight gain groups (Table 1).
Figure 2. Rate and composition of weight gain.
(A) Gestational weight gain is shown as grams per week for each individual participant. According to 2009 Institute of Medicine guidelines, weight gain was classified as inadequate (in gray, INA, <170 g/week, n = 10), recommended (in white, REC, ≥170 g/week and <270 g/week, n = 8), and excessive (in black, EXS, ≥270 g/week, n = 36). The highlighted box shows the weight gain recommendations. (B) Data shown represent change from early (14.9 ± 0.1 weeks) to late pregnancy (35.9 ± 0.1 weeks) and are presented for each individual and as mean ± SEM for fat-free mass, fetal size, and fat mass, as observed in kilograms. Differences among weight gain groups were tested using linear mixed effect models with group used as a covariate. ****P < 0.001 of the post-hoc comparison between groups of the linear mixed model.
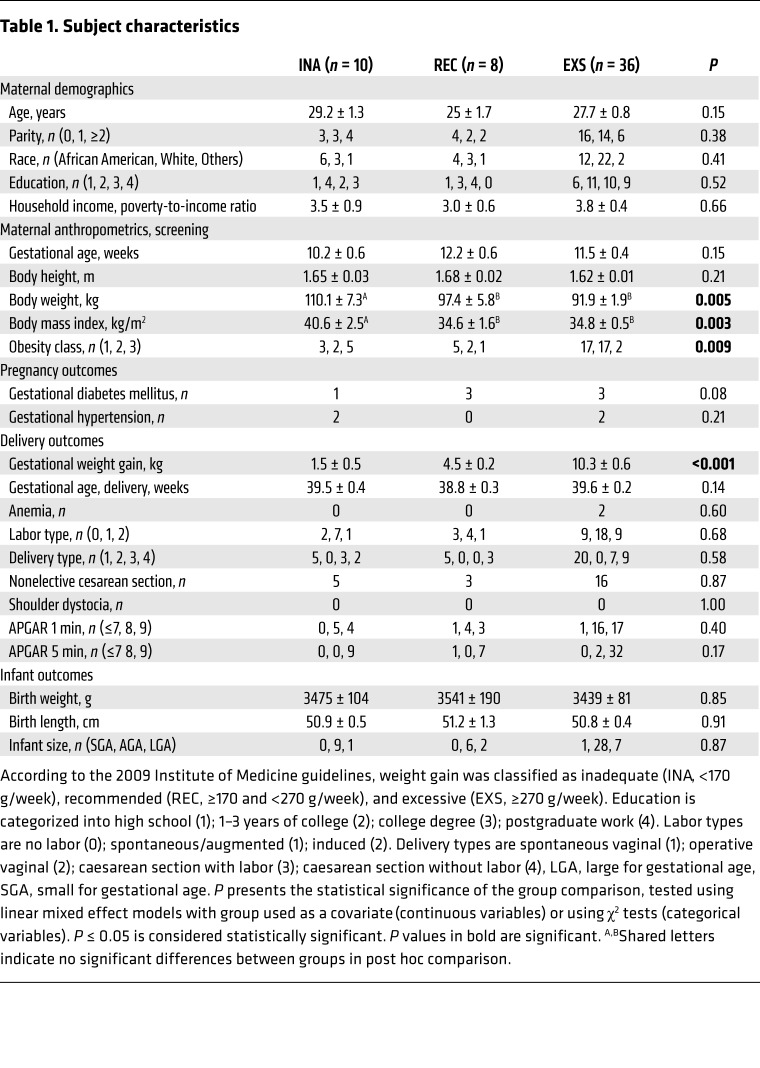
Table 1. Subject characteristics.
Recommended weight gain.
At a rate of weight gain of 218 ± 90 g/week, women with recommended weight gain increased body mass by 4.5 ± 0.2 kg during the observation period. While these women accumulated 7.0 ± 0.8 kg of fat-free mass (Figure 2B) that included fetal growth (2.7 ± 0.1 kg), the total weight gain was also the result of losing fat mass (–2.5 ± 0.8 kg).
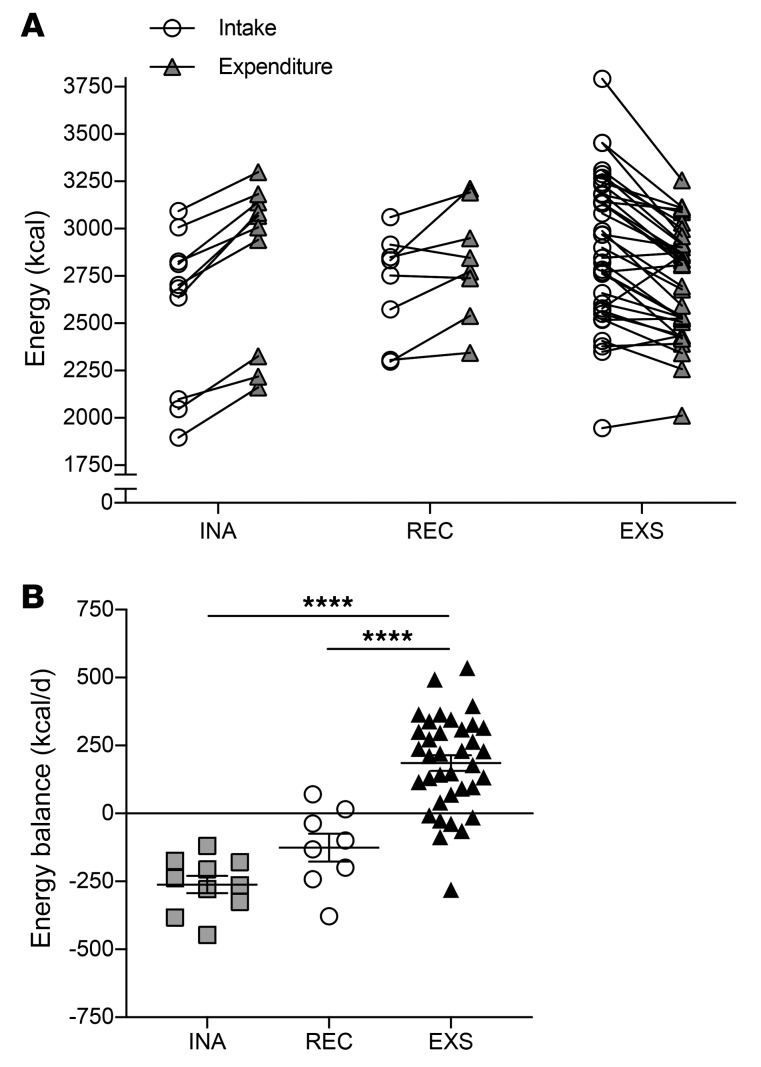
In Table 2, results of the primary outcomes — energy intake, energy expenditure and energy deposition — are summarized. Energy intake throughout the second and third trimesters was calculated as the sum of energy expenditure across pregnancy (calculated as mean of total daily energy expenditure early and late in pregnancy), and energy deposition, i.e. changes in fat mass and fat-free mass. Therefore, energy intake is the mean energy intake per day between 14.9 ± 0.1 weeks and 35.9 ± 0.1 weeks of pregnancy. In the REC group, daily energy intake was 2698 ± 99 kcal/d and energy expenditure was 2824 ± 105 kcal/d (Table 2 and Figure 3A). Therefore, women with recommended weight gain maintained a negative energy balance, i.e. intake minus expenditure, of –125 ± 52 kcal/d during pregnancy (Figure 3B).
Table 2. Energy intake, energy expenditure and energy deposition in pregnant women with obesity.
Figure 3. Energy intake, energy expenditure and energy balance.
(A) Energy intake (energy intake-balance method) and energy expenditure (doubly labeled water method) are presented for each individual and as mean ± SEM for 3 groups of women classified according to gestational weight gain as inadequate (in gray, INA, <170 g/week, n = 10), recommended (in white, REC, ≥170 g/week and <270 g/week, n = 8), and excessive (in black, EXS, ≥270 g/week, n = 36) by the 2009 Institute of Medicine guidelines. (B) Individual and mean ± SEM energy balance are presented as the difference in intake and expenditure for the 3 categories of gestational weight gain. Differences among weight gain groups were tested using linear mixed effect models with group used as a covariate. ****P < 0.001 of the post-hoc comparison between groups of the linear mixed model.
Excess weight gain.
The EXS group gained 10.3 ± 0.6 kg body weight during the observation period (P < 0.0001). Compared with the REC group, the difference in total weight gain was not due to the accumulation of fat-free mass, including fetal growth, but to gains in fat mass (2.2 ± 0.5 kg, P < 0.001, Figure 2B). For the EXS group, the energy intake and energy expenditure throughout the second and third trimesters were not significantly different from the REC group (P = 0.16 and P = 0.48, respectively, Table 2 and Figure 2A). However, energy balance was positive (186 ± 29 kcal/d) and significantly different from the REC group (P < 0.001, Figure 2B).
Inadequate weight gain.
In the INA group, women gained only 1.5 ± 0.5 kg (P = 0.03). While fat-free mass accumulation and fetal growth were comparable with the REC and EXS groups, the INA group lost fat mass (–4.5 ± 0.5 kg, P = 0.10, Figure 2B). Energy intake throughout the second and third trimesters was not different from energy intake in the REC group (P = 0.51). Energy balance was negative, but the difference to the REC group was not significant (–262 ± 32 kcal/d, P = 0.08, Figure 2B).
Physiologic and behavioral determinants of gestational weight gain.
The difference in energy balance among the groups was not accounted for by differences in physical activity (Supplemental Table 2). We observed a smaller increase in sleeping energy expenditure in women with excess and inadequate weight gain as compared with women with recommended weight gain (both P < 0.01, Supplemental Table 1). Physiological and behavioral factors including insulin, thyroid hormones, sympathetic nervous system activity and gut hormones, diet quality, and eating behavior constructs, including mindful eating and food cravings, were not different among the weight gain groups (Supplemental Tables 1–4).
Energy intake for recommended gestational weight gain.
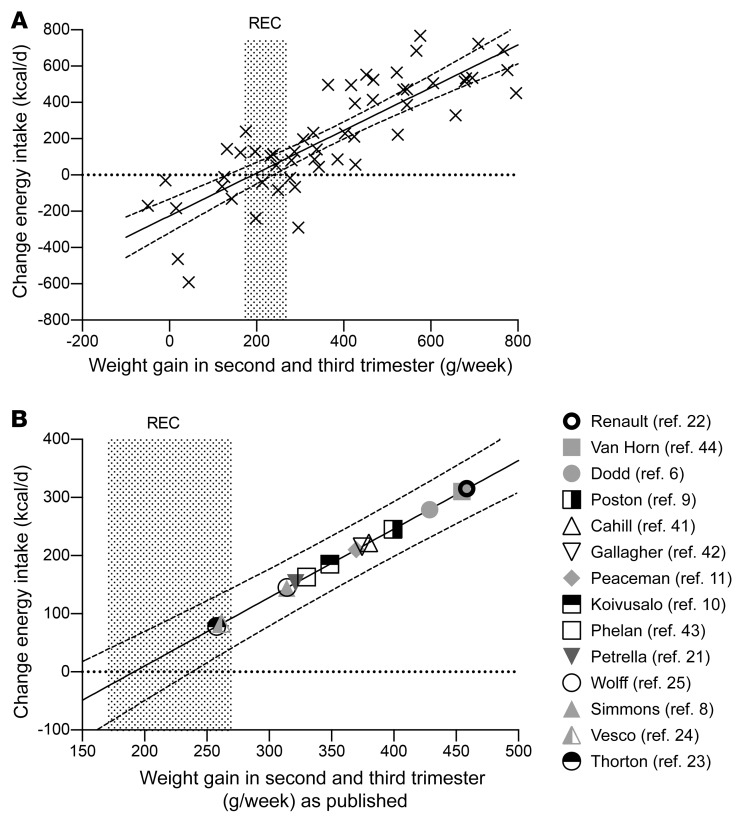
Using our data, we developed a linear regression equation to estimate the change in energy intake from early pregnancy to the second and third trimesters of pregnancy required to achieve recommended gestational weight gain. This approach assumed that energy intake requirements early in pregnancy were equivalent to total daily energy expenditure (1, 13, 14) and energy intake requirements during the second and third trimesters equal energy intake in women with recommended weight gain. Thus, the change in energy intake was calculated as difference between measured energy intake during pregnancy and total daily energy expenditure early in pregnancy. Using an observed gestational weight gain (GWG) as an independent variable, the change in energy intake (Change EI) can be estimated as: Change EI [kcal/d] = 1.178 ± 0.108*GWG [g/week] –225 ± 46; R2 = 0.70.
The Change EI is relative to energy intake and energy expenditure in early pregnancy and GWG is rate of gestational weight gain during second and third trimesters (Figure 4A). To achieve the recommended rate of weight gain suggested by the Institute of Medicine for women with obesity (170–270 g/week), the change in energy intake during the second and third trimesters would need to be between –25 ± 46 kcal/d to +93 ± 46 kcal/d. In Figure 4B, we estimated changes in energy intake for published weight gain data in lifestyle intervention studies. Our model of estimated energy intake showed that patients in the intervention groups consumed 196 ± 20 kcal/d more than early pregnancy energy requirements (range +78 to +310 kcal/d). Control groups in these respective studies consumed higher energy intakes (334 ± 32 kcal/d) during the same time period (data not shown).
Figure 4. Change in energy intake estimates for gestational weight gain.
Association between gestational weight gain and change in energy intake (Change EI), calculated as calculated energy intake during pregnancy minus measured baseline total daily energy expenditure for each individual in the present study (A, n = 54), and for intervention groups in lifestyle intervention studies for pregnant women with obesity (B, by first author). The association is defined by measured data in this study and defined as Change EI [kcal/d] = 1.178 ± 0.108*GWG [g/week] –225 ± 46; R2 = 0.70, in which Change EI is change in energy intake relative to early pregnancy total daily energy expenditure and GWG is gestational weight gain during the second and third trimesters. The regression line is presented with 95% confidence intervals. REC, recommended gestational weight gain (170–270 g/week).
Discussion
We believe that this is the first study to provide evidence-based recommendations for energy intake in pregnant women with obesity that are in contrast to current recommendations by the Institute of Medicine. To deliver such recommendations, we describe phenotypic, behavioral, and metabolic characteristics and determinants of gestational weight gain exclusively in women with obesity using a comprehensive battery of objective measures pertinent to body composition and energy balance phenotyping. The proportion of women with recommended, excess, and inadequate weight gain in our study is consistent with epidemiological data in that two-thirds of women had excess gestational weight gain (2). Our study has 4 major findings that inform management of pregnant women with obesity. First, the recommended rate of weight gain was achieved by the gain of fat-free mass alone (e.g., fetus, uterus, blood volume, breast tissue). Second, dietary intake must not exceed energy expenditure during pregnancy, and weight gain as recommended by the Institute of Medicine is achieved if energy intake is maintained but not increased from early pregnancy throughout the second and third trimesters. The increased energy demand of pregnancy and by the infant is compensated for by the mobilization of maternal fat mass. Third, energy imbalance determines weight gain, without influence of diet, physical activity or metabolic biomarkers. Fourth, weight maintenance during obese pregnancy, as suggested by recent epidemiological studies, requires approximately 10% energy deficit.
First, the Institute of Medicine weight gain recommendations were achieved by the accumulation of fat-free mass alone. The gain in fat-free mass, which includes tissue growth (e.g., fetus, placenta, breast, and uterus) and fluid expansion (e.g., blood volume, intracellular, and extracellular fluid) (19), was similar among the weight gain groups. Energy balance was not associated with nonfat tissue accumulation, and therefore we hypothesize that interventions designed to modify energy balance would not affect weight gain in these compartments. To infer causality from this association requires evidence from a prospective intervention study. In contrast, fat mass gain was variable and thus is more likely modifiable by interventions. Achieving the recommended rate of weight gain required that fat mass be reduced.
Second, the recommended rate of weight gain in obese pregnancies was accomplished when the daily energy intake throughout the second and third trimesters did not exceed energy expenditure. Our data suggest that pregnant women with obesity should not consume additional energy when pregnant. The energy requirement for fetal development was compensated by mobilization of maternal fat mass with no adverse effects in maternal or fetal outcomes observed. This observation challenges current advice by the Institute of Medicine and American College of Obstetrician and Gynecologists for women with obesity, which is to consume an additional 200–300 kcal/d during the second and third trimesters for optimal weight gain (1, 12). Consuming surplus energy throughout the second and third trimesters, even in these small amounts (~200 kcal/d) produced excess gestational weight gain. Dietary needs should be estimated on a per patient basis using an energy requirement model specific for women with obesity early in pregnancy, or clinicians should simply advise patients to not increase dietary energy intake (20).
Third, no differences in physical activity, metabolic biomarkers, dietary intake, and eating behavior constructs were observed among the Institute of Medicine weight gain groups. Our study was not powered to detect differences in these factors and could be prone to type 1 error. Nevertheless, this suggests that the impact of a lifestyle modification intervention in pregnancy depends on its ability to modify energy balance. By our calculations, such trials aimed to achieve a reduction in energy intake of 7%–37% in the second and third trimesters (21–25). Importantly, the achieved differences in energy intake between the intervention and control groups, as estimated by the regression equation, were only small. Estimates of energy intake based on observed weight gain from published lifestyle intervention studies showed that interventions reduced energy intake by –140 kcal/d (~5%) in comparison with the control groups. Recommended weight gain was only achieved by 2 studies and, of note, our model estimates that women in these interventions increased energy intake during pregnancy by less than 100 kcal/d (23, 24).
Past trials prescribing energy intake targets achieved the largest effect sizes (mean difference between intervention and control group) for modifying weight gain for women with obesity (21–25). Of the studies that examined modifying energy intake, most (21–24) but not all (25) showed that dietary modification reduced one or more adverse pregnancy outcomes. However, the studies were powered to detect intervention effects on weight gain; hence, the sample sizes were often too small to demonstrate intervention efficacy for improvements in other pregnancy outcomes. Conversely, those trials powered for pregnancy outcomes did not target energy intake or energy balance per se, and thereby achieved only modest reductions in energy intake and weight gain, and failed to modify adverse pregnancy and infant outcomes (6, 8–11). Appropriately powered studies designed to improve weight gain and pregnancy outcomes through evidence-based energy intake targets remain to be undertaken for women with obesity.
Finally, our study suggests that lifestyle interventions designed to achieve weight maintenance throughout pregnancy (<2.5 kg) require a 9% energy deficit. This finding is relevant to translate new recommendations from epidemiological studies that suggest that weight maintenance may be required to improve outcomes for pregnant women with obesity (26, 27). Advocating weight maintenance for pregnant women with obesity is however too premature until long-term effects on offspring development have been determined.
This study excels for its rigorous, objective methods. However, the approaches used in the study are limited to small, extensively phenotyped cohorts. Thus, our study is unique in its ability to explain how the current recommendations for weight gain can be achieved, and to demonstrate that excess gestational weight gain in women with obesity is due to differences in energy balance, which was not associated with differences or changes in metabolic determinants. The sample size is, however, too small to exclude the possibility of false-negative findings related to pregnancy, delivery, and fetal outcomes, or effect-modification by covariates, including demographic, behavioral, or metabolic factors. The next step is to evaluate the implementation of these new energy intake targets in appropriately powered studies and to understand the effects of maternal energy restriction on outcomes for women with obesity and their babies. Strategies to induce an energy gap may include attenuating the observed declines in physical activity and diet quality (28).
Using objective measures of energy balance, this study challenges current practice and argues that women with obesity should not be advised to consume additional energy during pregnancy as currently recommended. Preserving physical activity and improving diet quality may offer additional strategies to achieve current gestational weight gain recommendations, but only if an energy deficit of ~100 kcal/d is achieved. More stringent recommendations for weight gain during obese pregnancy (<2.5 kg) would require deficits of approximately 10%.
Methods
Design and subjects
MomEE (ClinicalTrials.gov, NCT01954342) was a prospective, observational cohort study conducted between February 2015 and January 2017 at Pennington Biomedical Research Center in Baton Rouge, Louisiana. Women were followed prospectively across pregnancy with outcome assessments measured in specialized clinic visits between 13–16 weeks and 35–37 weeks to encompass the second and third trimesters of gestation. Gestational weight gain per week was calculated, and using the 2009 Institute of Medicine criteria (1), women were classified as having recommended (REC, 170–270 g/week), excess (EXS, ≥270 g/week), or inadequate (INA, <170 g/week) weight gain. The primary outcome was daily energy intake throughout the second and third trimesters objectively assessed by the energy intake-balance method (29). Energy intake was calculated as the sum of mean energy expenditure across pregnancy (doubly labeled water) and energy deposition in fat and fat-free tissues (3-compartment model by plethysmography and isotope dilution) measured across the same observation period (29, 30). Secondary outcomes were changes in physical activity by accelerometry (31), energy expenditure during sleep by whole-body calorimetry (32), metabolic biomarkers, dietary intake by remote food photography (33, 34), and eating behavior constructs by validated questionnaires. Pregnancy, delivery, and infant outcomes were obtained from prenatal and delivery records.
Seventy-two pregnant women with obesity (BMI ≥ 30 kg/m2 at ≤15 weeks of gestation) were enrolled. Participants were required to be 18–40 years old and pregnant with a singleton gestation confirmed by ultrasound (≥6 weeks gestation). To study women with obesity who were otherwise healthy, participants were excluded for smoking, alcohol intake, drug use (prescription or recreational), hypertension (>160/110 mmHg), diabetes (HbA1c ≥6.5%), severe anemia (Hb <8 g/dL and/or Hct <24%), and for factors with the possibility of abnormally affecting gestational weight gain or adherence to the study protocol (e.g., preeclampsia, bed rest prescription) (20). The primary care obstetric provider and medical investigator provided medical clearance for participation. Women did not receive specific advice on diet or activity but were informed about the Institute of Medicine guidelines on healthy gestational weight gain.
Primary outcomes
Full descriptions of the study procedures have been previously described (20, 30, 34–36). In brief, at each assessment, participants presented to the research center for 2 outpatient visits and an overnight stay in a metabolic chamber (32). Body weight was measured fasted in a gown (with gown weight subtracted), and rate of gestational weight gain was calculated as change in measured body weight from early to late pregnancy, expressed in grams per week. Body fat mass was calculated using body weight, body volume by plethysmography (BODPOD, COSMED) and body water (mean estimate of using zero-intercepts of 2H and 18O-isotopes) (37). Fat-free mass was calculated as body weight minus fat mass. Energy deposition was calculated assuming that 1 kg of fat is equivalent to 9500 kcal and 1 kg of fat-free mass is equivalent to 771 kcal (29, 38). Free-living energy expenditure (TDEE) was measured over 7 days by doubly labeled water (1.25 g of 10% enriched H218O and 0.10 g of 99.9% enriched 2H2O per kg body weight) (20). TDEE across the observation period was calculated as the mean of the TDEE measured in early and late pregnancy. The primary outcome energy intake was calculated as sum of energy deposition and the mean energy expenditure across pregnancy.
Secondary outcomes
Energy metabolism was measured in the metabolic chamber. After participants ate a standard dinner at 1900 hours providing 30% of the estimated daily energy requirements (29) as 30% fat, 55% carbohydrate, and 15% protein, questionnaires were completed. Lights (including electronic screens) were off between 2230 hours and 0600 hours. Sleeping energy expenditure was the mean expenditure between 0200 hours and 0500 hours when activity (measured by infrared sensors) was <1% per minute, extrapolated to 24 hours (20). Adaptive thermogenesis is the difference between measured sleeping energy expenditure and the adjusted value. Upon waking, participants emptied their bladders and laid awake and supine on the bed for a 30-minute measurement of resting metabolic rate. Physical activity was assessed as physical activity level calculated as TDEE divided by resting metabolic rate as well as mean amplitude deviation by accelerometry (ActiGraph GT3X+) (31). Participants wore the accelerometer on the nondominant wrist during the 7-day doubly labeled water assessment. Simultaneously, diet quality was assessed using a validated SmartIntake smartphone application (33, 34). Eating behavior constructs were assessed using validated questionnaires as described (39). Fetal weight was estimated by 3D ultrasound with measurements of head circumference, biparietal diameter, abdominal circumference, and femoral length and volume (40), obtained by the same sonographer.
Estimate of change in energy intake for gestational weight gain
To estimate the change in energy intake needed for a certain gestational weight gain, we used data from the cohort to generate the following linear regression equation to estimate the energy intake from energy deposition (i.e., gestational weight gain): Change EI[kcal/d] = 1.178 ± 0.108*GWG [g/week] –225 ± 46; R2 = 0.70. In our cohort, we estimated change in energy intake as energy intake during pregnancy minus early pregnancy energy expenditure, assuming energy balance in early pregnancy, and gestational weight gain per week, as previously described in “Design and subjects.” Using the regression equation, gestational weight gain reported in previously published lifestyle intervention trials was used to compute the change in energy intake during pregnancy (6, 8–11, 21–25, 41–44).
Statistics
Power calculation.
Using our previous assessment of energy intake in a predominantly nonobese cohort (38), we conducted an a priori sample size analysis which assumed the following: β ≥ 0.80, α = 0.05, a 700 kcal/d SD for energy intake, and that the proportion of women with excess gestational weight gain would be 66% (1). Accordingly, a minimum of 51 subjects was required to detect a difference in energy intake of ±520 kcal/d. To achieve sufficient sample size considering miscarriages (n = 3), preterm deliveries (<37 weeks, n = 3), and attrition (n = 5), 72 women were enrolled.
Differences between weight gain groups were tested using linear mixed effect models with group used as a covariate. With change from early pregnancy values as the outcome, differences between weight gain groups were tested using linear mixed effect models with group and the initial observation (i.e., between 13–16 weeks gestation) used as a covariate. Additional covariates tested included maternal age, race, parity, and fetal sex, but inclusion of these did not change the outcomes of the analysis. Final models are therefore presented without these additional covariates. Only if a main effect of the weight gain groups was significant, post hoc comparisons were assessed. A P value less than 0.05 was considered significant. Reported P values in the manuscript refer to the pairwise post hoc comparison with the group with recommended weight gain (REC), unless indicated otherwise. Analyses were carried out using SAS, Version 9.4 (SAS Institute). Finally, a sensitivity analysis was performed with the 2 women with the highest BMI (46.0 and 57.1 kg/m2) removed. While the difference in weight and BMI noted for the INA group in early pregnancy was no longer significant, the results of the primary outcomes remained unchanged.
Study approval
The protocol was approved by the Institutional Review Board at Pennington Biomedical Research Center and all participants provided written informed consent prior to initiation of study procedures. This study is registered clinical trial at ClinicalTrials.gov (NCT01954342).
Author contributions
JM, LAG, MSA, ER, and LMR conceived the experiments and designed the study. JM, MSA, ADA, LAG, PMV, and DSH carried out experiments. JM, RAB, DMT, ER, and LMR analyzed data. JM and LMR drafted the manuscript. All authors had final approval of the submitted and published versions. LMR had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Supplementary Material
Acknowledgments
We would like to acknowledge administrative support from Elizabeth Sutton, Kelsey Olson, Alexandra Beyer, Alexis O’Connell, and Natalie Comardelle, and technical assistance of Jennifer Rood, Owen Carmichael, Kori Murray, Kevin McKlveen, Loren Cain, Kimberly Landry, Stephen Lee, Melissa Erickson, and Brian Gilmore (all Pennington Biomedical Research Center. This study was funded by the National Institutes of Health (R01DK099175 to LMR), with additional support by Clinical Research Cores at Pennington Biomedical Research Center (U54GM104940 and P30DK072476). We greatly appreciate the recruitment and retention support from Ralph Dauterive, Evelyn Griffin (Ochsner Health System), and Evelyn Hayes (Baton Rouge General Medical Center). Above all, we thank the participants for allowing us to follow their pregnancies.
Version 1. 08/01/2019
In-Press Preview
Version 2. 09/23/2019
Electronic publication
Version 3. 11/01/2019
Print issue publication
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Copyright: © 2019, American Society for Clinical Investigation.
Reference information: J Clin Invest. 2019;129(11):4682–4690.https://doi.org/10.1172/JCI130341.
See the related Commentary at Time to change weight gain recommendations for pregnant women with obesity.
Contributor Information
Jasper Most, Email: jasper.most@pbrc.edu.
Marshall St Amant, Email: marshallst.amant1@me.com.
Eric Ravussin, Email: Eric.Ravussin@pbrc.edu.
References
- 1. Institute of Medicine (US) National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines. In: Rasmussen KM, Yaktine AL, eds. Weight Gain During Pregnancy: Reexamining the Guidelines. Washington (DC); 2009. [Google Scholar]
- 2.Deputy NP, Sharma AJ, Kim SY, Hinkle SN. Prevalence and characteristics associated with gestational weight gain adequacy. Obstet Gynecol. 2015;125(4):773–781. doi: 10.1097/AOG.0000000000000739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Catalano PM, et al. Perinatal risk factors for childhood obesity and metabolic dysregulation. Am J Clin Nutr. 2009;90(5):1303–1313. doi: 10.3945/ajcn.2008.27416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mamun AA, Kinarivala M, O’Callaghan MJ, Williams GM, Najman JM, Callaway LK. Associations of excess weight gain during pregnancy with long-term maternal overweight and obesity: evidence from 21 y postpartum follow-up. Am J Clin Nutr. 2010;91(5):1336–1341. doi: 10.3945/ajcn.2009.28950. [DOI] [PubMed] [Google Scholar]
- 6.Dodd JM, et al. Antenatal lifestyle advice for women who are overweight or obese: LIMIT randomised trial. BMJ. 2014;348:g1285. doi: 10.1136/bmj.g1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simmons D, et al. Results from a European multicenter randomized trial of physical activity and/or healthy eating to reduce the risk of gestational diabetes mellitus: The DALI Lifestyle Pilot. Diabetes Care. 2015;38(9):1650–1656. doi: 10.2337/dc15-0360. [DOI] [PubMed] [Google Scholar]
- 8.Simmons D, et al. Effect of physical activity and/or healthy eating on GDM risk: The DALI Lifestyle Study. J Clin Endocrinol Metab. 2017;102(3):903–913. doi: 10.1210/jc.2016-3455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poston L, et al. Effect of a behavioural intervention in obese pregnant women (the UPBEAT study): a multicentre, randomised controlled trial. Lancet Diabetes Endocrinol. 2015;3(10):767–777. doi: 10.1016/S2213-8587(15)00227-2. [DOI] [PubMed] [Google Scholar]
- 10.Koivusalo SB, et al. Gestational diabetes mellitus can be prevented by lifestyle intervention: the Finnish gestational diabetes prevention study (RADIEL): a randomized controlled trial. Diabetes Care. 2016;39(1):24–30. doi: 10.2337/dc15-0511. [DOI] [PubMed] [Google Scholar]
- 11.Peaceman AM, et al. Lifestyle interventions limit gestational weight gain in women with overweight or obesity: LIFE-Moms prospective meta-analysis. Obesity (Silver Spring) 2018;26(9):1396–1404. doi: 10.1002/oby.22250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. American College of Obstetricians Gynecologists. Nutrition in Pregnancy. In: Your Pregnancy and Childbirth: Month to Month, Sixth Edition. Washington, DC: ACOG; 2016:313–327. [Google Scholar]
- 13. Institute of Medicine. Energy. In: Dietary Reference Intake for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington, DC: The National Academies Press; 2005:107–264. [Google Scholar]
- 14.Butte NF, Wong WW, Treuth MS, Ellis KJ, O’Brian Smith E. Energy requirements during pregnancy based on total energy expenditure and energy deposition. Am J Clin Nutr. 2004;79(6):1078–1087. doi: 10.1093/ajcn/79.6.1078. [DOI] [PubMed] [Google Scholar]
- 15.Goldberg GR, et al. Longitudinal assessment of energy expenditure in pregnancy by the doubly labeled water method. Am J Clin Nutr. 1993;57(4):494–505. doi: 10.1093/ajcn/57.4.494. [DOI] [PubMed] [Google Scholar]
- 16.Kopp-Hoolihan LE, van Loan MD, Wong WW, King JC. Longitudinal assessment of energy balance in well-nourished, pregnant women. Am J Clin Nutr. 1999;69(4):697–704. doi: 10.1093/ajcn/69.4.697. [DOI] [PubMed] [Google Scholar]
- 17.Evenson KR, Chasan-Taber L, Symons Downs D, Pearce EE. Review of self-reported physical activity assessments for pregnancy: summary of the evidence for validity and reliability. Paediatr Perinat Epidemiol. 2012;26(5):479–494. doi: 10.1111/j.1365-3016.2012.01311.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas DM, et al. Relationships between misreported energy intake and pregnancy in the pregnancy, infection and nutrition study: new insights from a dynamic energy balance model. Obes Sci Pract. 2016;2(2):174–179. doi: 10.1002/osp4.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lederman SA, Paxton A, Heymsfield SB, Wang J, Thornton J, Pierson RN. Body fat and water changes during pregnancy in women with different body weight and weight gain. Obstet Gynecol. 1997;90(4 Pt 1):483–488. doi: 10.1016/s0029-7844(97)00355-4. [DOI] [PubMed] [Google Scholar]
- 20.Most J, et al. Energy expenditure in pregnant women with obesity does not support energy intake recommendations. Obesity (Silver Spring) 2018;26(6):992–999. doi: 10.1002/oby.22194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Petrella E, et al. Gestational weight gain in overweight and obese women enrolled in a healthy lifestyle and eating habits program. J Matern Fetal Neonatal Med. 2014;27(13):1348–1352. doi: 10.3109/14767058.2013.858318. [DOI] [PubMed] [Google Scholar]
- 22.Renault KM, et al. The treatment of obese pregnant women (TOP) study: a randomized controlled trial of the effect of physical activity intervention assessed by pedometer with or without dietary intervention in obese pregnant women. Am J Obstet Gynecol. 2014;210(2):134.e1–134.e9. doi: 10.1016/j.ajog.2013.09.029. [DOI] [PubMed] [Google Scholar]
- 23.Thornton YS, Smarkola C, Kopacz SM, Ishoof SB. Perinatal outcomes in nutritionally monitored obese pregnant women: a randomized clinical trial. J Natl Med Assoc. 2009;101(6):569–577. doi: 10.1016/S0027-9684(15)30942-1. [DOI] [PubMed] [Google Scholar]
- 24.Vesco KK, et al. Efficacy of a group-based dietary intervention for limiting gestational weight gain among obese women: a randomized trial. Obesity (Silver Spring) 2014;22(9):1989–1996. doi: 10.1002/oby.20831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wolff S, Legarth J, Vangsgaard K, Toubro S, Astrup A. A randomized trial of the effects of dietary counseling on gestational weight gain and glucose metabolism in obese pregnant women. Int J Obes (Lond) 2008;32(3):495–501. doi: 10.1038/sj.ijo.0803710. [DOI] [PubMed] [Google Scholar]
- 26.Bodnar LM, et al. Low gestational weight gain and risk of adverse perinatal outcomes in obese and severely obese women. Epidemiology. 2016;27(6):894–902. doi: 10.1097/EDE.0000000000000535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Durie DE, Thornburg LL, Glantz JC. Effect of second-trimester and third-trimester rate of gestational weight gain on maternal and neonatal outcomes. Obstet Gynecol. 2011;118(3):569–575. doi: 10.1097/AOG.0b013e3182289f42. [DOI] [PubMed] [Google Scholar]
- 28.Tsigga M, Filis V, Hatzopoulou K, Kotzamanidis C, Grammatikopoulou MG. Healthy eating index during pregnancy according to pre-gravid and gravid weight status. Public Health Nutr. 2011;14(2):290–296. doi: 10.1017/S1368980010001989. [DOI] [PubMed] [Google Scholar]
- 29.Thomas DM, et al. Dynamic energy-balance model predicting gestational weight gain. Am J Clin Nutr. 2012;95(1):115–122. doi: 10.3945/ajcn.111.024307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Most J, et al. Is energy balance in pregnancy involved in the etiology of gestational diabetes in women with obesity? Cell Metab. 2019;29(2):231–233. doi: 10.1016/j.cmet.2018.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vähä-Ypyä H, Vasankari T, Husu P, Suni J, Sievänen H. A universal, accurate intensity-based classification of different physical activities using raw data of accelerometer. Clin Physiol Funct Imaging. 2015;35(1):64–70. doi: 10.1111/cpf.12127. [DOI] [PubMed] [Google Scholar]
- 32.Lam YY, Ravussin E. Analysis of energy metabolism in humans: a review of methodologies. Mol Metab. 2016;5(11):1057–1071. doi: 10.1016/j.molmet.2016.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Martin CK, et al. Validity of the remote food photography method (RFPM) for estimating energy and nutrient intake in near real-time. Obesity (Silver Spring) 2012;20(4):891–899. doi: 10.1038/oby.2011.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Most J, et al. Food photography is not an accurate measure of energy intake in obese, pregnant women. J Nutr. 2018;148(4):658–663. doi: 10.1093/jn/nxy009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Most J, et al. Propensity for adverse pregnancy outcomes in African-American women may be explained by low energy expenditure in early pregnancy. Am J Clin Nutr. 2018;107(6):957–964. doi: 10.1093/ajcn/nqy053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Most J, Redman LM. Does energy expenditure influence body fat accumulation in pregnancy? Am J Obstet Gynecol. 2019;220(1):119–120. doi: 10.1016/j.ajog.2018.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Most J, Marlatt KL, Altazan AD, Redman LM. Advances in assessing body composition during pregnancy. Eur J Clin Nutr. 2018;72(5):645–656. doi: 10.1038/s41430-018-0152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gilmore LA, Butte NF, Ravussin E, Han H, Burton JH, Redman LM. Energy intake and energy expenditure for determining excess weight gain in pregnant women. Obstet Gynecol. 2016;127(5):884–892. doi: 10.1097/AOG.0000000000001372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Most J, Rebello CJ, Altazan AD, Martin CK, Amant MS, Redman LM. Behavioral determinants of objectively assessed diet quality in obese pregnancy. Nutrients. 2019;11(7):E1446. doi: 10.3390/nu11071446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee W, et al. New fetal weight estimation models using fractional limb volume. Ultrasound Obstet Gynecol. 2009;34(5):556–565. doi: 10.1002/uog.7327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cahill AG, et al. Weight control program and gestational weight gain in disadvantaged women with overweight or obesity: a randomized clinical trial. Obesity (Silver Spring) 2018;26(3):485–491. doi: 10.1002/oby.22070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gallagher D, et al. Greater neonatal fat-free mass and similar fat mass following a randomized trial to control excess gestational weight gain. Obesity (Silver Spring) 2018;26(3):578–587. doi: 10.1002/oby.22079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Phelan S, Phipps MG, Abrams B, Darroch F, Schaffner A, Wing RR. Randomized trial of a behavioral intervention to prevent excessive gestational weight gain: the Fit for Delivery Study. Am J Clin Nutr. 2011;93(4):772–779. doi: 10.3945/ajcn.110.005306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Van Horn L, et al. Dietary approaches to stop hypertension diet and activity to limit gestational weight: maternal offspring metabolics family intervention trial, a technology enhanced randomized trial. Am J Prev Med. 2018;55(5):603–614. doi: 10.1016/j.amepre.2018.06.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.