Abstract
Background:
Vaccination rates against Human Papillomavirus (HPV) in the US remain alarmingly low. Physicians can significantly influence a parent’s decision to vaccinate their children. However, medical education often lacks training on specific strategies for communicating with vaccine hesitant parents.
Methods:
We created an innovative curriculum designed to teach medical students how to address HPV vaccine hesitancy. The curriculum consisted of (1) a presentation on the epidemiology, biology, and disease morbidity associated with HPV, (2) a video that teaches specific communication strategies and (3) role-playing simulations. This curriculum was delivered to medical students at two separate sites. Medical students were surveyed before and after completing the educational curriculum. The surveys assessed student comfort talking to HPV vaccine hesitant parents and their likelihood to recommend the HPV vaccine.
Results:
Pre- and post-intervention surveys were completed by 101 of the 132 participants (77% response rate). After the intervention, student awareness of the benefits of the HPV vaccine increased by a mean of 0.82 points (Likert scale 1–5, p < 0.01) and student comfort talking to vaccine hesitant parents increased by a mean of 1.37 points (p < 0.01). Prior to the intervention, students more strongly recommended the HPV vaccine to females compared to males, but this gender disparity was eliminated after the intervention (p < 0.01). Personal vaccination status was independately associated with a higher likelihood of recommending the HPV vaccine both before and after the intervention.
Conclusion:
Our innovative curriculum improved medical student comfort level discussing HPV vaccination with hesitant parents and increased the perceived likelihood of recommending HPV vaccination. The intervention is easy to implement, scalable, and requires minimal resources. Educating future providers on this important topic has the potential to improve vaccination rates nationwide and thus should be considered for all medical students.
Keywords: Human Papillomavirus (HPV), HPV vaccine, Vaccine hesitancy, Medical education, C.A.S.E. method, Curriculum
1. Introduction
Human Papillomavirus (HPV) is the most common sexually transmitted infection in the US, with approximately 14 million new cases occurring each year [1]. It is associated with the development of pre-invasive and invasive cancers of the cervix, vulva, vagina, anus, penis and oropharynx with over 38,000 HPV-associated cancers diagnosed in the US each year [2]. HPV vaccination holds promise for reduction of disease burden in the US and worldwide.
HPV vaccination was first approved for young women in the US in 2006. Since then, its approval has been expanded to both males and females. The newest 9-valent HPV vaccine protects against up to 73.5% of HPV-associated cancers [3]. Unfortunately, HPV vaccination rates in the US remain low, with completion rates of 49.5% for females and 37.5% for males nationwide [4]. Furthermore, HPV vaccination is becoming increasingly important as the prevalence of HPV-containing oropharyngeal squamous cell carcinomas has increased dramatically and is now the most common HPV associated cancer [5].
Vaccine hesitancy has become a concerning issue among healthcare providers, as many parents refuse or choose to delay vaccines for their children [6]. Vaccine refusal happens for many reasons, including social influences and concerns about vaccine safety, necessity, and cost [7]. Notably, lack of physician recommendation is frequently cited as the primary reason parents choose not to vaccinate [7–10]. Physicians influence parental beliefs and attitudes and it is well established that provider recommendation improves vaccination rates [11]. Results from US national immunization survey found that female adolescents who received a provider recommendation for the HPV vaccine were almost 5 times more likely to initiate the HPV vaccine series compared to adolescents who did not receive this recommendation, and this association persisted across all races and sociodemographic groups [12].
Many providers report inadequate training and low comfort levels responding to questions from vaccine hesitant parents [13,14]. Improving provider comfort and teaching communication strategies is key to addressing low vaccination rates [15]. Providing a curriculum that addresses vaccine hesitancy during medical school has the potential to reach a broad population of future physicians. In this study we hypothesized that applying a multi-modal curriculum (including evidence-based lecture, communication methodology, and simulation training) targeted at medical students would improve medical student confidence in addressing the concerns of vaccine hesitant parents. Improving confidence in addressing vaccine hesitant parents is an important step towards improving vaccination rates nationwide and thus should be a part of medical school training.
2. Materials and methods
All medical students at the University of Minnesota were eligible to participate in this educational curriculum and research study. This study was conducted at the University of Minnesota Medical School, Twin Cities (UMTC) and Duluth (UMD) campuses. Announcements were emailed to all medical school students at both campuses. On the day of the study pre-clinical students were notified by an in class announcement. After obtaining informed consent, medical students completed a pre-intervention survey. They then participated in an HPV vaccination curriculum consisting of a lecture, video, and role-play simulation. At the end of the study period they completed a post-intervention survey. Participation in the surveys and the HPV vaccination curriculum was voluntary. This study was approved by the University of Minnesota Institutional Review Board.
2.1. HPV vaccination curriculum
The curriculum began with a presentation by a board-certified Gynecologic Oncology physician. The presentation highlighted the epidemiology of HPV associated disease, basic science of the HPV virus and vaccine, and treatment and prognosis of HPV related cancers.
Next, students watched a video on implementing both the presumptive method and the C.A.S.E. (Corroborate, About me, Science, and Explain/advise) method with vaccine hesitant parents [16].
The presumptive method teaches students to use a direct statement when discussing vaccination, such as “Today you will be receiving your HPV vaccine.” Students were taught not to use participatory language, such as “Would you like to receive your vaccine today?”. If the presumptive approach was unsuccessful, students were instructed to then use the C.A.S.E. method to provide a framework to address the parent’s concerns in a compassionate manner.
The C.A.S.E. method provides an organized approach toward conversing with a vaccine hesitant parent [16]. It allows the physician to address the parent’s concern, while keeping the conversation focused. First, the clinician asks for the parent’s specific concern regarding vaccination. Then they proceed through the following steps: (C) Corroborate by acknowledging and validating the patient’s concern, (A) About Me by explaining how the physician became an expert on the issue, (S) Science by relaying the scientific facts addressing the parent’s concern, and (E) Explain/Advise by summarizing the recommendation, emphasizing the health risks of HPV infection, and strongly urging the parent to agree to the vaccine. If the exact science behind the concern was not known, students were instructed to ensure parents that the vaccine is safe, effective, and protects against a dangerous disease. The video explained the C.A.S.E. method and showed medical students interacting with a vaccine hesitant parent who believed natural immunity was better for their child.
The final segment of the curriculum involved a simulation roleplay. Students self-sorted into groups of 3 and role-played 3 separate scenarios using the presumptive and C.A.S.E. methods. For each scenario students played the role of either a provider, patient or observer. An example C.A.S.E conversation with a checklist was provided to the observer to help direct the conversation if students needed guidance and to facilitate giving constructive feedback after each scenario.
2.2. Pre-intervention and post-intervention surveys
An anonymous, 9-question pre-intervention survey and 14-question post-intervention survey were administered to assess each student’s gender, personal vaccination status, likelihood of recommending the HPV vaccine to varying age groups/genders, and comfort conversing with HPV vaccine hesitant parents. The post-intervention survey also assessed student opinion on the C.A.S.E. method as a useful approach in talking to vaccine hesitant parents. Both surveys contained Likert scales, which ranged from 1 to 5 with 1 corresponding to “never recommend” or “not comfortable” and 5 corresponding to “always recommend” or “extremely comfortable.” The pre-intervention survey was administered to all participants at the beginning of the training session. The post-intervention survey was administered immediately following completion of the HPV vaccination curriculum. Students who did not complete a question or illegibly circled an answer were treated as missing for that question.
2.3. Statistical analysis
Our primary objective was to determine if the HPV curriculum increased HPV vaccine awareness, likelihood to recommend, and comfort level conversing with vaccine hesitant parents. We initially performed Wilcoxon signed rank tests for all statistical analyses with resulting p values <0.01. Based on our sample size and the robustness of parametric tests, we determined that paired T-tests would better represent the data [17]. Thus, for the primary outcome, paired T-tests were performed to determine if there were differences in Likert responses between pre- and post-intervention surveys and between various survey questions. Paired T-tests were performed for various questions for the different strata of location, gender, and student vaccination status. To investigate the effect of student vaccination status, cumulative logit models were performed, with and without adjustment for gender. Subjects’ opinions on the C.A.S.E. method post intervention were descriptively summarized using bar plots. A one-sample T-test was performed to determine if the Likert responses for the C.A.S.E. method questions were different from neutral. Due to the nature of this study, we did not perform a sample size calculation, and used a sample size of convenience. All reported p-values were two sided. An alpha of less than 0.05 was considered statistically significant. All statistical analyses were performed using SAS (version 9.4, SAS Institute, Inc., Cary, North Carolina).
3. Results
3.1. Demographics
In our study, 132 medical students participated in the HPV vaccine training session (14% of the student body). Of these, 101 completed the pre- and post-intervention surveys, yielding an overall response rate of 77%. Of the respondents, 83 (82%) were in pre-clinical training, 13 (13%) were in clinical training years, and 5 (5%) did not specify. 67 (66%) of the students self-identified as female, 33 (33%) self-identified as male, and 1 (1%) did not specify (Table 1). Of the 101 respondents, 71 (70%) self-reported that they had personally been vaccinated against HPV. Female medical students reported a higher vaccination rate than their male counter-parts (91% vs 30%, p < 0.01).
Table 1.
Demographics of survey participants (n = 101).
| Variable | n (%) |
|---|---|
| Year in Medical School | |
| 1 | 64 (63) |
| 2 | 19 (19) |
| 3 | 12 (12) |
| 4 | 1 (1) |
| Did not specify | 5 (5) |
| Gender | |
| Female | 67 (66) |
| Male | 33 (33) |
| Did not specify | 1 (1) |
| Personally received HPV vaccination | |
| Yes | 71 (70) |
| No | 28 (28) |
| Did not specify | 2 (2) |
3.2. Likert scale responses
Our intervention increased students’ awareness of the benefits of the HPV vaccine, likelihood of recommending the vaccine to both females and males, and comfort level in talking to vaccine hesitant parents (Table 2). On a Likert scale of 1–5, students increased their awareness of the benefits of the HPV vaccine by an average of 0.82 points (95% CI 0.66–0.97, p < 0.01) and students increased their comfort level in talking to vaccine hesitant parents by an average of 1.37 points (95% CI 1.20–1.54, p < 0.01) (Table 2). More specifically, after the curriculum, more students felt they were very aware (score of 5) of the benefits of the HPV vaccine (73% vs 27%, p < 0.01). Results for all questions remained significant even after stratifying by gender, personal vaccination status, and location of curriculum.
Table 2.
Results for paired survey questions asked before and after HPV vaccine curriculum (N = 101).b
| Question | Mean Change in Likert response (95% CI)c |
p-valuea |
|---|---|---|
| Please rate your level of awareness of the benefits of the HPV Vaccine | +0.82 (0.66, 0.97) | <0.01 |
| Please rate how strongly you would recommend the HPV Vaccine to a female patient during a physical | +0.46 (0.33, 0.59) | <0.01 |
| Please rate how strongly you would recommend the HPV Vaccine to a female patient during a other visit | +0.84 (0.67, 1.01) | <0.01 |
| Please rate how strongly you would recommend the HPV Vaccine to a male patient during a physical | +0.96 (0.77, 1.15) | <0.01 |
| Please rate how strongly you would recommend the HPV Vaccine to a male patient during a other visit | +1.21 (1.01, 1.41) | <0.01 |
| Providers should recommend the HPV Vaccine to all eligible patients in their practice | +0.35 (0.23, 0.48) | < 0.01 |
| I would recommend the HPV Vaccine to eligible 9–10 year olds with vaccine hesitant parents | +0.81 (0.61, 1.01) | <0.01 |
| I would recommend the HPV Vaccine to eligible 11–17 year olds with vaccine hesitant parents | +0.41 (0.27, 0.55) | <0.01 |
| I would recommend the HPV Vaccine to eligible 17–26 year olds with vaccine hesitant parents | +0.32 (0.20, 0.43) | <0.01 |
| Please rate your comfort level conversing with HPV vaccine hesitant parents/patients | +1.37 (1.20, 1.54) | <0.01 |
| Please rate your comfort level educating patients and families who are hesitant about other medical decision (test, treatments, etc.) | +1.20 (1.04, 1.36) | <0.01 |
P-value is for paired t-test comparing pre- and post-intervention Likert responses for each survey question.
N varies by question and ranges between 98 and 101.
Mean change and 95% CI are for the difference in Likert responses between pre- and post-intervention.
This curriculum was performed at two separate sites (Minneapolis, MN and Duluth, MN) and by two distinct facilitators to examine ease of implementation and reliability between sites. The mean differences in pre- and post-intervention survey results were consistent between the two sites on all questions except one. There was a statistically significant difference in improvement of awareness of the benefits of the HPV vaccine between the two sites, with more improvement in awareness noted at the Duluth site (mean change 1.24 vs 0.67, p < 0.01).
Before the intervention, students recommended the HPV vaccine more strongly to females compared to males at routine physicals (mean difference 0.51, 95% CI 0.37–0.66, p < 0.01). After the intervention, students no longer recommended more strongly to females compared to males (mean difference 0.01, 95% CI 0.02–0.04, p = 0.57). Thus, after the intervention, the gender disparity was eliminated.
We also examined differences in student frequency of recommendation of the HPV vaccine to three different age groups: pre-adolescents (age 9–10), adolescents (age 11–17), and young adults (age 17–26). Students were more likely to recommend to both adolescents and young adults compared to pre-adolescents (p < 0.01). The curriculum did not change this inclination (p < 0.01).
We also sought to investigate the impact of provider vaccination status on likelihood of recommending the HPV vaccine. Before and after the intervention, subjects who had personally received the HPV vaccine were more likely to recommend the vaccine compared to those who were unvaccinated (p < 0.01). Even when adjusting for gender (as more female students were personally vaccinated against HPV), this effect of vaccination status remained significant.
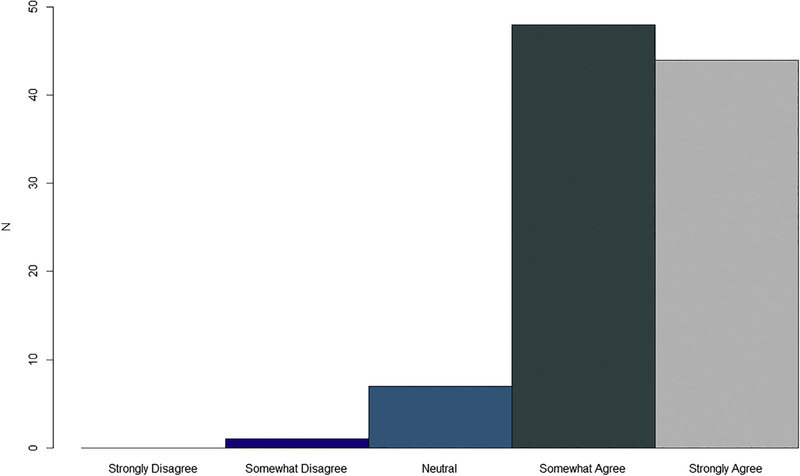
Finally, students were surveyed on their perceived usefulness of the C.A.S.E method to address HPV vaccine hesitancy in their future clinical encounters (1 = strongly disagree, 5 = strongly agree). Scores of 4 and 5 were categorized as agreement that the C.A.S.E. method is a useful tool. Greater than 90% of students found the C.A.S.E approach useful not only to talk about vaccine hesitancy but also to discuss other medical concerns (Fig. 1).
Fig. 1.
Likert responses for the statement “The C.A.S.E. approach is very useful in talking to HPV hesitant patients/parents”.
3.3. Likert scale assessment
The survey was evaluated post hoc- using Cronbach’s Alpha to evaluate internal consistency of the Likert scale responses. Variables were assigned to 5 groupings. Group 1 broadly measured HPV vaccine awareness. Group 2 measured self-perceived likelihood to recommend the HPV vaccine during a physical. Group 3 measured self-perceived likelihood to recommend during any other visit type. Group 4 broadly assessed comfort level in holding conversations in with vaccine hesitant parents. Finally, group 5 measured perception of the C.A.S.E. method as a useful tool in both HPV vaccine-specific conversations and when discussing other medical concerns with parents. All Cronbach’s alphas were found to be greater than 0.70, suggesting that the pre- and post-surveys are reliable both overall and when looking at groupings of variables expected to measure similar items.
4. Discussion
In this study we demonstrated that our novel HPV vaccine hesitancy curriculum increased students’ awareness of the benefits of the HPV vaccine, perceived likelihood of recommending the vaccine to both females and males, and comfort level in talking to vaccine hesitant parents. This curriculum was performed at two different locations with similar results, supporting its applicability to other medical schools. Vaccine hesitancy continues to be a difficult problem to address, yet evidence clearly supports the benefit of a strong clinician recommendation to vaccinate [7,9,18,19]. Furthermore, strength of recommendation is a significant factor in a parent’s decision to vaccinate [11]. In a survey of parents of adolescents, quality of the clinician recommendation for HPV vaccination had a significant association with HPV vaccine initiation and completion [20]. A strong recommendation was defined by a strong endorsement, inclusion of a cancer prevention message, and recommendation of same day vaccination [20]. This concept has been replicated in other studies as well, further emphasizing that a strong provider recommendation improves vaccine uptake [21].
The type of communication most effective for HPV vaccine initiation has been examined in many studies. Opel, et al. found that the presumptive approach, included in our curriculum, leads to a 74% acceptance rate of the vaccine, compared to only 4% with a participatory approach [22]. A study comparing two interventions to address anti-vaccination attitudes found that providing factual information about the dangers of vaccine preventable diseases is more effective than an alternative intervention aimed at countering vaccination myths [23]. Greater knowledge of HPV and the HPV vaccine among pediatric and family medicine doctors has been shown to be associated with higher rates of HPV vaccination initiation and completion [24]. Dempsey et al. used a 5 component method (provider education, patient education, disease pictures, presumptive method, how to make recommendations) to improve HPV vaccination initiation [15]. This body of research on effective methods for communication with HPV vaccine hesitant parents indicates that a multi-faceted approach is best, beginning with a presumptive statement, followed by a statement of scientific fact regarding the risk of disease pertaining to the individual patient, and concluding with a strong recommendation to vaccinate. Our novel HPV vaccine training curriculum for medical school students incorporates all these elements.
Vaccine communication training is not currently a standard component of medical education. A recent study found that of 92 pediatric residency programs in the US, only 41% of programs had formal training in vaccine safety and communication strategies for vaccine-hesitant patients [25]. Moreover, intervening by teaching communication methods to physicians after residency has not been effective at improving physician comfort conversing with vaccine hesitant parents [14]. Therefore, by initiating an intervention at the medical school level we have a potential to fill this training gap, target all medical specialties, and make future physicians more comfortable conversing with vaccine hesitant parents before practice patterns are established.
The primary limitation of this study is the absence of a comparison intervention with students who did not complete the HPV vaccination curriculum. It was important that all students had access to this curriculum in our medical school, as vaccine education is an important medical school initiative. Therefore, we chose to allow all interested students to participate in the curriculum. Future studies may include randomizing students to various interventions to determine specifically the most effective intervention. In addition, future studies should incorporate longitudinal follow up of student attitudes to ensure that student comfort talking to vaccine hesitant parents remains high over time.
Our primary outcome was self-reported comfort in HPV vaccine counseling and perceived likelihood to recommend the HPV vaccine. Because the ultimate goal is improvement in HPV vaccination rates, a more objective outcome would be measuring changes in individual provider vaccination rates. This was not feasible given the long time between medical student education and individual practice patterns that are seen after residency training. However, future research at our institution is aimed at identifying statewide trends in vaccination rates as multiple interventions are being implemented.
Finally, health disparities were not addressed in this study, but should be addressed in future interventions. Rates of HPV series completion are lower for black adolescents than white adolescents in the US [26], and lower among females below the poverty level compared with females at or above poverty level [19]. This disparity is particularly concerning given that cervical cancer incidence and mortality are higher among black women than white women [7]. It is essential that information about the HPV vaccine is provided to underserved populations in a culturally sensitive and more effective manner, and that access and cost of vaccination be investigated. Future studies should incorporate attitudes about barriers to vaccination in underserved populations and educational curriculum regarding these disparities.
5. Conclusions
Educating all future physicians to recommend vaccination and respond compassionately to vaccine hesitant parents is a core responsibility of medical training. Though most of this training is expected to happen in residency, vaccine training thus far has not been consistently provided to residents. This study is unique in that it targets medical students at an earlier stage of training by providing a multi-modal educational curriculum involving didactic teaching, video instruction, and role-play simulation. Our curriculum is based on a large body of research that provides insight into how to best talk to vaccine hesitant parents. After the intervention, medical students were more likely to recommend the HPV vaccine and reported a higher comfort level in discussing the HPV vaccine with vaccine hesitant parents. The intervention is easy to implement, scalable, and requires minimal resources. Further studies should investigate whether attitudes and comfort levels persist months to years following this type of intervention.
Acknowledgments
We would like to thank the entire Hands-On Advocacy 2016–2017 team for their work on this project and other projects in their campaign to increase Minnesota’s vaccination rates. We would like to thank Juliana Milhofer and the Minnesota Medical Association for providing graphic design of curriculum materials. We would like to thank Robert Jacobson, MD; Eric Schnaith, MD; and Suzanne van den Hoogenhof, PhD. for reviewing and editing the curriculum and pre-/post-intervention surveys.
Financial support
This work was supported by Hub and Spoke Initiative Focused on Improving HPV Rates, AAP Chapter MN, ND, SD. Research support in this publication to KMT was supported by NIH grant P30 CA77598 utilizing the Biostatistics and Bioinformatics Core shared resource of the Masonic Cancer Center, University of Minnesota and by the National Center for Advancing Translational Sciences of the National Institutes of Health Award Number UL1TR000114. Research support to BKE was from the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number K12HD055887. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of interest
The authors do not have any commercial or other associations that might pose a conflict of interest.
References
- [1].Incidence, Prevalence, and Cost of Sexually Transmitted Infections in the United States. Centers for Disease Control and Prevention, National Center for HIV Viral Hepatitis STD and TB Prevention; 2013. [Google Scholar]
- [2].Viens LJ, Henley J, Thom TD. Human papillomavirus-associated cancers United States, 2008–2012. Mmwr-Morbidity Mortality Weekly Report 2016;65:661–6. 10.15585/mmwr.mm6526a1. [DOI] [PubMed] [Google Scholar]
- [3].Petrosky E, Bocchini JA, Hariri S, Chesson H, Curtis CR, Saraiya M, et al. Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the advisory committee on immunization practices. Mmwr-Morbidity Mortality Weekly Report 2015;64:300–4. [PMC free article] [PubMed] [Google Scholar]
- [4].Walker TY, Elam-Evans LD, Singleton JA, Yankey D, Markowitz LE, Fredua B, et al. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years - United States, 2016. Mmwr-Morbidity and Mortality Weekly Report. 2017;66:874–82. 10.15585/mmwr.mm6633a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Saraiya M, Unger ER, Thompson TD, Lynch CF, Hernandez BY, Lyu CW, et al. US assessment of HPV types in cancers: implications for current and 9-valent HPV vaccines. Jnci-J Nat Cancer Inst 2015;107 10.1093/jnci/djv086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Smith PJ, Humiston SC, Marcuse EK, Zhao Z, Dorell CG, Howes C, et al. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the health belief model. Public Health Reports. 2011;126:135–46. 10.1177/00333549111260s215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents a systematic review of the literature. Jama Pediatrics 2014;168:76–82. 10.1001/jamapediatrics.2013.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Brewer NT, Gottlieb SL, Reiter PL, McRee AL, Liddon N, Markowitz L, et al. Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sex Transm Dis 2011;38:197–204. 10.1097/OLQ.0b013e3181f12dbf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Moss JL, Reiter PL, Rimer BK, Brewer NT. Collaborative patient-provider communication and uptake of adolescent vaccines. Soc Sci Med 2016;159:100–7. 10.1016/j.socscimed.2016.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Lindley MC, Jeyarajah J, Yankey D, Curtis CR, Markowitz LE, Stokley S. Comparing human papillomavirus vaccine knowledge and intentions among parents of boys and girls. Hum Vaccines Immunotherap 2016;12:1519–27. 10.1080/21645515.2016.1157673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Rosenthal SL, Weiss TW, Zimet GD, Ma L, Good MB, Vichnin MD. Predictors of HPV vaccine uptake among women aged 19–26: Importance of a physician’s recommendation. Vaccine 2011;29:890–5. 10.1016/j.vaccine.2009.12.063. [DOI] [PubMed] [Google Scholar]
- [12].Ylitalo KR, Lee H, Mehta NK. Health care provider recommendation, human papillomavirus vaccination, and race/ethnicity in the US national immunization survey. Am J Public Health 2013;103:164–9. 10.2105/ajph.2011.300600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Kerneis S, Jacquet C, Bannay A, May T, Launay O, Verger P, et al. Vaccine education of medical students: a nationwide cross-sectional survey. Am J Prev Med 2017;53:E97–E104. 10.1016/j.amepre.2017.01.014. [DOI] [PubMed] [Google Scholar]
- [14].Henrikson NB, Opel DJ, Grothaus L, Nelson J, Scrol A, Dunn J, et al. Physician communication training and parental vaccine hesitancy: a randomized trial. Pediatrics 2015;136:70–9. 10.1542/peds.2014-3199. [DOI] [PubMed] [Google Scholar]
- [15].Dempsey AF, Pyrznawoski J, Lockhart S, Barnard J, Campagna EJ, Garrett K, et al. Effect of a health care professional communication training intervention on adolescent human papillomavirus vaccination a cluster randomized clinical trial JAMA. Pediatrics 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Jacobson R, Van Etta L, Bahta L . The C.A.S.E approach: guidance for talking with vaccine-hesitant parents. Minnesota Med 2013;96:49–50. 10.1001/jamapediatrics.2018.0016. [DOI] [PubMed] [Google Scholar]
- [17].Norman G Likert scales, levels of measurement and the “laws” of statistics. Adv Health Sci Educ 2010;15:625 10.1007/s10459-010-9222-y. [DOI] [PubMed] [Google Scholar]
- [18].Bartlett JA, Peterson JA. The Uptake of Human Papillomavirus (HPV) Vaccine among Adolescent Females in the United States: A Review of the Literature. J School Nurs 2011;27:434–46. 10.1177/1059840511415861. [DOI] [PubMed] [Google Scholar]
- [19].Smith PJ, Stokley S, Bednarczyk RA, Orenstein WA, Omer SB. HPV vaccination coverage of teen girls: The influence of health care providers. Vaccine 2016;34:1604–10. 10.1016/j.vaccine.2016.01.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Gilkey MB, Calo WA, Moss JL, Shah PD, Marciniak MW, Brewer NT. Provider communication and HPV vaccination: The impact of recommendation quality. Vaccine 2016;34:1187–92. 10.1016/j.vaccine.2016.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Kulczycki A, Qu H, Shewchuk R. Primary Care Physicians’ Adherence to Guidelines and Their Likelihood to Prescribe the Human Papillomavirus Vaccine for 11- and 12-Year-Old Girls. Women’s health issues: official publication of the Jacobs Institute of Women’s Health. 2016;26:34–9. 10.1016/j.whi.2015.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Opel DJ, Heritage J, Taylor JA, Mangione-Smith R, Salas HS, DeVere V, et al. The architecture of provider-parent vaccine discussions at health supervision visits. Pediatrics 2013;132:1037–46. 10.1542/peds.2013-2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Horne Z, Powell D, Hummel JE, Holyoak KJ. Countering antivaccination attitudes. Proc National Acad Sci United States of America 2015;112:10321–4. 10.1073/pnas.1504019112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Rutten LJF, St Sauver JL, Beebe TJ, Wilson PM, Jacobson DJ, Fan C, et al. Clinician knowledge, clinician barriers, and perceived parental barriers regarding human papillomavirus vaccination: Association with initiation and completion rates. Vaccine 2017;35:164–9. 10.1016/j.vaccine.2016.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Williams SE, Swan R. Formal training in vaccine safety to address parental concerns not routinely conducted in US pediatric residency programs. Vaccine 2014;32:3175–8. 10.1016/j.vaccine.2014.04.001. [DOI] [PubMed] [Google Scholar]
- [26].De P, Budhwani H. Human papillomavirus (HPV) vaccine initiation in minority Americans. Public Health. 2017;144:86–91. 10.1016/j.puhe.2016.11.005. [DOI] [PubMed] [Google Scholar]