Abstract
Objective
To compare the clinical and radiological outcomes of patients who underwent rotator cuff repair (RCR) concomitant with long head of the biceps tendon (LHBT) tenotomy or subpectoral mini‐open tenodesis.
Methods
Prospectively collected data was reviewed on 154 patients, who underwent a LHBT procedure (tenotomy or tenodesis) concomitant with RCR between January 2010 and January 2017. The exclusion criteria were irreparable massive rotator cuff tear, rotator cuff partial tear, subscapular tendon tear, glenohumeral arthritis, and prior shoulder surgery. The two patient groups are as follows: RCR + Tenotomy (Group A) and RCR + Subpectoral mini‐open tenodesis (Group B). The visual analog scale (VAS) for pain, Constant Score scale, American Shoulder and Elbow Surgeons (ASES) scores, and the Disabilities of the Arm, Shoulder and Hand (DASH) scores preoperatively and 1 month, 3 months, 6 months, 1 year postoperatively and the latest out‐patient clinic were compared between the two groups.
Results
Ninety‐two patients in Group A and 62 patients in Group B completed the follow‐up, with a median follow‐up time of 27 and 42 months respectively. At the final follow‐up, the VAS, Constant, ASES, and DASH scores in Group A were 0.1 ± 0.2, 87.0 ± 12.8, 96.4 ± 4.3 and 6.6 ± 4.8 respectively, and the VAS, Constant, ASES, and DASH scores in Group B were 0.1 ± 0.3, 92.5 ± 3.9, 96.3 ± 3.6 and 2.9 ± 1.3 respectively. Clinical evaluation scales showed satisfactory results in both groups, and there were no statistically significant differences between the two groups at the same follow‐up time. Popeye sign was detected in one case of Group A (1.1%) and in one case of Group B (1.6%, P > 0.05).
Conclusion
Both tenotomy and subpectoral mini‐open tenodesis are effective for concomitant lesions of the LHBT in patients with reparable rotator cuff tears, and subpectoral mini‐open tenodesis of the LHBT does not provide any significant clinical or functional improvement than isolated tenotomy.
Keywords: Long head of the biceps tendon, Rotator cuff injuries, Shoulder, Tenodesis, Tenotomy
Introduction
Lesions of proximal long head of the biceps tendon (LHBT) are common causes of shoulder pain and may cause flexion dysfunction1, 2. The cause of these lesions can be inflammation, dislocation, and trauma3. It has been suggested that injuries of the LHBT are rarely isolated conditions but are commonly associated with rotator cuff tear4, 5, 6. If the biceps tendon shows a tear less than 25%, it can be treated conservatively with rest, activity modification, physical therapy, nonsteroidal anti‐inflammatory drugs, and steroid injection. However, if the biceps tendon lesion exceeds 25% of the diameter of the tendon, or there is subluxation and dislocation of the tendon, it is an indication for treatment, such as tenotomy or tenodesis7.
Isolated tenotomy and tenotomy/tenodesis are two techniques used to treat symptomatic patients with proximal biceps pathology. The LHBT is severed at the junction with upper glenoid labrum in the glenohumeral joint. Then the free end of LHBT can be unattended, or fixed either openly or arthroscopically. A tenotomy can be performed arthroscopically, which is technically simple with lesser injury, and the postoperative rehabilitation protocol is easy, and the recovery is quicker. However, it may result in the deformity of upper arm called Popeye sign, possibly followed by recurrent muscle spasm, fatigue, discomfort with active elbow flexion and supination, and biomechanical changes in LHBT4, 8, 9, 10. Some authors believe that tenodesis can avoid these complications. The advantages include better elbow flexion strength, less cramping or fatigue pain, and less anatomical changes. On the other hand, a tenodesis is more of a technically demanding procedure which requires a prolonged rehabilitation5, 11, 12. Both techniques can address the problems with LHBT.
Many studies have shown various results about tenotomy versus tenodesis for LHBT lesions, but controversy revolves around optimal strategy for these lesions13. Sentürk et al. conducted a cohort study involving 20 patients treated with tenotomy or arthroscopy‐assisted tenodesis, and no Popeye deformity was seen in both groups14. Shank et al. found no statistically significant forearm supination or elbow flexion strength differences between biceps tenotomy and arthroscopic LHBT tenodesis groups15. While Koh et al.3 and Cho et al.16 argued that the incidence of Popeye deformity tended to be higher in the tenotomy group compared with the tenodesis group, and it was even up to 17% in the study conducted by De Carli et al.17. Wittstein et al. also recorded that isolated tenotomy of LHBT decreased supination peak torque relative to the nonoperative side and tenodesis18. Patients involved in studies by Sentürk et al.14 and Shank et al.15 were without rotator cuff tears. The studies above3, 14, 15, 16, 17, 18 involved relatively small numbers of patients and with different tenodesis techniques, such as soft tissue tenodesis, arthroscopic biceps tenodesis conducted by biodegradable interference screw, and suture anchor tenodesis. Furthermore, two meta‐analyses conducted by Leroux et al. and Ge et al. reported different results19, 20.
This study reviewed the prospectively collected data about Chinese patients who underwent a LHBT procedure (tenotomy or subpectoral mini‐open tenodesis) concomitant with arthroscopic rotator cuff repair (RCR), so as to: (i) determine the results of clinical and radiological outcomes of these patients after surgery; (ii) to compare the validity between the two treatment methods by visual analog scale (VAS) for pain, Constant Score scale, American Shoulder and Elbow Surgeons (ASES) scores, and Disabilities of the Arm, Shoulder and Hand (DASH) scores; and (iii) and to further determine the optimal method. The hypotheses were: (i) both tenotomy and tenodesis would provide a higher clinical and functional outcome in patients with repairable rotator cuff tears; and (ii) and they are equally effective.
Materials and Methods
This study is retrospective, and the Ethics Review Committee of the Second Affiliated Hospital, Zhejiang University School of Medicine, approved the study.
Patient Selection
Patients undergoing arthroscopic repair of a full‐thickness rotator cuff tear between January 2010 and January 2017 were retrospectively identified in a prospectively collected (1, 3, 6, and 12 months and the latest follow‐up) database.
The inclusion criteria were: (i) full‐thickness but reparable rotator cuff tear; (ii) the presence of an associated LHBT lesion (including tears, tenosynovitis, subluxation on the medial rim of the bicipital groove, and superior labrum anterior and posterior (SLAP) lesions); (iii) underwent shoulder arthroscopy surgery between January 2010 and January 2017 in our institution; and (iv) were followed up for at least 1 year.
The exclusion criteria were: (i) irreparable massive rotator cuff tear; (ii) partial rotator cuff tear, subscapular tendon tear, glenohumeral arthritis; and (iii) prior shoulder surgery.
Given the criteria above, 173 patients were enrolled in this study. Of these patients, 18 were lost to follow‐up, and one underwent intra‐articular injection because of rotator cuff re‐tear. Finally, 154 patients were included in this study. Baseline demographic data was shown in Table 1.
Table 1.
Descriptive data at baseline for groups (n = 154)
| Indexes | Group A (n = 92) | Group B (n = 62) |
|---|---|---|
| Age [years, Mean (SD)] | 64.4(8.2) | 61.8(7.8) |
| Gender, male/female, No. | 38/54 | 33/29 |
| Left/right side, No. | 24/68 | 8/54 |
| Diabetes, yes/no | 18/74 | 13/49 |
| Smoking, yes/no | 13/49 | 14/48 |
| Popeye, +/− | 1/91 | 1/61 |
Operative Techniques
All operations were performed by the same surgeon and were performed with the patient in a beach chair position. Standard posterior and anterior portals were used for glenohumeral joint evaluation.
For LHBT lesions, funnel‐shaped tenotomy was performed by identification of the LHBT at its proximal origin of the posterosuperior labrum at the supraglenoid tubercle and resection as close as possible to the origin of the biceps tendon (Fig. 1A). For the subpectoral mini‐open tenodesis, a 2.5 cm straight incision below the medial pectoralis major muscle was performed with the shoulder in slight abduction and external rotation (Fig. 1B). Skin incision was made, and the superficial fascia was bluntly separated along the course of biceps tendon. The tendon was then pulled out from the groove with a clamp (Fig. 1C), and the length was measured and the position was marked (Fig. 1D). At 20 mm proximately to the inferior border of pectoralis major tendon, the cortex of the humerus was drilled with a 2 mm K‐wire. The 2.8 mm double‐loaded suture anchor (Twinfix, Smith & Nephew) was inserted. The tendon was fixed in a lasso‐loop manner. The proximal end was then resected (Fig. 1E,F). The wound was closed (Fig. 1G,H).
Figure 1.
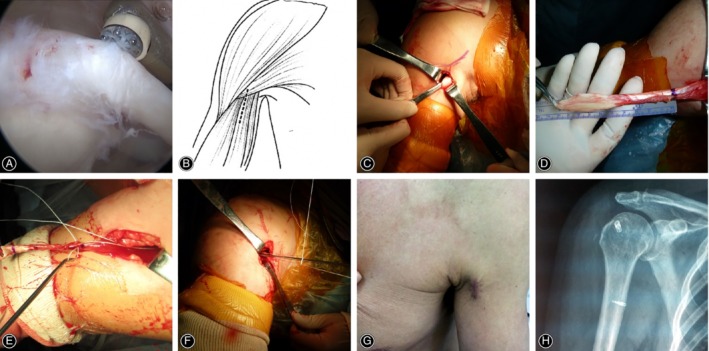
(A) Tenotomy of the LHBT. (B) Schematic diagram of the pectoralis major incision. (C) Exposed proximal end of the LHBT. (D) Measured length of the LHBT and identified mark. (E) Lasso Loop at musculotendinous junction with an anchor. (F) LHBT was fixed at inferior margin of the pectoralis major. (G) Surgical scars after operation. (H) Postoperative shoulder X‐ray shows anchor position.
Clinical Evaluations
VAS for pain, Constant score scale, ASES scores, and DASH scores were obtained preoperatively, at 1, 3, 6 months and 1 year postoperatively, and at the latest out‐patient clinic. Complications such as infection, nerve injury, fracture, and Popeye deformity were recorded at all follow‐up examinations.
VAS for Pain
VAS is the most commonly used questionnaire for quantification of pain. It is a continuous scale comprised of a horizontal or vertical line, usually 10 centimeters in length. For pain intensity, the scale is most commonly anchored by “no pain”(score of 0) and “pain as bad as it could be”(score of 10). Score of 0 is consider as no pain, 1–3 mild pain, 4–6 moderate pain, and 7–10 severe pain21.
Constant Score scale
Constant score is by far the most commonly used method for evaluation of rotator cuff tears. The 100‐point scoring scale takes into account both subjective and objective measurements: pain (0–15, 0 maximal pain and 15 no pain); activities of daily living (4 × (0–5) = 0–20, 0 worst and 5 best for each item); mobility (4 × (0–10) = 0–40, active, pain‐free range of elevation: +2 points per 30°, where 0 worst and 10 best for each item; position of hand: 0 worst to 10 best) and strength (0–25, 1 point per 0.5 kg, maximum 25 points). A total score of 0 is worst and 100 is best function22.
ASES Score
The ASES score was developed by the Society of the American Shoulder and Elbow Surgeons, including patient self‐assessment section (patient ASES [pASES]) and a section completed by the examiner (clinical ASES [cASES]). The cASES section includes physical examination and documentation of range of motion, strength, and instability, and demonstration of specific physical signs. No score is derived for this section. The pASES has 11 items that can be used to generate a score. These are divided into two areas: pain (one item) and function (10 items). The severity of pain is scored by VAS. The 10 items in the function area include activities of daily living. There are four categories for response options from 0 (unable to do) to 3 (not difficult). The final score is tabulated by multiplying (10‐VAS) by five (therefore total possible 50) and the cumulative activity score (maximum 30) by 5/3 (therefore, a total possible 50) for a total of 100. A total score 0 is worst and 100 is best function23.
DASH Score
The DASH questionnaire is a 30‐item questionnaire that assesses upper extremity‐related symptoms and measures functional status at the level of disability. The questionnaire consists of three sections: Symptoms; Sport and Music; and Work. The first section is composed of 30 items. The second and third sections are an optional module for Sport and Music, and four items for Work. Each item is scored with a 5‐point scale: 1, no difficulty/symptoms; 2, mild difficulty/symptoms; 3, moderate difficulty/symptoms; 4, severe difficulty/symptoms; 5, extreme difficulty/symptoms (unable to do). The result of each module is summed and transformed to obtain the DASH score ranging, for each section, from 0 (best function) to 100 (severe disability)24.
Statistical Analysis
The Statistical Package for the Social Sciences software package v. 21.0 (SPSS Inc., Chicago, Illinois, USA) was used for data analysis. Measured data were expressed as mean ± standard deviation. Categorical data and cosmetic deformity were analyzed using Pearson χ2 test. A paired t test was performed to assess the difference in preoperative and postoperative clinical scores of each group. An independent t test was used to compare clinical scores between the two groups. Significance was set at a level of 0.05 with 95% confidence intervals.
Results
General Outcome
One hundred and fifty‐four patients matched the inclusion/exclusion criteria. Group A consisted of 92 patients who underwent RCR along with a tenotomy of the LHBT; Group B consisted of 62 patients who underwent RCR along with subpectoral mini‐open tenodesis of the LHBT. The average age in Group A was 64.4 ± 8.2 years; the median follow‐up in Group A was 27 months (range, 12–96 months). The mean age in Group B was 61.8 ± 7.8 years; the median follow‐up was 42 months (range, 24–72 months).
Clinical Outcome
All incisions healed well, and no complications, such as infection, nerve injury, and fracture, occurred. Popeye deformity occurred in one patient in each group, but there was no pain and no significant decrease in elbow flexion strength in the two patients (Table 2, Fig. 2).
Table 2.
VAS, Constant, ASES and DASH scores of both groups
| Times | VAS | Constant | ASES | DASH | ||||
|---|---|---|---|---|---|---|---|---|
| Group A | Group B | Group A | Group B | Group A | Group B | Group A | Group B | |
| Pre | 5.8 (1.2) | 5.8 (1.1) | 17.9 (5.2) | 16.7 (5.3) | 37.5 (4.5) | 35.0 (6.0) | 72.1 (6.3) | 74.0 (7.3) |
| 1m | 3.5 (1.5) | 3.5 (1.3) | 23.8 (8.4) | 21.5 (7.2) | 44.8 (9.9) | 47.6 (8.7) | 69.8 (12.6) | 71.9 (9.2) |
| 2m | 1.9 (0.7) | 2.3 (1.1) | 41.1 (2.5) | 43.8 (9.7) | 62.7 (2.7) | 63.9 (9.7) | 54.2 (14.2) | 46.1 (16.2) |
| 3m | 1.0 (1.0) | 1.1 (1.3) | 70.1 (17.1) | 73.0 (13.1) | 83.5 (12.1) | 82.8 (10.1) | 23.7 (21.2) | 24.3 (17.0) |
| 6m | 0.7 (0.7) | 0.4 (0.6) | 87.5 (7.3) | 89.4 (4.3) | 93.6 (4.6) | 93.9 (4.1) | 4.8 (2.4) | 4.6 (1.8) |
| 1y | 0.4 (0.3) | 0.2 (0.1) | 89.8 (7.7) | 92.2 (4.0) | 95.5 (4.0) | 96.4 (3.7) | 4.7 (2.8) | 3.0 (1.4) |
| latest fo | 0.1 (0.2) | 0.1 (0.3) | 87.0 (12.8) | 92.5 (3.9) | 96.4 (4.3) | 96.3 (3.6) | 6.6 (4.8) | 2.9 (1.3) |
Data are expressed as mean (SD). pre, preoperatively; 1m, one month postoperatively; 2m, two months postoperatively; 3m, three months postoperatively; 6m, six months postoperatively; 1y, one year postoperatively; latest fo, latest follow‐up.
Figure 2.

A case of Popeye. A 72‐year‐old male, farmer, no obvious traumatic injury. The intraoperative exploration revealed that the long head of the biceps brachii of the right shoulder has been ruptured. The synovial membrane was removed by the planer and the stump was removed. Radiofrequency ablation stopped the bleeding and was not fixed. At present, there is no obvious pain in the right shoulder of the patient, and there is no significant decrease in the elbow flexion strength.
VAS for Pain
In Group A, the VAS score decreased from 5.8 ± 1.2 at baseline to 0.1 ± 0.2 at the latest follow‐up (P < 0.05). In Group B, it decreased from 5.8 ± 1.1 at baseline to 0.1 ± 0.3 at the latest follow‐up (P < 0.05). Both groups demonstrated significant improvement in VAS score since the first month follow‐up after surgery, but there was no significant difference between the two groups at the same follow‐up time (P > 0.05, Fig. 3).
Figure 3.
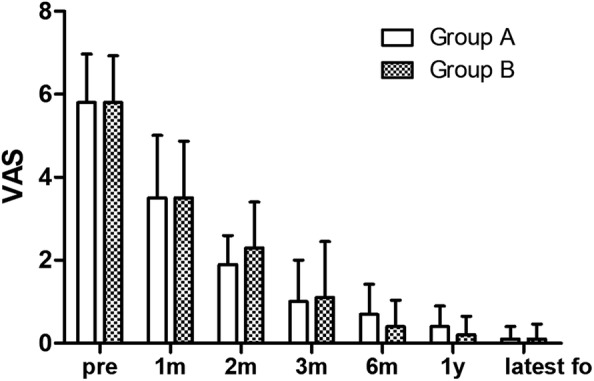
Preoperative and postoperative VAS scores. Both groups scored significantly lower than before surgery since the first month follow‐up after surgery, and there was no significant difference in VAS scores between the two groups at the same follow‐up phase.
Constant Score
The Constant score in Group A was 17.9 ± 5.2 before surgery and it increased significantly to 87.0 ± 12.8 at the latest follow‐up after surgery (P < 0.05), while in Group B this was 16.7 ± 5.3 before surgery and increased significantly to 92.5 ± 3.9 at the latest follow‐up after surgery (P < 0.05). Both groups demonstrated significant improvement in Constant score since the second month follow‐up after surgery, but there was no significant difference between the two groups at the same follow‐up period (P > 0.05, Fig. 4).
Figure 4.
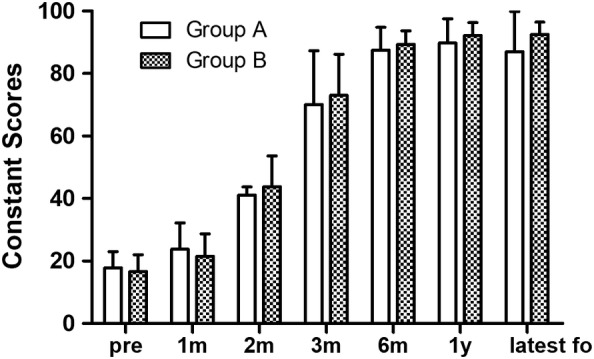
Preoperative and postoperative Constant scores. Both groups scored significantly more than before surgery since the second month follow‐up after surgery. There was no significant difference in the Constant score between the two groups at the same follow‐up period.
ASES Score
In Group A, the ASES score increased significantly from 37.5 ± 4.5 preoperatively to 96.4 ± 4.3 at the latest follow‐up (P < 0.05). In Group B, it also increased significantly from 35.0 ± 6.0 preoperatively to 96.3 ± 3.6 at the latest follow‐up (P < 0.05). Both groups demonstrated significant improvement in ASES score since the first month follow‐up after surgery, but there was no significant difference between the two groups at the same follow‐up phase (P > 0.05, Fig. 5).
Figure 5.
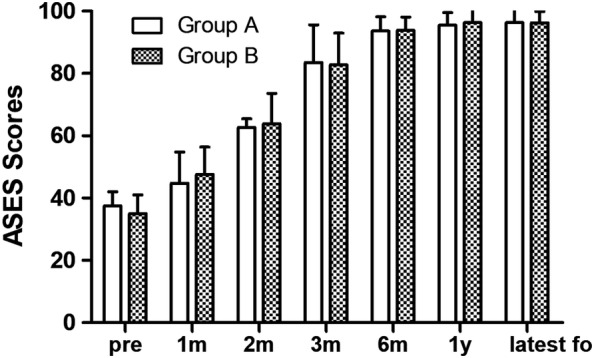
Preoperative and postoperative ASES scores. Both groups scored significantly more than before surgery since the first month follow‐up after surgery, and there was no significant difference in ASES scores between the two groups at the same follow‐up phase.
DASH Score
The DASH scores in groups A and B were 72.1 ± 6.3 and 74.0 ± 7.3 respectively before surgery, and these scores decreased significantly to 6.6 ± 4.8 and 2.9 ± 1.3 respectively at the latest follow‐up (P < 0.05 in each group). Both groups demonstrated significant improvement in DASH score since the second month follow‐up after surgery, but there was no significant difference between the two groups at the same follow‐up period (P > 0.05, Fig. 6).
Figure 6.
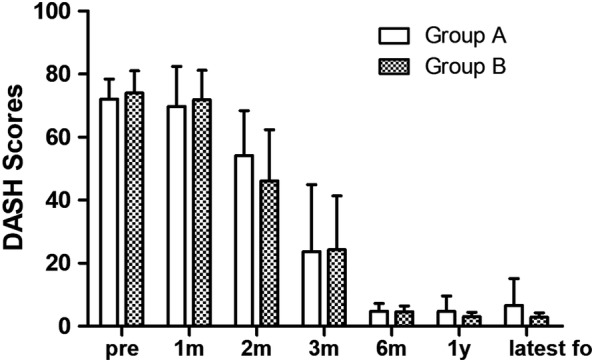
Preoperative and postoperative DASH scores. The scores of the two groups were significantly lower than those before surgery since the second month follow‐up after surgery. There was no significant difference in the DASH score between the two groups at the same follow‐up period.
Discussion
This study did not find any significant difference in clinical scores between the tenotomy group and the subpectoral mini‐open tenodesis group. Both techniques are commonly used in the clinical practice. A tenotomy is relatively simple and easy, but it is reported that cosmetic deformity and weakness of the biceps are likely to occur after surgery3, 20, while tenodesis requires longer operation time.
Gilcreest first described the tenodesis of LHBT in 1925. He fixed the LHBT on coracoid25. Originally, it was believed that the cause of biceps tendinitis or tendonitis was the instability of the biceps tendons, so the tendon was fixed in the intertubercular sulcus after tenotomy. Boileau et al. arthroscopically cut the LHBT at the supraglenoid tubercle and then fixed it in the intertubercular sulcus with an interface screw7. However, this may give rise to a new source of pain, sometimes lasting for 6 months to a year and postoperative stiffness may occur26. Various methods for tenodesis have been developed. The fixation sites include the osteochondral junction line, intertubercular sulcus, and inferior margin of the pectoralis major. It was later recognized that biceps tendon lesions, including wear and tendonitis, extend distally to the intertubercular sulcus, which incurs postoperative pain after proximal fixation27. It has been reported that intertubercular sulcus tenodesis may result in a re‐tear rate of at least 25%, and may result in post‐operative pain, stiffness, and loss of external rotation. In a retrospective study of 188 patients, arthroscopic proximal tenodesis resulted in a 36% revision rate, while the revision rate of intertubercular sulcus distal open tenodesis was only 3%28, 29, indicating that the inferior margin of pectoralis major tenodesis can effectively avoid re‐tear and inflammatory pain.
Maintaining the normal tension of the LHBT during subpectoral mini‐open tenodesis is important for the recovery of postoperative biceps tendon function. Since musculotendinous junction is located at approximately 2 cm proximal to the inferior margin of the pectoralis major30. The fixation of the musculotendinous junction should be done in order to maintain the tension.
In this study, the fixation of the musculotendinous junction was fixed with suture anchors, which were stable and easy to operate, and suitable for subpectoral mini‐open tenodesis. No complications were found in the follow‐up, such as loosening of anchors, injury to the musculocutaneous nerve, or persistent pain in the front of the upper arm. In addition to fixation with suture anchors, some scholars reported good results using interface screws to fix the proximal ends31.
This study showed that subpectoral mini‐open tenodesis of the LHBT could effectively relieve pain with mini‐incision, and fixation with suture anchors was simple and effective with few complications. The advantages of tenodesis include maintaining the length‐tension relationships of LHBT, maintaining postoperative elbow flexion and supination strength, and preventing Popeye deformity. Subpectoral mini‐open tenodesis is a minimally invasive surgical procedure for the treatment of biceps tendon lesions without the need for arthroscopic assistance. Subpectoral mini‐open tenodesis can avoid the postoperative pain caused by residual intertubercular sulcus lesions and the inflammatory pain caused by the proximal fixation.
There is no significant difference in the clinical effects between tenotomy and subpectoral mini‐open tenodesis. In clinical practice, it is believed that a tenotomy is more likely to cause Popeye cosmetic deformity, and the incidence is between 3% and 70%4, 7, 32, 33. However, the higher incidence of Popeye deformity in the tenotomy group did not significantly affect the clinical function scores during follow‐up7, 17.
This follow‐up did not reveal more Popeye deformity in the tenotomy group. There was one patient with Popeye deformity in each group, both of whom were patients with spontaneous ruptured LHBT. We believe that spontaneous rupture of LHBT sometimes occurs in the intertubercular sulcus, and it is more likely to retract after activity and results in Popeye deformity. However, the tenotomy of LHBT is at the starting point, and the retraction is usually not obvious. It is more likely to adhere to the rotator interval after postoperative immobilization for 1 month. Another important reason for the low rate of Popeye deformity in this study was the selection of patients. In order to obtain a better surgical vision and avoid postoperative inflammatory pain, we chose to perform arthroscopic subacromial tenodesis or subpectoral mini‐open tenodesis when we found that the ruptured LHBT retracted below acromion during surgery. If the massive rotator cuff tears cannot be repaired or can only be partially repaired, we chose to perform LHBT tenotomy and fix it under the pectoralis major, but never under the acromion, with the fear that a subacromial fixed ruptured end could become a new source of inflammatory pain.
Except for cosmetic issue, there was no obvious cramping, fatigue pain, or other complications in the tenotomy group in this study. DASH scores showed no significant difference between the two groups. Shank et al. found no significant difference in forearm rotation and elbow flexion strength between the tenotomy group and the arthroscopic tenodesis group, which was consistent with our clinical observations15. According to the report by Kelly et al., 40% of patients had biceps spasm, fatigue, and discomfort with active elbow flexion and supination34. However, the above situations often occurred in patients under the age of 60 years. Most of the patients in our study were older and had lower requirements for postoperative strength. Simultaneously, we requested that patients should use slings or braces for 4–6 weeks after RCR surgery to avoid active shoulder joint activity, and to some extent reduce the retraction of LHBT, and promote the adhesion of the LHBT stump.
This study is not a randomized, controlled study, so it is difficult to draw a definitive conclusion. Meanwhile, there were limited cases and a significant difference between the two groups in gender and the history of diabetes.
Conclusion
For the treatment of concomitant lesions of the LHBT in patients with reparable rotator cuff tears, both isolated tenotomy and subpectoral mini‐open tenodesis showed good clinical outcomes with low incidence of complications, such as Popeye deformity, cramping, or fatigue pain. And subpectoral mini‐open tenodesis of the LHBT does not provide any significant clinical or functional improvement over isolated tenotomy.
Acknowledgments
We wish to thank all of those who agreed to be interviewed for this research.
Disclosure: The authors report no actual or potential conflict of interest in relation to this article.
Contributor Information
Jing‐hua Fang, Email: raginmund@zju.edu.cn.
Xue‐song Dai, Email: daixshz@zju.edu.cn.
References
- 1. Slenker NR, Lawson K, Ciccotti MG, Dodson CC, Cohen SB. Biceps tenotomy versus tenodesis: clinical outcomes. Art Ther, 2012, 28: 576–582. [DOI] [PubMed] [Google Scholar]
- 2. Hsu AR, Ghodadra NS, Provencher MT, Lewis PB, Bach BR. Biceps tenotomy versus tenodesis: a review of clinical outcomes and biomechanical results. J Shoulder Elbow Surg, 2011, 20: 326–332. [DOI] [PubMed] [Google Scholar]
- 3. Koh KH, Ahn JH, Kim SM, Yoo JC. Treatment of biceps tendon lesions in the setting of rotator cuff tears: prospective cohort study of Tenotomy versus Tenodesis. Am J Sports Med, 2010, 38: 1584–1590. [DOI] [PubMed] [Google Scholar]
- 4. Walch G, Edwards TB, Boulahia A, Nové‐Josserand L, Neyton L, Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg, 2005, 14: 238–246. [DOI] [PubMed] [Google Scholar]
- 5. Checchia SL, Doneux PS, Miyazaki AN, et al Biceps tenodesis associated with arthroscopic repair of rotator cuff tears. J Shoulder Elbow Surg, 2005, 14: 138–144. [DOI] [PubMed] [Google Scholar]
- 6. Nho SJ, Shindle MK, Sherman SL, Freedman KB, Lyman S, MacGillivray JD. Systematic review of arthroscopic rotator cuff repair and mini‐open rotator cuff repair. J Bone Joint Surg Am, 2007, 89: 127. [DOI] [PubMed] [Google Scholar]
- 7. Ball C, Galatz LM, Yamaguchi K. Tenodesis or Tenotomy of the biceps tendon: why and when to do it. Tech Shoulder Elbow Surg, 2001, 2: 140–152. [Google Scholar]
- 8. Boileau P, Baqué F, Valerio L, Ahrens P, Chuinard C, Trojani C. Isolated arthroscopic biceps Tenotomy or Tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am, 2007, 89: 747–757. [DOI] [PubMed] [Google Scholar]
- 9. Elser F, Braun S, Dewing CB, Giphart JE, Millett PJ. Anatomy, function, injuries, and treatment of the long head of the biceps Brachii tendon. Art Ther, 2011, 27: 581–592. [DOI] [PubMed] [Google Scholar]
- 10. Nassos JT, Chudik SC. Arthroscopic rotator cuff repair with biceps tendon augmentation. Am J Orthop (Belle Mead NJ), 2009, 38: 279–281. [PubMed] [Google Scholar]
- 11. Berlemann U, Bayley I. Tenodesis of the long head of biceps brachii in the painful shoulder: improving results in the long term. J Shoulder Elbow Surg, 1995, 4: 429–435. [DOI] [PubMed] [Google Scholar]
- 12. Boileau P, Krishnan SG, Coste JS, Walch G. Arthroscopic biceps tenodesis: a new technique using bioabsorbable interference screw fixation. Tech Shoulder Elbow Surg, 2002, 18: 1002–1012. [DOI] [PubMed] [Google Scholar]
- 13. Miller T, Jones G, Moon Shoulder Group . Arthroscopic evaluation and treatment of biceps brachii long head tendon injuries: a survey of the MOON shoulder group. Int J Shoulder Surg, 2011, 5: 68–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sentürk I, Ozalay M, Akpınar S, Leblebici B, Cınar BM, Tuncay C. Clinical and isokinetic comparison between tenotomy and tenodesis in biceps pathologies. Acta Orthop Traumatol Turc, 2011, 45: 41–46. [DOI] [PubMed] [Google Scholar]
- 15. Shank JR, Singleton SB, Braun S, et al A comparison of forearm supination and elbow flexion strength in patients with long head of the biceps tenotomy or tenodesis. Art Ther, 2011, 27: 9–16. [DOI] [PubMed] [Google Scholar]
- 16. Cho NS, Cha SW, Rhee YG. Funnel tenotomy versus intracuff tenodesis for lesions of the long head of the biceps tendon associated with rotator cuff tears. Am J Sports Med, 2014, 42: 1161–1168. [DOI] [PubMed] [Google Scholar]
- 17. De Carli A, Vadalà A, Zanzotto E, et al Reparable rotator cuff tears with concomitant long‐head biceps lesions: tenotomy or tenotomy/tenodesis?. Knee Surg Sports Traumatol Arthrosc, 2012, 20: 2553–2558. [DOI] [PubMed] [Google Scholar]
- 18. Wittstein JR, Queen R, Abbey A, Toth A, Moorman CT 3rd. Isokinetic strength, endurance, and subjective outcomes after biceps tenotomy versus tenodesis: a postoperative study. Am J Sports Med, 2011, 39: 857–865. [DOI] [PubMed] [Google Scholar]
- 19. Leroux T, Chahal J, Wasserstein D, Verma NN, Romeo AA. A systematic review and meta‐analysis comparing clinical outcomes after concurrent rotator cuff repair and long head biceps Tenodesis or Tenotomy. Sports Health, 2015, 7: 303–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ge H, Zhang Q, Sun Y, Li J, Sun L, Cheng B. Tenotomy or tenodesis for the long head of biceps lesions in shoulders: a systematic review and meta‐analysis. PLoS One, 2015, 10: e0121286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: visual analog scale for pain (VAS pain), numeric rating scale for pain (NRS pain), McGill pain questionnaire (MPQ), short‐form McGill pain questionnaire (SF‐MPQ), chronic pain grade scale (CPGS), short Form‐36 bodily pain scale (SF‐36 BPS), and measure of intermittent and Constant osteoarthritis pain (ICOAP). Arthritis Care Res (Hoboken), 2011, 63: S240–S252. [DOI] [PubMed] [Google Scholar]
- 22. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res, 1987, 214: 160–164. [PubMed] [Google Scholar]
- 23. Richards RR, An KN, Bigliani LU, et al A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg, 1994, 3: 347–352. [DOI] [PubMed] [Google Scholar]
- 24. Hudak PL, Amadio PC, Bombardier C, et al Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder, and head). Am J Ind Med, 1996, 29: 602–608. [DOI] [PubMed] [Google Scholar]
- 25. Gilcreest EL. Rupture of muscles and tendons: particularly subcutaneous rupture of the biceps flexor cubiti. JAMA, 1925, 84: 1819–1822. [Google Scholar]
- 26. Werner BC, Evans CL, Holzgrefe RE, et al Arthroscopic suprapectoral and open subpectoral biceps tenodesis: a comparison of minimum 2‐year clinical outcomes. Am J Sports Med, 2014, 42: 2583–2590. [DOI] [PubMed] [Google Scholar]
- 27. Moon SC, Cho NS, Rhee YG. Analysis of “hidden lesions” of the extra‐articular biceps after subpectoral biceps Tenodesis: the subpectoral portion as the optimal Tenodesis site. Am J Sports Med, 2015, 43: 63–68. [DOI] [PubMed] [Google Scholar]
- 28. Sanders B, Lavery K, Pennington S, Warner JJ. Biceps tendon tenodesis: success with proximal versus distal fixation (SS‐16). Arthroscopy, 2008, 24: e9. [Google Scholar]
- 29. Sanders B, Lavery KP, Pennington S, Warner JJ. Clinical success of biceps tenodesis with and without release of the transverse humeral ligament. J Shoulder Elbow Surg, 2012, 21: 66–71. [DOI] [PubMed] [Google Scholar]
- 30. Denard PJ, Dai X, Hanypsiak BT, Burkhart SS. Anatomy of the biceps tendon: implications for restoring physiological length‐tension relation during biceps Tenodesis with interference screw fixation. Art Ther, 2012, 28: 1352–1358. [DOI] [PubMed] [Google Scholar]
- 31. Millett PJ, Sanders B, Gobezie R, Braun S, Warner JJ. Interference screw vs. suture anchor fixation for open subpectoral biceps tenodesis: does it matter?. BMC Musculoskelet Disord, 2008, 9: 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gill TJ, McIrvin E, Mair SD, Hawkins RJ. Results of biceps tenotomy for treatment of pathology of the long head of the biceps brachii. J Shoulder Elbow Surg, 2001, 10: 247–249. [DOI] [PubMed] [Google Scholar]
- 33. Patzer T, Kircher J, Lichtenberg S, Sauter M, Magosch P, Habermeyer P. Is there an association between SLAP lesions and biceps pulley lesions?. Art Ther, 2011, 27: 611–618. [DOI] [PubMed] [Google Scholar]
- 34. Kelly AM, Drakos MC, Fealy S, Taylor SA, O'brien SJ. Arthroscopic release of the long head of the biceps tendon: functional outcome and clinical results. Am J Sports Med, 2005, 33: 208–213. [DOI] [PubMed] [Google Scholar]


