Abstract
Background
Person-centered care is widely recognized as a gold standard and is based on a supportive psychosocial climate for both residents and staff in nursing homes. Residents and staff may have different perspectives as to whether the climate in which they interact is person-centered, perhaps due to their different expectations of the nursing home environment and the provision of care services. The aim of this study was to explore and compare resident and staff perspectives of person-centered climate in aged care nursing homes.
Methods
This is a descriptive cross-sectional study using a cluster random sampling method. The study collected data in 2016 from residents (n = 251) and nursing staff (n = 249) in 23 nursing homes using a Person-centered Climate Questionnaire-Patient version and Person-centered Climate-Staff version. T-tests for independent-samples were used to compare scores ranked by nursing staff and residents.
Results
The mean scores of ‘A climate of safety’ subscale and ‘A climate of everydayness’ subscale rated by residents were significantly lower than those rated by nursing staff. The mean scores of ‘A climate of hospitality’ rated by residents were very low among the three subscales, an indicator of the need to improve a more home-like environment for residents. Residents in larger size nursing homes showed a higher score of person-centered climate compared with their counterparts in small size nursing homes.
Conclusions
This study reveals that the perspectives and perceptions of person-centered climate differ between residents and nursing staff. Therefore, both resident and staff perspectives should be taken into account in attempting to improve person-centered climate for better care outcomes.
Keywords: Aged care, Nursing homes, Nursing staff, Older people, Person-centered care
Background
Person-centered care is widely recognized as a gold standard and needs to be embedded into policies, regulations and quality improvement in aged care in a global context [1, 2]. This care approach emphasizes that each person is unique and worthy of respect regardless of disability or illness [3]. Person-centered care standards enable staff in aged care to achieve high-quality care for residents and improve resident satisfaction with care services [4–6]. This care approach is conditioned by a positive psychosocial environment in aged care homes where both residents and staff have a sense of being valued and receiving organizational support to achieve person-centered care [7–9]. However, research evidence in this field is mainly from high-income countries where the aged care system is better developed compared to the system in lower- and middle-income countries (LMICs) [10, 11]. Research evidence in person-centered care from LMICs is much needed considering that the most older people live in LMICs and the disparities of quality of aged care between in a global context [12]. Additionally, studies that compare resident and nursing staff perspectives of person-centered climate are scarce. This study addresses the gaps in research by engaging both residents and staff in assessing person-centered climate, from the perspective of a lower-middle income country (LMIC).
Unlike other LMICs, China shows the highest rate of population aging [13]. In 2015, the number of people aged 65 and over reached 144 million, which comprised 10.5% of the total population [14]. It is estimated that the proportion of older people will increase to 23% in 2050 [14]. Older Chinese are traditionally cared for by their family members due to the influence of filial piety [15, 16]. However, the number of family caregivers has decreased because of internal migration of the labor force, the tendency towards a small family size, and the “empty-nest families” [17, 18]. Consequently the growth of nursing homes has become significant in China in recent years [19]. It is expected that nursing homes will play a crucial role in the next few decades to meet the demand for caring for older people with complex care needs [13].
Nursing homes in China share many similarities with other LMICs where policies, resources and regulations are largely underdeveloped to govern quality care [20]. Although great efforts have been made to improve nursing home care by the Central Government in China, the workforce and the care environment to support high-quality care have become issues of concern [20–22]. Most staff employed in nursing homes are untrained workers with low education levels and the majority are migrants from rural areas with little experience in aged care [23]. It is predicted that the number of professional care workers in nursing homes in China will be 6.91 million in 2030 and 32.62 million in 2050 [19]. Research evidence on consumers’ expectations of person-centered high-quality care is much needed so as to inform education and training for staff.
High-quality care for residents in nursing homes has a core component of person-centered care [8, 24]. The concept of “person-centeredness” was first mentioned by Rogers [25] and was first applied to aged care by Kitwood (1997). Person-centered care refers to maintaining one’s personhood despite disabilities or illness, endeavoring to adopt the residents’ values and lifestyles, recognizing their life experiences and relationships, and creating a positive psychosocial environment for them to achieve the highest level of quality of life [1, 26, 27].
It has been strongly argued that person-centered care must be supported by a positive psychosocial environment in nursing homes [28]. Such an environment has the following characteristics: (i) valuing residents as individuals with unique life experiences; (ii) preserving their autonomy and dignity; (iii) encouraging them or their family members to participate in decision making involving their care, and (iv) organizational support for staff via education, adequate resources and staffing levels [29, 30]. Residents and staff may have different and sometimes competing views about what constitutes an ideal psychosocial environment due to their different interests and perspectives. For example, residents expect the nursing homes to be their own homes where they can exercise their autonomy to control the environment and the care activities to meet their care needs [31, 32]. Staff on the other hand, usually perceive the nursing home as a workplace where they can exercise their right to create a safe workplace, have a reasonable workload and in return receive a decent income [33, 34].
The concept of positive psycho-social environment was built into the Person-centered Climate questionnaire in a resident version and a staff version [8]. The Person-centered Climate Questionnaire-Patient version (PCQ-P) was originally developed in a hospital setting, but was validated and tested in nursing home settings [7, 35]. This scale comprises three subscales: a climate of safety, a climate of everydayness and a climate of hospitality [35]. A climate of safety focuses on a safe place for residents to be cared for while a climate of everydayness emphasizes an environment that enables residents to have daily positive experiences. A climate of hospitality represents residents’ expectations of being welcomed in a caring environment. The Staff version of PCQ shares similar subscales, namely a climate of safety, a climate of everydayness and a climate of community [26]. A climate of safety points out a safe workplace for staff while a climate of everydayness refers to staff expectations of an environment that enables them to have daily positive experiences. A climate of community represents staff expectations of a caring and welcome environment for residents while a positive psychosocial environment needs to be developed by both residents and staff together [8, 26]. Engaging both residents and staff in assessing the person-centered climate is the first step towards achieving an ideal climate expected by both residents and staff to support person-centered care.
Methods
Aims
The aim of the study was to explore and compare resident and staff perspectives of person-centered climate to facilitate both residents and staff engaged in person-centered care in nursing homes.
Design
A cross-sectional survey was employed in the study.
Participants
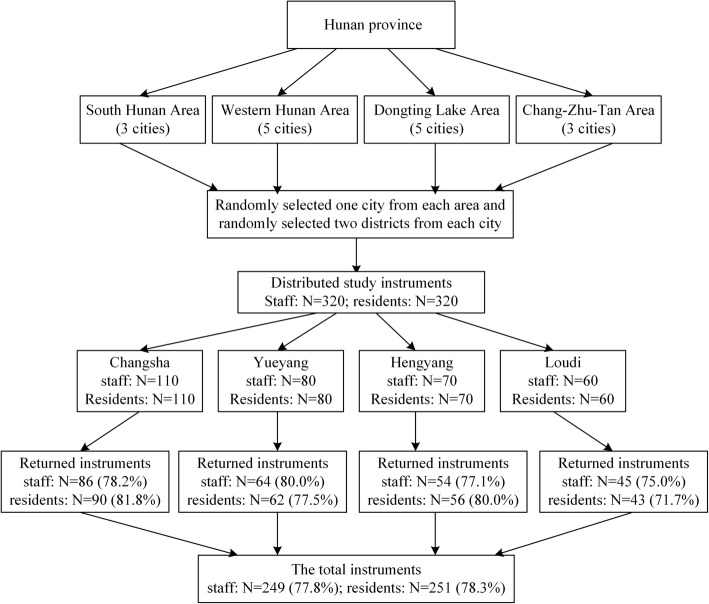
Participants recruited in the study were from nursing homes in Hunan Province, China where in 2015, the population in the province aged 60 and over was 11.64 million, and there were 326 nursing homes with a total of 275,000 beds [36]. A cluster random sampling method was used to recruit residents and staff from nursing homes in four geographic areas of the Province. The researchers searched the website of the Department of Civil Affairs of Hunan Province to identify a name list of all nursing homes in the province. SPSS version 23.0 was used to randomly select one city from each geographic area and then select two districts from the selected cities. The total number of nursing homes in these selected districts was 32. All nursing homes from these selected districts were invited to participate in the study via a letter of invitation sent to the facility manager.
In total 23 nursing homes, or 72% of the total numbers in the selected districts agreed to participate in the study, evidenced by returned letters and information about the total number of nursing staff and residents from nursing home managers. In total, there were 320 nursing staff who cared for approximately 2210 residents in these nursing homes. The size of nursing homes varied widely, ranging from those accommodating 36 residents to as many as 380 residents. The number of staff employed in these nursing homes ranged from 8 to 110. Regarding the facility ownership, there were 8 state-owned nursing homes and 15 not-for-profit privately-owned nursing homes.
All nursing staff, including registered nurses and personal care assistants, in the nursing homes were invited to participate to the study. Inclusion criteria for nursing staff were as follows: (1) having more than 1 month’s work experience in the nursing home; (2) ability to understand and complete the survey; (3) willingness to participate. Nursing staff who were on vacation, were not on duty and or who had engaged in advanced studies were excluded.
Residents were randomly selected to achieve a 1:1 resident to staff ratio if they met the following inclusion criteria: (1) aged 60 or over; (2) having lived in the nursing home for at least 1 month; (3) able to understand and respond to the questionnaires; and (4) willing to participate. The sample frame and numbers of participants from each city are shown in Fig. 1.
Fig. 1.
The sample frame
Data collection
Data were collected from self-report questionnaires by staff and residents. A letter of invitation with the survey questionnaire was distributed to each potential participant in the nursing homes via their internal mail systems. Participants were assured that they could choose or refuse to participate in the survey without any consequences. Participants were provided with pre-addressed, prepaid and sealable envelopes to return their survey to the researcher directly. Residents were informed in the letter that researcher assistants would be available in their nursing homes and would visit them to help explain any questions they might have about the survey. All participants were reassured of strict confidentiality of the information they provided in the survey. This study was conducted from June 2016 to August 2016.
Survey instruments
Person-centered climate questionnaire-patient
Resident perceived person-centered climate was assessed by the Person-centred Climate Questionnaire-Patient version (PCQ-P) [35]. The English version of the PCQ-P was validated in long-term care [7]. The scale is a 17-item scale with three dimensions: safety (10 items), everydayness (4 items), and hospitality or a caring and welcome place for residents (3 items). Responses ranged from 1 “completely disagree” to 6 “completely agree” with higher scores indicating a more person-centered climate.
The person-centred climate questionnaire-staff
The Person-centred Climate Questionnaire-Staff version (PCQ-S) [26] was used to measure staff perceived person-centered climate in their workplace. The PCQ-S contains 14 items and consists of three subscales: safety (5 items), everydayness (5 items) and community or a caring and welcome place for residents (4 items). A 6-point rating system is used and higher scores indicate a more person-centered climate.
Although the descriptive items of the three subscales in PCQ-P and PCQ-S slightly differ, they share the core concepts that the climate should be: (i) a safe place for residents and staff to interact with; (ii) a place for these two groups to have daily positive experiences; and (iii) a caring and welcome place for residents who are cared for in the environment. Additionally, PCQ-P and PCQ-S use the same 6-Likert scale scoring system rated from 1 to 6 with higher scores indicating more person-centered climate. Therefore, the similar factor (concept) structures and scoring systems of the PCQ-P and PCQ-S support the comparison of the three subscales from the two participant groups.
Physical self-maintenance scale
The Physical Self-Maintenance Scale (PSMS) questionnaire was used to measure the activities of daily living of residents [37]. Six basic functional abilities were assessed: toilet, feeding, dressing, grooming, physical ambulation and bathing. All items were rated by discussion between the resident and his/her caregiver on a 4-point rating scale from 1 (no impairment) to 4 (severe impairment). A total score of 6 is defined as activities of daily living intact and scores higher than 6 represent activities of daily living impairment. The PSMS has been widely used in China, and the PSMS for Chinese version has been shown to have satisfactory reliability and validity [38, 39].
Reliability and validity
As the Person-centered Climate Questionnaire-Staff version and Person-centered Climate Questionnaire-Patient version were originally developed in Swedish and no Chinese versions were available. The principal chief investigator contacted the original author of the scales and gained permission to translate and validate the two scales. A forward-backward translation method was used to translate the scales, and psychometric properties were evaluated. First, the research group translated the English versions into Chinese. Second, a professionally qualified translator carried out the back translation of the Chinese versions into English. Third, a thorough comparison between the original versions, the translated Chinese versions and the back-translated English versions was conducted to examine any discrepancies. Construct validity was estimated using a principal component analysis with varimax orthogonal rotation. The internal consistency reliability was evaluated using test-retest reliability and Cronbach’s α coefficient was calculated.
PCQ-P and PCQ-S had the same factor structure with original scales and most of the original items loaded on the same factor. The Chinese PCQ-S consists of 14 items and includes three factors: Factor 1-a climate of safety (3 items), Factor 2-a climate of everydayness (5 items) and Factor 3-a climate of community (6 items). The total Cronbach’s α coeffient for the Chinese PCQ-S was 0.91 and each subscale showed acceptable Cronbach’s α coefficient. The factor analysis result of the Chinese PCQ-S was summarized in Table 1. The Chinese PCQ-P consists of 17 items with three factors: Factor 1-a climate of safety (6 items), Factor 2-a climate of everydayness (7 items) and Factor 3-a climate of hospitality (4 items). The total Cronbach’s α coefficient for the Chinese PCQ-P was 0.93 and each subscale showed acceptable Cronbach’s α coefficient. The factor analysis result of the Chinese PCQ-S was presented in Table 2.
Table 1.
Factor loading matrix of each item in Chinese PCQ-S a(n = 249)
| Items | Factor-1 | Factor-2 | Factor-3 |
|---|---|---|---|
| Safety | Everydayness | Community | |
| S12 A place where it is easy for the residents to receive visitors | 0.830 | ||
| S11 A place where it is easy for the residents to keep in contact with their loved ones | 0.830 | ||
| S13 A place where it is easy for the residents to talk to the staff | 0.797 | ||
| S14 A place where the residents have someone to talk to if they so wish | 0.637 | ||
| S4 A place where the residents are in safe hands | 0.482 | ||
| S5 A place where the staff use a language that the residents can understand | 0.447 | ||
| S7 A place where there is something nice to look at | 0.818 | ||
| S8 A place where it is quiet and peaceful | 0.770 | ||
| S9 A place where it is possible to get unpleasant thoughts out of your head | 0.720 | ||
| S6 A place which feels homely even though it is in an institution | 0.666 | ||
| S10 A place which is neat and clean | 0.613 | ||
| S1 where I feel welcome | 0.822 | ||
| S2 where I feel acknowledged as a person | 0.804 | ||
| S3 where I feel I can be myself | 0.717 | ||
| Percent total variance explained(%)b | 16.626 | 22.481 | 24.685 |
aPCQ-S Person-centred Climate Questionnaire-Staff version
bBartlett’s test statistic was significant (χ2(91) = 2032.70, p < .05). Kaiser-Meyer-Olkin’s (KMO) indicated sampling adequacy appropriate for factor analysis (KMO = .90)
Table 2.
Factor loading matrix of each item in Chinese PCQ-P a(n = 251)
| Items | Factor-1 | Factor-2 | Factor-3 |
|---|---|---|---|
| Safety | Everydayness | Hospitality | |
| P9 A place which is neat and clean | 0.741 | ||
| P14 A place where people talk about ordinary things, not just illness | 0.737 | ||
| P4 A place where I feel welcome | 0.684 | ||
| P11 A place where there is something nice to look at | 0.648 | ||
| P3 A place where I feel in safe hands | 0.648 | ||
| P13 A place where it is possible to get unpleasant thought out of your head | 0.595 | ||
| P8 A place where the staff use language I can understand | 0.570 | ||
| P15 A place where the staff make extra efforts on my behalf | 0.885 | ||
| P17 A place where I can get “that little bit extra” | 0.875 | ||
| P12 A place where which feels homely even though I am in an institution | 0.662 | ||
| P16 A place where I can make choices, for example what to wear | 0.532 | ||
| P6 A place where the staff take notice of what I say | 0.811 | ||
| P5 A place where it is easy to talk to the staff | 0.777 | ||
| P7 A place where the staff come quickly when I need help | 0.664 | ||
| P1 A place where the staff is knowledgeable | 0.565 | ||
| P2 A place where I rely on receiving the best care | 0.548 | ||
| P10 A place where the staff have time for the residents | 0.439 | ||
| Percent total variance explained (%)b | 5.968 | 48.474 | 8.130 |
aPCQ-P Person-centred Climate Questionnaire-Patient version
bBartlett’s test statistic was significant (χ2(136) = 2503.64, p < .05). Kaiser-Meyer-Olkin’s (KMO) indicated sampling adequacy appropriate for factor analysis (KMO = .93)
Ethical considerations
The research was approved by the Nursing and Behavioral Medicine Institutional Review Boards, Xiangya School of Nursing, Central South University (Ref No. 2017035). Participating nursing homes accepted the ethical approval. An information pack was provided for participants that explained the purpose of the study, participants’ right to refuse to participate in the study, the benefits and potential risks, and strategies used to ensure the confidentiality of information that participants provided. An information session was also provided for staff and residents to ask questions they might have in relation to their participation in the study. The survey utilized anonymity and participants were not asked to provide their identity. Each nursing home site was assigned a code for data comparison purposes. Returning a completed survey to the researchers was regarded as evidence of participants’ consent to participate in the survey.
Data analysis
SPSS version 23.0 was used for data analyses. Descriptive statistics were used to summarize data. Subscale means, standard deviations (SD), 95% confidence interval of subscale means, percentages and frequencies were calculated for items and scales. Internal consistency for the PCQ-P and PCQ-S was estimated by calculating Cronbach’s α coefficents, and factor structure was evaluated by exploratory factor analysis. T-tests for independent-samples were used to compare scores ranked by nursing staff and residents on the three sub-scales of person-centered climate. Values of p < 0.05 was considered significant statistics for all analysis.
Results
The demographic characteristics of staff were presented in Table 3. Staff had an average age of 47.8 years old and had an average of a 2.1-year experience in nursing home care. The majority of staff were female (90.8%), married (79.1%) and had junior middle school education or below (62.3%). Most of the staff participants were personal care assistants (79.5%) and Registered Nurses made up 20.5% of staff participants.
Table 3.
Characteristics of staff participants (n = 249)
| Variable | n (%) | Mean (SD) |
|---|---|---|
| Gender | ||
| Male | 23 (9.2) | |
| Female | 226 (90.8) | |
| Age (years) | 47.8 (11.9) | |
| Marital status | ||
| Unmarried | 31 (12.4%) | |
| Married | 197 (79.1%) | |
| Divorced or widowed | 21 (8.5%) | |
| Education | ||
| Primary school or below | 39 (15.7%) | |
| Junior middle school | 116 (46.6%) | |
| Senior high school | 78 (31.3%) | |
| Bachelor or master | 16 (6.4%) | |
| Years of experience in facility | 2.1 (1.9) | |
| Qualifications | ||
| Registered nurses | 51 (20.5%) | |
| Nurses’ assistants | 198 (79.5%) | |
| Attending training activities in aged care | ||
| Yes | 226 (90.8) | |
| No | 23 (9.2) | |
The demographic characteristics of residents were summarized in Table 4. Resident participants had a mean age of 82.3 years old and the mean length of stay in the nursing homes was 14 months. Most residents were female (59.8%) and more than half of residents (50.2%) had activities of daily living impairment. The majority of residents (63.8%) also had two or above chronic diseases.
Table 4.
Characteristics of resident participants (n = 251)
| Variable | n (%) | Mean (SD) |
|---|---|---|
| Gender | ||
| Male | 101 (40.2%) | |
| Female | 150 (59.8%) | |
| Age (years) | 82.3 (10.4) | |
| Marital status | ||
| Unmarried | 9 (3.6%) | |
| Married | 75 (29.9%) | |
| Divorced or widowed | 167 (66.5%) | |
| Education | ||
| Primary school | 83 (33.1%) | |
| Junior middle school | 71 (28.3%) | |
| Senior high school | 67 (26.7%) | |
| Bachelor or master | 30 (12.0%) | |
| Length of stay in facility, months | 14 (7.9) | |
| BADL a | 8.81 (4.10) | |
| impaired | 126 (50.2%) | |
| intact | 125 (49.8%) | |
| The number of chronic diseases b | ||
| None | 29 (11.6%) | |
| One | 62 (24.7%) | |
| Two | 84 (33.5%) | |
| Three or above | 76 (30.3%) | |
Perceived person-centered climate
In the PCQ-P, the mean total score was 59.7 (SD 11.5). The subscale of a climate of hospitality was scored the lowest (mean 2.72, SD 0.78), followed by a climate of safety subscale (mean 3.25, SD 0.76) and a climate of everydayness (mean 4.19, SD 0.74). The result revealed that residents had a relatively low level of sense of being welcomed in the care home.
In PCQ-S, the mean total score was 52.1(SD 9.4). The subscale that showed the lowest mean-score was the climate of everydayness (mean 4.49, SD 0.86), followed by a climate of safety (mean 4.55, SD 0.82) and a climate of community (mean 5.01, SD 0.71). The result indicated that staff had some level of agreement that the environment would enable them to have positive experiences and a feeling of safe workplace. Staff indicated strongly agreed that the nursing home was a caring community for residents.
Comparisons of mean subscale scores of PCQ-P and PCQ-S
Comparison of mean subscale scores of PCQ-P and PCQ-S revealed that staff perceived significantly higher mean scores for subscales of (i) safety [Mean difference 1.30 (95% CI 1.16–1.44), p < .001], (ii) everydayness [Mean difference 0.30 (95% CI 0.16–0.45), p < .001] and (iii) a caring and welcome climate [Mean difference 2.28 (95% CI 2.15–2.41), p < .001] (see Table 5).
Table 5.
Comparisons of subscale scores between staff and residents
| Subscales | Staff (n = 249) | Residents (n = 251) | Mean differences | Group comparison |
|---|---|---|---|---|
| Mean (SD a) | Mean (SD) | Mean (95% CI b) | p value | |
| Safety | 4.55 (0.82) | 3.25 (0.76) | 1.30 (1.16, 1.44) | p < 0.001 |
| Everydayness | 4.49 (0.86) | 4.19 (0.74) | 0.30 (0.16, 0.45) | p < 0.001 |
| Community/Hospitality | 5.01 (0.71) | 2.72 (0.78) | 2.28 (2.15, 2.41) | p < 0.001 |
aSD standard deviation
bCI Confidence interval
Differences based on the size of nursing homes
When comparing smaller nursing homes (≤60 residents) with larger nursing homes (> 60 residents), there were significant differences in the subscales ‘a climate of safety’ (p = .048) and ‘a climate of everydayness’ (p < .001) for residents. Residents in larger nursing homes perceived better climate of person-centeredness, a better climate of safety and everydayness than those in smaller facilities (see Table 6). There were no significant differences on the ratings of nursing staff between the large and smaller nursing homes (p > 0.05).
Table 6.
Impacts of facility size on participants’ person-centeredness
| Subscales | Larger facilities (> 60 residents) | Smaller facilities (< 60 residents) | Mean differences | Group comparison |
|---|---|---|---|---|
| Mean (SD) | Mean (SD a) | Mean (95% CI b) | p value | |
| Safety- PCQ-S c | 4.59 (0.85) | 4.38 (0.65) | 0.22 (0.00,0.44) | p = 0.053 |
| Everydayness- PCQ-S | 4.51 (0.85) | 4.40 (0.93) | 0.11(−0.17,0.38) | p = 0.437 |
| Community- PCQ-S | 5.00 (0.70) | 5.04 (0.77) | −0.04(−0.27,0.18) | p = 0.723 |
| Safety- PCQ-P d | 3.29 (0.71) | 2.89 (1.04) | 0.40 (0.08,0.71) | p = 0.013 |
| Everydayness- PCQ-P | 4.25 (0.71) | 3.66 (0.80) | 0.58 (0.28,0.88) | p < 0.001 |
| Hospitality- PCQ-P | 2.73 (0.76) | 2.64 (0.95) | 0.09(−0.23,042) | p = 0.579 |
aSD Standard deviation
bCI Confidence interval
cPCQ-S Person-centred Climate Questionnaire-Staff version
dPCQ-P Person-centred Climate Questionnaire-Patient version
Differences based on the ownership of nursing homes
When comparing state-owned nursing homes and not-for-profit privately-owned nursing homes, there were no significant differences in any subscales (p > 0.05).
Discussion
The present study compared resident and staff perspectives of person-centered climate in nursing homes and identified differences that would provide a better understanding of residents’ expectations of a positive climate to support person-centered care. Findings indicated that residents perceived a lower level of person-centered climate in the nursing homes in which they lived compared with staff. Residents in larger nursing homes perceived better climate of person-centered care compared with their counterparts in smaller facilities.
In the present study, the total mean score of PCQ-P was 59.7 (SD 11.5) and was much lower than the total mean score of 86.5 (SD 11.4) reported in a study in Norway [9]. The gap reveals the room for improvement person-centered care for residents in nursing homes in China. The gap also supports the need to conduct studies in this field across the global to promote best practice. Person-centered care ranked by residents is viewed as a crucial quality indicator [5]. A low score should trigger internal investigation into the quality of care for residents by the management group in nursing homes. It is widely recognized that creating person-centered climate requires a system approach to ensure governance, regulation, staffing level and educated preparation for staff to support person-centered care [2, 5]. A low score of person-centered care perceived by residents should also be an indicator for policy review and resource development in the aged care system.
In this study, the perception of person-centered climate by staff was 52.1(SD 9.4) and was lower than the total mean score of 69.9 (SD 9.0) reported in Swedish nursing homes, using the same tools (PCQ-S) [8, 28]. The workload and working conditions across countries might have contributed to the different perspectives of staff about person-centered climate. Nursing homes in China experienced staff high turnover intention, poor staffing stability and found it difficult to retain staff with quality and experience in aged care [20, 42]. These workplace issues were reported as the main factors affecting quality of care, lack of a person-centered care approach for residents and lower staff job satisfaction. Improving staff perspectives of person-centered climate requires organizational cultural change and policy development to value care staff and their contributions to the aged care industry and support them to develop their careers in aged care.
In the present study, the high mean scores (‘somewhat agree’) from staff and the low mean scores (‘somewhat disagree’) from residents on safety climate provided evidence that residents’ expectation of a safe climate was much higher for them than for staff. A climate of safety from the residents’ perspective is usually related to an environment where staff are approachable, available for residents and are competent to care for them [26]. It has been well-documented that safety climate of nursing homes was associated with staffing levels, staff workload and their abilities to identify and meet residents’ care needs in a timely manner [2, 5]. Although the shortage of staff and a low level of staffing were widely reported in higher-income countries, these situations seemed to be much worse in China due to lack of national standards and regulation for staffing levels, and education and training requirements for staff in nursing homes [20, 42]. It has been reported that most nursing homes in China provided residents with very basic services including personal care, basic medical care, room cleaning, meals and laundry, and that the standards and the quality of these care services were not monitored and regulated [42]. Personal care assistants were mainly untrained and had heavy workloads that might have contributed to their inability to attend and respond to residents’ care needs in a timely manner in nursing homes in China [20, 42]. A quality improvement process should address residents’ expectations of a safe environment.
Everydayness climate indicates that an environment enables positive experiences and the sense of belonging to the adopted home as perceived by residents [35]. The higher scores by staff and the lower scores by residents on everydayness climate provided evidence that residents did not share the same level or sense of positive experiences with staff. Studies identified that factors affecting residents’ sense of positive experiences included their autonomy to control their lives, their preferences, care plans and treatment in the nursing home [31, 32]. In these studies, residents usually had a sense of loss of their own homes and had negative experiences when they were admitted to the nursing homes. However, studies also identified that residents were capable of adjusting to their new life in nursing homes if the climate of the nursing homes supported their transition from home care to nursing home care [43]. Developing relationships with staff and other residents were indicators of their successful transition [31, 43]. In China, most personal care assistants were untrained, migrant workers from rural areas who were lacking professional skills necessary to support residents to exercise their autonomy, their preferences and to build meaningful relationships with others [23].
The finding supported previous studies that residents in larger nursing homes perceived a higher level of person-centered climate in the total scale, the subscales of ‘a climate of safety’ and ‘a climate of everydayness’ than those in smaller nursing homes [9]. In the previous study, the differences were explained in that large nursing homes created more spaces for residents to spend the day in different areas of the facility, and had more opportunities to socialize and interact with other residents [9]. Additionally, large nursing homes may also attract more competent employees. Therefore, residents may have had positive experiences and developed good relationships with staff whereby they developed a sense of home and sense of safety.
Limitations
There are several limitations of this study. First, the survey was based on self-selection to participate. The findings therefore might not represent the perspectives of those who chose not to participate in the study. Second, the nature of self-administered survey is associated with bias. Participants, particularly staff might have chosen socially accepted answers in responding to the questions. Third, as this study was undertaken in one province in China, the findings may not reflect nursing homes located in other provinces or regions. In addition, most participants in the study had no cognitive impairment and therefore the findings cannot be generalized to these with cognitive impairment in nursing homes.
Conclusion
In a country with an underdeveloped residential aged care system, residents and staff rank person-centered climate of nursing homes relatively low compared with their counterparts in countries with well-established residential aged care systems. The levels of person-centered climate perceived by residents are significantly lower than that perceived by nursing staff. The findings also indicate that large nursing homes seem to demonstrate better person-centered climate and further studies are needed to explore the factors contributing to these outcomes. The lack of regulations on staffing, workload and staff education and training in China might have contributed to the situations. In addition, the lack of culture to support consumer-directed care in nursing homes in China might also have contributed to the low scores of Person-centered Climate Questionnaire in residents. More studies are needed to explore the impact of these factors on the quality of care for residents. As person-centered climate is one of quality indicators in nursing home care, the findings suggest that both residents and staff need to be engaged in assessing this indicator to identify room for quality improvement. The PCQ-P and PCQ-S provide nurses in leadership and management positions with useful instruments to explore and engage both residents and staff to assess person-centered climate. These tools can be used on items, subscales or total scales based on the need to improve the quality of care for residents or for staff development purposes. Nursing managers should pay attention to the different mean subscale scores from residents and staff, to investigate factors that contributed to the differences. They can also use the results of the mean scores from the three subscales to plan staff development sessions to improve staff knowledge, skills and competence in providing residents with person-centered high-quality care. Nursing managers should also use the assessment outcomes to plan actions to improve organizational culture to facilitate and provide adequate staffing levels and support for staff development.
Acknowledgements
We acknowledge the residents and staff of the nursing homes in this survey, we also thank to the Department of Civil Affairs of Hunan Province for the help and support.
Abbreviations
- PCQ-P
Person-centred Climate Questionnaire-Patient version
- PCQ-S
Person-centred Climate Questionnaire-Staff version
- PSMS
Physical Self-Maintenance Scale
Authors’ contributions
YYX, LH, LDX and HF designed the study. MHX, YYX and LH performed most of the data collection. LH, YYX and WHZ undertook the data analysis and wrote the first draft of this paper. All authors (YYX, LH, LDX, WHZ, MHX, and HF) contributed to manuscript preparation and approved the final manuscript.
Funding
This study was funded by China Medical Board (Grant Number:17–268) and the National Social Science Foundation Project (Grant number: 16BSH055) in China. The funding sources had no role in the design of the study, collection, analysis, and interpretation of data, and in writing the manuscript.
Availability of data and materials
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The research was approved by the Ethical Committee of Xiangya Nursing School, Central South University (Ref No. 2017035). Each nursing home site was assigned a code for data comparison purposes. Returning a completed survey to the researchers was regarded as evidence of participants’ consent to participate in the survey, which was approved by the institutional review board.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yunxia Yang and Hui Li contributed equally to this work.
Contributor Information
Yunxia Yang, Phone: +86-15616247732, Email: xiaoyunyyx@csu.edu.cn.
Hui Li, Phone: +86-13574131432, Email: 167811007@csu.edu.cn.
Lily Dongxia XIAO, Phone: +61882013419, Email: lily.xiao@flinders.edu.au.
Wenhui Zhang, Phone: 1-512-968-8985, Email: vivianzhang@utexas.edu.
Menghan Xia, Phone: +86-18670389739, Email: xia_menghan@qq.com.
Hui Feng, Phone: +86-15173121969, Email: feng.hui@csu.edu.cn.
References
- 1.World Health Organization . Draft WHO global action plan on the public health response to dementia 2017–2025. 2016. [Google Scholar]
- 2.Chenoweth L, Forbes I, Fleming R, King MT, Stein-Parbury J, Luscombe G, et al. PerCEN: a cluster randomized controlled trial of person-centered residential care and environment for people with dementia. Int Psychogeriatr. 2014;26(7):1147–1160. doi: 10.1017/S1041610214000398. [DOI] [PubMed] [Google Scholar]
- 3.Wilberforce M, Challis D, Davies L, Kelly MP, Roberts C, Loynes N. Person-centredness in the care of older adults: a systematic review of questionnaire-based scales and their measurement properties. BMC Geriatr. 2016;16(63). 10.1186/s12877-016-0229-y. [DOI] [PMC free article] [PubMed]
- 4.Chenoweth L, King MT, Jeon YH, Brodaty H, Stein-Parbury J, Norman R, et al. Caring for aged dementia care resident study (CADRES) of person-centred care, dementia-care mapping, and usual care in dementia: a cluster-randomised trial. Lancet Neurol. 2009;8(4):317–325. doi: 10.1016/S1474-4422(09)70045-6. [DOI] [PubMed] [Google Scholar]
- 5.Edvardsson D, Watt E, Pearce F. Patient experiences of caring and person-centredness are associated with perceived nursing care quality. J Adv Nurs. 2017;73(1):217–227. doi: 10.1111/jan.13105. [DOI] [PubMed] [Google Scholar]
- 6.Gilmore-Bykovskyi AL, Roberts TJ, Bowers BJ, Brown RL. Caregiver person-centeredness and behavioral symptoms in nursing home residents with dementia: a timed-event sequential analysis. Gerontologist. 2015;55:S61–SS6. doi: 10.1093/geront/gnu164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yoon JY, Roberts T, Grau B, Edvardsson D. Person-centered climate questionnaire-patient in English: a psychometric evaluation study in long-term care settings. Arch Gerontol Geriatr. 2015;61(1):81–87. doi: 10.1016/j.archger.2015.03.010. [DOI] [PubMed] [Google Scholar]
- 8.Edvardsson D, Sjögren K, Lindkvist M, Taylor M, Edvardsson K, Sandman PO. Person-centred climate questionnaire (PCQ-S): establishing reliability and cut-off scores in residential aged care. J Nurs Manag. 2015;23(3):315–323. doi: 10.1111/jonm.12132. [DOI] [PubMed] [Google Scholar]
- 9.Bergland Å, Hofoss D, Kirkevold M, Vassbø T, Edvardsson D. Person-centred ward climate as experienced by mentally lucid residents in long-term care facilities. J Clin Nurs. 2015;24:406–414. doi: 10.1111/jocn.12614. [DOI] [PubMed] [Google Scholar]
- 10.Chatterji S, Byles J, Cutler D, Seeman T, Verdes E. Health, functioning, and disability in older adults—present status and future implications. Lancet. 2015;385:563–575. doi: 10.1016/S0140-6736(14)61462-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Word Back . Country and lending groups. 2018. [Google Scholar]
- 12.Sjogren K, Lindkvist M, Sandman PO, Zingmark K, Edvardsson D. To what extent is the work environment of staff related to person-centred care? A cross-sectional study of residential aged care. J Clin Nurs. 2014;24:1310–1319. doi: 10.1111/jocn.12734. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization . China country assessment report on ageing and health. 2015. [Google Scholar]
- 14.National Bureau Statistics of China . China statistical yearbook. 2015. [Google Scholar]
- 15.Shen J, Xiao LD. Factors affecting nursing students’ intention to work with older people in China. Nurs Educ Today. 2012;32(3):219–223. doi: 10.1016/j.nedt.2011.03.016. [DOI] [PubMed] [Google Scholar]
- 16.Xiao LD, Shen J, Paterson J. Cross-cultural comparison of attitudes and preferences for Care of the Elderly among Australian and Chinese nursing students. J Transcult Nurs. 2013;24(4):408–416. doi: 10.1177/1043659613493329. [DOI] [PubMed] [Google Scholar]
- 17.Wang J, Xiao LD, He GP, De Bellis A. Family caregiver challenges in dementia care in a country with undeveloped dementia services. J Adv Nurs. 2014;70(6):1369–1380. doi: 10.1111/jan.12299. [DOI] [PubMed] [Google Scholar]
- 18.Xiao LD, Wang J, He GP, De Bellis A, Verbeeck J, Kyriazopoulos H. Family caregiver challenges in dementia care in Australia and China: a critical perspective. BMC Geriatr. 2014;14:6. [DOI] [PMC free article] [PubMed]
- 19.Ministry of Civil Affairs of People's Republic of China . The 2016 of social service development statistical report. 2017. [Google Scholar]
- 20.Shum MHY, Lou VWQ, He KZJ, Chen CCH, Wang JF. The “leap forward” in nursing home development in urban China: future policy directions. J Am Med Dir Assoc. 2015;16(9):784–789. doi: 10.1016/j.jamda.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 21.Wang J, Wang JQ, Cao YL, Jia SM, Wu B. Older Residents’ perspectives of Long-term care facilities in China. J Gerontol Nurs. 2016;42(8):34–43. doi: 10.3928/00989134-20160615-05. [DOI] [PubMed] [Google Scholar]
- 22.Yang W, He AJ, Fang LJ, Mossialos E. Financing institutional long-term care for the elderly in China: a policy evaluation of new models. Health Policy Plan. 2016;31(10):1391–1401. doi: 10.1093/heapol/czw081. [DOI] [PubMed] [Google Scholar]
- 23.Chan T-C, Luk JK-H, Chu L-W, Chan FH-W. Low education level of nursing home staff in Chinese nursing homes. J Am Med Dir Assoc. 2013;14(11):849–850. doi: 10.1016/j.jamda.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 24.Brooker D. What is person-centred care in dementia? Rev Clin Gerontol. 2003;13:215–222. doi: 10.1017/S095925980400108X. [DOI] [Google Scholar]
- 25.Rogers CR. On becoming a person. Houghton Mifflin: New York; 1961. [Google Scholar]
- 26.Edvardsson D, Sandman PO, Rasmussen B. Construction and psychometric evaluation of the Swedish language person-centred climate questionnaire – staff version. J Nurs Manag. 2009;17(7):790–795. doi: 10.1111/j.1365-2834.2009.01005.x. [DOI] [PubMed] [Google Scholar]
- 27.Eve JD. Sustainable practice: how practice development frameworks can influence team work, team culture and philosophy of practice. J Nurs Manag. 2004;12(2):124–130. doi: 10.1111/j.1365-2834.2003.00456.x. [DOI] [PubMed] [Google Scholar]
- 28.Sjögren K, Lindkvist M, Sandman PO, Zingmark K, Edvardsson D. To what extent is the work environment of staff related to person-centred care? A cross-sectional study of residential aged care. J Clin Nurs. 2015;24:1310–1319. doi: 10.1111/jocn.12734. [DOI] [PubMed] [Google Scholar]
- 29.Sjögren K, Lindkvist M, Sandman PO, Zingmark K, Edvardsson D. Person-centredness and its association with resident well-being in dementia care units. J Adv Nurs. 2013;69(10):2196–2206. doi: 10.1111/jan.12085. [DOI] [PubMed] [Google Scholar]
- 30.Lehuluante A, Nilsson A, Edvardsson D. The influence of a person-centred psychosocial unit climate on satisfaction with care and work. J Nurs Manag. 2012;20(3):319–325. doi: 10.1111/j.1365-2834.2011.01286.x. [DOI] [PubMed] [Google Scholar]
- 31.Custers AFJ, Westerhof GJ, Kuin Y, Gerritsen DL, Riksen-Walraven JM. Relatedness, autonomy, and competence in the caring relationship: the perspective of nursing home residents. J Aging Stud. 2012;26(3):319–326. doi: 10.1016/j.jaging.2012.02.005. [DOI] [Google Scholar]
- 32.Falk H, Wijk H, Persson LO, Falk K. A sense of home in residential care. Scand J Caring Sci. 2013;27(4):999–1009. doi: 10.1111/scs.12011. [DOI] [PubMed] [Google Scholar]
- 33.Choi J, Flynn L, Aiken LH. Nursing practice environment and registered Nurses’ job satisfaction in nursing homes. Gerontologist. 2012;52(4):484–492. doi: 10.1093/geront/gnr101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wallin AO, Jakobsson U, Edberg A-K. Job satisfaction and associated variables among nurse assistants working in residential care. Int Psychogeriatr. 2012;24(12):1904–1918. doi: 10.1017/S1041610212001159. [DOI] [PubMed] [Google Scholar]
- 35.Edvardsson D, Sandman PO, Rasmussen B. Swedish language person-centred climate questionnaire - patient version: construction and psychometric evaluation. J Adv Nurs. 2008;63(3):302–309. doi: 10.1111/j.1365-2648.2008.04709.x. [DOI] [PubMed] [Google Scholar]
- 36.Department of Civil Affairs of Hunan Province . The 2015 of statistical bulletin on aging development. 2015. [Google Scholar]
- 37.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179. doi: 10.1093/geront/9.3_Part_1.179. [DOI] [PubMed] [Google Scholar]
- 38.Deng J, Hu J, Wu W, Dong B, Wu H. Subjective well-being, social support, and age-related functioning among the very old in China. Int J Geriatr Psychiatry. 2009;25(7):697–703. doi: 10.1002/gps.2410. [DOI] [PubMed] [Google Scholar]
- 39.Su P, Ding H, Zhang W, Duan G, Yang Y, Long J, et al. Joint Association of Obesity and Hypertension with disability in the elderly-- a community-based study of residents in Shanghai, China. J Nutr Health Aging. 2017;21(4):362–369. doi: 10.1007/s12603-016-0777-z. [DOI] [PubMed] [Google Scholar]
- 40.World Health Organization . International statistical classification of diseases and related health problems (ICD-10) 10. Geneva: WHO; 1992. [Google Scholar]
- 41.Ho SH, Hung WS. The impacts of widowhood, chronic disease, and physical function on mortality among older people. J Nurs Res. 2013;21(2):110–119. doi: 10.1097/jnr.0b013e3182921ff6. [DOI] [PubMed] [Google Scholar]
- 42.Hao Q, Wu S, Ying L, Luo L, Dong D, Dong B. Current dilemmas of nursing homes in Chengdu: a cross-sectional survey. J Am Med Dir Assoc. 2012;13(4):406.e9–406e12. doi: 10.1016/j.jamda.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 43.Brownie S, Horstmanshof L, Garbutt R. Factors that impact residents’ transition and psychological adjustment to long-term aged care: a systematic literature review. Int J Nurs Stud. 2014;51(12):1654–1666. doi: 10.1016/j.ijnurstu.2014.04.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.