Abstract
Small cell neuroendocrine carcinoma (SNEC) of the sino-nasal tract is a rare tumor with aggressive behavior. Invasion of the orbit, brain and base of skull is reported in advanced cases, however clinical presentation of SNEC, primarily as an orbital mass is distinctly rare. A 25-year-old female, presented to a local ophthalmologist with sudden protrusion of eyeball and was diagnosed as an orbital abscess which was incised and drained. She presented to us after six months of initial drainage with rapid increase in protrusion and associated eyelid swelling and was lactating at the time of presentation. The patient underwent clinico-pathological work up and was diagnosed as a primary case of orbital SNEC. She received chemotherapy, with an initial response followed by massive recurrence and subsequently succumbed to the disease after 18 months of presentation to us.
The authors present a literature review and describe the challenges in diagnosis and management of a primary orbital SNEC, which has high propensity to progress, recur, invade neighboring sites, and show distant metastasis inspite of multimodal therapy. Author's recommend close follow up during disease free intervals.
Abbreviation: SNEC, Small cell neuroendocrine carcinoma
Keywords: Small cell neuroendocrine carcinoma, Orbit, Sinonasal, Proptosis, Abscess
Introduction
Small cell neuroendocrine carcinoma (SNEC) is a rare neuroendocrine malignancy with an aggressive behavior. Along with typical, atypical carcinoid and esthesioneuroblastoma, they comprise the spectrum of neuroendocrine malignancies due to their similar cell of origin.1 Presentation of sino nasal and orbital SNEC as an orbital neoplasm is exceedingly rare and to the authors’ best knowledge; there are only 3 reports of SNEC with primarily orbital involvement.[2], [3], [4] Authors hereby report the clinico- pathological features and behavior of SNEC of the orbit and paranasal sinus presenting as an orbital abscess in a young lactating female. Informed consent was taken from the patient and Ethics committee of our Institute approved the study.
Case report
A 25-year-old female, was referred to our Ophthalmic plastic and oncology clinic for a clinically diagnosed left orbital abscess. She was lactating at the time of presentation, with one month history of a full term normal vaginal delivery of a healthy baby. Her symptoms started during first month of pregnancy, with sudden onset of protrusion of left eyeball associated with pain. She noticed a swelling of the left upper lid after 3 months of onset of protrusion and was clinically diagnosed as orbital abscess by a local ophthalmologist. The swelling was surgically drained, however, neither the aspirated material was sent for laboratory evaluation, nor was she prescribed any medications since she was pregnant. She was counseled to visit the clinic only after delivery by the local ophthalmologist.
The patient presented to us after her delivery (six months, status post drainage elsewhere), for further management. Her visual acuity (VA) was 20/20 right eye and 20/80 left eye, unimproved with pinhole. There was a relative afferent pupillary defect of grade III, with an asymmetric left face, swollen and discolored left upper lid with downward and forward protrusion of left eye. There was an abduction and supraduction limitation of −3, and Hertel’s exophthalmometry was asymmetric at 19 mm right eye and 22 mm left eye. Slit lamp examination revealed an upper lid mechanical ptosis with a lagophthalmos of 4 mm. A firm, tender nodule was noted on the lateral aspect of left upper lid with a pus point, increased vascularity, hyperemia and fixity to underlying subcutaneous tissue (Fig. 1a). Dilated fundus examination revealed choroidal folds on the retina. Intraocular pressures were 14 and 18 mm Hg in the right and left eye respectively. General examination revealed few posterior tiny cervical lymph nodes, without any clinically discernible mass in the oropharynx and nasopharynx. Fine needle aspiration of the cervical nodes displayed reactive, non specific morphology.
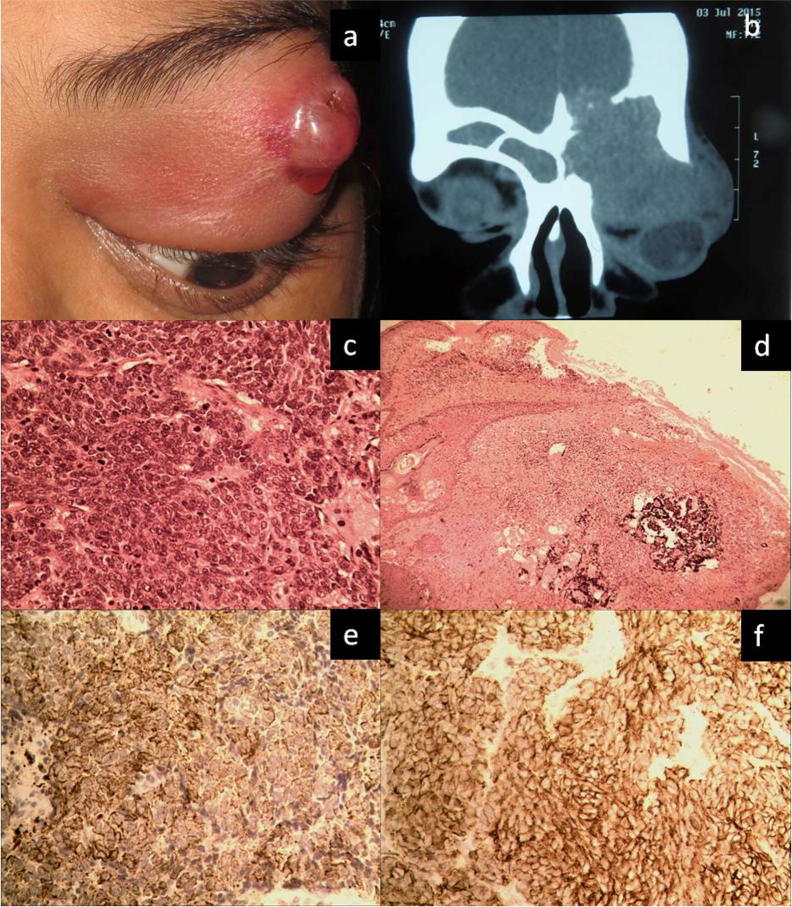
Fig. 1.
Clinical appearance of the patient and histopathology evaluation: Clinical photograph shows left eye proptosis, inferonasal dystopia and a skin nodule on temporal aspect of the upper lid. Also seen is a focal area of suppuration with surrounding vasculature (a). Computed tomography of orbits, coronal view shows a large ill defined homogenous mass filling the entire left orbit and indenting the eyeball. Erosion of the orbital roof is seen with effacement of the left frontal sinus and intracranial extension of the mass (b). Photomicrograph shows syncytial arrangement of small to medium sized round cells with fine granular chromatin. There are brisk mitoses (c, haematoxylin-eosin, original magnification 400×). Tumor cells with crush artefacts are noted in the eyelid dermis (d, original magnification 100×). Tumor cells demonstrate strong cytoplasmic staining with antibodies to cytokeratin (CK) AE1/AE3 (e), and synaptophysin (f) (original magnification 400×).
CT scan of the orbits and brain without contrast displayed a homogenous ill-defined large mass filling the entire left orbit causing globe displacement with anterior ethmoidal and frontal sinus extension. Prominent roof erosion with intracranial invasion was also noted (Fig. 1b). Considering a left sided orbital mass lesion with fronto-ethmoidal sinus involvement, a debulking surgery was performed, under general anaesthesia. Intra-operatively, the eyelid skin was found to be infiltrated by the mass. The tissue was sent for intra operative squash imprint, microbiology evaluation and histopathology evaluation. Squash Imprint smears showed sheets of small round blue cells with scant cytoplasm, and dense nuclei amidst necrotic debris. The permanent sections (Haematoxylin &eosin stain) revealed small to medium sized cells in a syncytial arrangement, scant cytoplasm with focal vacuolations, fine nuclear chromatin and inconspicuous nucleoli (Fig. 1c). There was brisk mitoses and intervening rich fibrovascular network. There was absence of rosettes and neuro-fibrillary stroma. Tumor cell aggregates were also noted in the dermis (Fig. 1d).
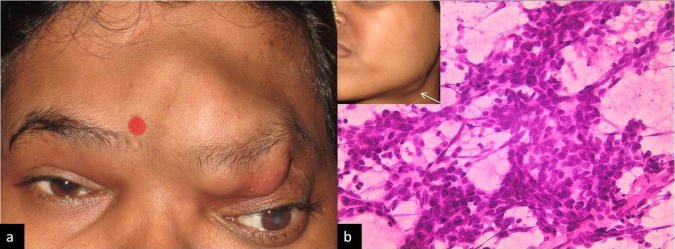
Immunohistochemical staining with Ki-67 showed a proliferation index close to 90%. The tumor cells failed to express CD99, MyoD1, desmin, CD45, CD10, myeloperoxidase, CD68 and CD34. There was strong expression of pan cytokeratin [(pan CK), Fig. 1e] and epithelial membrane antigen. Further, the tumor cells failed to express CK7 and CK20, with strong expression of synaptophysin [(Syn); Fig. 1f], neuron specific enolase (NSE) and CD56. Tumor cells did not express Thyroid transcription factor (TTF-1). Hence a diagnosis of Small cell carcinoma; Neuroendocrine type, left orbit was made and the patient was referred for extensive systemic examination including CT scan chest and bone marrow evaluation, which were unremarkable. Patient was requested to discontinue breastfeeding and was advised 6 cycles of chemotherapy with Cisplatin 30 mg/m2 and Etoposide 100 mg/m2. At follow up after completion of 6 cycles, the patient showed good response, and was advised radiation. The patient deferred further treatment and returned after 7 weeks with a recurrence involving the superomedial orbit left eye, left ethmoid and frontal sinus. With further non compliance, the patient returned after 12 weeks with a massive recurrence progressing further laterally in the orbit and the forehead, left eye; also crossing the midline to involve, the right paranasal sinus, right orbit, eyebrow and forehead [Fig. 2a] VA in the left eye reduced to 20/400 with both eyes, restriction in ocular motility in all directions. VA in the right eye was 20/20. The patient was immediately treated with 4 cycles of chemotherapy again, however showed chemoresistance. Inspite on treatment, she developed left submandibular lymphnode [arrow marked, Inset, Fig. 2b], which was firm, and measured 22 × 14 mm. On aspiration, the smears were involved by the tumor [Fig. 2b]. The patient was counseled and referred to radiation oncologist for palliative radiotherapy. The patient was still under chemo radiation therapy and the patient succumbed to disease after 15 months of presentation to our clinic or after 21 months of her initial presentation to a local ophthalmologist.
Fig. 2.
Clinical follow up and laboratory evaluation, five months after completion of chemotherapy: Clinical presentation with a large nodular left fronto-orbital mass with extension beyond the midline. (a) Aspiration smears show syncytial arrangement of round to oval medium sized cells with fine granular chromatin in a background of necrotic debris (b, Giemsa stain X400). Inset shows the enlarged submandibular lymph node (arrow marked).
Discussion
SNEC are rare neoplasms of the head and neck, and present as sinonasal masses, with or without orbital and intracranial involvement. The medial age of presentation is 5th decade, with slight male preponderance,5 and epistaxis, nasal stuffiness and facial pain as the frequent presenting symptoms.1 A Pubmed search of English literature revealed 3 cases of SNEC presenting as primarily orbital masses with rapid onset peri orbital pain, orbital swelling and proptosis [Table 1]. The cases of primarily orbital SNEC (including our case) showed female preponderance, with median age at diagnoses of 40 years.
Table 1.
Review of cases of small cell neuroendocrine carcinoma with primarily orbital involvement.
| Cases | Age/Sex | Laterality | Symptoms/duration | CT scan | Disease recurrence/outcome after therapy | Treatment | Overall survival |
|---|---|---|---|---|---|---|---|
| Renuka et al.2 | 46/F | Right orbit | Swelling, pain and protrusion/4 weeks | Right orbit, ethmoid sinus and right nostril | NM | Radiotherapy followed by chemotherapy | NM |
| Han et al.3 | 54/M | Right orbit | Pain, swelling and loss of vision/NM | Right orbit, ethmoid, maxillary sinus, posterior sphenoid sinus and nasopharynx | Distant metastasis to lung, pancreas and bone after initial response to radiation therapy | Chemotherapy followed by radiotherapy | 11 months |
| Atik et al.4 | 35/F | Right orbit | Periorbital pain and fullness/3 weeks | Right orbit, ethmoid and right frontal bone. | Left sinonasal and orbital involvement Right cervical lymph node, submandibular and parotid gland involvement. |
Chemotherapy followed by radiation | 2 years |
| Our case | 26/F | Left orbit | Pain, protrusion, swelling/sudden onset | Left orbit, ethmoid, frontal sinus involvement at recurrence | Right sinonasal, right orbit, eyelid and forehead. Left submandibular lymph node involvement |
Chemotherapy followed by radiation (deferred radiation therapy for 5 months) | Succumbed to disease after 21 months. |
Abbreviation: F: female; M: male; NM: not mentioned; f/up- follow up.
Histopathologically diagnosis of SNEC of the orbit poses a major diagnostic challenge to the pathologist, not only for its rarity, or a clinical suspicion of cellulitis, but for its differentiation from other small round blue cell tumors and metastatic lesions. A comprehensive immunohistochemical panel may be required to exclude EWS/ PNET family of tumors, rhabdomyosarcoma, high grade lymphoma, myeloid sarcoma, merkel cell carcinoma, olfactory neuroblastoma, sinonasal undifferentiated carcinoma, amelanotic melanoma and metastatic neuroendocrine malignancies. Young age of our patient, history of lactation, previous drainage which possibly dislodged the tumour cells in the eyelid skin, further compounded the diagnostic and therapeutic challenges. Strong expression of epithelial markers (CK and EMA) and neuroendocrine markers (Synaptophysin and EMA) helped in establishing the diagnosis.
Although, limited literature exists on management and behavior of orbital SNEC, it is known to have an aggressive behavior with frequent recurrences, loco-regional and distant metastasis, poor disease free survival and short overall survival (OS). An average OS of 57% and 10% is reported in literature at the end of 1st and 5th year respectively, inspite of aggressive multimodal therapy. A recent meta- analysis of sino nasal SNEC (127 cases) reported 5-year disease-specific survival of 70.2%.5 Multimodality therapy has been more commonly employed by most clinicians in treating SNEC,6 however recent literature advocates surgical treatment as the corner stone of management of SNEC, with no significant improvement in median disease specific survival with chemotherapy and radiotherapy.5
To summarize, SNEC, may rarely present primarily early in second decade, as an orbital mass of rapid onset and may clinically mimic an abscess. Thus, it is imperative to seek histopathology evaluation of all orbital lesions and drainage specimens. A comprehensive immunohistochemistry panel with systemic evaluation helps in establishing the diagnosis and its differentiation from other small round cell tumors including sinonasal undifferentiated malignancies. Early treatment with close follow up is warranted for better management, with adequate counseling, seeking patient compliance; considering the recurrent and aggressive behavior of the lesion.
Acknowledgments
Acknowledgement
Authors express their gratitude to Operation Eyesight Universal Institute for Eye Cancer and Hyderabad Eye Research Foundation for their support.
Authors also express their gratitude to their senior histotechnician Kalindi Charan Muduli for the technical support.
Funding
This work was supported by Operation Eyesight Universal Institute for Eye Cancer and Hyderabad Eye Research Foundation.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Perez-Ordonez B., Caruana S.M., Huvos A.G., Shah J.P. Small cell neuroendocrine carcinoma of the nasal cavity and paranasal sinuses. Hum Pathol. 1998;29:826–832. doi: 10.1016/s0046-8177(98)90452-x. [DOI] [PubMed] [Google Scholar]
- 2.Renuka I.V., Rao B.S., Sasank R. Sinonasal neuro endocrine carcinoma extending into orbit - a case report. Ind J Otolaryngol Head Neck Surg. 2008;60:156–158. doi: 10.1007/s12070-008-0061-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Han G., Wang Z., Guo X., Wang M., Wu H., Liu D. Extrapulmonary small cell neuroendocrine carcinoma of the paranasal sinuses: a case report and review of the literature. J Oral Maxillofac Surg. 2012;70:2347–2351. doi: 10.1016/j.joms.2011.10.034. [DOI] [PubMed] [Google Scholar]
- 4.Atik A., Krilis M., Shannon K. Small cell neuroendocrine carcinoma masquerading as cellulitis and causing blindness via bilateral orbital involvement. Orbit. 2013;32:197–199. doi: 10.3109/01676830.2013.772209. [DOI] [PubMed] [Google Scholar]
- 5.Van der Laan T.P., Iepsma R., Witjes M.J., Van der Laan B.F., Plaat B.E., Halmos G.B. Meta-analysis of 701 published cases of sinonasal neuroendocrine carcinoma: the importance of differentiation grade in determining treatment strategy. Oral Oncol. 2016;63:1–9. doi: 10.1016/j.oraloncology.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 6.Van der Laan T.P., Bij H.P., van Hemel B.M. The importance of multimodality therapy in the treatment of sinonasal neuroendocrine carcinoma. Eur Arch Otorhinolaryngol. 2013;270:2565–2568. doi: 10.1007/s00405-013-2554-5. [DOI] [PubMed] [Google Scholar]