Abstract
Objective
The aim of this study was to compare single-shot adductor canal block and continuous infusion adductor canal block techniques in total knee arthroplasty patients.
Methods
We prospectively randomized 123 patients who were scheduled for unilateral primary total knee arthroplasty surgery into single shot (n = 60; mean age: 67.1 ± 6.9 years) and continuous (n = 63; mean age: 66.9 ± 6.8 years) adductor canal block groups. Postoperative visual analog scale pain scores, need for additional opioids and functional results as; timed up and go test, the 30-s chair stand test, 5 times sit-to-stand test, the 6-min walking test, the time to active straight leg raise, time to walking upstairs, maximal flexion at the time of discharge, duration of stay in hospital were compared between the two groups.
Results
Pain scores were lower in the continuous adductor canal block group as compared to the single-shot adductor canal block group throughout the postoperative period (p = 0.001). Rescue analgesia was required for 6 (10%) patients in the single shot group and for 1 (1.59%) patient in the continuous group (p = 0.044). Patients in the continuous adductor canal block group displayed better functional results than the single-shot adductor canal block group with respect to active straight-leg rise time (25.52 ± 4.56 h vs 30.47 ± 8.07 h, p = 0.001), 6-min walking test (74.52 ± 29.38 m vs 62.18 ± 33.32 m, p = 0.035) and maximal knee flexion degree at discharge (104.92 ± 5.35° vs 98.5 ± 7.55°, p = 0.001). There was no significant difference between the two groups for other functional and ambulation scores.
Conclusion
Pain control following total knee arthroplasty was found to be better in those patients treated with continuous adductor canal block as compared to those treated with single-shot adductor canal block. Patients treated with continuous adductor canal block also displayed better ambulation and functional recovery following total knee arthroplasty.
Level of evidence
Level I, Therapeutic Study.
Keywords: Adductor canal block, Continuous, Functional recovery, Knee arthroplasty, Single shot
Introduction
Efficient pain management after total knee arthroplasty (TKA) surgery facilitates the rehabilitation and provides better functional results.1 However, despite recent developments in pain control, postoperative pain remains a challenge for both patients and surgeons after TKA. Many modalities, such as epidural analgesia, periarticular infiltration and peripheral nerve block, are used for pain relief after TKA, but there is still no widely accepted guidelines or clear evidence present for an optimum postoperative analgesic regimen.2
Opioid analgesics that are traditionally used via the parenteral or epidural route for the control of pain following TKA surgery are insufficient for pain control and can have side-effects.3 Peripheral nerve blocks (PNB) have become more widely used in recent years as they have fewer side-effects and provide a comparable level of pain control.4 Although femoral nerve block (FNB) is accepted as being very effective in the prevention of pain, as the motor block is formed with the sensory nerve block, postoperative early mobilization is adversely affected due to a reduction in the strength of quadriceps muscle and there is an increased risk of falling.5, 6 Therefore, adductor canal block (ACB), which protects the quadriceps strength by occurrence of an almost pure sensory nerve block, has become an acceptable alternative to FNB as a part of current multimodal pain management protocol.7
The application of ACB can be as a single-shot injection or as a continuous infusion via catheter. The aim of the current study was to compare single-shot adductor canal block (SACB) and continuous infusion adductor canal block (CACB) techniques with regard to early period pain levels, need for additional opioids, and ambulation and functional scores in patients who had undergone primary TKA.
Patients and methods
Study design and subjects
Approval for the study was granted by the Mugla Sitki Kocman University Ethics Committee (File No: 05/1). Written informed consent was obtained from all of the participants. Prospective assessment was done for 128 patients who were scheduled for unilateral primary TKA surgery in our clinic by a single senior surgeon (NHA) between January 2017 and January 2018. Power analysis was applied before the study using a two-sided test at an alpha level of 0.05 and power of 80%, to determine the required sample size for statistical significance. A total of 44 patients was found to be sufficient to determine a 10 mm difference on the pain scale.
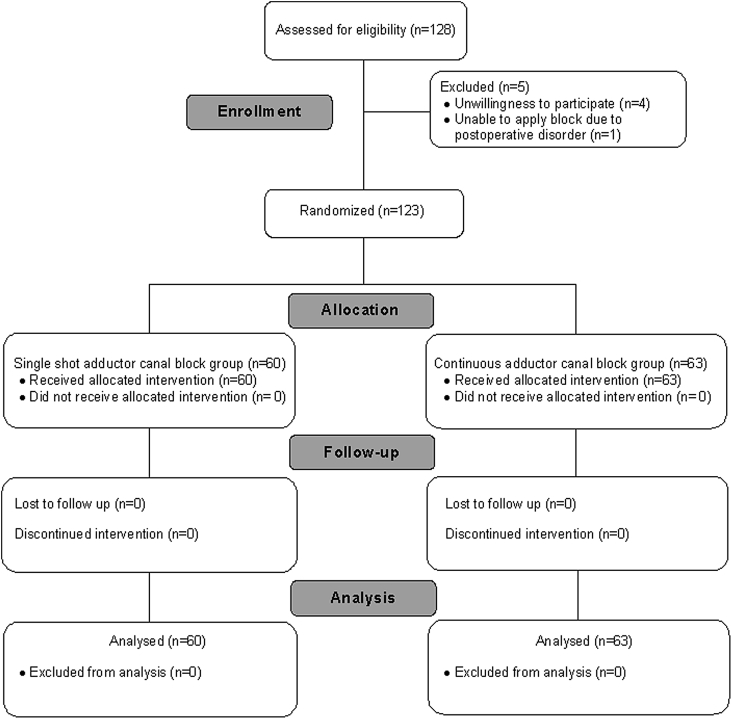
Inclusion and exclusion criteria of the study are given in Table 1. A total of 5 patients were excluded; 4 did not wish to participate and 1 developed a need for postoperative intensive care. With these exclusions, 123 patients were enrolled in the study and randomized into two groups as a continuous adductor canal group (CACB) and a single-shot adductor canal block group (SACB), using a computer-generated randomization table. After randomization, 63 patients were included in the CACB group and 60 patients in the SACB group. No insufficiency of the block developed in any patient and no patient was lost during follow-up. Fig. 1 shows the CONSORT flow diagram of the study. The postoperative functional status analyses were performed prospectively by a single physiotherapist with no knowledge of the patient groups. There was no significant difference between the groups with respect to demographic data, preoperative ASA scores and operating times (Table 2).
Table 1.
Inclusion and exclusion criteria of the study.
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Fig. 1.
CONSORT flow diagram of the study.
Table 2.
Demographic characteristics of patients.
| Parameter | SACB (n = 60) | CACB (n = 63) | p Value |
|---|---|---|---|
| Age (years) | 67.1 ± 6.9 | 66.9 ± 6.8 | 0.895 |
| Gender, n (%) | 0.325 | ||
| Male | 10 (16.7) | 15 (23.8) | |
| Female | 50 (83.3) | 48 (76.2) | |
| Body mass index (kg/m2) | 32.3 ± 4.3 | 31.4 ± 4.8 | 0.785 |
| ASA grade, n (%) | 0.161 | ||
| 1 | 53 (88.3) | 60 (95.2) | |
| 2 | 7 (11.7) | 3 (4.8) | |
| Preoperative VAS pain score | 3.95 ± 0.79 | 4.05 ± 0.85 | 0.551 |
| Operation time (min) | 62.6 ± 6.5 | 61.1 ± 6.2 | 0.18 |
Variables are mean ± standard deviation (SD) or number.
SACB: single shot adductor canal block group; CACB: continuous adductor canal block group; ASA: American Society of Anesthesiologists physical status; VAS: visual analog scale.
Administration of adductor canal block
ACB was applied to all patients immediately after the operation with the technique described by Jenstrup et al.8 Following sterile preparations and draping, a high frequency linear ultrasound (US) transducer (S-Nerve Ultrasound, Sonosite Inc., Bothell, WA, USA) was placed horizontally at the mid-thigh level (approximately halfway between the anterior superior iliac spine and the patella). A 10 cm, 18-gauge needle (Stimuplex, Braun Medical, Melsungen, Germany) was introduced in plane, through the sartorius muscle. Correct position for the tip of the needle in adductor canal was checked with an injection of 10 ml saline. In all patients, 30 ml of 0.25% bupivacaine was administered as a bolus injection with US guidance. In the CACB group patients, a 21-gauge catheter (Contiplex S Set, Braun Medical, Melsungen, Germany) was placed in adductor canal with US guidance and 125 ml of 0.125% bupivacaine infusion was given 5 ml/h for 24 h with a continuous infusion set (Easy Pump, Braun Medical, Melsungen, Germany). All the blocks were applied by a senior anesthesia specialist experienced in US-guided nerve blocks.
Surgical procedure and perioperative management
All of the operations were performed by a single senior surgeon, using a tourniquet and a medial parapatellar approach. Cruciate-retaining implants were used in all cases, as none of the patients were inflammatory arthritis or required posterior cruciate ligament resection and the patella was not changed in any patient. Intra-articular analgesic infiltration was not applied to any patient. For deep vein thrombosis prophylaxis, 40 mg enoxaparin sodium was applied subcutaneously once a day for 4 weeks after discharge.
Preoperative prophylactic intravenous 1 g cefazolin were administered to all patients and postoperative antibiotics were continued for 24 h. In patients with a known allergy to penicillin, 500 mg vancomycin was preferred for prophylaxis. If serum creatinine levels were normal, a dose of 75 mg diclofenac sodium in 100 cc saline was given 8 hourly, for patient controlled analgesia. Otherwise infusion of 1000 mg paracetamol was administered. In both groups, 50 mg tramadol was given as rescue analgesia at the request of the patient in presence of intolerable pain despite the use of standard analgesic regimen. No threshold of VAS pain score was determined for administration of rescue analgesia. The adductor canal catheter was removed at 24 h postoperatively.
Outcome assessments
On admittance, the patients were informed about the VAS and mobilization ability evaluation. Pain was evaluated hourly for the first 12 h postoperatively, and then at 24, 36, 48 and 72 h. On postoperative days 1 and 2, pain on mobilization, opioid consumption and side-effects were evaluated. Ambulation ability was evaluated at 48 h after the surgery using the Timed Up and Go test (TUG), the 30-s chair stand test (30 s-CST), 5 times sit-to-stand test (5×SST) and the 6-min walking test (6MWT). In addition, the time to active straight leg raise (SLR), time to walking upstairs, maximal flexion at the time of discharge, and duration of stay in hospital were evaluated.
Pain was evaluated on a 10 cm VAS, where 0 = no pain and 10 = the worst pain imaginable. The TUG test measures the time taken for an individual to rise from a chair, walk 3 m and return to the chair. The 30 s-CST measures how many times within 30 s the individual can rise from a full sitting position to a full standing position with the arms crossed touching the opposite shoulders. The 5×SST measures the time taken by the individual to rise from a full sitting position to a full standing position 5 times with the arms crossed touching the opposite shoulders. The 6MWT evaluates the distance that can be walked in 6 min. Tests that evaluate function have been validated in previous studies.9, 10
Statistical analysis
Statistical analyses were conducted using SPSS v22.0 software (IBM, Chicago, IL, USA). Conformity of the data to normal distribution was tested with the Kolmogorov–Smirnov test. Independent two samples t-test was used for comparison of continuous variables and Pearson Chi Square test was used for comparison of categorical variables. Results were evaluated in a confidence interval of 95% and at a significance level of p < 0.05.
Results
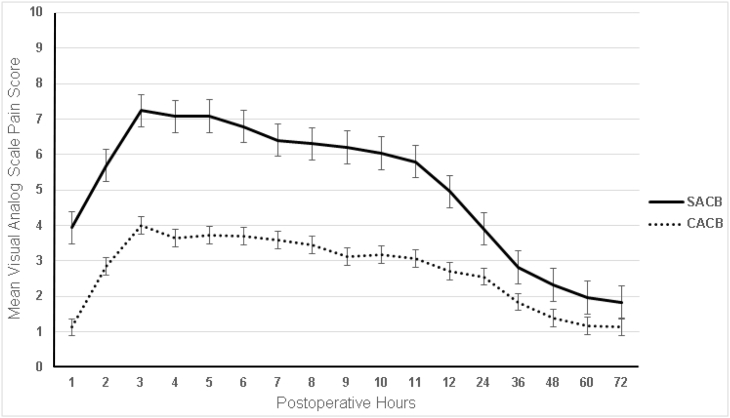
The postoperative mean pain scores for both groups are shown in Table 3. All the pain scores at rest and upon mobilization were determined to be lower in the CACB group patients as compared to the SACB group. The mean difference between the pain scores was the greatest between first 24 h, and the difference between the groups was observed to decrease after 24 h (Fig. 2).
Table 3.
Visual analog scale pain scores of patients according to adductor block technique.
| Postoperative time (h) | Visual analog scale score |
F value | p Value | 95% CI of difference |
||
|---|---|---|---|---|---|---|
| SACB (n = 60) | CACB (n = 63) | Lower | Upper | |||
| At rest | ||||||
| 1 | 3.93 ± 3.73 | 1.13 ± 1.83 | 38.107 | <0.001 | 1.763 | 3.850 |
| 2 | 5.68 ± 3.53 | 2.84 ± 2.61 | 10.854 | <0.001 | 1.735 | 3.949 |
| 3 | 7.23 ± 2.67 | 4 ± 2.62 | 0.031 | <0.001 | 2.288 | 4.179 |
| 4 | 7.07 ± 2.49 | 3.63 ± 2.07 | 1.393 | <0.001 | 2.614 | 4.249 |
| 5 | 7.08 ± 2.36 | 3.73 ± 1.78 | 3.944 | <0.001 | 2.608 | 4.098 |
| 6 | 6.78 ± 2.3 | 3.7 ± 1.91 | 2.638 | <0.001 | 2.332 | 3.838 |
| 7 | 6.4 ± 2.47 | 3.59 ± 2.16 | 1.033 | <0.001 | 1.983 | 3.643 |
| 8 | 6.3 ± 2.51 | 3.46 ± 2.32 | 0.548 | <0.001 | 1.977 | 3.702 |
| 9 | 6.2 ± 2.41 | 3.13 ± 2.15 | 2.446 | <0.001 | 2.258 | 3.888 |
| 10 | 6.03 ± 2.65 | 3.17 ± 2.31 | 3.419 | <0.001 | 1.973 | 3.745 |
| 11 | 5.8 ± 2.74 | 3.06 ± 2.21 | 6.57 | <0.001 | 1.848 | 3.625 |
| 12 | 4.95 ± 2.7 | 2.71 ± 2.09 | 4.023 | <0.001 | 1.374 | 3.097 |
| 24 | 3.9 ± 1.67 | 2.56 ± 2.05 | 2.136 | <0.001 | 0.674 | 2.015 |
| 36 | 2.82 ± 1.37 | 1.84 ± 1.71 | 1.932 | 0.001 | 0.421 | 1.53 |
| 48 | 2.32 ± 1.15 | 1.4 ± 1.23 | 1.892 | <0.001 | 0.492 | 1.348 |
| 60 | 1.97 ± 1.02 | 1.16 ± 1.15 | 4.357 | <0.001 | 0.418 | 1.198 |
| 72 | 1.83 ± 0.99 | 1.14 ± 1.06 | 2.268 | <0.001 | 0.323 | 1.058 |
| After mobilization | ||||||
| 24 | 4.75 ± 1.55 | 3.3 ± 1.84 | 1.74 | <0.001 | 0.837 | 2.06 |
| 48 | 3.13 ± 1.15 | 2.21 ± 1.2 | 1.996 | <0.001 | 0.0505 | 1.349 |
Variables are mean ± standard deviation (SD) or number.
SACB: single shot adductor canal block group; CACB: continuous adductor canal block group; CI: confidence interval.
Fig. 2.
The course of mean visual analog pain scale scores given with standard errors of single-shot adductor canal block (SACB) group and continuous adductor canal block (CACB) group according to postoperative hours following knee arthroplasty.
Postoperative functional recovery and ambulation ability test results according to adductor block technique is shown in Table 4. Patients in the CACB group showed significantly better results than the SACB group in 6MWT, active SLR time and maximal knee flexion at discharge. No difference was determined between the groups with respect to the TUG test, 30 s-CST, 5×SST, the time to ambulation with a walker and time to walking upstairs.
Table 4.
Postoperative functional recovery results according to adductor block technique.
| Variable | SACB (n = 60) | CACB (n = 63) | F value | p Value | 95% CI of difference |
|
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Timed up and go test | 279.75 ± 8.45 | 280.79 ± 8.22 | 0.003 | 0.489 | −1.93 | 4.02 |
| 30-s chair stand test | 5.97 ± 2.48 | 6.67 ± 2.43 | 2.359 | 0.140 | −0.23 | 1.63 |
| 5 times sit-to-stand test (s) | 34.07 ± 17.79 | 29.18 ± 13.11 | 3.594 | 0.084 | −0.66 | 10.45 |
| 6-min walking test (m) | 62.18 ± 33.32 | 74.52 ± 29.38 | 1.354 | 0.035 | −23.54 | −1.13 |
| Active SLR time (h) | 30.47 ± 8.07 | 25.52 ± 4.56 | 47.744 | 0.001 | 2.61 | 7.27 |
| Time to walking upstairs (h) | 71.93 ± 0.36 | 71.71 ± 1.56 | 4.398 | 0.291 | −0.19 | 0.62 |
| Maximal flexion at discharge (degrees) | 98.5 ± 7.55 | 104.92 ± 5.35 | 3.788 | 0.001 | −8.74 | −4.09 |
| Duration of hospital stay (days) | 4.22 ± 0.41 | 4.17 ± 0.38 | 1.371 | 0.561 | −0.11 | 0.18 |
Variables are mean ± standard deviation (SD) or number.
SACB: single shot adductor canal block group; CACB: continuous adductor canal block group; CI: confidence interval; SLR: straight leg raise.
There was a requirement for rescue analgesia for 6 (10%) patients in the SACB group and for 1 (1.59%) patient in the CACB group, with statistically significant difference (p = 0.044) between the two groups in that regard. Rescue analgesia consisting of 50 mg tramadol was applied to 7 patients at 8 h following surgery, and in 1 patient in the SACB group an additional injection was required in the 16th hour. Apart from these patients, the standard analgesia program was administered to all of the other patients. No additional complications related to analgesia developed in any patient.
Discussion
The early postoperative period of TKA is associated with severe pain.11, 12 In pain management protocols following TKA, there has been an increase in the use of PNBs to achieve effective analgesia.13 Adductor canal blocks, just like all other PNBs, cannot provide total analgesia around the knee after TKA, because the knee is innervated by both the lumbar plexus (femoral and obturator nerve) and the sacral plexus (sciatic nerve).14 Nevertheless, the analgesia quality of PNBs has been shown to be close to that of continuous epidural analgesia and the systemic side-effects are fewer.15, 16 In the current study, no systemic side-effects related to ACB developed in any patients.
Although it is known that FNB is very effective with respect to the relief of pain, this method decreases quadriceps muscle strength, thereby impairing postoperative mobilization and increasing the risk of falls.17 In recently published extensive reviews, ACB was shown to facilitate early mobilization by protecting quadriceps strength and provided an analgesic effect similar to that of FNB.7, 18 One of the aims of pain management after TKA should be to achieve a balance between analgesia and muscle strength. As ACB is a purely sensory block, the motor function of only the rectus medialis is affected.19 In a study conducted on healthy individuals, ACB was seen to reduce quadriceps strength by 8%, whereas FNB initially reduced quadriceps strength by 49%.20 Currently, ACB can be applied as single-shot injection or continuous infusion.
In recent years, a few noteworthy studies were published that compare the efficacy of SACB and CACB.21, 22, 23, 24 Shah et al evaluated the results of two adductor block methods after TKA and found better pain scores at postoperative 4, 8, 12 and 24 h in patients with continuous adductor blockade were used.21 Conversely, Zhang et al, Lee et al and Turner et al found similar pain scores after TKA with SACB and CACB techniques.22, 23, 24 We expected similar pain scores in first postoperative 4–6 h with SACB and CACB techniques, and better pain scores in CACB group after 4–6 h as the half-life of bupivacaine is about 3 h.25 However, in the current study, CACB was found to be more effective than SACB in postoperative analgesia following TKA and the mean VAS scores at all the measured time-points were determined to be lower in the CACB group patients than in the SACB group. We think that, dilution of the local anesthetic concentration at the adductor canal with the initial 10 ml saline injection used for dilatation of adductor canal may have caused the poor pain control in the SACB group, as more anesthetic given through the catheter in the CACB group provides higher anesthetic concentration. Additionally, with single shot technique only saphenous nerve is blocked, however the delivery of larger quantity of local anesthetic spreading to adductor canal with continuous infusion may lead to blockade of nerves at the proximal and distal region of the adductor canal such as nerve to vastus medialis and deep nerve plexus and providing better pain relief.14
The greatest difference between the groups was in the postoperative first 24 h and the difference was observed to decrease after 24 h. In a review by Fisher et al of 112 randomized studies, it was stated that pain following TKA was most severe in the first 24 h and was reduced after 24 h.26 The decrease in the difference after 24 h can be attributed to a lessening of the severe pain resulting from TKA after 24 h.
In their study, Shah et al applied rescue analgesia to 2 patients in the SACB group, while no rescue analgesia was needed for any patients in the CACB group. Interestingly, Lee et al found higher opioid consumption in CACB group patients. Catheter displacement and secondary block failure were thought to be the reason for their results.23 In our study, no catheter displacement was observed and there was a need for rescue analgesia in 6 SACB patients and 1 CACB patient. We observed higher need for rescue analgesia in the SACB group compared to CACB group. We think that the higher number of patients requiring rescue analgesia compared to Shah et al is due to local infiltration analgesia or IV-PCA was not used as an assistive analgesia method in our study.
Although the hypothesis of the current study was similar to other studies, there were some differences between these studies and our study with respect to surgical methodology and postoperative care. Unlike the Shah et al study, periarticular infiltration analgesia and postoperative intravenous, patient-controlled analgesia (IV-PCA) were not applied in the current study.21 Local infiltration analgesia is used as a separate technique in postoperative pain management following TKA and there are studies in the literature that have compared it with an adductor block.27, 28 Turner et al performed a sciatic nerve block and a posterior capsule injection to all patients after ACB, that may have influenced the results.23 In our opinion, a clearer analysis could be done to compare the efficacy of the CACB and SACB methods by eliminating the effects of other analgesic techniques.
In the literature, diverse functional results were reported in the comparisons of applying a single shot or continuous ACB. Although the postoperative functional scores of the CACB group were better than those of the SACB group in the study by Shah et al, the difference was not statistically significant.21 Turner et al found a trend of improved straight leg raise ability in SACB group compared to CACB group, with no significant difference. Contrarily, Zhang et al found better quadriceps strength in SACB performed patients compared to patients in the CACB group and they considered that blockade of motor branch of vastus medialis nerve and additionally the spread of local anesthetics to femoral triangle in the CACB group may have caused these results.22
In the current study, the time to SLR was significantly shorter, the degree of knee flexion on discharge was significantly greater, and the distance in the 6MWT was significantly longer in the CACB group as compared to the SACB group. In addition, although there was no statistically significant difference, the CACB group showed better performance than the SACB group with respect to functional recovery times and ambulation ability tests, including mean time to ambulation, mean time to walking upstairs, the TUG test, the 30 s-CST and the 5×STT test. In our opinion, the better functional results obtained in the CACB group was the result of better and longer pain prevention with continuous infusion. Although we did not observed clinically, there are some reports concerning about occurrence of motor nerve block after excessive local anesthetic infiltration into adductor canal.29 We think that, more researches should be required to investigate the quantity of local anesthetics that form motor nerve block with ACB.
Although there are certain advantages of PNB compared to conventional pain control techniques, there are some side-effects such as prolonged nerve paresthesia and infection of the catheter region.30, 31 However, we did not encounter these types of complications in our study after adductor canal blockade.
There are several limitations to the study. Although the physiotherapist performing the ambulation ability tests was blinded to the block technique, the study participants were not blinded to the treatment group and this could lead to bias. Performing all the adductor canal blocks at the same level of the thigh (as the individuals may have had nervous variations) may have affected the results. Although mean BMI levels were similar among the two groups, no dosage adjustment of bupivacaine by weight was done, and a standard dosage was used for all patients, which represents another limitation. Additionally, not performing a cost analysis, that is relevantly important for decision making, among two peripheral nerve block techniques is another limitation of this study. Strengths of the study include the randomized design, the performance of operations by a single surgeon, and the performance of nerve blocks by a single anesthesiologist.
In conclusion, pain control following TKA was found to be superior in the patients given CACB as compared to those given SACB, and with better ambulation and functional recovery. Therefore, if an adductor block is to be used as an analgesia method following TKA, the continuous infusion method is recommended.
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
Contributor Information
Umut Canbek, Email: umutcanbek@mu.edu.tr.
Ulas Akgun, Email: ulasakgun@mu.edu.tr.
Nevres Hurriyet Aydogan, Email: nhaydogan@gmail.com.
Cem Yalin Kilinc, Email: cykilinc@gmail.com.
Ali Ihsan Uysal, Email: aliihsanuysal@gmail.com.
References
- 1.Elmallah R.K., Cherian J.J., Pierce T.P., Jauregui J.J., Harwin S.F., Mont M.A. New and common perioperative pain management techniques in total knee arthroplasty. J Knee Surg. 2016;29(2):169–178. doi: 10.1055/s-0035-1549027. [DOI] [PubMed] [Google Scholar]
- 2.Terkawi A.S., Mavridis D., Sessler D.I. Pain management modalities after total knee arthroplasty: a network meta-analysis of 170 randomized controlled trials. Anesthesiology. 2017;126(5):923–937. doi: 10.1097/ALN.0000000000001607. [DOI] [PubMed] [Google Scholar]
- 3.Gonzales J., Lovald S.T., Lau E.C., Ong K.L. Risk of opioid-related adverse events after primary and revision total knee arthroplasty. J Surg Orthop Adv. 2018;27(2):148–154. [PubMed] [Google Scholar]
- 4.Elmallah R.K., Chughtai M., Khlopas A. Pain control in total knee arthroplasty. J Knee Surg. 2018;31(6):504–513. doi: 10.1055/s-0037-1604152. [DOI] [PubMed] [Google Scholar]
- 5.Kovalak E., Dogan A.T., Uzumcugil O. A comparison of continuous femoral nerve block and periarticular local infiltration analgesia in the management of early period pain developing after total knee arthroplasty. Acta Orthop Traumatol Turc. 2015;49(3):260–266. doi: 10.3944/AOTT.2015.14.0263. [DOI] [PubMed] [Google Scholar]
- 6.Li D., Yang Z., Xie X., Zhao J., Kang P. Adductor canal block provides better performance after total knee arthroplasty compared with femoral nerve block: a systematic review and meta-analysis. Int Orthop. 2016;40(5):925–933. doi: 10.1007/s00264-015-2998-x. [DOI] [PubMed] [Google Scholar]
- 7.Zhao X.Q., Jiang N., Yuan F.F., Wang L., Yu B. The comparison of adductor canal block with femoral nerve block following total knee arthroplasty: a systematic review with meta-analysis. J Anesth. 2016;30(5):745–754. doi: 10.1007/s00540-016-2194-1. [DOI] [PubMed] [Google Scholar]
- 8.Jenstrup M.T., Jaeger P., Lund J. Effects of adductor-canal-blockade on pain and ambulation after total knee arthroplasty: a randomized study. Acta Anaesthesiol Scand. 2012;56(3):357–364. doi: 10.1111/j.1399-6576.2011.02621.x. [DOI] [PubMed] [Google Scholar]
- 9.Scivoletto G., Tamburella F., Laurenza L., Foti C., Ditunno J.F., Molinari M. Validity and reliability of the 10-m walk test and the 6-min walk test in spinal cord injury patients. Spinal Cord. 2011;49(6):736–740. doi: 10.1038/sc.2010.180. [DOI] [PubMed] [Google Scholar]
- 10.Yeung T.S., Wessel J., Stratford P., Macdermid J. Reliability, validity, and responsiveness of the lower extremity functional scale for inpatients of an orthopaedic rehabilitation ward. J Orthop Sports Phys Ther. 2009;39(6):468–477. doi: 10.2519/jospt.2009.2971. [DOI] [PubMed] [Google Scholar]
- 11.Grosu I., Lavand'homme P., Thienpont E. Pain after knee arthroplasty: an unresolved issue. Knee Surg Sports Traumatol Arthrosc. 2014;22(8):1744–1758. doi: 10.1007/s00167-013-2750-2. [DOI] [PubMed] [Google Scholar]
- 12.Liu S.S., Buvanendran A., Rathmell J.P. Predictors for moderate to severe acute postoperative pain after total hip and knee replacement. Int Orthop. 2012;36(11):2261–2267. doi: 10.1007/s00264-012-1623-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gaffney C.J., Pelt C.E., Gililland J.M., Peters C.L. Perioperative pain management in hip and knee arthroplasty. Orthop Clin North Am. 2017;48(4):407–419. doi: 10.1016/j.ocl.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 14.Burckett-St Laurant D., Peng P., Giron Arango L. The nerves of the adductor canal and the innervation of the knee: an anatomic study. Reg Anesth Pain Med. 2016;41(3):321–327. doi: 10.1097/AAP.0000000000000389. [DOI] [PubMed] [Google Scholar]
- 15.Gerrard A.D., Brooks B., Asaad P., Hajibandeh S., Hajibandeh S. Meta-analysis of epidural analgesia versus peripheral nerve blockade after total knee joint replacement. Eur J Orthop Surg Traumatol. 2017;27(1):61–72. doi: 10.1007/s00590-016-1846-z. [DOI] [PubMed] [Google Scholar]
- 16.Leung P., Dickerson D.M., Denduluri S.K. Postoperative continuous adductor canal block for total knee arthroplasty improves pain and functional recovery: a randomized controlled clinical trial. J Clin Anesth. 2018;49(Sep):46–52. doi: 10.1016/j.jclinane.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 17.Kwofie M.K., Shastri U.D., Gadsden J.C. The effects of ultrasound-guided adductor canal block versus femoral nerve block on quadriceps strength and fall risk: a blinded, randomized trial of volunteers. Reg Anesth Pain Med. 2013;38(4):321–325. doi: 10.1097/AAP.0b013e318295df80. [DOI] [PubMed] [Google Scholar]
- 18.Koh I.J., Choi Y.J., Kim M.S., Koh H.J., Kang M.S., In Y. Femoral nerve block versus adductor canal block for analgesia after total knee arthroplasty. Knee Surg Relat Res. 2017;29(2):87–95. doi: 10.5792/ksrr.16.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vora M.U., Nicholas T.A., Kassel C.A., Grant S.A. Adductor canal block for knee surgical procedures: review article. J Clin Anesth. 2016;35(Dec):295–303. doi: 10.1016/j.jclinane.2016.08.021. [DOI] [PubMed] [Google Scholar]
- 20.Jaeger P., Nielsen Z.J., Henningsen M.H., Hilsted K.L., Mathiesen O., Dahl J.B. Adductor canal block versus femoral nerve block and quadriceps strength: a randomized, double-blind, placebo-controlled, crossover study in healthy volunteers. Anesthesiology. 2013;118(2):409–415. doi: 10.1097/ALN.0b013e318279fa0b. [DOI] [PubMed] [Google Scholar]
- 21.Shah N.A., Jain N.P., Panchal K.A. Adductor canal blockade following total knee arthroplasty – continuous or single shot technique? Role in postoperative analgesia, ambulation ability and early functional recovery: a randomized controlled trial. J Arthroplasty. 2015;30(8):1476–1481. doi: 10.1016/j.arth.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Y., Tan Z., Liao R. The prolonged analgesic efficacy of an ultrasound-guided single-shot adductor canal block in patients undergoing total knee arthroplasty. Orthopedics. 2018;41(5):e607–e614. doi: 10.3928/01477447-20180621-05. [DOI] [PubMed] [Google Scholar]
- 23.Lee S., Rooban N., Vaghadia H., Sawka A.N., Tang R. A randomized non-inferiority trial of adductor canal block for analgesia after total knee arthroplasty: single injection versus catheter technique. J Arthroplasty. 2018;33(4):1045–1051. doi: 10.1016/j.arth.2017.11.018. [DOI] [PubMed] [Google Scholar]
- 24.Turner J.D., Dobson S.W., Henshaw D.S. Single-injection adductor canal block with multiple adjuvants provides equivalent analgesia when compared with continuous adductor canal blockade for primary total knee arthroplasty: a double-blinded, randomized, controlled, equivalency trial. J Arthroplasty. 2018;33(10):3160–3166. doi: 10.1016/j.arth.2018.05.026. e3161. [DOI] [PubMed] [Google Scholar]
- 25.Babst C.R., Gilling B.N. Bupivacaine: a review. Anesth Prog. 1978;25(3):87–91. [PMC free article] [PubMed] [Google Scholar]
- 26.Fischer H.B., Simanski C.J., Sharp C. A procedure-specific systematic review and consensus recommendations for postoperative analgesia following total knee arthroplasty. Anaesthesia. 2008;63(10):1105–1123. doi: 10.1111/j.1365-2044.2008.05565.x. [DOI] [PubMed] [Google Scholar]
- 27.Kampitak W., Tanavalee A., Ngarmukos S., Amarase C., Songthamwat B., Boonshua A. Comparison of adductor canal block versus local infiltration analgesia on postoperative pain and functional outcome after total knee arthroplasty: a randomized controlled trial. Malays Orthop J. 2018;12(1):7–14. doi: 10.5704/MOJ.1803.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tong Q.J., Lim Y.C., Tham H.M. Comparing adductor canal block with local infiltration analgesia in total knee arthroplasty: a prospective, blinded and randomized clinical trial. J Clin Anesth. 2018;46(May):39–43. doi: 10.1016/j.jclinane.2018.01.014. [DOI] [PubMed] [Google Scholar]
- 29.Veal C., Auyong D.B., Hanson N.A., Allen C.J., Strodtbeck W. Delayed quadriceps weakness after continuous adductor canal block for total knee arthroplasty: a case report. Acta Anaesthesiol Scand. 2014;58(3):362–364. doi: 10.1111/aas.12244. [DOI] [PubMed] [Google Scholar]
- 30.Cuvillon P., Ripart J., Lalourcey L. The continuous femoral nerve block catheter for postoperative analgesia: bacterial colonization, infectious rate and adverse effects. Anesth Analg. 2001;93(4):1045–1049. doi: 10.1097/00000539-200110000-00050. [DOI] [PubMed] [Google Scholar]
- 31.Feibel R.J., Dervin G.F., Kim P.R., Beaule P.E. Major complications associated with femoral nerve catheters for knee arthroplasty: a word of caution. J Arthroplasty. 2009;24(6 Suppl):132–137. doi: 10.1016/j.arth.2009.04.008. [DOI] [PubMed] [Google Scholar]