Abstract
Ramp lesions are increasingly recognized as a hallmark of posteromedial knee instability. Although the precise mechanisms through which these lesions occur is not completely understood, the distal semimembranosus complex has been implicated in their pathogenesis due to its attachment to the posterior horn of the medial meniscus (PHMM). Arthroscopic dissection of the distal semimembranosus tendon, and the application of traction to it, results in posterior translation of the PHMM and stretching of the meniscocapsular region. This demonstrates a mechanism through which ramp lesions can occur. Furthermore, the subsequent open dissection highlights the complex anatomical relationships of the distal semimembranosus tendon complex, particularly its tensioning effect on the posterior oblique ligament. The clinical relevance of this is that when a ramp lesion occurs, it is likely to be part of a spectrum of posteromedial injury and it should be considered a hallmark of posteromedial instability rather than an isolated meniscocapsular injury.
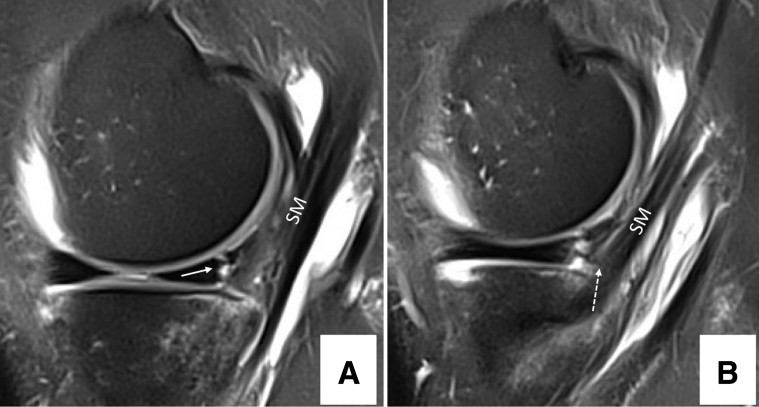
Ramp lesions1, 2, 3, 4 are increasingly recognized as a hallmark of posteromedial knee instability. Several biomechanical studies have demonstrated that these injuries are associated with increased anteroposterior and rotational laxity and that their repair can result in restoration of normal knee kinematics. Although the precise mechanisms through which these lesions occur is not completely understood, the distal semimembranosus complex has been implicated in their pathogenesis due to its attachment to the posterior horn of the medial meniscus (PHMM). This has been demonstrated on both anatomical and imaging studies5 (Fig 1 demonstrates the magnetic resonance imaging appearances of the relationship between semimembranosus and the PHMM). It is hypothesized that during an anterior cruciate ligament (ACL) rupture, excessive anterior tibial translation results in violent semimembranosus contraction and in turn this leads to excessive loading of the posteromedial structures of the knee (PHMM, meniscocapsular junction, meniscotibial ligament, posterior oblique ligament [POL]) resulting in the potential for injury and posteromedial instability.5, 6, 7, 8
Fig 1.
Right knee. Sagittal T2-weighted fat suppression magnetic resonance image. (A) Posterior medial meniscus lesion (white arrow) and its close relationship with semimembranosus tendon. (B) Semimembranosus insertion (white dotted arrow) in the posteromedial tibia plateau. (SM, semimembranosus.)
We present an arthroscopic technique for dissection of the distal semimembranosus tendon complex. This technique has both research and clinical implications for the management and study of posteromedial knee instability.
Surgical Technique
This cadaveric study was conducted in 2 parts. In the first part, the semimembranosus tendon and its attachment to the posterior part of the medial meniscus were arthroscopically dissected. The influence of application of load through the semimembranosus was evaluated. In the second part, an open anatomic dissection of the posteromedial corner was performed to demonstrate the overall relationship with adjacent structures and attachments of the distal semimembranosus complex.
Step 1: Arthroscopic Identification—Transnotch Approach
After a standardized arthroscopic inspection of the joint, the knee was placed in 90° of flexion. Transnotch visualization of the posteromedial compartment was performed by introducing the arthroscope through the anterolateral portal in the triangle limited by the medial condyle, posterior cruciate ligament, and tibial spines. After the contact with this zone, the arthroscope can pass through the space at the condyle border when one is applying a valgus force in flexion.
Step 2: Transseptal Approach and Posteromedial Capsule Resection
The arthroscope was placed through the anteromedial portal, under the ACL, and into the posterolateral compartment. A posterolateral portal was created using the needle localization technique (posterior and proximal to the popliteus tendon). The shaver was introduced through the posterolateral portal and pushed under the septum. The arthroscope was switched from the anteromedial to the anterolateral portal to visualize the septum. The shaver was pushed through the septum, into the posteromedial compartment, under direct arthroscopic visualization. The posteromedial capsule was resected from medial to lateral.
Step 3: Medial Gastrocnemius and Semimembranosus Identification
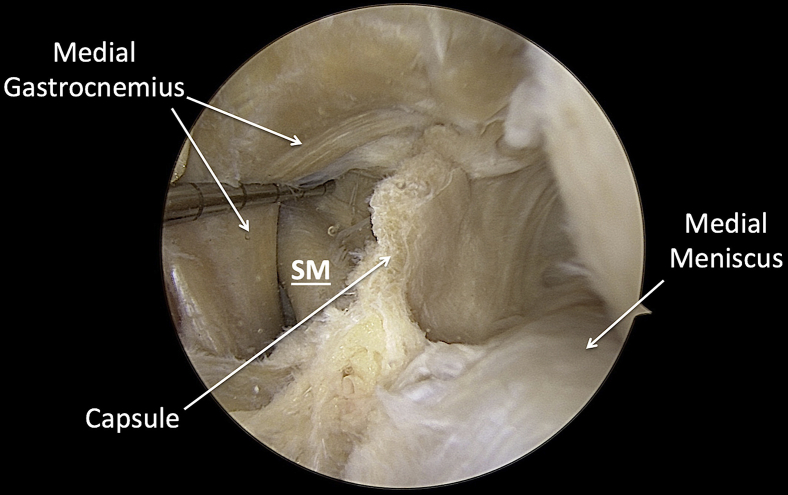
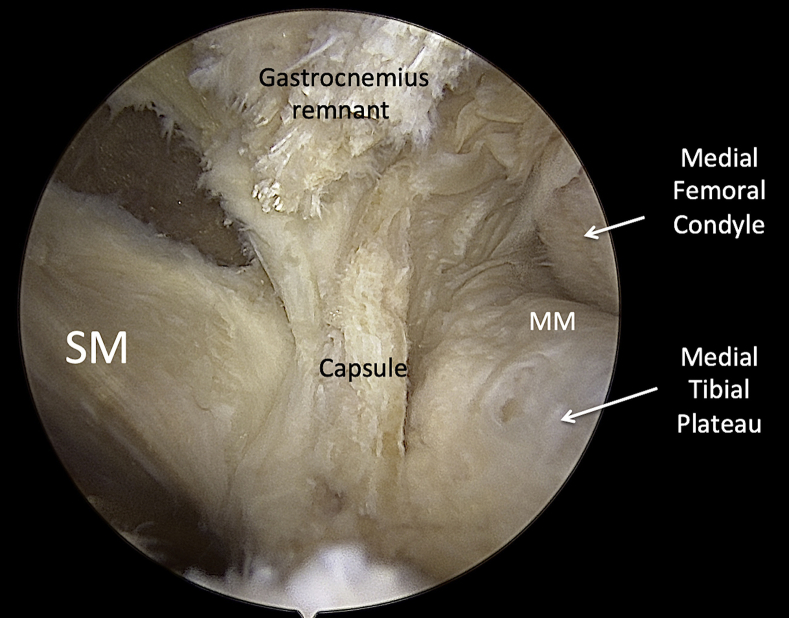
The medial gastrocnemius tendon and the semimembranosus tendon were identified by a combination of probing structures through the posteromedial capsule and then by direct visualization after its resection (Fig 2). The medial gastrocnemius tendon was sectioned at its femoral insertion, facilitating exposure of the semimembranosus tendon (Fig 3) and revealing its anatomical relationships with the adjacent structures described by Sims and Jacobson8 (Fig 4). An arthroscopic suture passer (Knee Scorpion; Arthrex, Naples FL) was used to place a suture within the semimembranosus tendon for the purposes of identification at open exploration and also to allow an assessment of the outcomes of application of load to the semimembranosus on other structures in the posteromedial aspect of the knee.
Fig 2.
Right knee. Transnotch view of the posteromedial compartment after partial capsulectomy. (SM, semimembranosus tendon.)
Fig 3.
Right knee. Transseptal view of the posteromedial compartment after gastrocnemius section. (SM, semimembranosus tendon.)
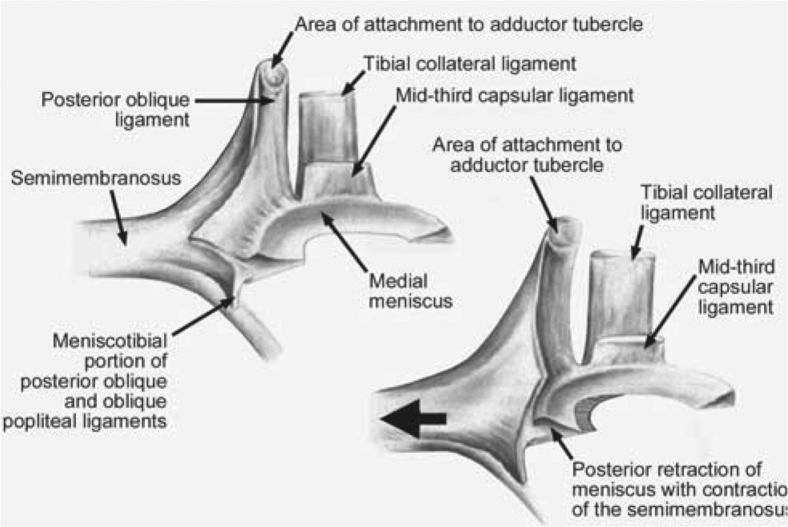
Fig 4.
Original drawing from Sims and Jacobson.8 Intracapsular orientation of the posteromedial corner structures showing the proposed dynamizing action (arrow) of the semimembranosus. Note the relationship of the semimembranosus capsular expansion, the posterior oblique ligament, and the posteromedial meniscus (reprinted with permission).
Step 4: Arthroscopic Evaluation of the Kinematics of the Semimembranosus Tendon and the Posteromedial Corner
The suture that was placed in the semimembranosus tendon was then retrieved externally. The influence of application of load to the distal semimembranosus complex (via the suture) on the posteromedial corner was evaluated arthroscopically during knee flexion and extension (Video 1).
Step 5: Posteromedial Corner Dissection
An open anatomic step-by-step dissection of the posteromedial corner was performed to confirm the correct identification of the semimembranosus tendon and its neighboring structures (Figs 5 and 6). The skin and superficial soft tissues were excised. The sartorius fascia, gracilis, and semitendinosus tendon were reflected. The medial collateral ligament and POL were identified. The previously placed sutures and normal anatomy were used to identify the semimembranosus. The proximal POL was detached and reflected to visualize the strong connection between the semimembranosus and the medial meniscus. Traction on the semimembranosus demonstrated this attachment as well as the tensioning effect it has on the POL (Video 1).
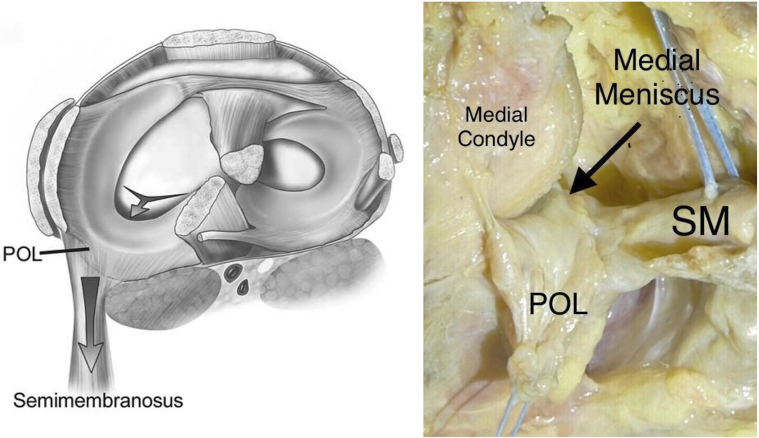
Fig 5.
On the left, the scheme proposed by Sims and Jacobson8: bird's-eye view of the proposed dynamizing action of the semimembranosus. The large arrow represents tension created in the posterior meniscocapsular complex by the semimembranosus. Note the ability of the semimembranosus to tension the posterior oblique ligament (POL) and aid in posterior meniscal retraction, represented by the small arrow (reprinted with permission). IOn the right, the anatomic dissection of the posteromedial corner show on the left. (SM, semimembranosus tendon.)
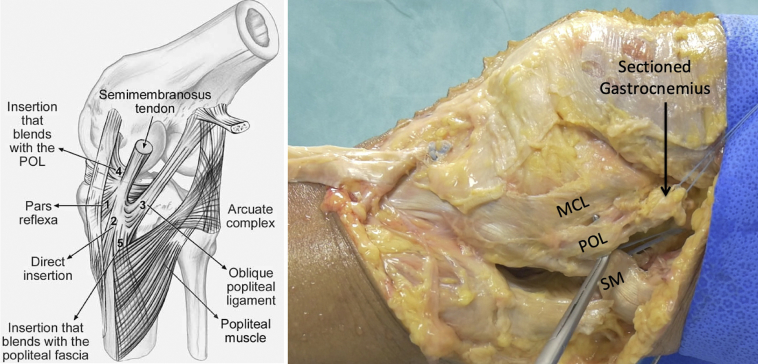
Fig 6.
On the left, the original drawing from Sims and Jacobson8: the semimembranosus expansions. The 5 insertions are (1) pars reflexa, (2) direct posteromedial tibial insertion, (3) oblique popliteal ligament insertion, (4) expansion to posterior oblique ligament (POL), and (5) popliteus aponeurosis expansion. Note the investment into the POL (reprinted with permission). On the right, the anatomic dissection of the posteromedial corner, right knee (MCL, medial collateral ligament; POL, posterior oblique ligament; SM, semimembranosus tendon.).
The pearls and pitfalls of this arthroscopic dissection are given in Table 1, and the advantages and disadvantages of this dissection are given in Table 2.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls | |
|---|---|---|
| Transseptal approach | Allows visualization and dissection of the far medial part of the semimembranosus through the posterolateral approach. | By making the posterolateral portal too posteriorly, one may not properly reach the posteromedial corner. By opening the capsule too distally, one could erroneously resect the semimembranosus expansions to the posterior horn of medial meniscus. |
| Dissection of the medial gastrocnemius tendon | The medial gastrocnemius tendon should be dissected from its femoral insertion for better visualization of the semimembranosus tendon. | By cutting the gastrocnemius tendon too distally, one could also erroneously resect the semimembranosus expansions. |
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| Allows arthroscopic visualization of the relationship between the distal semimembranosus tendon complex and the posterior horn medial meniscus/meniscocapsular junction. | Cadaveric model. Gastrocnemius tendon requires resection for optimal visualization of the distal semimembranosus tendon. |
| No need for extensive dissection. Provides a technique that can be used for future biomechanical studies of posteromedial instability without the need for disrupting normal anatomical relationships by an open dissection. | No biomechanical analysis was performed in this study. |
Discussion
The structural arrangements of the distal semimembranosus tendon and its expansions form the anatomical basis of posteromedial knee instability, including the pathophysiology of ramp lesions. Specifically, at arthroscopic evaluation, the application of load to the semimembranosus tendon resulted in posterior translation of the PHMM and stretching of the meniscocapsular region. This finding is consistent with the work of several previous authors.6, 7
In 1962, Kaplan6 reported that posterior displacement of the medial meniscus during knee flexion occurs as a result of both passive displacement by the femoral condyles and active contraction of the semimembranosus. Hughston,7 in 1993, suggested that the semimembranosus insertion to the posteromedial capsule may stress the peripheral meniscus, resulting in meniscocapsular tearing and posteromedial corner and medial meniscal instability. Similarly, Sims and Jacobson8 identified and described posteromedial injury patterns that may occur as a result of the dynamizing action of the semimembranosus tendon in posterior meniscal retraction.
More recently Yoon et al.9 hypothesized a “contrecoup mechanism” of injury. The authors suggested that excessive anterior translation of the tibia during an ACL rupture would result in a reflex contraction of semimembranosus and that this could explain the high incidence of associated ramp lesions. This hypothesis is compatible with work from Saygi et al.10 who proved the presence of a reflex arc between the medial meniscus and the semimembranosus muscle. The authors demonstrated that electrical stimulation of the PHMM produced an electroneuromyography-verified response of the semimembranosus muscle. Subsequently, Akgun et al.11 reported that mechanical stimulation of the posterior horn receptors during flexion or rotation of the rabbit knee joint also causes semimembranosus muscle contraction and therefore posterior translation of the medial meniscus.
Despite the consistent message in the literature that the semimembranosus tendon and the PHMM share an important relationship, the current dissection study is the first to demonstrate this relationship arthroscopically. Furthermore, the subsequent open dissection highlights the complex anatomical relationships of the distal semimembranosus tendon complex, particularly its tensioning effect on the POL. The clinical relevance of this is that when a ramp lesion occurs, it is likely to be part of a spectrum of posteromedial injury and it should be considered a hallmark of posteromedial instability rather than an isolated meniscocapsular injury.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: B.S-C. is a consultant and receives royalties from Arthrex. M.T. is a consultant for Arthrex. E.C. is a consultant for Arthrex. A.S is a consultant for Arthrex and has provided consultancy for Smith & Nephew within the last 12 months. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Video demonstrating the surgical technique for arthroscopic dissection of the distal semimembranosus tendon in a right knee. The video also demonstrates the influence of simulated semimembranosus contraction on the kinematics of the posterior horn of the medial meniscus and other structures of the posteromedial corner. The skin and superficial soft tissues were excised. The sartorius fascia, gracilis, and ST were reflected. The medial collateral ligament and posterior oblique ligament (POL) were identified. The previously placed sutures and normal anatomy were used to identify semimembranosus (SM). The proximal POL was detached and reflected to visualize the strong connection between SM and the medial meniscus. Traction on SM demonstrated this attachment as well as the tensioning effect it has on the POL.
References
- 1.Liu X., Feng H., Zhang H., Hong L., Wang X.S., Zhang J. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med. 2011;39:832–837. doi: 10.1177/0363546510388933. [DOI] [PubMed] [Google Scholar]
- 2.Sonnery-Cottet B., Conteduca J., Thaunat M., Gunepin F.X., Seil R. Hidden lesions of the posterior horn of the medial meniscus: A systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med. 2014;42:921–926. doi: 10.1177/0363546514522394. [DOI] [PubMed] [Google Scholar]
- 3.Thaunat M., Fayard J.M., Guimaraes T.M., Jan N., Murphy C.G., Sonnery-Cottet B. Classification and surgical repair of ramp lesions of the medial meniscus. Arthrosc Tech. 2016;5:e871–e875. doi: 10.1016/j.eats.2016.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Śmigielski R., Becker R., Zdanowicz U., Ciszek B. Medial meniscus anatomy—from basic science to treatment. Knee Surg Sports Traumatol Arthrosc. 2015;23:8–14. doi: 10.1007/s00167-014-3476-5. [DOI] [PubMed] [Google Scholar]
- 5.DePhillipo N.N., Moatshe G., Chahla J. Quantitative and qualitative assessment of the posterior medial meniscus anatomy: Defining meniscal ramp lesions. Am J Sports Med. 2018 doi: 10.1177/0363546518814258. 363546518814258. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan E.B. Some aspects of functional anatomy of the human knee joint. Clin Orthop. 1962;23:18–29. [PubMed] [Google Scholar]
- 7.Hughston J.C. Mosby Year-Book; St. Louis, MO: 1993. Knee ligaments: injury and repair. [Google Scholar]
- 8.Sims W.F., Jacobson K.E. The posteromedial corner of the knee: Medial-sided injury patterns revisited. Am J Sports Med. 2004;32:337–345. doi: 10.1177/0363546503261738. [DOI] [PubMed] [Google Scholar]
- 9.Yoon K.H., Yoo J.H., Kim K.I. Bone contusion and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture. J Bone Joint Surg Am. 2011;93:1510–1518. doi: 10.2106/JBJS.J.01320. [DOI] [PubMed] [Google Scholar]
- 10.Saygi B., Yildirim Y., Berker N., Ofluoglu D., Karadag-Saygi E., Karahan M. Evaluation of the neurosensory function of the medial meniscus in humans. Arthroscopy. 2005;21:1468–1472. doi: 10.1016/j.arthro.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Akgun U., Kocaoglu B., Orhan E.K., Baslo M.B., Karahan M. Possible reflex pathway between medial meniscus and semimembranosus muscle: An experimental study in rabbits. Knee Surg Sports Traumatol Arthrosc. 2008;16:809–814. doi: 10.1007/s00167-008-0542-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video demonstrating the surgical technique for arthroscopic dissection of the distal semimembranosus tendon in a right knee. The video also demonstrates the influence of simulated semimembranosus contraction on the kinematics of the posterior horn of the medial meniscus and other structures of the posteromedial corner. The skin and superficial soft tissues were excised. The sartorius fascia, gracilis, and ST were reflected. The medial collateral ligament and posterior oblique ligament (POL) were identified. The previously placed sutures and normal anatomy were used to identify semimembranosus (SM). The proximal POL was detached and reflected to visualize the strong connection between SM and the medial meniscus. Traction on SM demonstrated this attachment as well as the tensioning effect it has on the POL.