Abstract
Visual art activities and physical exercise are both low-intensity and low-cost interventions. The present study aims to comprehensively describe published literature on the effectiveness of a combination of these interventions on well-being or quality of life (QoL) and mood of older adults. Embase, CINAHL, Ovid Medline (R), PsycINFO, and Web of Science databases were searched for studies published between 1990 and 2015 that evaluated interventions combining visual art therapy and exercise for people aged 50 years or older with at least one resultant well-being or QoL or mood outcome. We found 10 studies utilizing different combination programs and outcome measures, and most had small sample sizes. Seventy percent of the studies reported that combining both interventions was effective in improving well-being or QoL and mood in older adults. Future studies are, however, requisite to investigate whether in the respective population such a combination is more effective than either of the interventions alone.
Keywords: visual art, exercise, older adults, well-being, quality of life
Increased life expectancy, longevity, and improved living conditions have all contributed to the rapid growth of the older adult population globally (Hutton, 2008; World Health Organization [WHO], 2011). This growth poses challenges on pensions, social insurance, and health care systems (Van Katwyk, 2012; Ng, Hakimi, Byass, Wilopo, & Wall, 2010; Priebe & Howell, 2014). Obviously, appropriate health care for older adults is important given that health problems increase sharply with age (Parker & Thorslund, 2007) and have a negative impact on numerous daily activities (Joshi, Kumar, & Avasthi, 2003). Furthermore, in older adults, problems can easily develop into serious physical and mental health problems, which could increase costs related to medical care, social services, and long-term care (Hutton, 2008; Joshi et al., 2003). Physical health problems could also increase disability and mortality (Schuch et al., 2016) while mental health problems could decrease older people’s well-being, cognitive functioning, and mood, for example, depression (Strawbridge, Wallhagen, & Cohen, 2002). Previous studies affirmed that depression is the most common mental health problem in older people (Cloosterman, Laan, & Alphen, 2013; Neufeld, Freeman, Joling, & Hirdes, 2014). In addition, Jorm (2000) emphasized that depression is a risk factor for cognitive decline and a major source of suffering and disability for older adults. As a result, it is important to maintain an adequate level of well-being in older adults to facilitate successful aging.
The terms well-being and quality of life (QoL) are related and overlap. In Peplau’s theory, QoL is a synonym for well-being or psychological health (Peplau, 1994). QoL represents “a broad range of human experiences related to one’s overall well-being. It implies value based on subjective functioning in comparison with personal expectations and is defined by subjective experiences, states and perceptions” (Revicki et al., 2000, p. 888). Well-being is defined as the evaluation of the self. It involves the presence of positive emotions and the absence of negative emotions, satisfaction with life, fulfillment, and positive functioning in the individual’s entire condition (psychological, social, and spiritual aspects; Deci & Ryan, 2008; Gasper, 2009; Mohan, 2004). Research has found that well-being or QoL is consistently higher in later life than it is among young or middle-aged adults (George, 2010). Nevertheless, the older adults’ well-being will be threatened if they experience health problems. Good physical health is associated with higher levels of life satisfaction and lower levels of depressive symptoms (Mroczek & Spiro, 2005; Strawbridge et al., 2002). Thus, effective interventions for older adults to enable them to adapt successfully to age-related mental and physical decline are welcome (Bowling, 2008; Buman et al., 2010).
Visual art therapy and physical exercise are low-intensity and low-cost interventions that can be easily delivered to older adults and that, indeed, are structured and frequently delivered in nursing homes or community centers (Alders & Levine-Madori, 2010; Fabre, Chamari, Mucci, Masse-Biron, & Prefaut, 2002; Tse, Vong, & Ho, 2012). Visual art therapy has been defined as “a therapeutic process based on spontaneous or prompted creative expression using various art materials and art techniques such as painting, drawing, sculpture, modeling (clay or substitutes), and collage” (Avrahami, 2006, p. 6). It is “a form of psychotherapy that uses art media as its primary mode of communication” (Edwards, 2014, p. 3). During visual art therapy sessions, older adults are asked to perform certain art activities and to utilize art materials to express their thoughts and feelings (Brooke, 1996). In particular, art activities are suitable for older adults who have difficulty expressing themselves because these activities allow them to express their emotions and the art activities could enhance the process of individuation, which is important for older adults to achieve well-being (Brooke, 1996; Edwards, 2014; Fadul, 2014; Jones, Warren, & McElroy, 2006; Knill, Barba, & Fuchs, 1995; Ryff, 1995; Schrade, Tronsky, & Kaiser, 2011). Art offers people the opportunity to explore personal problems without depending on a verbal mode of communication and thereby helps them cope with symptoms, stress, and traumatic experiences in their lives (Brooke, 1996; Buchalter, 2004; Edwards, 2014; Johnson & Sullivan-Marx, 2006; Jones et al., 2006; Stewart, 2004). Previous studies on visual art therapy have revealed that it is effective in reducing depressive symptoms, relieving a sense of despair and improving happiness, peacefulness, satisfaction, and calmness (Im & Lee, 2014; Jones et al., 2006; Rusted, Sheppard, & Waller, 2006).
A systematic review of the clinical effectiveness of art therapy reported that visual art therapy has statistically significant positive effects on depression, anxiety, mood, trauma, distress, QoL, coping ability, and self-esteem, but not on cognition (Uttley et al., 2015). Other reviews of visual art therapy have found that it may be useful across a broad range of populations and specifically for healthy aging and addressing problems related to Alzheimer’s disease (Blomdahl, Gunnarsson, Guregård, & Björklund, 2013; Maujean, Pepping, & Kendall, 2014).
Another intervention that is regularly recommended for older adults is physical exercise, which is defined as a “form of physical activity that is structured and repetitive for a particular length of time and which aims to improve health and fitness” (Caspersen, Powell, & Christenson, 1985, p. 128). Older adults could perform low to moderate intensity of physical exercise. It can be executed all days of the week, or minimally twice a week for a minimum of 30 min of exercise per day, and it has proven beneficial in preventing and treating illnesses as well as in delaying the symptoms of cognitive diseases such as dementia, and of mood disorders, such as depression (Mazzeo & Tanaka, 2001; Stathopoulou, Powers, Berry, Smits, & Otto, 2006; Tse, Wong, & Lee, 2015).
Previous studies found that physical exercise is useful for improving fitness and performance and reducing depression in older adults (Caspersen et al., 1985; Park, Han, & Kang, 2014; Salguero, Garcia, Molinero, & Marquez, 2011; Stanton & Reaburn, 2014; Tse et al., 2015). Physical exercise can also improve cognitive performance, QoL, self-esteem, and mental alertness (Langlois et al., 2012). In addition, physical exercise has been found to decrease anxiety, depression, frustration, tension, and fatigue (Schaefer & Brennan, 2009). It helps older adults become more resilient to the physiological and emotional consequences of psychological stressors (Salmon, 2001). Previous systematic reviews of physical exercise for older adults have reported that physical exercise programs are useful for treating depressive symptoms (Blake, Mo, Malik, & Thomas, 2009; Krogh, Nordentoft, Sterne& Lawlor, 2011; Tse et al., 2015). A meta-analysis of randomized controlled trial (RCT) studies also found that exercise can be a powerful intervention for depression (Stathopoulou et al., 2006). In conclusion, exercise can be beneficial in general, not only for treating diseases but also for improving the mental health of older adults (Viña, Rodriguez-Mañas, Salvador-Pascual, Tarazona-Santabalbina, & Gomez-Cabrera, 2016).
Previous studies have described the utilization of art activities and physical exercise for older adults separately. To some extent, however, a combination of art activities and physical exercise could potentially be more beneficial for older adults than each activity on its own. Clearly, both art therapy and physical exercise can improve mental health, but via different routes. While visual art therapy focuses on mental relaxation after self-expression through nonverbal communication, physical exercise focuses on physical fitness and relaxation. When the interventions are combined, synergistic effects may be reached. Even though each intervention has benefits on its own, the benefit of the one may be expected to reinforce the benefit of the other (Gunnarsson & Eklund, 2009; Monti et al., 2006). To date, however, there is no coherent review of the literature on the combination of these interventions. The aim of this review is, thus, to identify published studies on the combination of visual art activities and physical exercise for adults aged 50 years and older, and to summarize what is understood from these studies regarding the effectiveness of the combination of visual art activities and physical exercise on well-being or QoL and mood of older adults.
Method
The present study is a scoping review, the objective of which is to summarize previous studies that focused on the combination of visual art activities and physical exercise for older adults. As noted in Colquhoun et al. (2014), scoping review is a “form of knowledge synthesis, which incorporates a range of study designs to comprehensively summarize and synthesize evidence with the aim of informing practice, programs and policy and to provide direction to future research priorities” (p. 1291). A scoping review is useful in investigating broader topics of study that have not been discussed previously, and it helps to identify research gaps (Arksey & O’Malley, 2005). In designing and reporting our scoping review, we adopted the framework developed by Arksey and O’Malley (2005).
Search Strategy and Identification of Eligible Studies
The Embase, CINAHL, Ovid Medline (R), PsycINFO, and Web of Science databases were searched for target data in September 2015. The search strategy used keywords related to visual art activities and physical exercises. For visual art activities, we used keywords such as crafts, quilting, pottery, sculpturing, sculpting, painting, drawing, art therapy, and art activity. For physical exercises, we used keywords such as Tai Chi, Qigong, physical activity, yoga, and exercise. The searches were refined with the keywords “combin*” and “integrat*.” Details of the search strategy are displayed in Online Appendix A. We searched for articles published between January 1, 1990,l and September 17, 2015, written in any language. References from relevant articles were scrutinized to identify extra information.
Data were limited to studies that were original reports inclusive of visual art activities and physical exercise carried out by subjects aged 50 and/or older with at least one identified (positive) outcome related to psychological well-being or QoL and mood. Studies that included a mixed age group were, however, excluded unless the results were reported separately for subsample(s) >50 years old. All forms of visual art therapy were included in the data, while music, drama, poetry or writing, storytelling, and dance therapy were excluded. In the case of observational designs, included studies needed to report at least one self-reported well-being or QoL outcome pre- and postintervention. Meanwhile, in terms of RCTs, studies involved needed to measure outcomes immediately before and after intervention. Last but not least, the resultant cognitive abilities and physical symptoms found in the data, as well as fatigue and pain, were not considered well-being or QoL outcomes.
Initially, two reviewers independently reviewed the titles and abstracts of publications identified via the search strategy. Then, if one or both of the reviewers deemed an article to be potentially eligible, the full texts of the relevant articles were examined. At this article selection stage, any discrepancies between the reviewers’ judgments were resolved by discussion.
Data Extraction
A few steps were conducted in the data gathering and analyses. First, one reviewer entered data items into a standardized spreadsheet, which was subsequently checked by the second reviewer. Data that were extracted from the articles comprised (a) author(s), year of publication, country; (b) study design; (c) participant characteristics; (d) interventions; (e) well-being, QoL, or mood outcome; and (f) other key outcomes. A descriptive, analytical approach was used to summarize the data.
We also computed the effect size (ES; Cohen’s d) for the RCTs using the difference between the means of the intervention and control group postintervention, divided by the pooled standard deviations. The ESs would indicate the magnitude of the difference between groups and were interpreted as small (.20 ≤ ES < .50), medium (.50 ≤ ES < .80), and large (ES ≥ .80; Cohen, 1988; Durlak, 2009).
Results
Figure 1 presents a flowchart of the selection process of the included studies.The electronic database search yielded 958 unique publications for review. Nonetheless, during the title and abstract reviews, 801 studies were excluded and, subsequently, 134 other studies were also excluded during full-text review because they did not meet the inclusion criteria. Unfortunately, 10 other articles were also omitted from the study due the unavailability of access to their full texts. Finally, three other articles were irrelevant to the study as well as they were conference abstracts without sufficient information to be included. Thus, in total, 10 articles were included in this scoping review.
Figure 1.
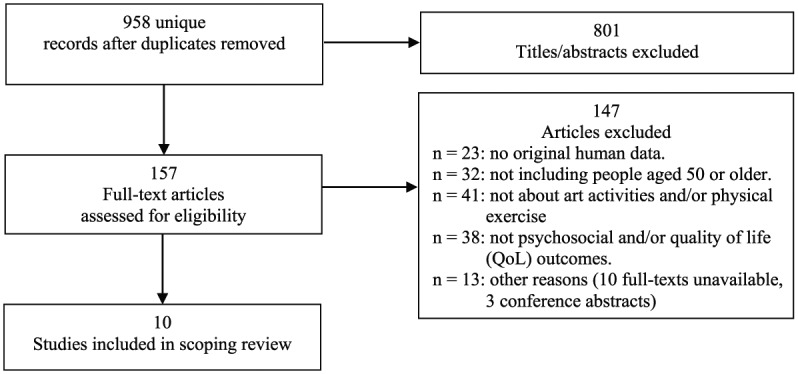
Flowchart of the selection process of the included studies.
Characteristics of Included Studies
Table B1 (Online Appendix B) provides a summary of the characteristics of the 10 studies. Four of the studies were conducted in Asian countries (China, Japan, Korea, and Singapore) and three in European countries (the United Kingdom, Germany, and Finland). The two other studies were from the United States and Canada, and one was conducted in South America (Brazil). Participants in the studies were drawn from the community, clinic/hospital settings, a nursing home, and a center for older adults. The study designs included five studies with RCTs, one non-RCT design, and four observational designs. The sample sizes ranged from 11 to 535 participants, with mean ages ranging from 67 to 85 years.
Participants had to be older adults who did not participate in regular activities, particularly physical exercise (conducted 2 or 3 times a week for at least 20 min at a time) on a regular basis. Four of the 10 studies included participants who had been diagnosed with cognitive impairment (Clinical Dementia Rating Scale [CDR], score 0.5 or 1.0 on the Mini-Mental State Examination [MMSE] score 16 and above; Dannhauser et al., 2014; Kang et al., 2010; Tesky et al., 2014; Viola et al., 2011). Four studies included healthy adults with psychological complaints (subjective feelings of loneliness and depression according to participants’ self-reports, reports by health care providers, or based on a score between 1 and 5 on the Geriatric Depression Scale [GDS] or between 3 and 10 on the Geriatric Anxiety Inventory [GAI]; Kamegaya, Araki, Kigure, & Yamaguchi, 2014; McCaffrey, Liehr, Gregersen, & Nishioka, 2011; Pitkala, Routasalo, Kautiainen, & Tilvis, 2009; Rawtaer et al., 2015). In two of the 10 studies, the participants had experienced medical problems (pain in the previous 6 months or a stroke at least 12 months prior to the study; Rand, Eng, Liu-Ambrose, & Tawashy, 2010; Tse et al., 2012).
The interventions described in the 10 studies had an average duration per session of 1 to 2 hr (ranging from 30 min to 5 hr); the average number of sessions per week was one to two, and total duration of the intervention ranged from 6 weeks to 16 months. Health professionals who delivered the interventions were physiotherapists, certified art psychotherapists, art therapists, nurses or public health nurses, physical trainers or fitness instructors, and a certified Tai Chi instructor. The primary outcomes of the studies were physiological functioning, cognitive performance, and pain reduction, while well-being or QoL or mood was secondary outcomes. Additional information about the interventions can be found in Online Appendix C.
The Effectiveness of a Combination of Art Activities and Physical Exercise Interventions
The outcome measures of well-being or QoL and mood were assessed using different types of measurement. Well-being or QoL outcomes were evaluated in five of the 10 studies using seven different measures, including the Satisfaction in Daily Life (SDL), the Chinese version of the Life Satisfaction Index–A (LSI-A), the Health Survey Short Form questionnaire (SF-12), the Chinese version of the Subjective Happiness Scale, the World Health Organization Quality of Life (WHOQoL)–BREF, the Quality of Life in Alzheimer’s Disease Evaluation Scale (QoL-AD), and Skala zur Erfassung der Lebenszufriedenheit (LBZ, Quality of life scale; Dannhauser et al., 2014; Kamegaya et al., 2014; Tesky et al., 2014; Tse et al., 2012; Viola et al., 2011). In three of these five studies, participants showed a significant improvement in well-being or QoL (Dannhauser et al., 2014; Kamegaya et al., 2014; Viola et al., 2011). The other two studies reported no significant differences between intervention group and control group in terms of well-being or QoL (Tesky et al., 2014; Tse et al., 2012).
Nine studies assessed symptoms of depression using a validated questionnaire (Kamegaya et al., 2014; Kang et al., 2010; McCaffrey et al., 2011; Pitkala et. al., 2009; Rand et al., 2010; Rawtaer et al., 2015; Tesky et al., 2014; Tse et al., 2012; Viola et al., 2011). The most commonly used questionnaire (six out of nine studies) of symptoms of depression was the GDS. Five of the studies reported that feelings of depression had decreased significantly (Kang et al., 2010; McCaffrey et al., 2011; Rawtaer et al., 2015; Tse et al., 2012; Viola et al., 2011). Four other studies showed no significant changes in depression scores between the intervention groups and the control groups. One study did not measure depression as an outcome (Dannhauser et al., 2014). A summary of outcomes is provided in Online Appendix B, Table B2.
There were varieties in the study designs and intervention that consisted of RCTs, non-RCTs, and observational designs. A summary of research designs and description of the interventions is provided in Online Appendix B, Table B2.
RCTs
Five studies had an RCT design. Kamegaya et al. (2014), Tse et al. (2012), and Viola et al. (2011) included outcomes on well-being, QoL, and depression in older people, while Pitkala et al. (2009) assessed depressive symptoms and subjective health outcomes, and McCaffrey et al. (2011) only assessed depressive symptoms.
Kamegaya et al. (2014) conducted an intervention with the primary aim to prevent cognitive decline in elderly subjects who lived in the community. A 12-week intervention program consisting of physical exercise (such as stretching, walking, and taking aerobic exercise) and leisure activities (such as cooking, handcrafting, and competitive games) was administered for 2 hr per week. A sample of 52 participants was randomly allocated to intervention (n = 26) and control (n = 26) groups. Participants in the control group did not attend any art-related or physical-related program during the intervention period. Forty-three remained for the analysis because during the intervention, seven participants dropped out. The results show that the intervention group (n = 19) had improved in well-being or QoL (d = 0.09) compared with the control group (n = 24), but there were no significant differences between the groups in depression (d = 0.2). The result on the Five-Cog test also revealed that there was improvement in cognitive functioning (d = 0.3) in the intervention group but not in the control group after the intervention.
Tse et al. (2012) studied the effects of an integrated pain management program (IPMP) for staff (n = 147) and older people (n = 535) in nursing homes. The program was an 8-week intervention that consisted of pain education for staff and physical exercise and multisensory stimulation through art and craft therapy for residents. Physical exercises included muscle strengthening, stretching, and balance exercises. In the multisensory session and craft therapy, the elderly participants were instructed to control their pain through relaxation techniques and the use of the five primary senses: touch, smell, taste, hearing, and vision. They were also instructed to take deep breaths while listening to relaxing music, to look at attractive pictures and imagine the environment, and to smell the essential oil that was distributed by a diffuser. They also made artworks such as photo albums, paper flowers, and paper fans, and discussed the process with each other. Participants completed pre- and postmeasures. The results revealed that the staff’s knowledge and attitude toward pain management improved significantly. Participants in the experimental group showed higher happiness (d = 0.2) and life satisfaction (d = 0.1) after the program. The QoL in both physical and mental scores in the experimental group was not significantly improved (d = −0.03 for QoL physical and d = 0.09 for QoL mental). Participants were less lonely (d = −0.1) and depressed (d = −0.04). The program was also effective in reducing geriatric pain (d = −0.3).
Viola et al. (2011) evaluated the effects of a multidisciplinary rehabilitation program on cognition, QoL, and neuropsychiatric symptoms in patients with mild Alzheimer disease. The study included 25 Alzheimer patients and their caregivers and involved a 12-week stimulation and psychoeducational program. The control group consisted of 16 Alzheimer’s patients on a waiting list. The program included memory training, computer-assisted cognitive stimulation, expressive activities (painting, verbal expression, and writing), physiotherapy, and physical exercise (walking and stretching). The program was administered twice a week for 60 to 90 min for each activity and performed in group sessions at the hospital. Each session lasted 6.5 hr and included lunch and refreshments. The control group received standard outpatient care, including monthly follow-up visits to the memory clinic. The result revealed that there was a significant improvement in well-being/QoL (d = 0.5). Moreover, there was improvement in depression but the ES was small (d = −0.5), and cognitive functioning remained unchanged.
McCaffrey et al. (2011) examined the effect of a 6-week intervention using garden walking (either alone or guided) compared with art therapy in older adults with depression. Participants in the walk alone group walked alone in the garden for 1 to 2 hr each time. The garden provided benches, resting places, and water stations along the 7- or 8-mile walk. The guided walk group was led by an individual trained in guided imagery. Participants walked together for 1 to 2 hr and were prompted to reflect on thoughts regarding life and nature. The art therapy group, on the contrary, met with a certified art therapist twice a week at a location away from the gardens. This group began by drawing a self-portrait and presenting their portrait to the entire group. Discussions took place each week. During the final session, all of the drawings were hung around the room and a general discussion was held concerning how participants had changed during the 6-week period. The results indicated that depression had decreased from pretest to posttest in the art and exercise groups (d = −0.3). Furthermore, all participants showed a lower percentage of negative-emotion word use and a higher percentage of positive-emotion word use.
Pitkala et al. (2009) investigated the effect of rehabilitation conducted in a new psychosocial group on subjective health, use and cost of the health services, and mortality of lonely older individuals. The intervention was implemented in groups. The participants could choose their activities according to their interests: (a) therapeutic writing and group psychotherapy (n = 48), (b) group exercise and discussions (n = 92), and (c) art and inspiring activities, such as visiting cultural events and sights and actively producing their own artwork (n = 48). The psychosocial intervention in this study included art activities and exercise although there was no direct combination of art and exercise as an intervention. The control group met the study nurses 3 times in 2-hr assessment sessions in which they received personal attention. The psychosocial intervention comprised 12 weekly sessions over 3 months. The results showed that the participants’ health condition improved over a period of a year. No information concerning depressive symptoms after the intervention was given by the authors.
None of these five studies with an RCT design reported large ESs. Four studies described positive result on well-being/QoL and depression, and one study confirmed an improvement in subjective health of older people.
Non-RCT
One study had a non-RCT design. Kang et al. (2010) examined the effects of an integrated dementia intervention for older Korean adults. The intervention consisted of cognitive stimulation training, exercise, music, art, and horticultural therapy. Each session had three phases: an introductory phase, a main phase, and a completion phase. The introductory phase was a 5-min greeting followed by 10 min of warm-up hand exercises. The main phase consisted of a 30-min cognitive stimulation activity involving training aids, followed by a 30-min session of music therapy, a 10-min snack time, 30 min of art therapy, 30 min of a horticultural activity, and 30 min of memory training. A 5-min completion phase ended the session. The intervention comprised two 3-hr sessions each week for 9 weeks. The participants were older adults with mild dementia (n = 38). Twenty participants were assigned to the experimental group and attended 18 program sessions. Eighteen participants were assigned to the control group and received dementia prevention education and consultations. The study found significant differences between the two groups in depression levels as well as mental-emotional health and cognitive functioning. A significant decrease in depression was found in the experimental group compared with the control group. Mental-emotional health was significantly higher in the experimental group than in the control group (d = 1.1). The experimental group also showed significantly higher cognitive function after the intervention, while in the control group, cognitive functioning was found to have decreased. Unfortunately, there were no data available for the ES (Cohen’s d) for the outcome of depression and cognitive functioning except that of mental-emotional health.
Observational Design
Four studies with an observational design were included. Tesky et al. (2014) included well-being/QoL and depression outcomes; the two other studies included a measure of depressive symptoms only (Rand et al., 2010; Rawtaer et al., 2015), whereas one study reported only a well-being/QoL outcome (Dannhauser et al., 2014).
Tesky et al. (2014) investigated the active cognitive stimulation–prevention for elderly people: German: Aktive Kognitive Stimulation – Vorbeugung im Alter–Mild Cognitive Impairment (AKTIVA-MCI) intervention training to improve cognition and mood. There were two groups: (a) cognitive stimulating activities, such as reading, drawing, playing music, or playing chess, and (b) cognitive stimulating activities plus exercise. Exercise such as regular aerobic exercise (stationary biking) was an additional sports intervention. Each intervention was conducted for 30 to 45 min, twice a week over 6 months. Neither participants’ well-being or QoL nor their depressive symptoms had improved after the intervention.
Rand et al. (2010) evaluated the effect of a 6-month exercise and recreation program to improve executive functioning and memory in 27 individuals who had suffered from chronic strokes. The intervention sessions for participants consisted of a 1-hr exercise session and a 1-hr recreational program session twice a week. The exercises included stretching, balance training, and task-specific exercises (steppers, fast walking, and repetitive sit to stand). Participants performed the exercises according to their abilities, although they were supervised throughout the program. The recreation and leisure sessions comprised activities such as playing billiards, bowling, making arts and crafts, and cooking. The results revealed that there was no significant change in depression. Executive functioning and memory are, however, improved.
Rawtaer et al. (2015) evaluated a community-based psychosocial intervention program and its effect on mental health outcomes in older Singaporean adults. Included in the intervention groups were Tai chi exercise (TCE), art therapy (AT), mindfulness awareness practice (MAP), and music reminiscence therapy (MRT). The program was divided into a single intervention phase and a combination intervention phase. Participants could choose between the interventions, then attended weekly activities for 10 weeks, once every 2 weeks for 18 weeks, and monthly for the rest of the year. They adhered to a single intervention for 10 weeks. Subsequently, participants participated in a combination of all four activities for 2 hr, with 30 min each for TCE, MAP, MRT, and AT. In the single intervention phase, there was a significant decrease in depression and anxiety level, but there were no significant differences between the respective groups (TCE, MAP, MRT, and AT). In the combination intervention period, there was a significant improvement regarding depression and anxiety outcomes from baseline to postintervention.
Dannhauser et al. (2014) investigated a complex multimodal activity intervention to reduce the risk of dementia in mildly cognitively impaired patients from two memory clinics. For this study, participants served as their own controls. Data were collected at T0, T1, and T2. The control period was from T0 to T1 and the intervention period from T1 to T2. During the control period of 4 weeks, participants were asked to complete an activity every day. Afterward, participants followed the intervention program, which consisted of three activities: (a) physical activity, such as walking for 30 to 45 min and upright biking; (b) group-based cognitive stimulation training (GCST), which was an arts and crafts education class; and (c) individual cognitive stimulation training (ICST), which was a training to improve cognitive functions such as attention, speed of processing, working memory, problem solving, and reasoning. The results revealed that the 12-week intervention program improved well-being/QoL. Other findings also demonstrated that there were improvements in physical fitness and cognitive outcomes after the intervention.
In summary, two of the observational studies demonstrated that a combination intervention could decrease depression and improve well-being or QoL; in the other two studies, nevertheless, there was no improvement in well-being, QoL, or depression outcomes.
Discussion
This scoping review examined empirical evidence of a combination of art activities and physical exercise on well-being or QoL and mood of older adults. We identified 10 studies, five of which were RCTs (Kamegaya et al., 2014; McCaffrey et al., 2011; Pitkala et al., 2009; Tse et al., 2012; Viola et al., 2011). Over all 10 studies, there was some proof that combining the two interventions could be effective in improving well-being, QoL, or mood among older adults (Dannhauser et al., 2014; Kamegaya et al., 2014; Kang et al., 2010; McCaffrey et al., 2011; Rawtaer et al., 2015; Tse et al., 2012; Viola et al., 2011). In these studies, there were varieties in the intervention programs and outcome measures. In particular, there were three different study designs, seven different questionnaires for measuring well-being or QoL, and nine different ways to assess mood. The primary outcomes were cognitive and physical functioning rather than well-being, QoL, or mood.
Based on this review, we identified four relevant avenues for further research. First, the combination intervention may be useful for older adults with different problems. As noted, the participants are those who experience pain, MCI, Alzheimer’s disease, and psychological problems, such as depression, loneliness, and anxiety.
Second, short-term duration of the intervention is suggested. The studies that showed a positive result conducted the intervention sessions between 1 and 2 hr, once to twice a week for 6 to 18 weeks. Our results are consistent with the previous studies (Mazzeo & Tanaka, 2001; Stathopoulou et al., 2006) which recommend the same duration and intensity of the physical exercise for older adults. Theou et al. (2011) found that it is important to consider the physical limitations of older adults when designing an intervention. Short-term duration (<5 months) of the intervention may be suitable for older adults because it is more structured and focused on the problems of the individual (Pinquart & Sörensen, 2001), whereas long-term duration (>5 months) may have more dropouts as many older adults will most likely experience health problems or may not be able to complete a protracted intervention (Theou et al., 2011).
Third, we recommend assessing well-being and mood as the primary outcomes. We acknowledge that mental health problems, such as depression, are a major source of suffering and disability for older adults (Cloosterman et al., 2013; Neufeld et al., 2014) and a risk factor for cognitive decline (Jorm, 2000). The condition can lead to psychological stress that could accelerate the aging process (Zannas, 2016). Unfortunately, depression in older adults is often underdiagnosed and undertreated (Mansbach, Mace, & Clark, 2015). Thus, knowing older adults’ well-being and mood is an important information while planning and evaluating interventions to improve older adults’ lives and to address their needs (National Research Council, 2013; Steptoe, Deaton, & Stone, 2015; Scholten, Seeley, Mugisha, Zalwango & Wright, 2011). It also prevents and reduces physical and mental health decline of older adults (Friedman, 2012). In addition, we found that 60% of the studies had cognitive and physical function as outcome measures.
Fourth, no studies have evaluated a combination of visual art activities and physical exercise only, although some studies have examined this combination together with additional activities included in the intervention programs. Such activities included games, cooking, speech therapy, occupational therapy, horticultural therapy, writing, and music therapy.
Limitations
There were some limitations in the present study. First, there were wide variations in the study designs and outcome measurements, which preclude our judging the effectiveness of the combination intervention. In particular, there were four observational studies and a nonrandomized study, which have a less strong claim to empirical rigor, and the sample sizes were small (N < 100), which means that the studies are underpowered. As a result, the ESs were generally small (d < 0.5). Second, it was difficult to trace articles on combination interventions for this review. Most of the studies reported the effect of visual art activities and physical exercise separately. There was no direct comparison in the included studies between the combination of visual art activities and physical exercise and single interventions. Hence, it was also difficult to determine the actual effect of the interventions of the included studies as a number of the intervention programs also comprised other activities. Third, given the narrow scope on visual art therapy in combination with physical exercise, the number of articles that we could include in this study is small. In addition, there was no adequate information regarding the visual art activities chosen, which makes it difficult to come up with a detailed visual art activities program for older adults. Fourth, the population of older adults in the included studies was heterogeneous, which makes it hard to generalize the results.
Future Research
Despite all these limitations, the findings of the present study indicate the need for a high-quality research on a combination of visual art activities and physical exercise for older adults. In designing a combination intervention, it needs to be taken into account that additional activities might influence the program’s beneficial effects. Besides, it would be useful to make clear distinctions between the different interventions to find out which specific program is responsible for which particular outcomes. Next, future studies should include cognitive and physical function as another measurement to evaluate the severity of mental and physical functioning before conducting a study. It will be helpful in designing intervention that is suitable for the needs of older adults. As a final point, adequately powered and well-designed studies are needed to investigate whether the combination intervention is more effective than the single intervention discussed in the study.
Conclusion
The findings from this review indicate that an intervention combining visual art activities and physical exercise may offer psychological, cognitive, and physical health benefits for people aged 50 years and older with different psychological and physical problems. Yet, research that directly compares the effect of combination interventions versus the two single interventions still needs to be conducted.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The first author received financial support from Universitas Tarumanagara, Indonesia for the research, and Radboud University, The Netherlands for the authorship and publication of this article.
Supplementary Material: Online Appendix for this article is available online.
References
- Alders A., Levine-Madori L. (2010). The effect of art therapy on cognitive performance of Hispanic/Latino older adults. Art Therapy, 27, 127-135. doi: 10.1080/07421656.2010.10129661 [DOI] [Google Scholar]
- Arksey H., O’Malley L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8, 19-32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Avrahami D. (2006). Visual art therapy’s unique contribution in the treatment of posttraumatic stress disorders. Journal of Trauma & Dissociation, 6, 5-38. doi: 10.1300/J229v06n04_02 [DOI] [PubMed] [Google Scholar]
- Blake H., Mo P., Malik S., Thomas S. (2009). How effective are physical activity interventions for alleviating depressive symptoms in older people? A systematic review. Clinical Rehabilitation, 23, 873-887. doi: 10.1177/0269215509337449 [DOI] [PubMed] [Google Scholar]
- Blomdahl C., Gunnarsson B., Guregård S., Björklund A. (2013). A realist review of art therapy for clients with depression. The Arts in Psychotherapy, 40, 322-330. doi: 10.1016/j.aip.2013.05.009 [DOI] [Google Scholar]
- Bowling A. (2008). Enhancing later life: How older people perceive active ageing? Aging & Mental Health, 12, 293-301. [DOI] [PubMed] [Google Scholar]
- Brooke S. L. (1996). Tools of the trade: A therapist’s guide to art therapy assessments. Springfield, IL: Charles C Thomas. [Google Scholar]
- Buchalter S. I. (2004). A practical art therapy. Pentonville Road, UK: Jessica Kingsley. [Google Scholar]
- Buman M. P., Hekler E. B., Haskell W. L., Pruitt L., Conway T. L., Cain K. L., . . . King A. C. (2010). Objective light-intensity physical activity associations with rated health in older adults. American Journal of Epidemiology, 172, 1155-1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspersen C. J., Powell K. E., Christenson G. M. (1985). Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Reports, 100, 126-131. [PMC free article] [PubMed] [Google Scholar]
- Cloosterman N. H. M., Laan A. J., Van Alphen B. P. J. (2013). Characteristics of psychotherapeutic integration for depression in older adults: A Delphi study. Clinical Gerontologist, 36, 395-410. doi: 10.1080/07317115.2013.816815 [DOI] [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum. [Google Scholar]
- Colquhoun H. L., Levac D., O’Brien K. K., Straus S., Tricco A. C., Perrier L., . . . Moher D. (2014). Scoping reviews: Time for clarity in definition, methods, and reporting. Journal of Clinical Epidemiology, 67, 1291-1294. doi: 10.1016/j.jclinepi.2014.03.013 [DOI] [PubMed] [Google Scholar]
- Dannhauser T. M., Cleverley M., Whitfield T. J., Fletcher B. C., Stevens T., Walker Z. (2014). A complex multimodal activity intervention to reduce the risk of dementia in mild cognitive impairment-thinkingfit: Pilot and feasibility study for a randomized controlled trial. BMC Psychiatry, 14, Article 129. doi: 10.1186/1471-244X-14-129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deci E. L., Ryan R. M. (2008). Hedonia, eudaimonia, and well-being: An introduction. Journal of Happiness Studies, 9, 1-11. doi: 10.1007/s10902-006-9018-1 [DOI] [Google Scholar]
- Durlak J. A. (2009). How to select, calculate, and interpret effect sizes. Journal of Pediatric Psychology, 34, 917-928. doi: 10.1093/jpepsy/jsp004 [DOI] [PubMed] [Google Scholar]
- Edwards D. (2014). Creative Therapies in Practice Series: Art therapy (2nd ed., Wilkins P., Series Ed.). London, England: SAGE Publications, Ltd. [Google Scholar]
- Fabre C., Chamari K., Mucci P., Masse-Biron J., Prefaut C. (2002). Improvement of cognitive function by mental and/or individualized aerobic training in healthy elderly subjects. International Journal of Sports Medicine, 23, 415-421. [DOI] [PubMed] [Google Scholar]
- Fadul J. A. (2014). Encyclopedia of theory & practice in psychotherapy & counseling. Raleigh, NC, USA: Lulu Press Inc. [Google Scholar]
- Friedman E. M. (2012). Well-being, aging, and immunity. In Segerstrom S. C. (Ed.), The Oxford handbook of psychoneuroimmunology. Oxford University Press. doi: 10.1093/oxfordhb/9780195394399.013.0003 [DOI] [Google Scholar]
- Gasper D. (2009). Understanding the diversity of conceptions of well-being and quality of life (Working Paper No.483). Hague, The Netherlands: International Institute of Social Studies. [Google Scholar]
- George L. K. (2010). Still happy after all these years: Research frontiers on subjective wellbeing in later life. Journal of Gerontology Series B: Psychological Sciences & Social Sciences, 65B, 331-339. doi: 10.1093/geronb/gbq006 [DOI] [PubMed] [Google Scholar]
- Gunnarsson A. B., Eklund M. (2009). The tree theme method as an intervention in psychosocial occupational therapy client acceptability and outcomes. Australian Occupational Therapy Journal, 56, 167-176. doi: 10.1111/j.1440-1630.2008.00738.x [DOI] [PubMed] [Google Scholar]
- Hutton D. (2008). Older people in emergencies: Considerations for action and policy development. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Im M. L., Lee J. I. (2014). Effects of the art and music therapy on the depression and cognitive function of elderly. Technology and Health Care, 22, 453-458. doi: 10.3233/THC-140803 [DOI] [PubMed] [Google Scholar]
- Johnson C. M., Sullivan-Marx E. M. (2006). Art therapy: Using the creative process for healing and hope among African American older adults. Geriatric Nursing, 27, 309-316. doi: 10.1016/j.gerinurse.2006.08.010 [DOI] [PubMed] [Google Scholar]
- Jones F., Warren A., McElroy S. (2006). Home-based art therapy for older adults with mental health needs: Views of clients and caregivers. Journal of the American Art Therapy Association, 23, 52-58. doi: 10.1080/07421656.2006.10129640 [DOI] [Google Scholar]
- Jorm A. F. (2000). Is depression a risk factor for dementia or cognitive decline? A review. Gerontology, 46, 219-227. doi: 10.1159/000022163 [DOI] [PubMed] [Google Scholar]
- Joshi K., Kumar R., Avasthi A. (2003). Morbidity profile and its relationship with disability and psychological distress among elderly people in Northern India. International Journal of Epidemiology, 32, 978-987. doi: 10.1093/ije/dyg204 [DOI] [PubMed] [Google Scholar]
- Kamegaya T., Araki Y., Kigure H., Yamaguchi H. (2014). Twelve-week physical and leisure activity programme improved cognitive function in community-dwelling elderly subjects: A randomized controlled trial. Psychogeriatrics, 14, 47-54. doi: 10.1111/psyg.12038 [DOI] [PubMed] [Google Scholar]
- Kang H. Y., Bae Y. S., Kim E. H., Lee K. S., Chae M. J., Ju R. A. (2010). An integrated dementia intervention for Korean older adults. Journal of Psychosocial Nursing and Mental Health Services, 48, 42-50. [DOI] [PubMed] [Google Scholar]
- Knill P., Barba H., Fuchs M. (1995). Minstrels of the soul. Toronto, Ontario, Canada: Palmerston Press. [Google Scholar]
- Krogh J., Nordentoft M., Sterne J. A., Lawlor D. A. (2011). The effect of exercise in clinically depressed adults: Systematic review and meta-analysis of randomized controlled trials. Journal of Clinical Psychiatry, 72, 529-538. doi: 10.4088/JCP.08r04913blu [DOI] [PubMed] [Google Scholar]
- Langlois F., Vu T. T. M., Chassé K., Dupuis G., Kergoat M. J., Bherer L. (2012). Benefits of physical exercise training on cognition and quality of life in frail older adults. Journals of Gerontology Series B: Psychological Sciences & Social Sciences, 68, 400-404. doi: 10.1093/geronb/gbs069 [DOI] [PubMed] [Google Scholar]
- Mansbach W. E., Mace R. A., Clark K. M. (2015). The Brief Anxiety and Depression Scale (BADS): A new instrument for detecting anxiety and depression in long-term care residents. International Psychogeriatrics, 27, 673-681. [DOI] [PubMed] [Google Scholar]
- Maujean A., Pepping C. A., Kendall E. (2014). A systematic review of randomized controlled studies of art therapy. Art Therapy, 31, 37-44. doi: 10.1080/07421656.2014.873696 [DOI] [Google Scholar]
- Mazzeo R. S., Tanaka H. (2001). Exercise prescription for the elderly: Current recommendations. Sports Medicine, 31, 809-818. [DOI] [PubMed] [Google Scholar]
- McCaffrey R., Liehr P., Gregersen T., Nishioka R. (2011). Garden walking and art therapy for depression in older adults. Research in Gerontological Nursing, 4, 237-242. doi: 10.3928/19404921-20110201-01 [DOI] [PubMed] [Google Scholar]
- Mohan K. (2004). Eastern perspectives and implications for the west. In Jewell A. (Ed.), Ageing, spirituality and well-being (pp. 116-179). London, England: Jessica Kingsley. [Google Scholar]
- Monti D. A., Peterson C., Shakin Kunkel E. J., Hauck W. W., Pequignot E., Rhodes L., Brainard G. C. (2006). A randomised, controlled trial of mindfulness-based art therapy (MBAT) for women with cancer. Psycho-Oncology, 15, 363-373. doi: 10.1002/pon.988 [DOI] [PubMed] [Google Scholar]
- Mroczek D. K., Spiro A., III (2005). Change in life satisfaction during adulthood: Findings from the veterans affairs normative aging study. Journal of Personality and Social Psychology, 88, 189-202. [DOI] [PubMed] [Google Scholar]
- National Research Council. (2013). Subjective well-being: Measuring happiness, suffering, and other dimensions of experience. In Stone A. A., Mackie C. (Eds.), Committee on national statistics: Division of behavioral and social sciences and education (pp. 1-190). Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Neufeld E., Freeman S., Joling K., Hirdes J. P. (2014). “When the golden years are blue”: Changes in depressive symptoms over time among older adults newly admitted to long-term care facilities. Clinical Gerontologist, 37, 298-315. doi: 10.1080/07317115.2014.885919 [DOI] [Google Scholar]
- Ng N., Hakimi M., Byass P., Wilopo S., Wall S. (2010). Health and quality of life among older rural people in purworejo district, Indonesia. Global Health Action, 3, Article 2125. doi: 10.3402/gha.v3i0.2125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S.-H., Han K. S., Kang C.-B. (2014). Effects of exercise programs on depressive symptoms, quality of life and self-esteem in older people: A systematic review of randomized controlled trials. Applied Nursing Research, 27, 219-226. doi: 10.1016/j.apnr.2014.01.004 [DOI] [PubMed] [Google Scholar]
- Parker M. G., Thorslund M. (2007). Health trends in the elderly population: Getting better and getting worse. The Gerontologist, 47, 150-158. [DOI] [PubMed] [Google Scholar]
- Peplau H. E. (1994). Quality of life: An international perspective. Nursing Science Quarterly, 7, 10-15. doi: 10.1177/089431849400700107 [DOI] [PubMed] [Google Scholar]
- Pinquart M., Sörensen S. (2001). How effective are psychotherapeutic and other psychosocial interventions with older adults? A meta-analysis. Journal of Mental Health and Aging, 7, 207-243. [Google Scholar]
- Pitkala K. H., Routasalo P., Kautiainen H., Tilvis R. S. (2009). Effects of psychosocial group rehabilitation on health, use of health care services, and mortality of older persons suffering from loneliness: A randomized, controlled trial. Journals of Gerontology Series A: Biological Sciences & Medical Sciences, 64A, 792-800. doi: 10.1093/gerona/glp011 [DOI] [PubMed] [Google Scholar]
- Priebe J., Howell F. (2014). Old-age poverty in Indonesia: Empirical evidence and policy options—A role for social pensions (TNP2K Working Paper 07-2014). Tim Nasional Percepatan Penanggulangan Kemiskinan (TNP2K), Jakarta, Indonesia. [Google Scholar]
- Rand D., Eng J. J., Liu-Ambrose T., Tawashy A. E. (2010). Feasibility of a 6-month exercise and recreation program to improve executive functioning and memory in individuals with chronic stroke. Neurorehabilitation and Neural Repair, 24, 722-729. doi: 10.1177/1545968310368684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawtaer I., Mahendran R., Yu J., Fam J., Feng L., Kua E. H. (2015). Psychosocial interventions with art, music, tai chi and mindfulness for subsyndromal depression and anxiety in older adults: A naturalistic study in singapore. Asia-Pacific Psychiatry, 7, 240-250. doi: 10.1111/appy.12201 [DOI] [PubMed] [Google Scholar]
- Revicki D. A., Osoba D., Fairclough D., Barofsky I., Berzon R., Leidy N. K., Rothman M. (2000). Recommendations on health-related quality of life research to support labeling and promotional claims in the United States. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 9, 887-900. [DOI] [PubMed] [Google Scholar]
- Rusted J., Sheppard L., Waller D. (2006). A multi-centre randomized control group trial on the use of art therapy for older people with dementia. Group Analysis, 39, 517-536. doi: 10.1177/0533316406071447 [DOI] [Google Scholar]
- Ryff C. D. (1995). Psychological well-being in adult life. Current Directions in Psychological Science, 4, 99-104. doi: 10.1111/1467-8721.ep10772395 [DOI] [Google Scholar]
- Salguero A., Garcia R. M., Molinero O., Marquez S. (2011). Physical activity, quality of life and symptoms of depression in community-dwelling and institutionalized older adults. Archives of Gerontology and Geriatrics, 53, 152-157. doi: 10.1016/j.archger.2010.10.005 [DOI] [PubMed] [Google Scholar]
- Salmon P. (2001). Effects of physical exercise on anxiety, depression, and sensitivity to stress: A unifying theory. Clinical Psychology Review, 21, 33-61. doi: 10.1016/S0272-7358(99)00032-X [DOI] [PubMed] [Google Scholar]
- Schaefer P., Brennan J. (2009, Spring). Psychological benefits of exercise. The Ohio Family Physician, pp. 30-32. [Google Scholar]
- Scholten F., Seeley J., Mugisha J., Zalwango F., Wright S. (2011). Well-being of older people study: A study on global ageing and adult health (SAGE) sub-study. Medical Research Council/ Uganda Virus Research Unit, Research Unit on AIDS, Entebbe, Uganda. Switzerland: World Health Organisation. [Google Scholar]
- Schrade C., Tronsky L., Kaiser D. H. (2011). Physiological effects of mandala making in adults with intellectual disability. The Arts in Psychotherapy, 38, 109-113. doi: 10.1016/j.aip.2011.01.002 [DOI] [Google Scholar]
- Schuch F. B., Vancampfort D., Rosenbaum S., Richards J., Ward P. B., Veronese N., . . . Stubbs B. (2016). Exercise for depression in older adults: A meta-analysis of randomized controlled trials adjusting for publication bias. Revista Brasileira de Psiquiatria, 38, 247-254. doi: 10.1590/1516-4446-2016-1915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton R., Reaburn P. (2014). Exercise and the treatment of depression: A review of the exercise program variables. Journal of Science and Medicine in Sport, 17, 177-182. doi: 10.1016/j.jsams.2013.03.010 [DOI] [PubMed] [Google Scholar]
- Stathopoulou G., Powers M. B., Berry A. C., Smits J. A. J., Otto M. W. (2006). Exercise interventions for mental health: A quantitative and qualitative review. Clinical Psychology: Science and Practice, 13, 179-193. doi: 10.1111/j.1468-2850.2006.00021.x [DOI] [Google Scholar]
- Steptoe A., Deaton A., Stone A. (2015). Subjective wellbeing, health, and ageing. The Lancet, 385, 640-648. doi: 10.1016/S0140-6736(13)61489-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart E. G. (2004). Art therapy and neuroscience blend: Working with patients who have dementia. Art Therapy, 21, 148-155. [Google Scholar]
- Strawbridge W. J., Wallhagen M. I., Cohen R. D. (2002). Successful aging and wellbeing: Self-rated compared with Rowe and Kahn. The Gerontologist, 42, 727-733. [DOI] [PubMed] [Google Scholar]
- Tesky V. A., Sahlender S., Koebe T., Witte V., Floel A., Pantel J. (2014). Development of cognition and mood in participants of the AKTIVA-MCI intervention training. Alzheimer’s & Dementia, 10, P612. [Google Scholar]
- Theou O., Stathokostas L., Roland K. P., Jakobi J. M., Patterson C., Vandervoort A. A., Jones G. R. (2011). The effectiveness of exercise interventions for the management of frailty: A systematic review. Journal of Aging Research, 2011, Article 569194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tse A. C. Y., Wong T. W. L., Lee P. H. (2015). Effect of low-intensity exercise on physical and cognitive health in older adults: A systematic review. Sports Medicine, 1, 37. doi: 10.1186/s40798-015-0034-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tse M. M., Vong S. K., Ho S. S. (2012). The effectiveness of an integrated pain management program for older persons and staff in nursing homes. Archives of Gerontology and Geriatrics, 54, e203-e212. doi: 10.1016/j.archger.2011.04.015 [DOI] [PubMed] [Google Scholar]
- Uttley L., Scope A., Stevenson M., Rawdin A., Buck E. T., Sutton A., . . . Wood D. (2015). Systematic review and economic modelling of the clinical effectiveness and costeffectiveness of art therapy among people with non-psychotic mental health disorders. Health Technology Assessment, 19(18), 1-120. doi: 10.3310/hta19180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Katwyk P. T. (2012). The changing workforce demographics in Asia Pacific: A diversity of work and retirement trends. In Borman W. C., Hedge J. W. (Eds.), The Oxford handbook of work and aging. Oxford, UK: Oxford University Press. doi: 10.1093/oxfordhb/9780195385052.013.0058 [DOI] [Google Scholar]
- Viña J., Rodriguez-Mañas L., Salvador-Pascual A., Tarazona-Santabalbina F. J., Gomez-Cabrera M. C. (2016). Exercise: The lifelong supplement for healthy ageing and slowing down the onset of frailty. The Journal of Physiology, 594, 1989-1999. doi: 10.1113/JP270536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viola L. F., Nunes P. V., Yassuda M. S., Aprahamian I., Santos F. S., Santos G. D., . . . Forlenza O. V. (2011). Effects of a multidisciplinar cognitive rehabilitation program for patients with mild Alzheimer’s disease. Clinics, 66, 1395-1400. doi: 10.1590/s1807-59322011000800015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2011). Global health and aging. Washington DC, US: National Institute on Aging, National Institutes of Health. [Google Scholar]
- Zannas A. S. (2016). Editorial perspective: Psychological stress and epigenetic aging—What can we learn and how can we prevent? Journal of Child Psychology and Psychiatry, 57, 674-675. doi: 10.1111/jcpp.12535 [DOI] [PubMed] [Google Scholar]


