Abstract
Background:
Physical activity is recommended for kidney transplant recipents as it may improve outcomes including mortality, exercise capacity, muscle strength, and health-related quality of life.
Objective:
The objective of this study was to examine accelerometer-based physical activity and sedentary time profiles among kidney transplant recipients and examine possible demographic and clinical correlates of physical activity and sedentary time.
Design:
Cross-sectional.
Setting:
Edmonton, Alberta, Canada.
Patients:
Kidney transplant recipients were recruited (N = 1,284) from the Northern Alberta Renal Program’s Nephrology Information System database (1993-2016).
Measurements:
Participants wore an ActiGraph GT3X+ accelerometer on their hip during waking hours for seven consecutive days.
Methods:
Kidney transplant recipients (1993-2016) recruited from the Northern Alberta Renal Program’s Nephrology Information System database wore an accelerometer and completed a self-reported questionnaire. Multiple linear regression was used to determine associations between activity level, demographic, and clinical characteristics.
Results:
Participants’ (n = 133; 11% response rate) mean age (SD) was 58 (14) years and 56% were female. Mean total sedentary time was 9.4 (1.4) hours per day; total moderate-to-vigorous physical activity (MVPA) time was 20.7 (19.6) minutes per day. MVPA was significantly associated with age where each additional year was associated with 0.48 fewer min/day (ie, ~30 seconds) (unstandardized beta: B = −0.48 min/day, 95% confidence interval [95% CI]: −0.75, −0.22). Sedentary time was significantly associated with age (B = 1.0 min/day, 95% CI: 0.03, 1.9), body mass index (B = 2.7 min/day, 95% CI: 0.2, 5.13), education (B = 39.1 min/day, 95% CI: 12.3, −65.8), and inversely associated with income (B = −44.9 min/day, 95% CI: −73.1, −16.8).
Limitations:
Limitations include the cross-sectional design, poor response rate, and limited generalizability of the results.
Conclusions:
Kidney transplant recipients showed high volumes of sedentary time and low volumes of health-enhancing physical activity. Understanding correlates of these behaviors may aid in the development of interventions to favorably change these behaviors.
Keywords: physical activity, sedentary behavior, accelerometer, kidney transplantation
Abrégé
Contexte:
L’activité physique est recommandée aux receveurs d’une greffe rénale puisqu’elle peut améliorer leur santé — augmentation de la tolérance à l’effort, de la force musculaire et de la qualité de vie liée à l’état de santé — et limiter les issues indésirables, notamment la mortalité.
Objectif:
L’objectif était double: caractériser l’activité physique et le profil de sédentarité des receveurs d’une greffe rénale avec un accéléromètre, et analyser les possibles corrélations démographiques et cliniques de l’activité physique et du comportement sédentaire.
Type d’étude:
Étude transversale
Cadre:
Edmonton, en Alberta (Canada).
Sujets:
Des patients ayant reçu une greffe rénale entre 1993 et 2016 (n = 1284) et recrutés dans la base de données du système d’information en néphrologie du Northern Alberta Renal Program (NARP).
Mesures:
Les participants portaient un accéléromètre Actigraph GT3X+ à la hanche durant les heures d’éveil pour sept jours consécutifs.
Méthodologie:
Les receveurs d’une greffe rénale (1993 à 2016) recrutés dans la base de données du système d’information en néphrologie du NARP ont porté un accéléromètre et rempli un questionnaire d’auto-déclaration. Une régression linéaire multiple a été employée pour établir les associations entre le niveau d’activité physique et les données démographiques et cliniques des patients.
Résultats:
Les participants (n = 133; taux de réponse de 11 %), dont 56 % étaient des femmes, étaient âgés de 58 ans en moyenne (écart-type [É-T]: 14 ans). La période de sédentarité s’élevait en moyenne à 9,4 heures par jour (É-T: 1,4 heure), alors que la période moyenne d’activité physique modérée à vigoureuse (APMV) s’établissait à 20,7 minutes par jour (É-T: 19,6 minutes). L’APMV a été associée de façon significative à l’âge du patient, où chaque année additionnelle en âge a correspondu à une réduction de 0,48 minute par jour (environ 30 sec.) de l’APMV (bêta non normalisé [ß] = -0,48 min/jour; 95% IC: -0,75 à -0,22). Les comportements sédentaires ont été associés de façon significative à l’âge (ß = 1,0 min/jour, 95% IC: 0,03 à 1,9), à l’IMC (ß = 2,7 min/jour, 95% IC: 0,2 à 5,13), au niveau de scolarité (ß = 39,1 min/jour, 95% IC: 12,3 à -65,8), et inversement associés au revenu du patient (ß = -44,9 min/jour, 95% IC: -73,1 à -16,8).
Limites:
La généralisation des résultats est limitée par la nature transversale de l’étude et par le faible taux de réponse.
Conclusion:
Les receveurs d’une greffe rénale sont largement sédentaires et pratiquent peu d’activité physique ayant un effet bénéfique sur leur santé. La compréhension des corrélations de ces comportements pourrait faciliter le développement d’interventions visant à les modifier favorablement.
What was known before
Previous interventions have found physical activity to be effective and safe for kidney transplant recipients. However, less is known about sedentary time and light intensity activities and the factors associated with activity and sedentary behaviours.
What this adds
This study examines sedentary time and light intensity activity among kidney transplant recipients. Furthermore, in this study, activity and sedentary time was examined using device-based methods (i.e., accelerometer) while allows for a more precise and accurate measure of these behaviours.
Introduction
Physical activity is recommended for kidney transplant recipents as it may improve outcomes including mortality, exercise capacity, muscle strength, and health-related quality of life.1,2 Despite these benefits, physical activity among kidney transplant recipients has been reported in several studies to be low.3,4
In the general population, excessive amounts of sedentary behavior has deleterious health consequences that are distinct from the beneficial effects of physical activity, and include an increased risk of mortality, some cancers, stroke, diabetes, and depression.5,6 Less is known about associations between sedentary behavior and health outcomes in the kidney transplant population. For individuals who have had a kidney transplant, high amounts of sedentary behavior have been associated with increased mortality.2 Sedentary behaviors are activities low in energy expenditure, such as sitting or reclining, and are in the energy-expenditure range of 1.0 to 1.5 metabolic equivalents (METs) and is distinct from physical inactivity (ie, performing insufficient amounts of moderate-to-vigorous physical activity [MVPA]).7,8
Light-intensity physical activity and sedentary time, which together may make up more than 95% of an individual’s total day, are difficult to measure reliably by questionnaire and often lead to inaccurate inferences about activity behaviors and associated outcomes.9 Accelerometers now provide a means for more precise and, accurate estimates of sedentary time and physical activity. A recent systematic review and meta analysis by Berben and colleagues10 examining correlates and outcomes of low physical activity post transplant reported few studies in the area of solid organ transplant recipients. These studies relied primarily on self-reported estimates of physical activity, and the authors recommended researchers should use activity monitors to document physical activity. A follow-up commentary to the review by Bittermann11 indicated the overall prevalence of low physical activity after solid organ transplant remains unknown, and future research using more objective measurements will advance the science.
To date, few studies have reported objective (device-based) physical activity and sedentary time estimates from kidney transplant recipients, and these studies are limited by very small sample sizes (<25 participants).12,13 Few studies have explored factors related to physical activity and/or sedentary behavior, and no studies have examined factors related to accelerometer-based sedentary behavior and physical activity. Such information can inform the development of interventions to target factors associated with low physical activity and high sedentary time. In this study, accelerometers were used to assess physical activity and sedentary time among a sample of kidney transplant recipients and we describe the sociodemographic and clinical factors associated with activity and sedentary time.
Materials and Methods
Adults kidney transplant recipients with a functioning graft at least 12 months post transplantation were recruited at a single center in Alberta, Canada, using the Nephrology Information System (NIS) database. At the time of recruitment, the NIS database had a record of approximately 1,284 kidney transplant recipients. All kidney transplant recipients in the database were sent a letter to participate in the study. Interested participants were prompted to email or telephone the study research coordinator who assessed participant eligibility. Eligibility criteria included (1) functioning kidney transplant 12 months post transplantation (due to more severe side effects immediately after transplant), including recipients of combined organ transplant (eg, kidney-pancreas); (2) age ≥18 years; (3) ability to read and understand English; (4) willingness to wear an activity monitoring device on the hip for seven consecutive days (during waking hours); and (5) residing in Alberta, Canada.
Study participants were mailed a study package including an ActiGraph GT3X+ accelerometer (ActiGraph, LLC, Pensacola, Florida), along with an instructional pamphlet describing how to use the accelerometer, an accelerometer diary to record non-wear periods, and a survey assessing sociodemographic characteristics. At the end of the 7-day accelerometer monitoring period, participants returned their signed consent form, completed survey and diary, and accelerometer. This study was approved by the University of Alberta Health Research Ethics Board (ID: Pro00063054) and the Athabasca University Research Ethics Board (ID: 22180).
Measures
Clinical information including age, sex, body mass index (BMI), transplant date, type of donor (living vs. deceased), and laboratory data (last available clinic/lab work at the time of the study) including estimated glomerular filtration rate (eGFR), hemoglobin, serum albumin, and comorbidities (diabetes, cardiovascular disease, stroke/transient ischemic attack [TIA], peripheral vascular disease, and amputation) were obtained from the database. Other information including smoking (current smoker) and sociodemographic (eg, marital status, education, employment, income) factors were collected via self-report survey.
Physical activity and sedentary time were assessed by the ActiGraph GT3X+ accelerometer (Actigraph, LLC, Pensacola, Florida). These accelerometers (4 cm × 3 cm × 1.5 cm) are worn on an elasticized band around the waist. Commonly accepted activity count cutoffs were used to differentiate between moderate and vigorous intensity physical activity (counts/min ≥1952) from light intensity activity (100-1951 counts/min) and sedentary time (<100 counts/min).14 Data were recorded in 60-second epochs. Nonwear time was defined as intervals of at least 60 consecutive minutes of zero counts, with allowance for up to 2 minutes of observations of <50 counts per minute within the nonwear interval. To be considered valid, days of data collection required at least 600 minutes (10 hours) of wear time and no excessive counts (>20,000 counts per minute).
To account for non-wear periods, participants are asked to record when they put on and remove the device in an accelerometer diary.
Statistical Analysis
Descriptive statistics were used to examine the sociodemographic and clinical characteristics of the sample, as well as average daily light intensity physical activity, MVPA, sedentary time, and steps. One linear regression model was fitted for each accelerometer outcome (ie, MVPA, light PA, steps, sedentary time) for a total of four models. Sociodemographic variables included age, sex, marital status (not married vs. married or common law), education (less than college/university vs. at least college/university/trade), employment (not employed vs. employed part or full time), and income (<$60,000 vs. >$60,000). The clinical predictors included years since transplant, eGFR, hemoglobin, serum albumin, BMI, and comorbidities. To prevent overfitting the models, independent variables were included in the models that were associated (P < .20) (analysis of variance [ANOVA] for categorical independent variables, bivariate correlations for continuous independent variables) with the dependent variable. All models were adjusted for accelerometer weartime. All models were generated using SPSS Version 24.0 (SPSS, Chicago, IL).
Results
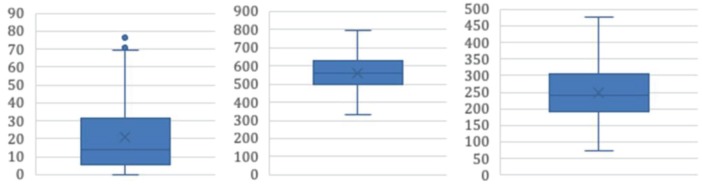
Demographic, behavioural, and clinical variables describing the sample are found in Tables 1 and 2. Study invitation letters were mailed to all 1209 individuals in the registry. Of these individuals, 182 contacted the study team and expressed interest in participating in the study. Ten individuals were not eligible due to orthopedic conditions precluding physical activity (n = 6) and not willing to wear the accelerometer (n = 4). Of the 172 individuals who received the study materials, 23 did not return the accelerometer or did not wear the accelerometer, 11 decided not to participate, and 5 did not return a completed survey. The final response rate was 11% (133/1209). The mean (SD) age was 58.4 (14.3) years, 56% female, and the average time since transplant was 27.2 (21.5) months. To examine the generalizability of our sample, we compared study participants (n = 141) (ie, responders) to those in the registry who did not participate in the study (n = 1052) (ie, nonresponders) on available data and found no significant differences between the groups on age (P = .19) and gender (P = .07). Our sample were 2 years closer to their transplant date compared to nonresponders (9.5 vs. 11.4, P < .01). On average, participants were overweight with a BMI of 27.6 (5.4) kg/m2. Participants wore their accelerometer, on average, 14 (1.3) hr/day for 6.5 (1.1) days. The distribution of MVPA, light intensity activity, and sedentary time are shown in Figure 1. Mean values for these variables shown in Figure 2.
Table 1.
Sociodemographic and Clinical Characteristics.
| Characteristic | No. of respondents | % | Mean (SD) |
|---|---|---|---|
| Demographic | |||
| Sex | |||
| Female | 74 | 55.6 | |
| Age | 58.4 (14.3) | ||
| Marital status | |||
| Married/common law | 104 | 78.2 | |
| Not married | 29 | 21.8 | |
| Ethnicity | |||
| Caucasian | 116 | 87.2 | |
| Other | 17 | 12.8 | |
| Education | |||
| College/university | 80 | 60.2 | |
| Less than college/university | 53 | 39.8 | |
| Annual family income | |||
| ≤$60,000 | 50 | 37.6 | |
| >$60,000 | 83 | 62.4 | |
| Employment status | |||
| Working full or part time | 55 | 41.1 | |
| Not working | 78 | 58.6 | |
| Clinical | |||
| Body mass index (kg/m2) | 27.6 (5.4) | ||
| Normal weight (<25 kg/m2) | 42 | 31.6 | |
| Overweight/obese (>25 kg/m2) | 91 | 68.4 | |
| Years since transplant | 9.5 (7.6) | ||
| Type of transplant | |||
| Living donor | 67 | 50.4 | |
| Deceased donor | 66 | 49.6 | |
| Comorbidity history | |||
| Angina | 12 | 9.0 | |
| Heart attack | 13 | 9.8 | |
| Stroke | 4 | 3.0 | |
| Diabetes mellitus | 47 | 35.3 | |
| Hypertension | 108 | 81.2 | |
| Hypercholesteremia | 61 | 45.9 | |
| Peripheral vascular disease | 11 | 8.3 | |
| Cancer | 30 | 22.6 | |
| Amputation | 3 | 2.3 | |
| Current smoker | 7 | 5.3 | |
| Glomerular filtration rate (eGFR) (mL/min/1.73m2) | 53.8 (18.4) | ||
| Hemoglobin (g/L) | 131.3 (20.3) | ||
| Serum albumin (g/L) | 40.0 (4.6) | ||
Table 2.
Descriptive Statistics for Accelerometer-Based Physical Activity and Sedentary Time in Kidney Transplant Recipients (N = 133).
| Variable | Mean (SD) | Range | Interquartile range |
|---|---|---|---|
| Valid days | 6.5 (1.1) | 7 | 1.0 |
| Accelerometer wear time | |||
| Minutes/day | 833.6 (77.5) | 406.3 | 113.4 |
| Light-intensity physical activity | |||
| Minutes/day | 250 (83.4) | 405.4 | 115.7 |
| Moderate-intensity physical activity | |||
| Minutes/day | 20.3 (19.4) | 76.3 | 25.6 |
| Vigorous-intensity physical activity | |||
| Minutes/day | 0.4 (1.5) | 9.7 | 0.0 |
| MVPAa | |||
| Minutes/day | 20.7 (19.6) | 77.3 | 25.6 |
| Minutes/day in 10-minute bouts | 5.7 (9.8) | 59.9 | 8.8 |
| Percent achieving MVPA guidelinesb | 36.8% | — | |
| Steps per day | 5464 (2913) | 14 228 | 3545 |
| Sedentary time | |||
| Hours/day | 9.4 (1.4) | 7.6 | 2.1 |
| Hours/day in 30-minute bouts | 2.9 (1.5) | 7.2 | 2.2 |
Note. MVPA = moderate-to-vigorous physical activity.
Moderate and vigorous minutes combined.
Engage in moderate-intensity physical activity for a minimum of 150 minutes of MVPA a week.
Figure 1.
Box and whisker plot demonstrating the distribution of MVPA (left), sedentary time (center), and light activity (right) across the sample.
Note. MVPA = moderate-to-vigorous intensity physical activity.
Figure 2.
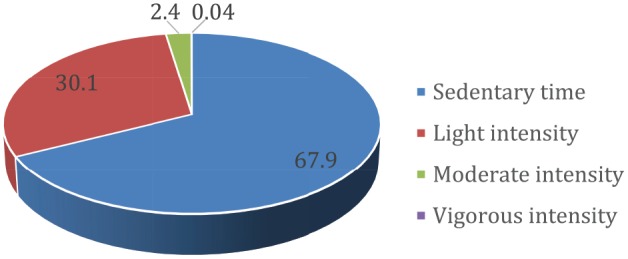
Kidney transplant recipients’ percentage of time spent in sedentary, light-intensity, moderate-intensity, and vigorous-intensity behaviors.
Physical Activity
Mean MVPA per day was 20.7 (19.6) min/day. For MVPA accumulated in 10-minute bouts, participants engaged in only 5.7 min/day of MVPA (9.8). All linear regression models indicating associations are located in Table 3. MVPA was significantly associated with age where each additional year was associated with 0.48 fewer min/day (ie, ~30 seconds) (unstandardized beta: B = −0.48 min/day, 95% confidence interval (95% CI): −0.75, −0.22). Participants accumulated 250 (83.4) min/day of light intensity physical activity which equates to just over 4 hr/day. Those participants with at least a college/university education reported 37.4 fewer min/day of light intensity physical activity compared to participants with less than a college/university education (B = −37.4 min/day, 95% CI: −62.24, −12.56), while participants earning >$60,000 per year reported 40.33 more min/day compared to those earning <$60,000 per year (B = 40.33 min/day, 95% CI: 12.41, 68.25). A one-point increase in BMI was associated with 2.4 fewer minutes of light intensity activity (B = −2.42 min/day, 95% CI: −4.75, −0.09).
Table 3.
Sociodemographic and Clinical Correlates of Accelerometer-Based Activity Variables.
| Model | B (95% CI) | P | Model | B (95% CI) | P |
|---|---|---|---|---|---|
| MVPA | Steps | ||||
| Age | −0.48 (−0.75, −0.22) | .000* | Age | −58.95 (−94.46, −23.44) | .001* |
| eGFR | 0.06 (−0.11, 0.24) | .458 | eGFR | 10.94 (−11.84, 33.74) | .344 |
| Albumin | 0.43 (−0.23, 1.08) | .198 | Albumin | 49.74 (−40.65, 140.14) | .278 |
| Hemoglobin | 0.10 (−0.07, 0.27) | .231 | BMI | −67.6 (−145.87, 10.68) | .090 |
| Employmenta | 0.11 (−7.75, 7.98) | .977 | >2 chronic diseases | −287.69 (−1183.51, 608.13) | .526 |
| Incomeb | 4.61 (−1.88, 11.1) | .162 | Employment | 377.33 (−714.41, 1469.07) | .495 |
| Income | 1085 (157.55, 2013.67) | .022* | |||
| Light PA | Sedentary time | ||||
| Age | −0.66 (−1.71, 0.40) | .220 | Age | 0.96 (0.03, 1.90) | .043* |
| eGRF | 0.17 (−0.51, 0.85) | .619 | Albumin | −2.50 (−5.32, 0.32) | .127 |
| Albumin | 1.78 (−0.91, 4.47) | .193 | BMI | 2.66 (0.20, 5.13) | .035* |
| BMI | −2.42 (−4.75, −0.09) | .042* | >2 chronic diseases | 4.65 (−23.71, 33.02) | .746 |
| ≥2 chronic diseases | −6.28 (−32.86, 20.30) | .641 | Education | 39.06 (12.29, 65.83) | .005* |
| Employment | −4.54 (−36.92, 27.85) | .782 | Gender | 12.63 (−13.43, 38.69) | .230 |
| Educationc | −37.40 (−62.24, −12.56) | .003* | Income | −44.93 (−73.08, −16.77) | .002* |
| Income | 40.33 (12.41, 68.25) | .005* |
Note. MVPA reported in minutes per day. Sedentary time reported in hours per day. All regression models were adjusted for accelerometer wear time. CI = confidence interval; MVPA = moderate-to-vigorous intensity physical activity; PA = physical activity; eGFR = estimated glomerular filtration rate; BMI = body mass index.
Not working versus working part or full time.
Less than college/university versus completed college/university education.
<$60,000 versus >$60,000.
P < .05.
Participants averaged 5464 (2913) steps/day. A one-year increase in age was associated with 59 fewer steps (B = −58.95, 95% CI: −94.46, −23.44) per day, while participants earning >$60,000 per year reported 1085 more steps compared to those earning less (B = −1085, 95% CI: −157.55, −2013.67).
Sedentary Time
Participants recorded 9.4 (1.4) hr/day of total sedentary time (562 min/day) and spent 173.4 min/day in sedentary bouts of at least 30 minutes. Sedentary time was significantly associated with age where each additional year was associated with 1 more min/day (B = 1.0 min/day, 95% CI: 0.03, 1.90). A one-point increase in BMI was associated with 2.66 more min/day of sedentary time (B = 2.66 min/day, 95% CI: 0.20, 5.13). Those participants with at least a college/university education reported 39.06 more min/day of sedentary time compared to participants with less than a college/university education (B = 39.06 min/day, 95% CI: 12.29, −65.83), while participants earning >$60,000 per year reported 45 fewer min/day of sedentary time compared to those earning <$60,000 per year (B = −44.93 min/day, 95% CI: −73.08, −16.77).
Discussion
Although several studies have examined accelerometer assessed physical activity and sedentary time in other chronic disease groups (eg, cancer, diabetes), few have examined kidney transplant recipients. Studies have used a variety of measurement devices, and different operationalizations of physical activity have been implemented. In one cross-sectional study (n = 24), recipients were engaging in 126 min/day of habitual physical activity (ie, light, moderate, and vigorous intensity combined assessed by the SenseWear Armband) and 564 min/day of sedentary time (9.4 hr/day).15 In a prospective study (n = 24), recipients accumulated ~90 min/day of MVPA (assessed by the SenseWear Armband) 12 months after transplantation.13 In another study, 23 kidney transplant recipients wore a DynaPort activity monitor and engaged in 311 min/day of activity time, 205 min/day of standing time, 288 min/day of sitting time, and 86 min/day of lying time.12 Activity time was defined as the sum of walking and standing time. Beddhu et al16 used the National Health and Nutrition Examination Survey (NHANES) and identified 383 participants with chronic kidney disease who wore an earlier version of the ActiGraph accelerometer. These participants engaged in 7 min/day of MVPA and 511 min/day (8.5 hr/day) of sedentary time. Although it is difficult to compare these findings to our physical activity and sedentary time estimates given the varying estimates, definitions of activity, and assessment devices used, the previous studies that used an objective measure recorded substantially higher MVPA compared to our study that suggested 21 min/day. However, there is consistency in sedentary time across the studies when we compare our sedentary time estimate (9.4 hr/day) to the sum of the sedentary domains of standing, sitting, and lying time variables (9.7 hr/day and 8.5 hr/day).
We also reported accelerometer-based light intensity physical activity and step counts. We found that kidney transplant recipients averaged 250 min/day (~4 hr/day) of light intensity physical activity. Other studies have yielded similar results. For example, Beddhu et al16 reported kidney transplant recipients engaged in approximately 185 min/day (~3 hr/day) of light intensity activity. Our study found recipients took approximately 5500 steps/day. Several studies have reported kidney transplant recipients engage in anywhere from ~4000 to ~9700 steps/day.12,13,15,17 Inconsistency in step counts across these studies may be due to a variety of factors including type of device used (step pedometer vs. accelerometer) and varying differences in time since transplant across samples. However, these studies all suggest kidney transplant recipients engage in low amounts of walking. A review by Tudor-Locke recommended individuals with disability or chronic illness engage in 6500 to 8500 steps/day.18
Few studies have examined correlates of physical activity and sedentary behaviors in the solid organ transplant context.10 Our study is one of the first to examine correlates of accelerometer-based physical activity, light intensity activity, steps, and sedentary time in kidney transplant recipients. While MVPA was inversely associated with age, steps/day was inversely associated with age and positively associated with income. Light intensity activity was positively associated with education and income, and inversely associated with BMI. Sedentary time was positively associated with age, BMI and education, and inversely associated with income. These findings suggest that further exploration of the barriers to reducing sedentary time for older patients and those with higher BMI is needed; however, this recommendation is not unique to the population of kidney transplant recipients. Of note, our findings suggesting more highly educated participants had higher sedentary time is not consistent with research often suggesting higher education is inversely associated with sedentary time19 and positively associated with MVPA.20 It is possible that participants with higher education had more opportunities to take time off from employment (eg, sick leave). No clinical variables were significantly associated with activity or sedentary time. While previous work has indicated individuals with chronic kidney disease with low eGFR have a higher likelihood of being sedentary,21 our study found no associations between sedentary time, physical activity, and eGFR. It is worth noting the Glavinovic study analyzed eGFR as a categorical variable (>60, 60-45, <45) while our study analyzed eGFR as a continuous variable.
Limitations of this study include the cross-sectional design, low recruitment rate (11%), and generalizability, given data collection occurred at a single center and the majority of participants were Caucasian with a relatively high income and education. While study participants were not significantly different than nonresponders on age and gender, they were significantly more proximal to their transplant date compared to nonresponders. Furthermore, the accelerometer used in this study does not distinguish between sitting and stationary standing (ie, sedentary time may include periods of standing still as well as sitting) and may undercount steps in those individuals who walk slow.22 Our study only included transplant recipients who were at least one-year post transplant. It is likely that recipients who are immediately post-transplant are less active and more sedentary, and therefore, time since transplantation should still be an important factor to consider in the rehabilitation context. Finally, our study only examined potential sociodemographic and clinical correlates of activity and sedentary behaviors. There are likely other correlates of these behaviors in this population and may include social cognitive (eg, self-efficacy, attitude) and neighborhood/environment (eg, access to parks and green space) correlates. Future research should utilize more rigorous study designs (eg, prospective studies or interventions) and recruit larger and more representative samples of kidney transplant recipients. Future research should also use devices with inclinometers to better able differentiate between sitting and standing (eg, activPAL).
Few studies to date have examined activity and sedentary behaviors among kidney transplant recipients using device-based measures. In this study, we report that the majority of kidney transplant recipients that were more than 12 months post-transplant were accumulating low amounts of MVPA (~20 min/day) and high amounts of sedentary time (exceeding 9 hr/day). We also reported correlates of different physical activity behaviors and sedentary time in this population. Interventions need to be developed to facilitate activity and reduce sedentary time in this population.
Footnotes
List of Abbreviations: BMI, body mass index; 95% CI, 95% confidence interval; METs, metabolic equivalents; MVPA, moderate-to-vigorous physical activity; NIS, Nephrology Information System.
Ethics Approval and Consent to Participate: This study was approved by the University of Alberta Health Research Ethics Board (ID: Pro00063054) and the Athabasca University Research Ethics Board (ID: 22180). All participants provided written consent to participating in this study.
Consent for Publication: All co-authors reviewed this final manuscript and consented to its publication.
Availability of Data and Materials: Data and materials may be made available upon written request to the corresponding author. Reasonable requests for data access will be assessed in consultation with the appropriate Research Ethics Boards.
Author Contributions: J.K.V. provided study funding, participated in the study conception, research design, writing of the paper, performance of the research, and in data analysis. S.S. participated in the study conception, editing of the paper, and providing access to the Nephrology Information Database. S.T., N.N.L., and K.W. participated in the research design and editing of the paper. S.J. participated in the study conception, research design, and editing of the paper. I.J. extracted database variables. T.B. processed the accelerometer data and participated in the editing of the paper.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Jeff K. Vallance  https://orcid.org/0000-0003-1135-8772
https://orcid.org/0000-0003-1135-8772
Ngan N. Lam  https://orcid.org/0000-0002-0129-7091
https://orcid.org/0000-0002-0129-7091
References
- 1. Takahashi A, Hu SL, Bostom A. Physical activity in kidney transplant recipients: a review. Am J Kidney Dis. 2018;72(3):433-443. doi: 10.1053/j.ajkd.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 2. Zelle DM, Klaassen G, van Adrichem E, Bakker SJL, Corpeleijn E, Navis G. Physical inactivity: a risk factor and target for intervention in renal care. Nat Rev Nephrol. 2017;13(3):152-168. doi: 10.1038/nrneph.2016.187. [DOI] [PubMed] [Google Scholar]
- 3. Beddhu S, Baird BC, Zitterkoph J, Neilson J, Greene T. Physical activity and mortality in chronic kidney disease (NHANES III). Clin J Am Soc Nephrol. 2009;4(12):1901-1906. doi: 10.2215/CJN.01970309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. vandenHam EC, Kooman JP, Schols AM, et al. Similarities in skeletal muscle strength and exercise capacity between renal transplant and hemodialysis patients. Am J Transplant. 2005;5(8):1957-1965. doi: 10.1111/j.1600-6143.2005.00944.x. [DOI] [PubMed] [Google Scholar]
- 5. Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123-132. doi: 10.7326/M14-1651. [DOI] [PubMed] [Google Scholar]
- 6. Vallance JK, Winkler EA, Gardiner PA, Healy GN, Lynch BM, Owen N. Associations of objectively-assessed physical activity and sedentary time with depression: NHANES (2005-2006). Prev Med. 2011;53(4-5):284-288. doi: 10.1016/j.ypmed.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 7. Tremblay MS, Aubert S, Barnes JD, et al. Sedentary Behavior Research Network (SBRN)—terminology consensus Project process and outcomes. Int J Behav Nutr Phys Act. 2017;14:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sedentary Behaviour Research Network. Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours.” Appl Physiol Nutr Metab. 2012;37(3):540-542. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 9. Ainsworth BE, Caspersen CJ, Matthews CE, Masse LC, Baranowski T, Zhu W. Recommendations to improve the accuracy of estimates of physical activity derived from self report. J Phys Act Health. 2012;9(suppl 1):S76-S84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Berben L, Engberg SJ, Rossmeissl A, et al. Correlates and outcomes of low physical activity posttransplant: a systematic review and meta-analysis. Transplantation. 2019;103:679-688. doi: 10.1097/TP.0000000000002543. [DOI] [PubMed] [Google Scholar]
- 11. Bittermann T. Physical activity after solid organ transplantation: comprehensive guidance is needed to advance future research efforts. Transplantation. 2019;103:666-667. doi: 10.1097/TP.0000000000002544. [DOI] [PubMed] [Google Scholar]
- 12. Carvalho EV, Reboredo MM, Gomes EP, et al. Physical activity in daily life assessed by an accelerometer in kidney transplant recipients and hemodialysis patients. Transplant Proc. 2014;46(6):1713-1717. doi: 10.1016/j.transproceed.2014.05.019. [DOI] [PubMed] [Google Scholar]
- 13. Dontje ML, deGreef MH, Krijnen WP, et al. Longitudinal measurement of physical activity following kidney transplantation. Clin Transplant. 2014;28(4):394-402. doi: 10.1111/ctr.12325. [DOI] [PubMed] [Google Scholar]
- 14. Freedson PS, Melanson E, Sirard J. Calibration of the computer science and applications, inc. Med Sci Sports Exerc. 1998;30(5):777-781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 15. Masajtis-Zagajewska A, Muras K, Nowicki M. Effects of a structured physical activity program on habitual physical activity and body composition in patients with chronic kidney disease and in kidney transplant recipients. Exp Clin Transplant. 2019;17:155-164. doi: 10.6002/ect.2017.0305. [DOI] [PubMed] [Google Scholar]
- 16. Beddhu S, Wei G, Marcus RL, Chonchol M, Greene T. Light-intensity physical activities and mortality in the United States general population and CKD subpopulation. Clin J Am Soc Nephrol. 2015;10(7):1145-1153. doi: 10.2215/CJN.08410814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Raymond J, Johnson ST, Diehl-Jones W, Vallance JK. Walking, sedentary time and health-related quality of life among kidney transplant recipients: an exploratory study. Transplant Proc. 2016;48(1):59-64. doi: 10.1016/j.transproceed.2015.12.022. [DOI] [PubMed] [Google Scholar]
- 18. Tudor-Locke C, Craig CL, Aoyagi Y, et al. How many steps/day are enough? For older adults and special populations. Int J Behav Nutr Phys Act. 2011;8:80. doi: 10.1186/1479-5868-8-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Koyanagi A, Stubbs B, Vancampfort D. Correlates of sedentary behavior in the general population: a cross-sectional study using nationally representative data from six low- and middle-income countries. PLoS One. 2018;13(8). doi: 10.1371/journal.pone.0202222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Droomers M, Schrijvers CTM, Mackenbach JP. Educational level and decreases in leisure time physical activity: predictors from the longitudinal GLOBE study. J Epidemiol Community Health. 2001;55(8):562-568. doi: 10.1136/jech.55.8.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Glavinovic T, Ferguson T, Komenda P, et al. CKD and sedentary time: results from the Canadian Health Measures Survey. Am J Kidney Dis. 2018;72(4):529-537. doi: 10.1053/j.ajkd.2018.03.031. [DOI] [PubMed] [Google Scholar]
- 22. Hergenroeder AL, BaroneGibbs B, Kotlarczyk MP, Kowalsky RJ, Perera S, Brach JS. Accuracy of objective physical activity monitors in measuring steps in older adults. Gerontol Geriatr Med. 2018;4. doi: 10.1177/2333721418781126. [DOI] [PMC free article] [PubMed] [Google Scholar]