Abstract
Propolis is one of the bee products that widely used in health therapy. However, there has no study evaluating the developmental toxicity of propolis. This study was aimed to analyze the effect of propolis administration during pregnancy on fetal development. The pregnant mice were divided into five groups including control group (Tween 80 1%), low-dose (380 mg/kg b.wt.) and high-dose (1400 mg/kg b.wt.) of water extract of propolis from Banten (WEB), and low-dose (380 mg/kg b.wt.) and high-dose (1400 mg/kg b.wt.) of ethanol extract of propolis from South Sulawesi (EES). Propolis was administered for 18 days of gestation and then sacrificed to analyze the fetal development by examining external and skeletal abnormalities. The histopathological examination of placenta was also conducted. The result showed both low-dose groups did not inhibit fetal development. However, the high-dose of EES significantly reduced the weight, crown-rump of fetuses and increased the number of resorption (p < 0.05). Fetal weight was the only significantly reduced parameter of fetal growth in the highdose group of WEB (p < 0.05). The histopathological examination of placenta showed a reduction of labyrinth development in both high-dose groups. Dose of 380 mg/kg dose of Indonesian propolis is relatively safe for consumption during pregnancy.
Keywords: Developmental biology, Toxicology, Natural product chemistry, Food science, Nutrition, Pharmaceutical science, Teratogenicity, Stingless bee propolis
Developmental biology; Toxicology; Natural product chemistry; Food science; Nutrition; Pharmaceutical science; Teratogenicity; Stingless bee propolis
1. Introduction
The thalidomide case in the late 1950s and early 1960s which caused 8000 malformed babies leads to highly consider the safety evaluation of drug use during pregnancy (Tyl and Marr, 2016). However, the focus is currently not only on drugs but also natural products. Some natural products which are commonly consumed, including ginseng, ginger, and ginko biloba, reported to inhibit fetal growth (Mohammed et al., 2016). Another surprising study by Park et al. (2009) found the administration of green tea increased cyclophosphamide-induced teratogenesis in mice. In addition, fenugreek and asparagus also may retard fetal growth (Goel et al., 2006; Taloubi et al., 2013).
Propolis is a natural product widely used to support the treatment of some diseases. Propolis is produced by bees from resins and beeswax and plays an important role in colony-level immunity (Bankova et al., 2000). Propolis varies greatly in the chemical composition. About 300 chemical compounds have been reported contained in propolis (Huang et al., 2014). However, it is confirmed that propolis has broad spectrum biological activities, including antibacterial, antitumor, antiinflammatory, antifungal, citotoxic, immunomodulatory and antioxidant properties (Lotfy, 2006; Król et al., 2013; Kalsum et al., 2017).
Unfortunately, there has no study investigating the effect of propolis administration on fetal development, where its biological activities may affect. The antitumor activity of natural product could inhibit embryonic cells development (Mohammed et al., 2016), while propolis has been reported to possess that activity (Suzuki et al., 2002; Oršolić; Bašić, 2003; Oršolic et al., 2005; Xuan et al., 2014). However, the chemical composition of propolis depends on location, season, bee species, and method of preparation (Salatino et al., 2005; Sun et al., 2015). Therefore, this study was aimed to investigate the effect of propolis administration during pregnancy on fetal development in mice for the first time. There were two types of propolis used in the present study, including water extract of propolis from Banten and ethanol extract of propolis from South Sulawesi, Indonesia.
2. Materials and method
2.1. Sample preparation
Raw samples were obtained from CV. Nutrima, Bogor, Indonesia and stored at -5 °C until used. All samples were harvested in 2016. Propolis from Banten was Mangifera-type, and propolis from South Sulawesi was Calophyllum-type with triterpenes as the main constituent (unpublished data). Samples were prepared with ultrasound-assisted extraction (Trusheva et al., 2007; Fikri et al., 2018). Grounded samples were dissolved in the solvent (water, 75% ethanol) and treated in the ultrasound bath for 4 h. The extracts were filtered and evaporated to obtain dried extracts. The extraction produced water extract of propolis from Banten (WEB) and ethanol extract of propolis from South Sulawesi (EES). Both types of propolis were selected based on our previous result which showed the highest antiemetic activity and potential to use as antiemetic agent for pregnant women (Fikri et al., 2018). The extracts were redissolved in 1% Tween 80 as vehicle solution when administering propolis by oral gavage. This vehicle solution has been reported not to cause toxicity (Ramadan et al., 2012).
2.2. Experimental animals
All animal procedures have been approved by the Animal Care and Use Committee, Bogor Agricultural University (No. 64-2017 IPB) and were in accordance with the recommendations of the proper care and use of laboratory animals.
Mice were purchased from The Tropical Biopharmaca Research Centre, Bogor, aged 8–10 weeks and 25–30 g b.wt. The animals were fed with pellet and water ad libitum and caged under controlled laboratory condition. To ensure the effectiveness of breeding, estrous cycle was checked using the method of Caligioni (2009) and Byers et al. (2012). Male mice were mated with the female at proestrous and estrous stage on a one-to-one basis. The presence of a vaginal plug on the next day was considered as day 0 of pregnancy. Twenty five pregnant mice were equally allotted to five groups including control group administered with 1% Tween 80 in a dose of 5 ml/kg b.wt., low-dose of WEB group (380 mg/kg b.wt.), high-dose of WEB group (1400 mg/kg b.wt.), low-dose of EES group (380 mg/kg b.wt.), high-dose of EES group (1400 mg/kg b.wt.). Dose of 380 mg/kg b.wt. was active dose as antiemesis according to the previous study after converting it to mice dose (Eda et al., 2005). This was part of big study “The Development of Propolis Candy as Antiemesis in Pregnant Women” and thus we chose antiemesis as the biological activity. In addition, dose of 1400 mg/kg b.wt. was non observed adverse effect level (NOAEL) (Burdock, 1998). The pregnant mice were administered from 0 until 18 days of gestation to cover embryogenesis, organogenesis, and functional development stages. The weight was measured every two days. The pregnant mice were sacrificed at 18 days of gestation to analyze external and skeletal abnormalities. The placentas were processed to analyze histopathological changes.
2.3. External examination
Laparotomy was done to exteriorize the gravid uterus then the amniotic sacs were then carefully opened. Placentas and fetuses were dried and weighed. The number of live fetuses, dead fetuses, and late resorptions were counted. Fetal crown-rump length was measured by taking the picture of each fetus using the stereomicroscope then measured using Java Image J program.
2.4. Histopathological examination of placenta
The examination of placenta was done using regular hematoxylin and eosin staining. The procedure was referred to Pillai et al. (2011). After removing from the amniotic sac, the samples were fixed in 10% neutral buffered formalin. The samples were dehydrated with alcohol, cleaned with xylene, infiltrated with paraffin, and followed with microtomized section and stained with hematoxylin and eosin.
2.5. Skeletal examination
Half of fetus was used for skeletal examination. The fetuses were fixed in 96% ethanol to examine skeletal ossification using Alizarin red S staining. The procedures were referred to Hassan et al. (2016) with slight modification. Fetuses were eviscerated and soaked in 1% KOH to clear non-calcified tissue. Subsequently, fetuses were stained with 0.01% Alizarin red S solution for 24, drained and destained using 25%, 50%, 75% glycerin in 1% KOH. The specimens were kept in 100% glycerin and observed under the stereomicroscope.
The observation of the fetuses was done by measuring the thickness of the ossification centre using Image J program. The bones measured were sternebrae 5, supraoccipital, forelimb bones (proximal phalanx 2-5, metacarpal 2-5), hindlimb bones (proximal phalanx 1-5, metatarsal 1-5), lumbar 1-6, and caudal 1-6. These bones are sensitive to growth retardation (Fritz and Hess, 1970; Aliverti et al., 1979).
2.6. Statistical analysis
Data were reported as mean ± standard deviation. The difference in external and skeletal examinations between groups was analysed using ANOVA. When there was a significant overall difference between the groups, Tukey's post-hoc test was conducted with p-value <0.05 was considered significant.
3. Result
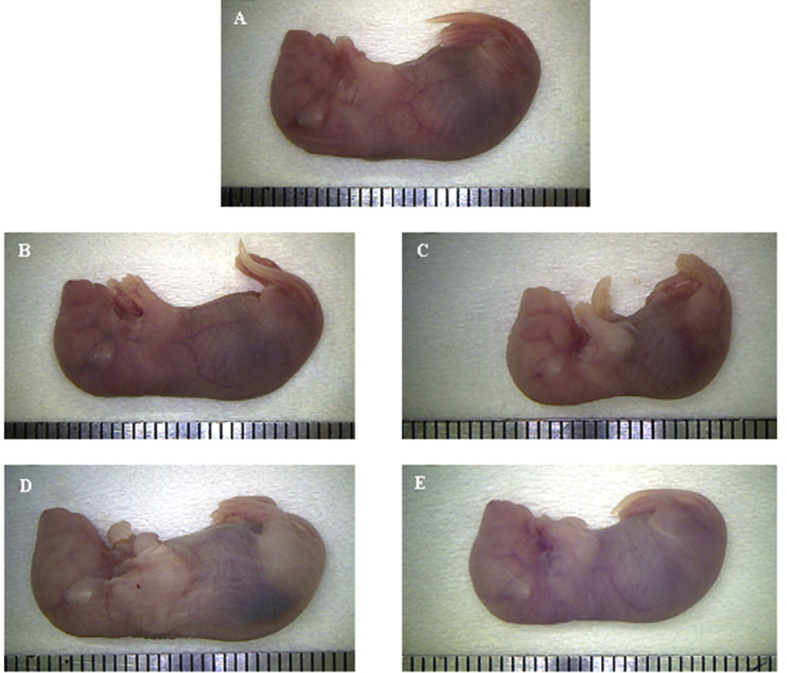
The external examination of fetuses is presented in Table 1 and illustrated in Fig. 1. High-dose of WEB and EES significantly decreased the weight of fetuses, but only high-dose of EES significantly decreased the crown-rump length and increased the number of late resorption compared to the control group. There were no significant differences in the number of live fetuses, dead fetuses, pre and post-implantation embryonic loss, and placental weight among all groups.
Table 1.
The effect of propolis administration on the external examination.
| Parameters | Groups |
||||
|---|---|---|---|---|---|
| Control (n = 5) | Low-dose of EES (n = 5) | High-dose of EES (n = 5) | Low-dose of WEB (n = 5) | High-dose of WEB (n = 5) | |
| Live fetuses | 8.83 ± 0.95 | 10.20 ± 0.5 | 8.86 ± 0.87 | 9.40 ± 0.77 | 9.00 ± 1.12 |
| Fetal weight (g) | 1.30 ± 0.16 | 1.21 ± 0.18 | 0.96 ± 0.15∗ | 1.36 ± 0.20 | 1.03 ± 0.19∗ |
| Crown-rump length (cm) | 2.42 ± 0.13 | 2.40 ± 0.13 | 2.15 ± 0.10∗ | 2.54 ± 0.14 | 2.27 ± 0.19 |
| Placental weight (g) | 0.12 ± 0.02 | 0.12 ± 0.01 | 0.12 ± 0.03 | 0.11 ± 0.01 | 0.13 ± 0.01 |
| Dead fetuses | 0.00 ± 0.00 (0.00%) | 0.20 ± 0.45 (1.82%) | 0.57 ± 1.51 (4.08%) | 0.60 ± 0.55 (5.98%) | 0.60 ± 1.34 (4.62%) |
| Late resorption | 0.50 ± 0.55 (6.68%) | 0.20 ± 0.45 (2.00%) | 1.33 ± 0.82∗ (13.17%) | 0.00 ± 0.00 (0.00%) | 0.40 ± 0.55 (4.86%) |
| Pre-implantation embryonic loss (%) | 0.00 ± 0.00 | 3.36 ± 4.62 | 8.06 ± 11.66 | 0.00 ± 0.00 | 0.00 ± 0.00 |
| Post-implantation embryonic loss (%) | 6.68 ± 6.40 | 3.82 ± 5.24 | 13.17 ± 8.05 | 4.99 ± 5.68 | 9.47 ± 9.85 |
High-dose of EES significantly reduced fetal weight and crown-rump length, and increased the number of late resorption. High-dose of WEB significantly reduced only fetal weight. Both low-dose groups did not appear to inhibit fetal growth.
Significant in relation to control at p < 0.05.
Fig. 1.
The external examination of fetuses. A: control; B: low-dose of EES; C: high-dose of EES; D: low-dose of WEB; E: high-dose of WEB. Lower size was found in high-dose of EES group followed by high-dose of WEB group.
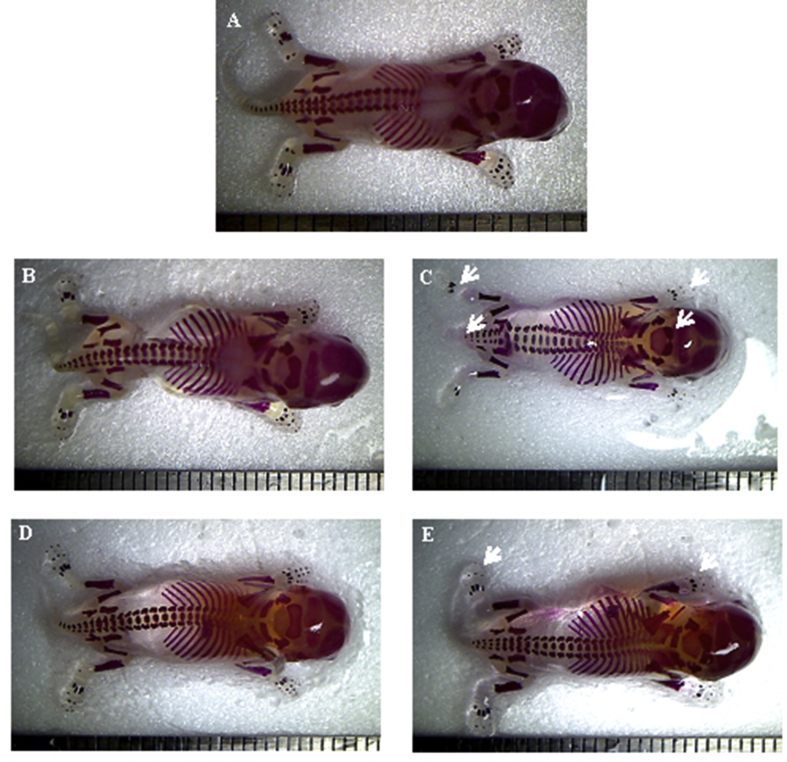
The skeletal examination of fetuses is presented in Table 2, and illustrated in Fig. 2. Both low-dose groups did not decrease the thickness of the ossfication centre. High dose of WEB showed relatively lower ossification than control, however, it was not statistically significant. In contrast, high dose of EES significantly decreased the thickness of several ossified bones, including metacarpal 2-4; proximal phalanx 2,3,5 of forelimb; metatarsal 1-5; proximal phalanx of hindlimb 2-5; caudal 6; compared to the control group. In addition, ossified supraoccipital bone showed a lower value than the control group, but not statistically significant. There is an interesting result, where the fetuses in low-dose of WEB group possessed relatively higher weight, crown-rump length, and thickness of ossification centre compared to the other groups.
Table 2.
The thickness of ossified bone of fetuses.
| Bone | The thickness (dm) |
||||
|---|---|---|---|---|---|
| Control (n = 28) | Low-dose of EES (28) | High-dose of EES (n = 30) | Low-dose of WEB (n = 29) | High-dose of WEB (n = 28) | |
| Sternebrae 5 | 0.222 ± 0.040a | 0.181 ± 0.101 | 0.148 ± 0.086 | 0.237 ± 0.040 | 0.185 ± 0.116 |
| Supraoccipital | 2.980 ± 0.225a,b | 3.130 ± 0.061 | 2.181 ± 1.106 | 3.202 ± 0.325 | 2.689 ± 0.559 |
| Forelimb | |||||
| Metacarpal 2 | 0.267 ± 0.043a,b | 0.271 ± 0.034 | 0.205 ± 0.047∗ | 0.304 ± 0.038 | 0.233 ± 0.049 |
| Metacarpal 3 | 0.411 ± 0.050a | 0.407 ± 0.036 | 0.316 ± 0.057∗ | 0.410 ± 0.074 | 0.353 ± 0.077 |
| Metacarpal 4 | 0.364 ± 0.039a,b | 0.366 ± 0.034 | 0.278 ± 0.048∗ | 0.390 ± 0.068 | 0.319 ± 0.058 |
| Metacarpal 5 | 0.144 ± 0.029a,b | 0.151 ± 0.020 | 0.099 ± 0.046 | 0.176 ± 0.032 | 0.110 ± 0.063 |
| Proximal phalanx 2 | 0.105 ± 0.024a | 0.106 ± 0.037 | 0.042 ± 0.046∗ | 0.118 ± 0.040 | 0.074 ± 0.045 |
| Proximal phalanx 3 | 0.151 ± 0.041a,b | 0.143 ± 0.034 | 0.081 ± 0.061∗ | 0.181 ± 0.047 | 0.105 ± 0.061 |
| Proximal phalanx 4 | 0.153 ± 0.039a,b | 0.151 ± 0.035 | 0.084 ± 0.066 | 0.177 ± 0.046 | 0.107 ± 0.065 |
| Proximal phalanx 5 | 0.094 ± 0.030a | 0.096 ± 0.017 | 0.035 ± 0.040∗ | 0.104 ± 0.070 | 0.053 ± 0.053 |
| Lumbar 1 | 0.678 ± 0.062a,b | 0.680 ± 0.034 | 0.646 ± 0.116 | 0.732 ± 0.098 | 0.600 ± 0.090 |
| Lumbar 2 | 0.697 ± 0.056a | 0.704 ± 0.021 | 0.661 ± 0.135 | 0.734 ± 0.105 | 0.629 ± 0.100 |
| Lumbar 3 | 0.693 ± 0.064a | 0.705 ± 0.021 | 0.669 ± 0.141 | 0.734 ± 0.081 | 0.615 ± 0.096 |
| Lumbar 4 | 0.643 ± 0.041a | 0.701 ± 0.029 | 0.631 ± 0.137 | 0.697 ± 0.078 | 0.604 ± 0.117 |
| Lumbar 5 | 0.601 ± 0.055a | 0.647 ± 0.020 | 0.578 ± 0.151 | 0.666 ± 0.077 | 0.541 ± 0.126 |
| Lumbar 6 | 0.563 ± 0.055a | 0.614 ± 0.012 | 0.528 ± 0.152 | 0.642 ± 0.081 | 0.510 ± 0.121 |
| Caudal 1 | 0.377 ± 0.055b | 0.443 ± 0.039 | 0.349 ± 0.129 | 0.525 ± 0.072 | 0.444 ± 0.166 |
| Caudal 2 | 0.341 ± 0.056a,b | 0.409 ± 0.041 | 0.283 ± 0.125 | 0.462 ± 0.078 | 0.402 ± 0.179 |
| Caudal 3 | 0.279 ± 0.075a | 0.350 ± 0.024 | 0.237 ± 0.140 | 0.388 ± 0.065 | 0.360 ± 0.193 |
| Caudal 4 | 0.246 ± 0.064a | 0.293 ± 0.033 | 0.180 ± 0.153 | 0.347 ± 0.065 | 0.320 ± 0.207 |
| Caudal 5 | 0.194 ± 0.087a,b | 0.258 ± 0.041 | 0.132 ± 0.139 | 0.311 ± 0.063 | 0.270 ± 0.168 |
| Caudal 6 | 0.169 ± 0.139a | 0.156 ± 0.073 | 0.026 ± 0.037∗ | 0.268 ± 0.056 | 0.211 ± 0.229 |
| Hindlimb | |||||
| Metatarsal 1 | 0.110 ± 0.042a | 0.090 ± 0.028 | 0.043 ± 0.052∗ | 0.139 ± 0.042 | 0.083 ± 0.050 |
| Metatarsal 2 | 0.442 ± 0.070a,b | 0.422 ± 0.057 | 0.303 ± 0.080∗ | 0.490 ± 0.063 | 0.353 ± 0.097 |
| Metatarsal 3 | 0.522 ± 0.070a,b | 0.504 ± 0.063 | 0.356 ± 0.084∗ | 0.550 ± 0.092 | 0.412 ± 0.106 |
| Metatarsal 4 | 0.564 ± 0.074a.b | 0.533 ± 0.069 | 0.393 ± 0.115∗ | 0.619 ± 0.093 | 0.459 ± 0.104 |
| Metatarsal 5 | 0.388 ± 0.064a,b | 0.385 ± 0.043 | 0.273 ± 0.082∗ | 0.435 ± 0.068 | 0.297 ± 0.089 |
| Proximal phalanx 1 | 0.023 ± 0.035b | 0.008 ± 0.015 | 0.011 ± 0.029 | 0.061 ± 0.039∗ | 0.013 ± 0.021 |
| Proximal phalanx 2 | 0.078 ± 0.033a | 0.080 ± 0.036 | 0.024 ± 0.041∗ | 0.101 ± 0.034 | 0.055 ± 0.045 |
| Proximal phalanx 3 | 0.098 ± 0.042a | 0.096 ± 0.042 | 0.032 ± 0.049∗ | 0.122 ± 0.039 | 0.067 ± 0.053 |
| Proximal phalanx 4 | 0.116 ± 0.038a | 0.110 ± 0.042 | 0.038 ± 0.063∗ | 0.133 ± 0.040 | 0.068 ± 0.056 |
| Proximal phalanx 5 | 0.094 ± 0.050a | 0.092 ± 0.038 | 0.001 ± 0.002∗ | 0.103 ± 0.061 | 0.044 ± 0.054 |
High-dose of EES significantly delayed the ossification of several bones, including metacarpal 2-3, proximal phalanx 2,3,5 of forelimb, caudal 6, metatarsal 1-5, proximal phalanx 2-5 of hindlimb. High-dose of WEB showed relative inhibition of ossification but not statistically significant compared to control group. However, both low-dose groups did not show any alteration.
Significant in relation to control at p < 0.05; n = number of fetuses.
Fig. 2.
The ossification of fetal bones after straining with Alizarin Red S. A: control; B: low-dose of EES; C: high-dose of EES; D: low-dose of WEB; E: high-dose of WEB. High dose of EES significantly reduced the thickness of ossified bones (white arrow), while high-dose of WEB gave moderate impact.
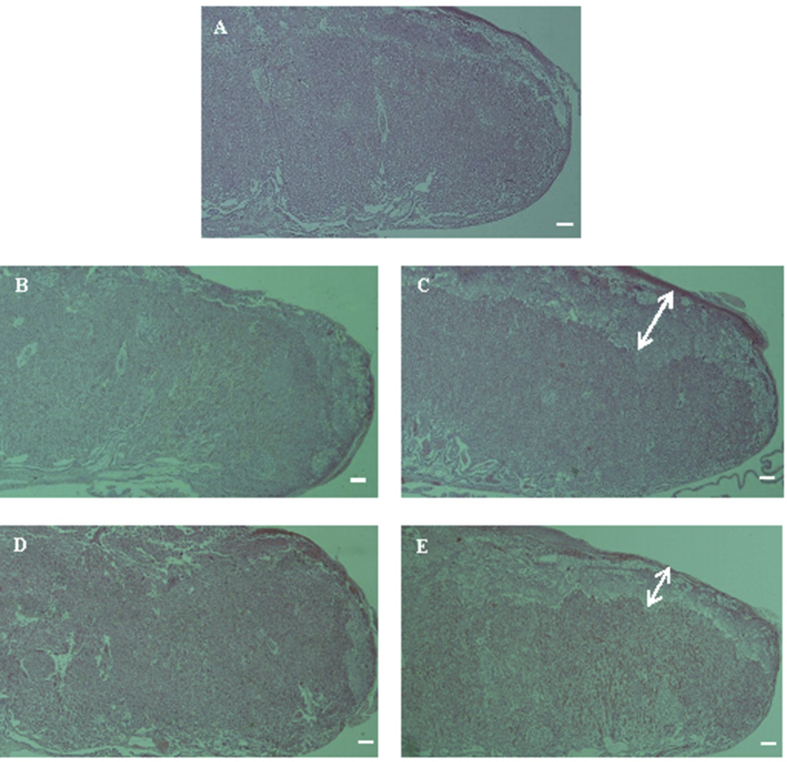
The histopathological examination of placenta is depicted in Fig. 3. We found a shortened labyrinth of placenta along with the expansion of basal zone in both high-dose groups. Blood vessels formed a short, dense, and highly branched network. The hypertrophy of placenta was also found in several pregnant dams in both high-dose groups.
Fig. 3.
The histopathological examination of placenta. A: control; B: low-dose of EES; C: high-dose of EES; D: low-dose of WEB; E: high-dose of WEB. Small labyrinth along with expansion of basal zone (white arrow) were found in both high-dose groups (bar = 125 μm).
4. Discussion
The present study showed that low-dose of propolis did not cause any alterations in fetal development. However, high-dose of propolis might retard the development. We found decreased fetal weight and crown-rump at high-dose groups. Fetal weight is the main parameter to assess developmental toxicity (FDA, 2005; Hoberman and Lewis, 2017). Moreover, crown-rump is another parameter to examine fetal development and bone maturation (Kjar, 1974; Hoberman and Lewis, 2017). This indicates high-dose of propolis could inhibit fetal development.
In addition, high-dose of EES increased the number of late resorption. Mice prefer absorbing the imperfect conception to aborting (Telford et al., 1962). The immunomodulatory property of propolis could be the underlying mechanism. Propolis has been known to possess immunomodulatory property (Orsi et al. 2000, 2005; Chan et al., 2013; Kalsum et al., 2017). Resorption may occur due to the rejection via immune system pathway. Increased macrophage activity in the endometrium during pregnancy leads to increased production of NO and TNF-α, which are toxic to embryo development (Baines et al., 1997). Indeed, Tartakovsky (1989) found colony stimulating factor-1 (CSF-1) might increase resorption in pregnant mice. CSF-1 plays an important role in the differentiation of macrophage.
Anticancer activity of propolis was proposed to be the underlying mechanism of fetal growth retardation in both high-dose groups. It has been known that the anticancer agents are mostly teratogen and vice versa (Blattner et al., 1958; Sieber et al., 1978; Blagosklonny, 2005). Some natural products which have anticancer effects are also teratogens. Mohammed et al. (2016) found 6-gingerol (ginger), gingkolide A, gingkolide B (Gingko biloba) and gingsennoside Rg1 (ginseng) at high-dose showed teratogenic effects on chick embryonic heart micromass and mouse D3 embryonic stem cell. However, the compounds had no effect at a low dose and it was similar to the present study. Therefore, the teratogenic effect of the natural product might appear only at a high dose.
Anticancer activity of propolis has been extensively examined (Suzuki et al., 2002; Oršolić; Bašić, 2003; Oršolic et al., 2005; Xuan et al., 2014). However, there were still few studies reported the anticancer activity of stingless bee propolis and its underlying mechanisms. Stingless bee propolis was reported active to against several cancer cells, including breast, colon, lung, gastric, liver, colorectal, skin, and bone cancer cell lines (Cinegaglia et al. 2013; Choudhari et al. 2013; Kustiawan et al. 2014). Propolis induces TNF-related apoptosis-inducing ligand (TRAIL) which mediates the programming of cell apoptosis (Oršolic et al., 2005). Propolis also activates caspase cascades and/or inhibit the production of bcl-2 and mitochondrial cytochrome c which lead to apoptosis (Sawicka et al., 2012).
It is interesting to discuss high-dose of WEB showed a moderate effect of inhibition compared to high dose of EES. However, we did not use raw propolis from the same origin, therefore we cannot compare its effect between the solvents. However, propolis works not as a single constituent but as a mixture (Watanabe et al., 2011). Regardless of propolis origin, pregnant mice were more tolerated to water extract than ethanol extract. Although there has no study comparing the anticancer activity of water and ethanol extract of propolis, some results of previous studies may help us to explain the findings. Water extraction produces more carbohydrates (sugar) but much less wax and resin than ethanol extract. Vitamins and amino acids coming from bee pollen could probably be extracted (Castaldo and Capasso, 2002; Najafi et al., 2007). This causes the phytochemical content of water extract of propolis less concentrated. It was confirmed by Sun et al. (2015) who compared the phytochemical profiles between water and ethanol extract of propolis. In addition, Do et al. (2014) found the major constituents of water extract of propolis were terpenes and carbohydrates. With respect to the theory that natural products induce teratogenic effect at high dose, it is reasonable that water extract was more tolerated than ethanol extract at high dose due to the less concentrated phytochemical composition. This might also explain why did only high-dose of EES increase the number of resorption.
Bone ossification generally reflects the maturity of fetal development (Hill, 1939; Gentili et al., 1984). This was confirmed by the present study which the fetuses of high-dose of EES group showed lower weight and crown-rump, and retarded bone ossification. Indeed, a high dose of WEB gave moderate effect on the weight and crown-rump length of fetuses and reflected moderate delayed bone ossification. The fetuses of high-dose of EES group seemed to be younger than 18 days of gestation. We found relatively shortened ossification of supraoccipital bone because it mostly had yet to be fused while the fusion should happen at 18 days of gestation (Tyl and Marr, 2016). In addition, high-dose of EES also decreased the thickness of ossification at caudal 6. We found the fetuses in this group mostly had the centre of caudal ossification only up to caudal 5. Moreover, metatarsal 2-4 which the centre of ossification that should appear at 17 days of gestation (Patton and Kaufman, 1995) seemed to be more sensitive in detecting delayed ossification. Instead, the bones which should appear later, including metacarpal 5 and some proximal phalanxes tended to have higher variation thus difficult to show a significant result.
The delayed ossification in high-dose groups was not a specific response. Similarly, previous research on developmental toxicity also found the same manner (Schwetz et al., 1978; Marques et al., 2010; Alfiah, 2017). The delay is due to general fetal growth retardation reflected by lower weight and crown-rump length. In addition, the retardation also followed the cephalocaudal manner, where the variations tend to be common on the hindlimb (Sucheston et al., 1986).
The inhibition of fetal growth in both high-dose groups might be caused by the disruption of placental development. The small labyrinth is commonly found in the failure of placental development due to the inadequate fabrication of vessels and trophoblast cells (Bolon, 2015). The trophoblast cells are the most common target by toxicity due to its rapid proliferation (Furukawa et al., 2011). The small labyrinth and thickening of the basal zone cause the inhibition of nutrient and gas transfer. The hypertrophy of placenta that found in several pregnant dams in both high-dose groups might be the compensatory response of intrauterine growth retardation (IUGR) (Furukawa et al. 2008, 2011).
5. Conclusion
This study concludes that Indonesian propolis at 380 mg/kg b.wt. does not inhibit fetal development. However, Indonesian propolis at 1400 mg/kg b.wt did appear to inhibit fetal development. Non-observed adverse effect level that has been established (1400 mg/kg) cannot be used as the safety level in pregnant condition. Placenta might be the targeted organ of toxicity by propolis that causing the retardation of fetal growth.
Declarations
Author contribution statement
Al Mukhlas Fikri, Mokhamad Fahrudin: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Ahmad Sulaeman: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data.
Ekowati Handharyani: Conceived and designed the experiments; Analyzed and interpreted the data.
Sri Anna Marliyati: Conceived and designed the experiments; Performed the experiments.
Funding statement
This work was supported by the Ministry of Research and Technology and Higher Education of the Republic of Indonesia.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- Alfiah E. 2017. The Safety of Ethanol Extract of Tobangun Leaves (Coleus Amboinicus Lour.) on Fetal Development. Thesis. Bogor Agricultural University. [Google Scholar]
- Aliverti V., Bonanomi L., Giavini E., Leone V.G., Mariani L. The extent of fetal ossification as an index of delayed development in teratogenic studies on the rat. Teratology. 1979;20(2):237–242. doi: 10.1002/tera.1420200208. [DOI] [PubMed] [Google Scholar]
- Baines M.G., Duclos A.J., Antecka E., Haddad E.K. Decidual infiltration and activation of macrophages leads to early embryo loss. Am. J. Reprod. Immunol. 1997;37(6):471–477. doi: 10.1111/j.1600-0897.1997.tb00262.x. [DOI] [PubMed] [Google Scholar]
- Bankova V.S., de Castro S.L., Marcucci M.C. Propolis: recent advances in chemistry and plant origin. Apidologie. 2000;31(1):3–15. [Google Scholar]
- Blagosklonny M.V. Teratogens as anticancer drugs. Cell Cycle. 2005;4(11):1518–1521. doi: 10.4161/cc.4.11.2208. [DOI] [PubMed] [Google Scholar]
- Blattner R.J., Williamson A.P., Simonsen L. Teratogenic changes in early chick embryos following administration of antitumor agent (Azaserine) PSEBM (Proc. Soc. Exp. Biol. Med.) 1958;97(3):560–564. doi: 10.3181/00379727-97-23805. [DOI] [PubMed] [Google Scholar]
- Bolon B., editor. Pathology of the Developing Mouse: A Systematic Approach. CRC Press; 2015. [Google Scholar]
- Burdock G.A. Review of the biological properties and toxicity of bee propolis (propolis) Food Chem. Toxicol. 1998;36(4):347–363. doi: 10.1016/s0278-6915(97)00145-2. [DOI] [PubMed] [Google Scholar]
- Byers S.L., Wiles M.V., Dunn S.L., Taft R.A. Mouse estrous cycle identification tool and images. PLoS One. 2012;7(4):1–5. doi: 10.1371/journal.pone.0035538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caligioni C.S. Assessing reproductive status/stages in mice. Curr. Protocol. Neurosci. 2009;48(1) doi: 10.1002/0471142301.nsa04is48. A-4I. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castaldo S., Capasso F. Propolis, an old remedy used in modern medicine. Fitoterapia. 2002;73:S1–S6. doi: 10.1016/s0367-326x(02)00185-5. [DOI] [PubMed] [Google Scholar]
- Chan G.C.F., Cheung K.W., Sze D.M.Y. The immunomodulatory and anticancer properties of propolis. Clin. Rev. Allergy Immunol. 2013;44(3):262–273. doi: 10.1007/s12016-012-8322-2. [DOI] [PubMed] [Google Scholar]
- Choudhari M.K., Haghniaz R., Rajwade J.M., Paknikar K.M. Anticancer activity of Indian stingless bee propolis: an in vitro study. Evid. Based Complement Altern. Med. 2013;2013 doi: 10.1155/2013/928280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cinegaglia N.C., Bersano P.R.O., Araújo M.J.A.M., Búfalo M.C., Sforcin J.M. Anticancer effects of geopropolis produced by stingless bees on canine osteosarcoma cells in vitro. Evid. Based Complement Altern. Med. 2013;2013 doi: 10.1155/2013/737386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Do Q.D., Angkawijaya A.E., Tran-Nguyen P.L., Huynh L.H., Soetaredjo F.E., Ismadji S., Ju Y.H. Effect of extraction solvent on total phenol content, total flavonoid content, and antioxidant activity of Limnophila aromatica. J. Food Drug Anal. 2014;22(3):296–302. doi: 10.1016/j.jfda.2013.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eda M., Hayashi Y., Kinoshita K., Koyama K., Takahashi K., Akutu K. Anti-emetic principles of water extract of Brazilian Propolis. Pharm. Biol. 2005;43(2):184–188. [Google Scholar]
- Fikri A.M., Sulaeman A., Marliyati S.A., Fahrudin M. Antiemetic activity of trigona spp. propolis from three provinces of Indonesia with two methods of extraction. Pharmacogn. J. 2018;10(1):120–122. [Google Scholar]
- Fritz H., Hess R. Ossification of the rat and mouse skeleton in the perinatal period. Teratology. 1970;3(4):331–337. doi: 10.1002/tera.1420030409. [DOI] [PubMed] [Google Scholar]
- Food and Drug Administration [FDA] 2005. Guideline for Industry: Detection of Toxicity to Reproduction for Medicinal Products & Toxicity to Male Fertility, (ICH) S5(R2)http://www.ich.org/products/guidelines/safety/safety-single/article/detectionof-toxicity-to-reproduction-for-medicinal-products-oxicity-to-malefertility.html Available at: [Google Scholar]
- Furukawa S., Hayashi S., Usuda K., Abe M., Ogawa I. Histopathological effect of ketoconazole on rat placenta. J. Vet. Med. Sci. 2008;70(11):1179–1184. doi: 10.1292/jvms.70.1179. [DOI] [PubMed] [Google Scholar]
- Furukawa S., Hayashi S., Usuda K., Abe M., Hagio S., Ogawa I. Toxicological pathology in the rat placenta. J. Toxicol. Pathol. 2011;24(2):95–111. doi: 10.1293/tox.24.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentili P., Trasimeni A., Giorlandino C. Fetal ossification centers as predictors of gestational age in normal and abnormal pregnancies. J. Ultrasound Med. 1984;3(5):193–197. doi: 10.7863/jum.1984.3.5.193. [DOI] [PubMed] [Google Scholar]
- Goel R.K., Prabha T., Kumar M.M., Dorababu M., Singh G. Teratogenicity of Asparagus racemosus Willd. root, a herbal medicine. Indian J. Exp. Biol. 2006;44:570–573. [PubMed] [Google Scholar]
- Hassan M.S., Morgan A.M., Mekawy M.M., Zaki A.R., Ghazi Z.M. Teratogenic effect of cisplatin in rats and the protective role of sodium selenate. Exp. Toxicol. Pathol. 2016;68(5):277–287. doi: 10.1016/j.etp.2016.02.003. [DOI] [PubMed] [Google Scholar]
- Hill A.H. Fetal age assessment by centers of ossification. Am. J. Phys. Anthropol. 1939;24(3):251–272. [Google Scholar]
- Hoberman A.M., Lewis E.M. Reproductive and Developmental Toxicology. second ed. 2017. Juvenile toxicology testing; pp. 129–144. [Google Scholar]
- Huang S., Zhang C.P., Wang K., Li G., Hu F.L. Recent advances in the chemical composition of propolis. Molecules. 2014;19(12):19610–19632. doi: 10.3390/molecules191219610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalsum N., Sulaeman A., Setiawan B., Wibawan I.W.T. The effect of liquid Trigona spp. propolis of the immune system of Sprague Dawley rats infected Sthapylococcus aureus. Jurnal Gizi dan Pangan. 2017;12(1):23–30. [Google Scholar]
- Kjar I. Skeletal maturation of the human fetus assessed radiographically on the basis of ossification sequences in the hand and foot. Am. J. Phys. Anthropol. 1974;40(2):257–275. doi: 10.1002/ajpa.1330400211. [DOI] [PubMed] [Google Scholar]
- Król W., Bankova V., Sforcin J.M., Szliszka E., Czuba Z., Kuropatnicki A.K. Propolis: properties, application, and its potential. Evid. Based Complement Altern. Med. 2013;2013 doi: 10.1155/2013/807578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kustiawan P.M., Puthong S., Arung E.T., Chanchao C. In vitro cytotoxicity of Indonesian stingless bee products against human cancer cell lines. Asian Pacific J. Trop. Biomed. 2014;4(7):549–556. doi: 10.12980/APJTB.4.2014APJTB-2013-0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotfy M. Biological activity of bee propolis in health and disease. Asian Pac. J. Cancer Prev. APJCP. 2006;7(1):22–31. [PubMed] [Google Scholar]
- Marques N.F.Q., Marques A.P.B.M., Iwano A.L., Golin M., De-Carvalho R.R., Paumgartten F.J.R., Dalsenter P.R. Delayed ossification in Wistar rats induced by Morinda citrifolia L. exposure during pregnancy. J. Ethnopharmacol. 2010;128(1):85–91. doi: 10.1016/j.jep.2009.12.029. [DOI] [PubMed] [Google Scholar]
- Mohammed O.J., Latif M.L., Pratten M.K. Evaluation of embryotoxicity for major components of herbal extracts using the chick embryonic heart micromass and mouse D3 embryonic stem cell systems. Reprod. Toxicol. 2016;59:117–127. doi: 10.1016/j.reprotox.2015.12.003. [DOI] [PubMed] [Google Scholar]
- Najafi M.F., Vahedy F., Seyyedin M., Jomehzadeh H.R., Bozary K. Effect of the water extracts of propolis on stimulation and inhibition of different cells. Cytotechnology. 2007;54(1):49–56. doi: 10.1007/s10616-007-9067-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orsi R.O., Funari S.R.C., Soares A.M.V.C., Calvi S.A., Oliveira S.L., Sforcin J.M., Bankova V. Immunomodulatory action of propolis on macrophage activation. J. Venom. Anim. Toxins. 2000;6(2):205–219. [Google Scholar]
- Orsi R.O., Sforcin J.M., Funari S.R., Bankova V. Effects of Brazilian and Bulgarian propolis on bactericidal activity of macrophages against Salmonella typhimurium. Int. Immunopharmacol. 2005;5(2):359–368. doi: 10.1016/j.intimp.2004.10.003. [DOI] [PubMed] [Google Scholar]
- Oršolić N., Bašić I. Immunomodulation by water-soluble derivative of propolis: a factor of antitumor reactivity. J. Ethnopharmacol. 2003;84(2-3):265–273. doi: 10.1016/s0378-8741(02)00329-x. [DOI] [PubMed] [Google Scholar]
- Oršolic N., Šver L., Terzić S., Bašić I. Peroral application of water-soluble derivative of propolis (WSDP) and its related polyphenolic compounds and their influence on immunological and antitumour activity. Vet. Res. Commun. 2005;29(7):575–593. doi: 10.1007/s11259-005-3303-z. [DOI] [PubMed] [Google Scholar]
- Park D., Jeon J.H., Shin S., Joo S.S., Kang D.H., Moon S.H. Green tea extract increases cyclophosphamide-induced teratogenesis by modulating the expression of cytochrome P-450 mRNA. Reprod. Toxicol. 2009;27(1):79–84. doi: 10.1016/j.reprotox.2008.11.058. [DOI] [PubMed] [Google Scholar]
- Patton J.T., Kaufman M.H. The timing of ossification of the limb bones, and growth rates of various long bones of the fore and hind limbs of the prenatal and early postnatal laboratory mouse. J. Anat. 1995;186(Pt 1):175–185. [PMC free article] [PubMed] [Google Scholar]
- Pillai P.G., Suresh P., Aggarwal G., Doshi G., Bhatia V. Pharmacognostical standardization and toxicity profile of the methanolic leaf extract of Plectranthus amboinicus (Lour) Spreng. J. Appl. Pharm. Sci. 2011;1(2):75–81. [Google Scholar]
- Ramadan A., Soliman G., Mahmoud S.S., Nofal S.M., Abdel-Rahman R.F. Evaluation of the safety and antioxidant activities of Crocus sative and propolis ethanolic extracts. J. Saudi Chem. Soc. 2012;16(1):13–21. [Google Scholar]
- Salatino A., Teixeira É.W., Negri G. Origin and chemical variation of Brazilian propolis. Evid. Based Complement Altern. Med. 2005;2(1):33–38. doi: 10.1093/ecam/neh060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawicka D., Car H., Borawska M.H., Nikliński J. The anticancer activity of propolis. Folia Histochem. Cytobiol. 2012;50(1):25–37. doi: 10.2478/18693. [DOI] [PubMed] [Google Scholar]
- Schwetz B.A., Smith F.A., Staples R.E. Teratogenic potential of ethanol in mice, rats and rabbits. Teratology. 1978;18(3):385–392. doi: 10.1002/tera.1420180313. [DOI] [PubMed] [Google Scholar]
- Sieber S.M., Whang-Peng J., Botkin C., Knutsen T. Teratogenic and cytogenetic effects of some plant-derived antitumor agents (vincristine, colchicine, maytansine, VP-16-213 and VM-26) in mice. Teratology. 1978;18(1):31–47. doi: 10.1002/tera.1420180107. [DOI] [PubMed] [Google Scholar]
- Sucheston M.E., Hayes T.G., Eluma F.O. Relationship between ossification and body weight of the CD-1 mouse fetus exposed in utero to anticonvulsant drugs. Teratog. Carcinog. Mutagen. 1986;6(6):537–546. doi: 10.1002/tcm.1770060607. [DOI] [PubMed] [Google Scholar]
- Sun C., Wu Z., Wang Z., Zhang H. Effect of ethanol/water solvents on phenolic profiles and antioxidant properties of Beijing propolis extracts. Evid. Based Complement Altern. Med. 2015;2015 doi: 10.1155/2015/595393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki I., Hayashi I., Takaki T., Groveman D.S., Fujimiya Y. Antitumor and anticytopenic effects of aqueous extracts of propolis in combination with chemotherapeutic agents. Cancer Biother. Radiopharm. 2002;17(5):553–562. doi: 10.1089/108497802760804781. [DOI] [PubMed] [Google Scholar]
- Taloubi L.M., Rhouda H., Belahcen A., Smires N., Thimou A., Mdaghri A.A. An overview of plants causing teratogenicity: fenugreek (Trigonella foenum graecum) Int. J. Pharm. Sci. Res. 2013;4:516–519. [Google Scholar]
- Tartakovsky B. CSF-1 induces resorption of embryos in mice. Immunol. Lett. 1989;23(1):65–69. doi: 10.1016/0165-2478(89)90157-0. [DOI] [PubMed] [Google Scholar]
- Telford I.R., Woodruff C.S., Linford R.H. Fetal resorption in the rat as influenced by certain antioxidants. Am. J. Anat. 1962;110(1):29–36. doi: 10.1002/aja.1001100104. [DOI] [PubMed] [Google Scholar]
- Trusheva B., Trunkova D., Bankova V. Different extraction methods of biologically active components from propolis: a preliminary study. Chem. Cent. J. 2007;1(1):13. doi: 10.1186/1752-153X-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyl R.W., Marr M.C. Developmental and Reproductive Toxicology. CRC Press; 2016. Developmental toxicity testing—Methodology; pp. 153–197. [Google Scholar]
- Watanabe M.A.E., Amarante M.K., Conti B.J., Sforcin J.M. Cytotoxic constituents of propolis inducing anticancer effects: a review. J. Pharm. Pharmacol. 2011;63(11):1378–1386. doi: 10.1111/j.2042-7158.2011.01331.x. [DOI] [PubMed] [Google Scholar]
- Xuan H., Li Z., Yan H., Sang Q., Wang K., He Q. Antitumor activity of Chinese propolis in human breast cancer MCF-7 and MDA-MB-231 cells. Evid. Based Complement Altern. Med. 2014;2014 doi: 10.1155/2014/280120. [DOI] [PMC free article] [PubMed] [Google Scholar]