Abstract
Background:
The incidence of rotator cuff repairs has risen dramatically over the past 10 years, most notably in the working-class population. Return to work (RTW) is a valuable outcome measure to set patient expectations before surgery.
Purpose:
To establish the rate of RTW after rotator cuff repair with respect to stratified levels of occupational demand (sedentary, light, moderate, and heavy) and to identify clinical factors significantly associated with postoperative RTW.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Patients who received rotator cuff repair between 2014 and 2017 were queried from a prospectively maintained institutional registry. Work status was evaluated from clinical and physical therapy notes, and RTW was stratified based on duty level. The minimal clinically important difference (MCID), substantial clinical benefit (SCB), and patient acceptable symptom state (PASS) values were calculated for American Shoulder and Elbow Surgeons (ASES) score and subjective Constant score through use of an anchor-based approach. Patient demographic factors, preoperative ASES scores, Constant scores, and health-related quality of life scores, as well as change in postoperative scores exceeding the thresholds for MCID, SCB, and PASS, were analyzed to determine significant associations with RTW without restriction.
Results:
In total, 89 patients with documented pre- and postoperative work status underwent surgery. Rates of RTW for sedentary, light, moderate, and heavy duties were 100%, 84.0%, 77.4%, and 63.3%, respectively, within return at less than 7 postoperative months on average. RTW was associated with achieving PASS (P = .004) but not achieving MCID and SCB (P = .429 and .452, respectively). Injury to a patient’s dominant side had reduced odds (0.057; 95% CI, 0.004-0.763; P = .030) for RTW at full duty. Tear characteristics and type of insurance were not associated with RTW. Preoperative Veterans RAND Mental Component Score (>53.3; area under the curve, 70.4%) was predictive of returning to work.
Conclusion:
A vast majority of patients undergoing rotator cuff repair can expect to return to work within 8 months of surgery. Preoperative mental health scores can predict future return to work, which supports the concept that mental health status plays an important role in the outcomes after rotator cuff repair surgery.
Keywords: rotator cuff repair, quality-based care, minimal clinically important difference, substantial clinical benefit, patient acceptable symptom state, return to work
The incidence of rotator cuff repair surgery is reported to have increased by more than 200% in the past 20 years in multiple countries, with an increasingly greater proportion of these procedures being performed arthroscopically.17,33,40,50,54 All-arthroscopic rotator cuff repair has demonstrated equivalent outcomes and reduced complications compared with the traditional open repair.6,13 Contributing factors to this recent surge may include improved diagnostic imaging modalities, increased expectations of patients to return to function, improved access to care for patients with rotator cuff injury, greater numbers of surgeons trained in arthroscopy, and advances in all-arthroscopic surgical techniques.6,13,15,23,45 Furthermore, the increase in repairs for rotator cuff tears within the past 2 decades has been most pronounced in patients between 45 and 65 years of age, who represent a significant percentage of the workforce.17,40
Validated patient-reported outcome measures (PROMs) are tools often used to assess patients’ postoperative recovery and function after rotator cuff repair.12,22 However, several deficiencies exist in the literature regarding patient-reported outcomes after rotator cuff repair. Retear rates have not been correlated with outcome scores, and differences in patient-related outcome scores have not significantly changed over the past 20 years.30 Statistically significant improvements in outcome scores may not necessarily be meaningful clinically, and therefore, a greater focus must be placed on detecting clinically significant patient improvements.24,38 The minimal clinically important difference (MCID), substantial clinical benefit (SCB), and patient acceptable symptom state (PASS) have become accepted measures to report clinically meaningful differences in PROMs.34,36,37 Alternatively, health-related quality of life (HRQoL) outcomes after rotator cuff surgery have also been recognized as valuable to determine holistic improvement in patient function after surgery.9
Despite the emergence of these newer tools to assist in detecting clinically significant patient improvement after surgery, patient-reported outcome questionnaires largely exclude any evaluation of patient return to preoperative employment. Return to work (RTW) has been shown to serve as an important correlate of patient function and quality of life after shoulder surgery.7,19 Given the expanding working-age patient population undergoing rotator cuff repair, surgeons in clinical settings are commonly asked whether a patient will achieve RTW. To better understand the relationship between RTW and clinical outcomes, it is important to examine any associations that may exist between return to preoperative employment and changes in the PROMs used to evaluate patients postoperatively.
The purpose of this study was to establish the rate of RTW after rotator cuff repair with respect to stratified levels of occupational demand (sedentary, light, moderate, and heavy duties) and to identify clinical factors significantly associated with the likelihood of postoperative RTW. Our hypothesis is that shoulder-specific questionnaires can predict the ability to return to preoperative employment, as these questionnaires assess factors that are known to restrict work abilities including pain, motion related to activities, and overall function.
Methods
Study Design
The study design was a retrospective analysis of prospectively collected PROMs. Our institution maintains a registry of all patients who underwent rotator cuff repair based on medical record procedural and billing data, including Current Procedural Terminology and International Classification of Diseases codes. This registry is managed by full-time research staff under direct supervision of clinical faculty. An electronic data collection service (Outcome Based Electronic Research Database; Universal Research Solutions) is used to enable patients to fill out validated preoperative and postoperative PROM questionnaires regarding their symptoms and recovery as part of routine clinical follow-up. In 2014, institutional policy regarding this data collection service was modified to ensure that all patients were asked a specific set of additional questions to evaluate their postoperative pain, function, and activity level as related to their shoulder. These questions, referred to as “anchor questions,” allowed for more sophisticated analyses regarding patient subjective clinical improvement and PROMs, which are described later in detail. Thus, the institutional registry was queried for all patients who underwent rotator cuff repair at our institution from 2014 until this study was conducted in 2017.
Outcomes
Patients completed shoulder-specific PROM questionnaires, such as the American Shoulder and Elbow Surgeons (ASES)32 score, the subjective Constant score,14 and the Single Assessment Numeric Evaluation (SANE),51 as well as HRQoL questionnaires including the Veterans RAND 12-Item Health Survey (VR-12) and the Veterans RAND 6-Dimensions (VR-6D),46 before surgery. The VR-12 and VR-6D questionnaires have been used in previous studies evaluating populations with rotator cuff tear as well as other civilian populations outside the realm of orthopaedic surgery.27,28,44 The subjective Constant score assesses pain and activities of daily living with a maximum score of 35. ASES score and SANE are both scored on a 100-point scale. The VR-12 mental and physical component scores (VRMCS and VRPCS, respectively) each have 100 possible points and are normed to a score of 50 in the US population, with a standard deviation of 10.
As stated previously, anchor questions were implemented at our institution to allow patients to subjectively evaluate their postoperative pain, function, and activity level pertaining to their shoulder. For the purposes of this analysis, we used the single anchor question related specifically to function, as this was expected to be most pertinent to RTW. The anchor question was, “Since your surgery, has there been any change in the overall function of your shoulder?” Postoperatively, patients completed both the shoulder-specific and HRQoL questionnaires mentioned previously, in addition to this anchor question, at the 1-year time point. After rotator cuff repair, 1 year is the expected time frame to achieve maximum medical improvement (MMI), defined as the postoperative time point when patients stop experiencing significant clinical benefits.55 To improve response rates, the surveys were sent electronically every 5 days until all of them were completed. Patients returning to the clinic for routine follow-up at 1 year postoperative were asked to complete the questionnaires in person. Finally, patients who were unable to complete the surveys electronically or in clinic were called once a week to maximize response rates. Upon completion, patients were not contacted further. Postoperative survey administration was ceased upon exceeding 1 month since the 1-year postoperative time point for all patients (ie, 13 postoperative months), as clinically significant outcomes were intended to be representative of the 1-year time point to create homogeneous data.
Responses to anchors were scored on a 15-point scale from “a very great deal worse” to “a very great deal better.” These scores were used to calculate the MCID, SCB, and PASS via an anchor-based approach for the ASES score.21 The anchor-based approach is a robust method to establish clinically based differences from patient-reported outcomes and has been used in a similar fashion in previous literature.21,49 Differences in delta (postoperative minus preoperative) outcomes between patients who reported “minimal change” and “no change” were used to construct a model predicting MCID. Differences in delta outcomes between patients who reported “significant change” and “no change” were used to construct a model predicting the SCB. Last, differences in postoperative PROMs of patients deeming surgery as satisfactory and those considering surgery as unsatisfactory were used to construct the PASS. The same PROMs as those used in calculating MCID and SCB were also used for the PASS (ASES, Constant, SANE).
Patient Selection
A total of 1158 patients who underwent rotator cuff repair procedures were registered during this time period. Of these, 356 patients met inclusion criteria of answering all PROMs, while the remaining patients had missing data points precluding them from inclusion. Upon review of medical records, patients were then excluded if they underwent previous same-side rotator cuff surgery or if they received concomitant augmentation via dermal allograft, platelet-rich plasma, or bone marrow aspirate concentrate during their rotator cuff repair. Medical records were also reviewed for preoperative work status to determine which patients held occupations before undergoing surgery. Patients who had no reported work status were compared with those who did have a reported work status according to several parameters, such as age, sex, workers’ compensation status, and baseline PROMs (Table 1). A 1-way analysis of variance (ANOVA) was used to make statistical comparisons between groups. This comparison was made in order to detect any potential differences in preoperative demographic factors between patients with versus without reported work status. For patients with reported occupations, the titles of those occupations were noted and correlated with the respective levels of duty per the US Department of Labor guidelines.48 Medical records were then examined to determine whether patients reached MMI after their rotator cuff repair, as stated by the managing physician upon clinical evaluation; whether they returned to work after the procedure; and whether they were able to perform their job at full duty. Patients with permanent restrictions were documented. Variables such as age, body mass index (BMI), sex, comorbidities, smoking status, and intraoperative details of cuff tear size and repair were also collected for regression analysis. After application of all inclusion and exclusion criteria, a total of 89 patients with verified pre- and postoperative work status were included in the final analysis.
TABLE 1.
Demographics of Patients With and Without Reported Work Statusa
| Return to Work Reported (Final Cohort) | Return to Work Not Reported (Excluded) | Rotator Cuff Repair Cohort | P Valueb | |
|---|---|---|---|---|
| Patients, n | 89 | 251 | 1158 | |
| Age, y | 52.1 ± 8.8 | 56.8 ± 7.9 | 55.5 ± 9.9 | <.001 |
| Male-to-female ratio (% male) | 74:30 (71.2) | 159:92 (63.3) | 1085:632 (63.2) | .153 |
| Body mass index, kg/m2 | 33.3 ± 6.9 | 30.0 ± 5.8 | 31.1 ± 4.9 | <.001 |
| Smoking status, n | .367 | |||
| Current smoker | 19 | 10 | 159 | |
| Never smoked | 57 | 159 | 894 | |
| Former smoker | 13 | 52 | 293 | |
| Not reported | 30 | 371 | ||
| History of diabetes, n | .556 | |||
| Yes | 7 | 26 | 206 | |
| No | 82 | 225 | 1509 | |
| History of thyroid problem, n | .566 | |||
| Yes | 4 | 16 | 124 | |
| No | 85 | 235 | 1593 | |
| Symptom duration, mo | 11.8 ± 22.5 | 16.6 ± 58.3 | N.A. | .457 |
| Receiving workers’ compensation, n | 79 | 18 | 287 | <.001 |
| Baseline ASES score | 36.5 ± 24.9 | 35.2 ± 22.7 | 41.9 ± 17.6 | .633 |
| Baseline SANE score | 37.5 ± 30.3 | 40.7 ± 35.3 | 35.1 ± 23.2 | .417 |
| Baseline Constant score | 10.8 ± 9.3 | 12.8 ± 9.3 | 13.0 ± 6.7 | .065 |
aValues are expressed as mean ± SD unless otherwise indicated. ASES, American Shoulder and Elbow Surgeons; SANE, Single Assessment Numeric Evaluation; N.A., not available.
bP values were obtained by use of 1-way analysis of variance to compare 3 groups. Boldface indicates statistical significance.
Statistical Analysis
Statistical analysis was performed using RStudio software version 1.0.143 (R Foundation for Statistical Computing).47 RTW rates were analyzed for the final study population (N = 89) as well for subgroups of patients with sedentary, light, moderate, and heavy duties. Time to return to full activity was measured in months and was differentiated by ANOVA with Turkey post hoc analysis. Differences in RTW rates among patients with sedentary, light, moderate, and heavy work duties were calculated by use of the chi-square test. Univariate analysis on all collected preoperative variables was performed using chi-square and unpaired Student t tests. All variables with P < .20 were incorporated into a multivariate logistical regression model in order to calculate the association between those preoperative variables and patient RTW. Final significance of each variable was considered with P < .05. Odds ratios were calculated for all variables from regression analysis.
A nonparametric receiver operating characteristic (ROC) curve was plotted for each preoperative PROM score in determining future ability of a patient to achieve RTW at full duty. Area under the curve (AUC) analysis was performed to determine whether this association was significant. Prediction was considered acceptable if AUC > 0.7 and excellent if AUC > 0.8.4 Optimal cutoff values for MCID, SCB, and PASS were calculated for each PROM (ASES, subjective Constant, SANE, and HRQoL component scores) through use of the Youden index to maximize sensitivity and specificity, as has been previously demonstrated in the literature for determining ideal score thresholds to predict postoperative outcomes in shoulder surgery.52 A chi-square test was performed to determine whether there was a significant relationship between RTW at full duty and achieving MCID, SCB, and PASS.
Results
Demographics
The final cohort included 89 patients with complete data sets and working status. There existed differences in age, BMI, and proportion receiving workers’ compensation between the entire registry cohort, the cohort that did not report work status, and the final cohort with a complete data set. The final cohort was older (P < .001), had higher BMI (P < .001), and had a greater proportion of workers’ compensation recipients (P < .001) than both the entire registry cohort and the cohort without occupation status (Table 1). Baseline ASES, SANE, and subjective Constant scores did not significantly differ between the registry cohort and the final cohort with work status (P = .633, .417, and .065, respectively).
Surgical Repair
All patients underwent clinically indicated rotator cuff repair from 1 of 7 fellowship-trained sports medicine or fellowship-trained shoulder and elbow surgeons. Tear type (partial- vs full-thickness), tear size (massive16 vs nonmassive), number and nature of concomitant procedures, repair construct (single vs double row), and number of tendons torn were analyzed via univariate analysis to determine whether there were any significant differences among these clinical characteristics for included patients. In total, 76 patients had full-thickness tears and 13 had partial-thickness tears (P = .463). Concomitant procedures included distal clavicle excision (n = 15; 17%; P = .287), biceps tenodesis (n = 58; 65%; P ≥ .999), and labral debridement (n = 36; 40%; P = .450). All except 1 surgeon routinely performed subacromial decompression and acromioplasty with rotator cuff repair, so this was not incorporated into the analysis. Repaired massive cuff tears, as classified by DeOrio and Cofield,16 comprised 21 (24%) of the repairs (P = .144). We found that 10 repairs contained single-row anchors (11%), whereas 79 repairs were double-row repairs (89%) (P = .456). A mean ± SD of 1.4 ± 0.6 tendons were torn. There were 21 cases of 2-tendon tears (24%) and 6 cases of 3-tendon tears (7%). All remaining tears were single-tendon supraspinatus tears (70%). A total of 5 patients returned to the operating room after their indexed surgery. Of these, 2 patients received manipulation under anesthesia, 1 patient received a revision rotator cuff repair, 1 patient received lysis of adhesions with acromioplasty and distal clavicle excision, and 1 patient received a reverse total shoulder replacement.
Patient-Reported Outcome Measures— MCID, SCB, and PASS
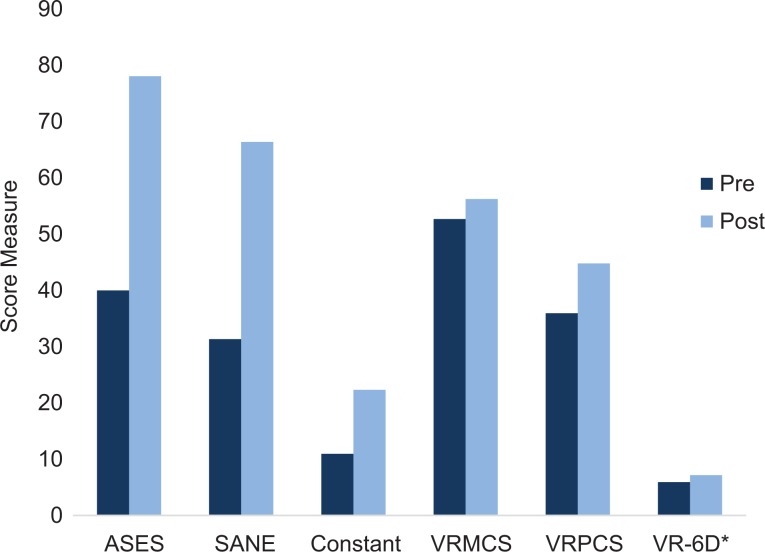
The ASES, subjective Constant, SANE, and HRQoL component scores (VRMCS and VRPCS) increased after rotator cuff surgery. The ASES score increased from a mean ± SD of 40.0 ± 17.1 to 78.0 ± 21.5 (P < .001). The SANE score increased from 31.3 ± 21.3 to 66.4 ± 30.7 (P < .001). The subjective Constant score increased from 11.0 ± 5.5 to 22.3 ± 8.7 (P < .001). The VRMCS increased from 52.7 ± 10.7 to 56.2 ± 8.6 (P = .164), and the VRPCS increased from 35.9 ± 6.3 to 44.8 ± 10.5 (P < .001). The VR-6D score increased from 0.6 ± 0.1 to 0.7 ± 0.1 (P < .001) (Figure 1). The calculated MCID, SCB, and PASS for the ASES score were 11.1, 17.5, and 86.7, respectively. The calculated MCID, SCB, and PASS for the subjective Constant score were 4.6, 5.5, and 23.3, respectively. These scores were established independently through use of nonparametric ROCs with the Youden index to maximize sensitivity and specificity and AUC analysis greater than 70% between patients who reported no change or unsatisfactory outcome and those who reported minimal or substantial change or satisfactory outcome (Figure 2).35
Figure 1.
Change in outcome measure before and after surgery. ASES, American Shoulder and Elbow Surgeons; SANE, Single Assessment Numeric Evaluation; VRMCS, Veterans RAND Mental Component Score; VRPCS, Veterans RAND Physical Component Score; VR-6D, Veterans RAND 6-Dimensions. *VR-6D graphically represented as 10 times the score for scale.
Figure 2.
Youden index estimate of minimal clinically important difference of the American Shoulder and Elbow Surgeons score in rotator cuff repair. AUC, area under the curve.
Work Outcomes
Overall, 67 (75.2%) patients returned to work at full duties at a mean ± SD of 6.6 ± 3.4 months after surgery. Workers who had heavy work duties were associated with the lowest RTW rate, although this was not statistically significant (P = .748). No statistical difference was found between the time required to return to full duty and the level of duty (P = .224) (Table 2). Achieving PASS, defined as having a greater change in PROMs than the established PASS for the ASES score, was associated with RTW at full duty in comparison with those who did not RTW at full duty (Table 3).
TABLE 2.
Return to Full-Duty Work as Stratified by Level of Dutya
| Level of Duty | Working Before RCR, n | Working After RCR, n | Rate of RTW, % | Time to RTW, mo, Mean ± SD |
|---|---|---|---|---|
| Sedentary | 3 | 3 | 100.0 | 7.3 ± 4.2 |
| Light | 25 | 21 | 84.0 | 6.2 ± 3.4 |
| Moderate | 31 | 24 | 77.4 | 7.0 ± 3.5 |
| Heavy | 30 | 19 | 63.3 | 6.6 ± 3.3 |
| Total | 89 | 67 | 75.2 | 6.6 ± 3.4 |
aRCR, rotator cuff repair; RTW, return to work.
TABLE 3.
Relationship Between Achieving MCID, SCB, and PASS for ASES and Constant Scores and Returning to Worka
| Metric | Light Duty | Moderate Duty | Heavy Duty | Overall |
|---|---|---|---|---|
| ASES score | ||||
| Achieving MCID (11.1) | .167 | ≥.999 | ≥.999 | .429 |
| Achieving SCB (17.5) | .222 | ≥.999 | ≥.999 | .452 |
| Achieving PASS (86.7) | .292 | .088 | .061 | .004 |
| Constant score | ||||
| Achieving MCID (4.6) | .118 | ≥.999 | ≥.999 | .523 |
| Achieving SCB (5.5) | .261 | ≥.999 | ≥.999 | .536 |
| Achieving PASS (23.3) | .245 | .039 | .074 | <.001 |
aValues are expressed as P values. Boldface indicates statistical significance (P < .05). Regarding change in ASES scores, achieving the cutoff value for PASS (86.7) was significantly associated with overall return to work (P = .004). Regarding change in Constant scores, achieving the cutoff value for PASS (23.3) was significantly associated with return to moderate duty work and return to overall work. ASES, American Shoulder and Elbow Surgeons; MCID, minimal clinically important difference; PASS, patient acceptable symptom state; SCB, substantial clinical benefit.
Univariate analysis of 23 variables found only workers’ compensation status and dominant-side injury to be significantly associated with not returning to work (P = .036 and P = .052, respectively). Subsequent multivariate analysis on significant variables revealed that injury or surgery to the dominant side was the only variable associated with inability to RTW (P = .030) (Table 4). Rotator cuff tear characteristics were not significantly associated with RTW.
TABLE 4.
Multivariate Analysis of Variables Associated With Return to Worka
| Univariate Regression, P Value | Multivariate Regression, P Value | Odds Ratio (95% CI) | |
|---|---|---|---|
| Workers’ compensation | .036 | .996 | NA |
| Dominant side injury | .052 | .030 | 0.057 (0.004-0.763) |
| Massive injury | .157 | .715 | 0.585 (0.052-6.54) |
aBoldface indicates statistical significance. NA, not applicable.
Predictive Outcome Scores for Return to Work
Prediction of return to sedentary work could not be performed because all patients with sedentary jobs were able to return to work. In the overall population, preoperative Veterans RAND scores were predictive of RTW at full duty (AUC, 70.4%). VRMCS greater than 53.3 had 66.7% specificity and 73.3% sensitivity in predicting RTW. In the groups with moderate and heavy duties, VRMCS demonstrated excellent predictive ability for RTW (AUC, 93.8% and 100.0%, respectively). The threshold was 53.4 and 63.1 for moderate and heavy duties, respectively. Scores greater than this threshold were highly predictive of RTW (Table 5).
TABLE 5.
Predictive Value of Preoperative Scores for Returning to Worka
| PROM Youden Estimate | Specificity, % | Sensitivity, % | AUC, % | |
|---|---|---|---|---|
| Light duty | ||||
| ASES score | 51.5 | 66.7 | 84.6 | 61.5 |
| SANE score | 40.4 | 100.0 | 33.3 | 50.0 |
| VRMCS | 59.3 | 100 | 40 | 60.0 |
| VRPCS | 38.4 | 50.0 | 100.0 | 65.0 |
| VR-6D score | 0.6 | 100.0 | 40.0 | 60.0 |
| Moderate duty | ||||
| ASES score | 49.2 | 100.0 | 71.4 | 77.8 |
| SANE score | 44.3 | 75.0 | 85.7 | 81.5 |
| VRMCS | 53.4 | 100.0 | 87.5 | 93.8 |
| VRPCS | 34.3 | 100.0 | 62.5 | 75.0 |
| VR-6D score | 0.6 | 100.0 | 62.5 | 75.0 |
| Heavy duty | ||||
| ASES score | 26.8 | 33.3 | 84.6 | 45.3 |
| SANE score | 50.2 | 100.0 | 38.5 | 57.2 |
| VRMCS | 63.1 | 100.0 | 100.0 | 100.0 |
| VRPCS | 35.6 | 66.7 | 100.0 | 66.7 |
| VR-6D score | 0.7 | 100.0 | 100.0 | 100.0 |
| Overall population | ||||
| ASES score | 51.6 | 60 | 80 | 62.1 |
| SANE score | 30.2 | 75.0 | 53.1 | 59.8 |
| VRMCS | 53.3 | 66.7 | 73.3 | 70.4 |
| VRPCS | 35.4 | 66.7 | 53.3 | 51.9 |
| VR-6D score | 0.6 | 100 | 40 | 60.0 |
aASES, American Shoulder and Elbow Surgeons; AUC, area under the curve; PROM, patient-reported outcome measure; SANE, Single Assessment Numeric Evaluation; VRMCS, Veterans RAND Mental Component Score; VRPCS, Veterans RAND Physical Component Score; VR-6D, Veterans RAND 6-Dimensions. Boldfaced values signify AUC >70%.
Discussion
In this study, rotator cuff repairs resulted in a 75.2% rate of RTW at full duty at a mean ± SD of 6.6 ± 3.4 months from surgery. Increasing level of intensity of work corresponded with a lower probability of returning to full duties, although this was not statistically significant. Higher preoperative mental status HRQoL scores were most predictive of overall RTW, while achieving the PASS was the only measure of clinical significance associated with RTW; specifically, meeting the PASS threshold of ASES and Constant scores was significantly associated with RTW at full duty. For moderate-intensity workers in particular, both shoulder-specific and HRQoL preoperative questionnaire scores were predictive of RTW. However, our original hypothesis that shoulder-specific questionnaires can predict the ability to return to preoperative employment was rejected, since only the mental component score of the VR-12 HRQoL questionnaire (ie, the VRMCS) was found to affect RTW status overall.
RTW after rotator cuff repair was 88.5% in a previous investigation.5 Although a smaller percentage of patients in the present study achieved RTW, our cohort exhibited faster RTW. This may reflect improvements in a number of potentially influential factors, such as surgical techniques, rehabilitation protocols, expectations with regard to successful rotator cuff surgery, and monitoring of the overall recovery process by the surgeon and rehabilitation specialists within the past 8 years.5 However, it is likely that differences in patient population characteristics may also have affected RTW outcomes. In the previous study, 40 of 78 (51.3%) patients reported working heavy-duty occupations preoperatively, compared with 30 of 89 (33.7%) in the current study. The previous study also included only patients insured by workers’ compensation. The decreased proportion of heavy-duty workers and workers’ compensation recipients may have affected time to RTW in the present study. The fact that achieving the PASS was associated with RTW at full duty suggests that RTW is an integral part of patient satisfaction after arthroscopic rotator cuff repair. The MCID and SCB are important measures of psychometric outcomes; however, they are largely reliant on the anchor question that is asked. Specifically, in our patient population, the anchor questions were geared toward the global function and pain domains, and these may not reflect improvements needed to achieve RTW. This finding is helpful for further refining our understanding of a clinically significant outcome. Meaningful outcomes can be achieved even in the absence of meeting RTW functional demands. To this end, PASS may be the more appropriate measure of clinical significance with regard to assessing outcome in a working population.
We found that preoperative scores that reflected better mental health significantly predicted the propensity to RTW at full duty. As the level of duty (labor) increased, the influence of preoperative mental health scores similarly increased, supporting the concept that psychosocial health is vital to musculoskeletal rehabilitation and successful outcomes after surgery. Calculated VRMCS is based on algorithms to demonstrate associations with mental health disorders such as depression and alcohol use disorders.25,26 Psychosocial factors have long been understood to influence outcomes after intervention in cardiac, orthopaedic, gynecologic, urologic, gastrointestinal, and transplant surgeries.18,31,35,42,43 Specifically, these factors include mood, attitude toward surgery, social support, coping, and personality. The association between mental health and RTW has not been previously demonstrated among patients undergoing rotator cuff repair, but our findings mirror previous literature regarding psychological influences on return to sport in anterior cruciate ligament reconstruction.1–3,35 A previous study on 169 patients with full-thickness rotator cuff tears demonstrated that a higher 36-Item Short Form Health Survey (SF-36) mental component score was significantly associated with lower preoperative visual analog scale scores for pain and function and greater ASES and Simple Shoulder Test scores. The association between low mental health score and failed RTW may be explained by diminished mental resiliency in these patients, although this was not specifically tested. Additionally, a low mental health score may be a proxy for other social determinants that may influence the ability for a patient to RTW after rotator cuff repair. It is also plausible that patients with lower preoperative mental health scores have lower preoperative expectations and self-fulfill their expectations for a lower postoperative outcome. High patient expectations have previously been associated with improved postoperative scores after rotator cuff repair.39 Furthermore, poor SF-36 mental component scores were associated with greater concerns before surgery, which reflected lower expectations.39
It is widely accepted that larger tear sizes are associated with less predictable and overall worse outcomes and greater incidence of retear.8,20,29 However, interestingly, this factor did not adversely affect our patients’ ability to return to the workforce. RTW is a relatively short-term outcome since it occurs at less than 1 year after surgery to repair the rotator cuff. A significant portion of patients will develop retears between 12 and 15 months after surgery that may become symptomatic at a later date.10 Further investigation into specific duty hazards that could potentially predispose patients to developing retears of the rotator cuff after RTW, such as repetitive lifting or cumulative trauma, would be clinically relevant. Cumulative trauma disorders are well-recognized orthopaedic conditions among working populations, particularly with respect to carpal tunnel syndrome and De Quervain tenosynovitis.11,41,53 With a high prevalence of rotator cuff repairs in younger members of the workforce (23.8-198 per 100,000 person-years at risk),17,50 dedicated research into these areas may potentially help patients maintain their work status postoperatively. Although the ability to maintain level of work is an outcome of interest, this study is underpowered to perform such an analysis.
A significant limitation within this study is that although data were collected prospectively, the patients were followed up to only their latest clinic visit. If their work status or capacity changed at any point beyond their final clinic visit or 1 postoperative year, we were unable to capture or analyze those findings. However, incorporating longer follow-up within this analysis would introduce additional variables that may be independent of shoulder surgery, such as work performance, retirement, and personal reasons for changing or discontinuing work. Additionally, we were unable to perform our analysis of sedentary workers to determine whether achieving MCID, SCB, and PASS predicted RTW, since all patients in this category successfully returned to employment. Some patients who have rotator cuff repair may be able to work shortly after their surgery because they perform sedentary work. Therefore, using PROM scores as a predictive tool to determine the likelihood of whether sedentary patients will return to their occupations may not be useful clinically. Additionally, the final population size was limited to only those patients with verified pre- and postoperative occupational status. At the study institution, the occupational status of all patients who receive workers’ compensation is documented before surgery and also during postoperative follow-up, as per standard medicolegal practices. However, time off and RTW are documented based on individual surgeon preference for patients not receiving workers’ compensation.
The authors recognize that selection bias may arise from the study population being composed of predominantly workers’ compensation recipients, in addition to non–workers’ compensation recipients with a verified occupational status, since all patients who have rotator cuff repair may not fall exclusively within these parameters. Comparisons of baseline demographic factors were made between the final study population and the overall population available in order to detect any potentially significant differences, which demonstrated that the final patient cohort was slightly younger and of higher BMI than those not included.
Conclusion
The majority of patients undergoing rotator cuff repair can expect to RTW within 8 months after surgery. Preoperative mental health scores can predict future RTW, supporting the concept that mental health plays a significant role in the clinical and work-related outcomes after rotator cuff repair surgery.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: G.L.C. has received research support from Arthrex and educational support from Medwest and Smith & Nephew. J.N.L. has received educational support from Smith & Nephew. B.J.C. has received consulting fees from Arthrex, Genzyme, Pacira Pharmaceuticals, Anika Therapeutics, Geistlich Pharma, Vericel, Bioventus, Zimmer, and Smith & Nephew; educational support from Arthrex and Pacira Pharmaceuticals; royalties from Arthrex and DJO; nonconsulting fees from Arthrex, Carticept Medical, and LifeNet Health; and hospitality payments from Aesculap/B.Braun, DePuy, and GE Healthcare. B.F. has received consulting fees from Sonoma Orthopedics and Stryker, honorarium from Arthrosurface, and educational support from Medwest. A.A.R. has received consulting fees and royalties from Arthrex. N.N.V. has received consulting fees from Smith & Nephew and Medacta USA, royalties from Smith & Nephew, nonconsulting fees from Pacira Pharmaceuticals, educational support from Medwest, and hospitality payments from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Rush University Medical Center Institutional Review Board (No. 14120505-IRB01-AM0).
References
- 1. Ardern CL, Osterberg A, Tagesson S, Gauffin H, Webster KE, Kvist J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med. 2014;48(22):1613–1619. [DOI] [PubMed] [Google Scholar]
- 2. Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2013;41(7):1549–1558. [DOI] [PubMed] [Google Scholar]
- 3. Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. Am J Sports Med. 2015;43(4):848–856. [DOI] [PubMed] [Google Scholar]
- 4. Berliner JL, Brodke DJ, Chan V, SooHoo NF, Bozic KJ. John Charnley Award: preoperative patient-reported outcome measures predict clinically meaningful improvement in function after THA. Clin Orthop Relat Res. 2016;474(2):321–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bhatia S, Piasecki DP, Nho SJ, et al. Early return to work in workers’ compensation patients after arthroscopic full-thickness rotator cuff repair. Arthroscopy. 2010;26(8):1027–1034. [DOI] [PubMed] [Google Scholar]
- 6. Bishop J, Klepps S, Lo IK, Bird J, Gladstone JN, Flatow EL. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg. 2006;15(3):290–299. [DOI] [PubMed] [Google Scholar]
- 7. Bulhoff M, Sattler P, Bruckner T, Loew M, Zeifang F, Raiss P. Do patients return to sports and work after total shoulder replacement surgery? Am J Sports Med. 2015;43(2):423–427. [DOI] [PubMed] [Google Scholar]
- 8. Chalmers PN, Granger E, Nelson R, Yoo M, Tashjian RZ. Factors affecting cost, outcomes, and tendon healing after arthroscopic rotator cuff repair. Arthroscopy. 2018;34(5):1393–1400. [DOI] [PubMed] [Google Scholar]
- 9. Cho C-H, Song K-S, Hwang I, Warner JJP. Does rotator cuff repair improve psychologic status and quality of life in patients with rotator cuff tear? Clin Orthop Relat Res. 2015;473(11):3494–3500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chona DV, Lakomkin N, Lott A, et al. The timing of retears after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2017;26(11):2054–2059. [DOI] [PubMed] [Google Scholar]
- 11. Cohen RB, Williams GRJ. Impingement syndrome and rotator cuff disease as repetitive motion disorders. Clin Orthop Relat Res. 1998;351:95–101. [PubMed] [Google Scholar]
- 12. Cole BJ, McCarty LP, III, Kang RW, Alford W, Lewis PB, Hayden JK. Arthroscopic rotator cuff repair: prospective functional outcome and repair integrity at minimum 2-year follow-up. J Shoulder Elbow Surg. 2007;16(5):579–585. [DOI] [PubMed] [Google Scholar]
- 13. Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012;94(3):227–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 15. Day M, Westermann R, Duchman K, et al. Comparison of short-term complications after rotator cuff repair: open versus arthroscopic. Arthroscopy. 2018;34(4):1130–1136. [DOI] [PubMed] [Google Scholar]
- 16. DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am. 1984;66(4):563–567. [PubMed] [Google Scholar]
- 17. Ensor KL, Kwon YW, Dibeneditto MR, Zuckerman JD, Rokito AS. The rising incidence of rotator cuff repairs. J Shoulder Elbow Surg. 2013;22(12):1628–1632. [DOI] [PubMed] [Google Scholar]
- 18. Fiabane E, Giorgi I, Candura SM, Argentero P. Return to work after coronary revascularization procedures and a patient’s job satisfaction: a prospective study. Int J Occup Med Environ Health. 2015;28(1):52–61. [DOI] [PubMed] [Google Scholar]
- 19. Garcia GH, Mahony GT, Fabricant PD, et al. Sports- and work-related outcomes after shoulder hemiarthroplasty. Am J Sports Med. 2016;44(2):490–496. [DOI] [PubMed] [Google Scholar]
- 20. Gulotta LV, Nho SJ, Dodson CC, Adler RS, Altchek DW, MacGillivray JD. Prospective evaluation of arthroscopic rotator cuff repairs at 5 years, part II: prognostic factors for clinical and radiographic outcomes. J Shoulder Elbow Surg. 2011;20(6):941–946. [DOI] [PubMed] [Google Scholar]
- 21. Guyatt GH, Osoba D, Wu AW, Wyrwich KW, Norman GR. Methods to explain the clinical significance of health status measures. Mayo Clin Proc. 2002;77(4):371–383. [DOI] [PubMed] [Google Scholar]
- 22. Henn RF, III, Kang L, Tashjian RZ, Green A. Patients’ preoperative expectations predict the outcome of rotator cuff repair. J Bone Joint Surg Am. 2007;89(9):1913–1919. [DOI] [PubMed] [Google Scholar]
- 23. Ide J, Maeda S, Takagi K. A comparison of arthroscopic and open rotator cuff repair. Arthroscopy. 2005;21(9):1090–1098. [DOI] [PubMed] [Google Scholar]
- 24. Jevsevar DS, Sanders J, Bozic KJ, Brown GA. An introduction to clinical significance in orthopaedic outcomes research. JBJS Rev. 2015;3(5). [DOI] [PubMed] [Google Scholar]
- 25. Kazis LE, Lee A, Spiro A, III, et al. Measurement comparisons of the medical outcomes study and Veterans SF-36 health survey. Health Care Financ Rev. 2004;25(4):43–58. [PMC free article] [PubMed] [Google Scholar]
- 26. Kazis LE, Miller DR, Skinner KM, et al. Patient-reported measures of health: the Veterans Health Study. J Ambul Care Manage. 2004;27(1):70–83. [DOI] [PubMed] [Google Scholar]
- 27. Kazis LE, Selim A, Rogers W, Ren XS, Lee A, Miller DR. Dissemination of methods and results from the Veterans Health Study: final comments and implications for future monitoring strategies within and outside the Veterans Healthcare System. J Ambul Care Manage. 2006;29(4):310–319. [DOI] [PubMed] [Google Scholar]
- 28. Kweon C, Gagnier JJ, Robbins CB, Bedi A, Carpenter JE, Miller BS. Surgical versus nonsurgical management of rotator cuff tears: predictors of treatment allocation. Am J Sports Med. 2015;43(10):2368–2372. [DOI] [PubMed] [Google Scholar]
- 29. Lambers Heerspink FO, Dorrestijn O, van Raay JJAM, Diercks RL. Specific patient-related prognostic factors for rotator cuff repair: a systematic review. J Shoulder Elbow Surg. 2014;23(7):1073–1080. [DOI] [PubMed] [Google Scholar]
- 30. McElvany MD, McGoldrick E, Gee AO, Neradilek MB, Matsen FA., III Rotator cuff repair: published evidence on factors associated with repair integrity and clinical outcome. Am J Sports Med. 2015;43(2):491–500. [DOI] [PubMed] [Google Scholar]
- 31. Mehrdad R, Ghadiri Asli N, Pouryaghoub G, Saraei M, Salimi F, Nejatian M. Predictors of early return to work after a coronary artery bypass graft surgery (CABG). Int J Occup Med Environ Health. 2016;29(6):947–957. [DOI] [PubMed] [Google Scholar]
- 32. Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons standardized shoulder assessment form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587–594. [DOI] [PubMed] [Google Scholar]
- 33. Monrad N, Ganestam A, Kallemose T, Barfod KW. Alarming increase in the registration of degenerative rotator cuff-related lesions: a nationwide epidemiological study investigating 244,519 patients. Knee Surg Sports Traumatol Arthrosc. 2018;26(1):188–194. [DOI] [PubMed] [Google Scholar]
- 34. Nwachukwu BU, Chang B, Fields K, et al. Defining the “substantial clinical benefit” after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med. 2017;45(6):1297–1303. [DOI] [PubMed] [Google Scholar]
- 35. Nwachukwu BU, Chang B, Voleti PB, et al. Preoperative short form health survey score is predictive of return to play and minimal clinically important difference at a minimum 2-year follow-up after anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(12):2784–2790. [DOI] [PubMed] [Google Scholar]
- 36. Nwachukwu BU, Fields K, Chang B, Nawabi DH, Kelly BT, Ranawat AS. Preoperative outcome scores are predictive of achieving the minimal clinically important difference after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med. 2017;45(3):612–619. [DOI] [PubMed] [Google Scholar]
- 37. Nwachukwu BU, Hamid KS, Bozic KJ. Measuring value in orthopaedic surgery. JBJS Rev. 2013;1(1). [DOI] [PubMed] [Google Scholar]
- 38. Nwachukwu BU, Runyon RS, Kahlenberg CA, Gausden EB, Schairer WW, Allen AA. How are we measuring clinically important outcome for operative treatments in sports medicine? Phys Sportsmed. 2017;45(2):159–164. [DOI] [PubMed] [Google Scholar]
- 39. Oh JH, Yoon JP, Kim JY, Kim SH. Effect of expectations and concerns in rotator cuff disorders and correlations with preoperative patient characteristics. J Shoulder Elbow Surg. 2012;21(6):715–721. [DOI] [PubMed] [Google Scholar]
- 40. Paloneva J, Lepola V, Aarimaa V, Joukainen A, Ylinen J, Mattila VM. Increasing incidence of rotator cuff repairs—a nationwide registry study in Finland. BMC Musculoskelet Disord. 2015;16:189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Rempel DM, Harrison RJ, Barnhart S. Work-related cumulative trauma disorders of the upper extremity. JAMA. 1992;267(6):838–842. [PubMed] [Google Scholar]
- 42. Rosenberger PH, Jokl P, Ickovics J. Psychosocial factors and surgical outcomes: an evidence-based literature review. J Am Acad Orthop Surg. 2006;14(7):397–405. [DOI] [PubMed] [Google Scholar]
- 43. Schultz IZ, Crook J, Meloche GR, et al. Psychosocial factors predictive of occupational low back disability: towards development of a return-to-work model. Pain. 2004;107(1-2):77–85. [DOI] [PubMed] [Google Scholar]
- 44. Selim AJ, Rogers W, Qian SX, Brazier J, Kazis LE. A preference-based measure of health: the VR-6D derived from the Veterans Rand 12-Item Health Survey. Qual Life Res. 2011;20(8):1337–1347. [DOI] [PubMed] [Google Scholar]
- 45. Severud EL, Ruotolo C, Abbott DD, Nottage WM. All-arthroscopic versus mini-open rotator cuff repair: a long-term retrospective outcome comparison. Arthroscopy. 2003;19(3):234–238. [DOI] [PubMed] [Google Scholar]
- 46. Stewart AL, Ware JE. Measuring Functioning and Well-Being: The Medical Outcomes Study Approach. Durham, NC: Duke University Press; 1992. [Google Scholar]
- 47. Team RC. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. [Google Scholar]
- 48. US Department of Labor Office of Administrative Law Judges Law Library. www.oalj.dol.gov/PUBLIC/DOT/REFERENCES/DOTAPPC.HTM. Accessed April 1, 2019.
- 49. Werner BC, Chang B, Nguyen JT, Dines DM, Gulotta LV. What change in American Shoulder and Elbow Surgeons score represents a clinically important change after shoulder arthroplasty? Clin Orthop Relat Res. 2016;474(12):2672–2681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. White JJE, Titchener AG, Fakis A, Tambe AA, Hubbard RB, Clark DI. An epidemiological study of rotator cuff pathology using the Health Improvement Network database. Bone Joint J. 2014;96-B(3):350–353. [DOI] [PubMed] [Google Scholar]
- 51. Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales: outcomes measures after shoulder surgery. Am J Sports Med. 1999;27(2):214–221. [DOI] [PubMed] [Google Scholar]
- 52. Wong SE, Zhang AL, Berliner JL, Ma CB, Feeley BT. Preoperative patient-reported scores can predict postoperative outcomes after shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25(6):913–919. [DOI] [PubMed] [Google Scholar]
- 53. Zakaria D, Robertson J, MacDermid J, Hartford K, Koval J. Work-related cumulative trauma disorders of the upper extremity: navigating the epidemiologic literature. Am J Ind Med. 2002;42(3):258–269. [DOI] [PubMed] [Google Scholar]
- 54. Zhang AL, Montgomery SR, Ngo SS, Hame SL, Wang JC, Gamradt SC. Analysis of rotator cuff repair trends in a large private insurance population. Arthroscopy. 2013;29(4):623–629. [DOI] [PubMed] [Google Scholar]
- 55. Zuke WA, Leroux TS, Gregory BP, et al. Establishing maximal medical improvement after arthroscopic rotator cuff repair. Am J Sports Med. 2018;46(6):1000–1007. [DOI] [PubMed] [Google Scholar]