Abstract
Kimura's disease was first described by Kimura and Sceto in China in 1937. Kimura disease is a chronic inflammatory disorder of idiopathic etiology. The clinical presentation of Kimura's disease is painless solitary or multiple subcutaneous nodules, asymmetric, mostly in the head and neck region with often association with lymphadenopathy. Typically, the nodules are found on preauricular, submandibular, and popliteal regions as well as oral cavity, larynx, and parotid glands. In the present report, we describe a case of a 27-year-old male presented to our hospital with history of right neck and lip swelling for 10 days. In the history, the patient mentioned that he had bloody diarrhea four to six times day and he lost 10 kg in 1 month. The specimen was sent for histopathological examination which showed the lymph node architecture is preserved with significant increase number of eosinophils which is consistent with Kimura's disease. There is no agreement on the management aspects in Kimura's disease so far. The primary treatment for Kimura's disease includes surgical resection. Additional medical therapy including regional or systemic steroid therapy, cytotoxic therapy, and radiation has also been utilized. Considered as an inflammatory process, the disease has an excellent prognosis, although it may recur locally and wax and wane over time.
Keywords: IBD, inflammatory, Kimura, lung, lymphadenopathy, mepolizumab, rare, Saudi Arabia, ulcerative colitis
Introduction
Kimura's disease was first described by Kimura and Sceto in China in 1937. Kimura's disease is a chronic inflammatory disorder of idiopathic etiology. The clinical presentation of Kimura's disease is painless solitary or multiple subcutaneous nodules, asymmetric, mostly in the head and neck region with often association with lymphadenopathy. Typically, the nodules are found on preauricular, submandibular, and popliteal regions as well as oral cavity, larynx, and parotid glands.
This case report focused on the discussion, presentation, investigation, and treatment of Kimura's disease.
Patient Information
A 27-year-old Saudi male patient known case of ulcerative colitis diagnosed 8 years ago based on history, clinical presentation, and histological features on mesalamine and prednisolone with poor compliance to medications. The patient presented to our hospital complaining of right neck and lip swelling for 10 days. In the history, the patient mentioned that he had bloody diarrhea four to six times day and he lost 10 kg in 1 month.
Clinical Findings
Clinically, there is a swelling in the right submandibular and anterior cervical lymph nodes. The masses were painless, firm, subcutaneous, nontender measured 2 × 3 cm and 1 × 1 cm, respectively.
Diagnostic Assessment
Biochemical tests showed an eosinophilic count of 23% (EAC: 3200 eosinophils/μL), immunoglobulin E (IgE) 339 g/L (normal <200). Liver and renal functions tests were within normal.
Computed tomography (CT) of the neck, chest, abdomen, and pelvis showed multiple homogeneous enhanced significant enlarged lymph nodes seen at both submandibular regions on both sides of the neck [Figure 1]. CT also showed tree in bud pattern in the anterior segment of the right upper lobe and middle lobe of the lung with mild cervical lymphadenopathy [Figure 2].
Figure 1.
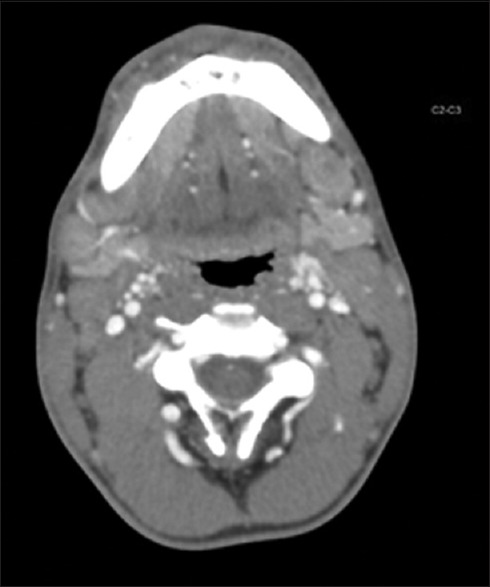
Axial CT scan of the neck demonstrate enlarged bilateral cervical LN
Figure 2.
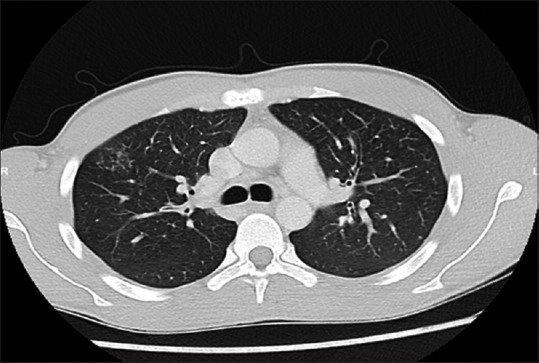
Axial CT scan of the chest (lung window) shows tree-in-bud appearance
Colonoscopy was performed which showed pancolitis up to the cecum with MAYO score of 2 and random biopsies were taken [Figure 3].
Figure 3.
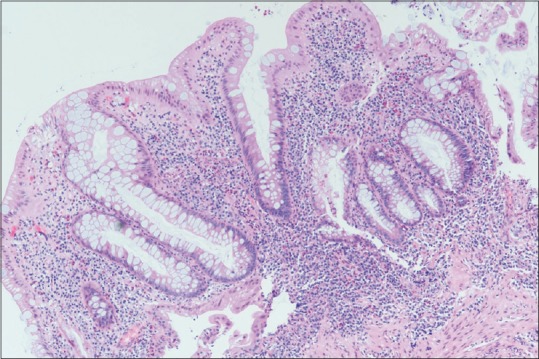
Histopathology of sigmoid colon sample shows chronic active colitis
Cervical lymph node true-cut biopsy was performed [Figure 4]. The specimen was sent for histopathological examination that showed the lymph node architecture is preserved with significant increase number of eosinophils which is consistent with Kimura's disease.
Figure 4.
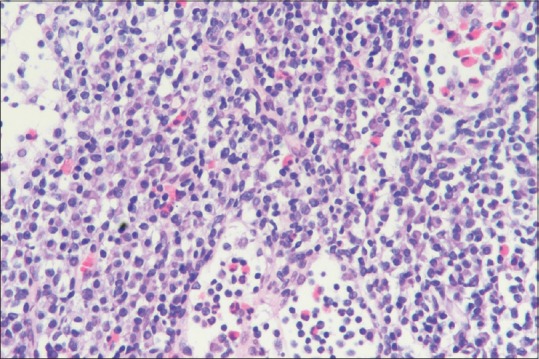
Lymph node architecture is preserved with significant increase number of eosinophils
Bone marrow aspiration and biopsy were performed and reported as there is no evidence of marrow infiltration by malignant lymphoma.
With correlation of all these finding diagnoses of Kimura's disease was established.
Therapeutic Intervention
The patient was discharged on prednisolone 40 mg once daily by mouth, for 10 days then tapered down by 5 mg every 2 weeks, azathioprine 75 mg po od, Levocetirizine 5 mg po od, Montelukast 10 mg po od, and discontinue the mesalamine with follow-up in the clinic with CT neck, chest, abdomen, and pelvis after 2 months.
Follow-up and Outcomes
During the follow-up in the clinic the patient developed bloody diarrhea four times per day after stopping of steroid. CT neck, chest, abdomen, and pelvis showed no enlarged lymph nodes in the body and his IgE level was 274 g/L. Azathioprine was increased to 125 mg po od, mesalamine 3 gm po od and anti-immunoglobulin E medications was started, mepolizumab 100 mg SC every 4 weeks.
After 2 and 3 months follow-ups, the patient has no bloody diarrhea, no abdominal pain, no neck or lips swelling, and his weight was increased by 2 kg.
Clinical exam for head and neck lymph nodes was negative for lymphadenopathy. CT neck, chest, abdomen, and pelvis again showed no enlarged lymph nodes in the body.
Discussion
Kimura's disease was first described by Kimura and Sceto in China in 1937.[1]
Kimura's disease is a chronic inflammatory disorder of idiopathic etiology that presents as painless lymphadenopathy or subcutaneous masses in the head and neck region.[2]
The etiology remains unknown; however, an allergic or autoimmune reaction to an unknown stimulus, or a viral or parasitic or infection, which would alter T lymphocyte regulation or induce a type I immunoallergic reaction have been proposed.[3,4]
Kimura's disease generally not only affects Asian men, but also non-Asians were frequently reported in the literature.[2,5,6,7]
Controversy has existed in the literature regarding whether angiolymphoid hyperplasia with eosinophilia (ALHE) and Kimura's disease are the same entity. However, the two conditions can distinguish based on clinical and histopathologic characteristics.[5,7]
The clinical presentation of Kimura's disease is painless solitary or multiple subcutaneous nodules, asymmetric, mostly in the head and neck region with often association with lymphadenopathy. Typically, the nodules are found on preauricular, submandibular, and popliteal regions as well as oral cavity, larynx, and parotid glands.[2,3,5]
They are rarely reported in other localizations like eyelids, lacrimal glands, orbit, axilla, groin, forearm, and kidneys.[1,8,9]
The differential diagnosis includes malignant disorder (acute lymphocytic leukemia, T-cell lymphoma, Kaposi sarcoma, Hodgkin's lymphoma, or parotid tumor), ALHE, Langerhans cell histiocytosis, florid follicular hyperplasia, and Castleman disease. Kimura's disease may be easily mistaken for a malignant disorder because of a mass localized in the parotid gland and associating with lymphadenopathy.[3,10,11,12,13]
Histologically, Kimura's disease comprised preserved lymph node architecture with reactive and florid germinal centers. Eosinophilic infiltration, lysis of the follicles, and occasionally microabscesses vascular proliferation are also present.[2,5,14,15]
The pathogenesis of Kimura's disease and ulcerative colitis is yet unknown. However, the development of these disorders may involve a systemic immune disorder.[6,16]
There is no agreement on the management aspects in Kimura's disease so far. The primary treatment for Kimura disease includes surgical resection. Additional medical therapy including regional or systemic steroid therapy, cytotoxic therapy, and radiation has also been utilized. Considered as an inflammatory process, the disease has an excellent prognosis, although it may recur locally and wax and wane over time.[11,17,18,19]
Patient Perspective
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Gregory X, Soon NI, Nur Aklina R. A rare case of inguinal kimura disease. Med J Malaysia. 2018;73:326–7. [PubMed] [Google Scholar]
- 2.Chen H, Thompson LDR, Aguilera NSI, Abbondanzo SL. Kimura disease: A clinicopathologic study of 21 cases. Am J Surg Pathol. 2004;28:505–13. doi: 10.1097/00000478-200404000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Abuel-Haija M, Hurford MT. Kimura disease. Arch Pathol Lab Med. 2007;131:650–1. doi: 10.5858/2007-131-650-KD. [DOI] [PubMed] [Google Scholar]
- 4.Jang K-A, Ahn S-J, Choi J-H, Sung KJ, Moon KC, Koh JK, et al. Polymerase chain reaction (PCR) for human herpesvirus 8 and heteroduplex PCR for clonality assessment in angiolymphoid hyperplasia with eosinophilia and Kimura's disease. J Cutan Pathol. 2001;28:363–7. doi: 10.1034/j.1600-0560.2001.280705.x. [DOI] [PubMed] [Google Scholar]
- 5.Drouillard M, Steve M, Ranoarivony T, Souraud JB. Kimura's disease in a 50-year-old Tunisian man. Eur Ann Otorhinolaryngol Head Neck Dis. 2017;134:127–1. doi: 10.1016/j.anorl.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 6.Sanjushree D, Debasis M, Subhajit H, Kaushik D, Tapan G, Sulekha G. A case of Angiolymphoid hyperplasia with eosinophilia in proximal ascending colon mimicking colon carcinoma. Bangladesh Journal of Medical Science. 2018;17:158–60. [Google Scholar]
- 7.Osuch-Wójcikiewicz E, Bruzgielewicz A, Lachowska M, Wasilewska A, Niemczyk K. Kimura's Disease in a Caucasian Female: A Very Rare Cause of Lymphadenopathy. Case Rep Otolaryngol. 2014;2014:415865. doi: 10.1155/2014/415865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoganathan P, Meyer DR, Farber MG. Bilateral lacrimal gland involvement with Kimura disease in an African American male. Arch Ophthalmol. 2004;122:917–9. doi: 10.1001/archopht.122.6.917. [DOI] [PubMed] [Google Scholar]
- 9.Othman SK, Daud KM, Othman NH. Kimura's disease: A rare cause of nephrotic syndrome with lymphadenopathy. Malays J Med Sci. 2011;18:88–90. [PMC free article] [PubMed] [Google Scholar]
- 10.Don DM, Ishiyama A, Johnstone AK, Fu Y-S, Abemayor E. Angiolymphoid hyperplasia with eosinophilia and vascular tumors of the head and neck. Am J Otolaryngol. 1996;17:240–5. doi: 10.1016/s0196-0709(96)90088-5. [DOI] [PubMed] [Google Scholar]
- 11.Shalini K, Rojan K, Remesh B, Lilly M. Recurrent Kimura's disease successfully treated with steroids and cetirizine? International Surgery Journal. 2016:947–9. Doi: 10.18203/2349-2902.isj20161173. [Google Scholar]
- 12.Chen QL, Dwa S, Gong ZC, Abasi K, Ling B, Liu H, et al. Kimura's disease: Risk factors of recurrence and prognosis. Int J Clin Exp Med. 2015;8:21414–20. [PMC free article] [PubMed] [Google Scholar]
- 13.Choi HJ. Kimura disease presenting as forehead soft mass. J Craniofac Surg. 2016;27:823–4. doi: 10.1097/SCS.0000000000002595. [DOI] [PubMed] [Google Scholar]
- 14.Sun QF, Xu DZ, Pan SH, Ding JG, Xue ZQ, Miao CS, et al. Kimura disease: Review of the literature. Intern Med J. 2008;38:668–72. doi: 10.1111/j.1445-5994.2008.01711.x. [DOI] [PubMed] [Google Scholar]
- 15.Sherpa M, Lamichaney R, Roy AD. Kimura's disease: A diagnostic challenge experienced with cytology of postauricular swelling with histopathological relevance. J Cytol. 2016;33:232–5. doi: 10.4103/0970-9371.190453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shimamoto C, Takao Y, Hirata I, Ohshiba S. Kimura's disease (angiolymphoid hyperplasia with eosinophilia) associated with ulcerative colitis. Gastroenterol Jpn. 1993;28:298–303. doi: 10.1007/BF02779234. [DOI] [PubMed] [Google Scholar]
- 17.Ye P, Ma DQ, Yu GY, Gao Y, Peng X. Comparison of the efficacy of different treatment modalities for Kimura's disease. Int J Oral Maxillofac Surg. 2017;46:350–4. doi: 10.1016/j.ijom.2016.08.013. [DOI] [PubMed] [Google Scholar]
- 18.Birol A, Bozdoğan Ö, Keleş H, Kazkayasi M, Bagci Y, Kara S, et al. Kimura's disease in a Caucasian male treated with cyclosporine. Int J Dermatol. 2005;44:1059–60. doi: 10.1111/j.1365-4632.2004.02527.x. [DOI] [PubMed] [Google Scholar]
- 19.Ma X-R, Xin S-J, Ouyang T-X, Ma Y-T, Chen W-Y, Chang M-L. Successful treatment of Kimura's disease with leflunomide and methylprednisolone: A case report. Int J Clin Exp Med. 2014;7:2219–22. [PMC free article] [PubMed] [Google Scholar]


