Abstract
Background:
The popularity of e-cigarettes is increasing rapidly worldwide and advertisements for such products are becoming ubiquitous in the media. Health concerns and smoking cessation are the most commonly reported reasons for traditional tobacco smokers to shift to e-cigarettes. As a result, the global market for e-cigarettes is on the rise. However, they are still a potential cause for many diseases.
Methods:
This is a cross-sectional study carried out at Qassim University in Buraydah, Saudi Arabia. A prevalidated questionnaire was distributed to medical students in April 2018 to evaluate the experience, knowledge, and awareness of e-cigarettes among the participants.
Results:
About one in ten students confirmed having smoked an e-cigarette. There was no significant relationship between e-cigarette users and demographic factors, such as gender, academic level, or age. However, the study showed a significant association between e-cigarette smoking and having an e-cigarette smoker among family members or friends. Most students 71.9% were not sure whether e-cigarettes were approved by the Food and Drug Administration (FDA) for smoking cessation. Only 23.3% of those surveyed believed that e-cigarettes can help in smoking cessation, whereas only 11% said that they would recommend it for a patient. On the contrary, 49.6% agreed that e-cigarettes are addictive. In response to another question, 92% reported receiving no education in medical school about e-cigarettes.
Conclusion:
Our study showed that medical students lacked knowledge about e-cigarettes. Therefore, more studies are needed to raise awareness about e-cigarettes, especially since the habit of using e-cigarettes is invading our society.
Keywords: E-cigarettes, electronic cigarettes, medical students, smoking, smoking cessation
Introduction
E-cigarettes are becoming popular among the young population globally, possibly due to the declining trend in conventional smoking over the last decade.[1,2,3] A meta-analysis found that conventional cigarette smoking is a strong predictor of e-cigarette use, especially in adolescents. The probability of traditional cigarette smokers using an e-cigarette is remarkably higher than that of noncigarette smokers trying an e-cigarette. Moreover, the study also concluded that adolescents are much more likely than adults to use an e-cigarette.[4] Conversely, studies suggest that use of e-cigarettes by nonsmokers encourages the use of other tobacco products.[5,6] This could have an adverse impact on health because tobacco smoking is responsible for most lung cancer cases worldwide, including Saudi Arabia.[7,8] A cross-sectional study in Great Britain found that about a fifth of participants currently use e-cigarettes and a third of them used e-cigarettes in the past. The three main reasons for traditional tobacco smokers shifting to e-cigarettes are health concerns, reduction of smoking, and cessation of smoking.[9] In 2015, the global market for e-cigarettes was estimated to be $10 billion USD. Although e-cigarettes have fewer toxins than traditional tobacco smoke, the toxin level can vary widely according to the brand.[10] However, advertisements for e-cigarettes are invading the media and promoting them as an alternative to conventional cigarettes in public places, claiming that they are harmless. They are also advertised as an aid for cutting or quitting smoking. There are many flavors and brands; some claim to be tobacco-free.[11]
A cross-sectional survey-based study was carried out in the United States on 659 medical students from the University of Minnesota to evaluate student knowledge about e-cigarettes. A total of 97 participants (14.7%) said they had used e-cigarettes in the past and four participants 0.6% confirmed that they were current users. Significantly, most participants (619, 94.8%) felt that they did not receive adequate education about e-cigarettes in medical school. (185\656) 28.2% of the participants said that e-cigarettes are helpful in smoking cessation and (258, 39.3%) opined that e-cigarettes have lower cancer risks than traditional cigarettes. This study suggests that there is a lack of knowledge about e-cigarettes among medical students at the University of Minnesota and promotes the inclusion of e-cigarettes in the medical school curriculum.[12]
A recent study in Hong Kong that assessed the perception of e-cigarettes among young adults showed that a perception of e-cigarettes as less addictive and less harmful was associated with higher odds of e-cigarettes use. Researchers found that 16.1% of participants had tried e-cigarettes and concluded that more educational programs should be carried out to the community to raise awareness about e-cigarettes.[13] In three primary care settings, a number of patients were evaluated for e-cigarettes use and asked why they indulged in the habit. More than 50% of the smokers had used e-cigarettes and 20% were current users. The most common reasons behind the use of e-cigarettes were a desire to stop smoking cigarettes or decrease the frequency of cigarettes smoking.[14] In primary health care clinics in Ontario, Canada, the links between e-cigarettes use and smoking cessation were analyzed by using e-cigarettes as a method of helping in smoking cessation. A total of 18.1% of the participants were e-cigarette users during treatment, and the majority of participants reported using e-cigarettes as a smoking cessation method. E-cigarettes were found to have negative association with smoking cessation at 3 and 6 month intervals.[15] Another recent study targeting Korean youth has linked drug use, alcohol drinking frequency, and availability with more likelihood of e-cigarette use.[16]
It is evident that e-cigarettes have become popular over the past few years, especially among the young population.[1,2,3] Due to the increasing prevalence of e-cigarettes, medical students should have some knowledge about e-cigarettes to increase awareness among their patients in the future. There are limited data about the use and perception of e-cigarettes among medical students in Saudi Arabia and the Middle East in general. The objective of this study was to analyze the knowledge and beliefs of medical students regarding e-cigarettes, as well as to ascertain how many medical students have used e-cigarettes. We hypothesized that knowledge is inadequate and misconceptions exist regarding e-cigarettes.
Materials and Methods
Study design
This cross-sectional study was conducted on medical students in the main campus of Qassim University in Buraydah, Saudi Arabia. All 562 students were invited to fill the study questionnaire. The sample size was 229 out of 562 medical students with a 95% confidence level and a 5% confidence interval. The inclusion criteria included medical students at Qassim University, Main Campus. The exclusion criteria were nonmedical students at Qassim University, Main Campus.
Methods for Data Collection
A printed version of a prevalidated questionnaire from a previous study in the University of Minnesota, US, was used.[12] The questionnaire was provided to the data collectors for distribution to medical students from each academic year. The authors obtained the completed questionnaires afterward.
List of variables
Students were asked to fill in demographic data, including sex, age, and current academic year. The survey had three parts: the first focused on e-cigarette experience, the second part based on knowledge and attitudes, and the final part of the survey on education.
Data analysis
Data were analyzed using the IBM SPSS Statistics 25 software program. We transferred the data from the printed questionnaires to an SPSS file and stored the questionnaires safely. Descriptive statistics was expressed as frequencies, percentages, and mean. A Chi-square (X2) test was used to compare the categorical variables.
We intended to determine the percentage of e-cigarette users and correlate it with other variables, such as gender, current academic year, and presence of a family member or a friend who smoked e-cigarettes. Moreover, we wanted to examine the students’ attitudes toward e-cigarettes, confidence in discussing e-cigarettes with patients, and knowledge about whether e-cigarettes are approved by the Food and Drug Administration (FDA) for smoking cessation. In addition, the study aimed to investigate the association, if any, between the academic year and prevalence of e-cigarette use.
Ethical consideration
The research objective was explained to the participants. They were given a choice to participate or abstain. Participants were informed that their answers would be confidential and used only for scientific purposes. The research was approved on the 25th of October in 2018 by the ethical committee at Qassim University.
Results
Out of 562 medical students, 256 participated in the survey and filled in the questionnaire. A total of 148 (57.8%) of participants were males and 108 (42.2%) were females. Their mean age was 22 years. About one in ten students 10.6% confirmed having tried an e-cigarette. As shown in Table 1. Although there was no correlation between past experience of an e-cigarette and gender, age, or academic year, there was a significant correlation between e-cigarette use and having a family member or friend who smoked e-cigarettes (P value < 0.001). As many as 24.3% of the participants reported having a family member or a close friend who smoked e-cigarettes, while 75.7% did not. Among those with past experience of e-cigarette use, 70.4% had an e-cigarette smoker as a family member or friend, while only 18.5% of those who had never tried an e-cigarette reported having someone in the family or a friend who smoked e-cigarettes. Most students 71.9% said they were not sure whether e-cigarettes were approved by the FDA for smoking cessation, while only 7.9% answered in the affirmative. There was a statically significant correlation between the belief that e-cigarettes are less risky for cancer and answering “Yes” to the FDA-approval question (P value < 0.001). Additionally, 44.9% of students believed that there is no reduction in cancer risk for e-cigarettes smokers, while 23.2% reported to the contrary. The remaining participants were not sure.
Table 1.
Demographic data of the participants
| Variables | n=256 (%) |
|---|---|
| Gender | |
| Male | 148 (57.8) |
| Female | 108 (42.2) |
| Academic year | |
| First year | 48 (18.8) |
| Second year | 73 (28.5) |
| Third year | 46 (18) |
| Fourth year | 53 (20.7) |
| Fifth year | 36 (14.1) |
| Age, mean (SD) Ever smoked an e-cigarette |
22 (1.6) 27 (10.6) |
There was a statically significant relationship between believing that e-cigarettes have a lower risk of cancer and saying “Yes” to recommending e-cigarettes for patients as a smoking cessation method (P value < 0.001). Only 23.3% of students said that e-cigarettes could help patients quit smoking, while only 11% said that they would recommend it for a patient. On the other hand, 41.9% of participants did not agree that e-cigarettes could help patients quit smoking, whereas the remaining participants 34.8% were not sure. There was also a statically significant relationship between believing that e-cigarettes can aid in smoking cessation and recommending e-cigarettes as a smoking cessation method for patients (p-value < 0.001). Moreover, believing that e-cigarettes aid in smoking cessation was correlated with favoring smoking e-cigarettes over traditional smoking among patients (p-value < 0.001). Most medical students 55.9% said that they would not recommend e-cigarettes as a smoking cessation method for patients, whereas 33.1% were not sure. These data are displayed in Figure 1.
Figure 1.

Knowledge and attitudes of e-cigarettes
For favoring e-cigarettes over traditional cigarettes for patients, 44.5% of male students strongly agreed or agreed in comparison with only 29% of female students who felt that way (P value 0.023). A few students 14.8% disagreed or strongly disagreed with the statement those e-cigarettes are addictive, whereas 49.6% of the participants agreed or strongly agreed. The remaining participants 35.6% neither agreed nor disagreed. Most students 65.8% said that e-cigarettes are less addictive than traditional cigarettes, while only 4.5% reported that e-cigarettes are more addictive than traditional cigarettes; the remaining 29.6% said that both types of cigarettes are equally addictive. Most participants with an e-cigarette smoker among their family members or close friends were convinced that e-cigarettes are less addictive than traditional cigarettes (P value 0.021). 86.8% of students agreed that physicians should be educated about e-cigarettes. Additionally, 63.5% of students strongly agreed or agreed that they felt confident to discuss traditional cigarettes with patients, while 20.6% neither agreed nor disagreed; the remaining 15.9% strongly disagreed or disagreed. For the same question regarding e-cigarettes, 31.3% of participants agreed or strongly agreed while 29.8% were unsure and 37.7% disagreed or strongly disagreed. There was a positive correlation between the confidence to discuss traditional cigarettes and the confidence to discuss e-cigarettes (P value < 0.001).
Responding to the question about education on e-cigarettes in medical school, 92.6% denied having received any education, while only 7.4% said they received such education in medical school. From the latter group, 50% said they received the education in basic science curriculum, 18.2% in clinical curriculum, 9.1% in student interest groups, 9.1% through informal interactions with medical doctor (MD) team. 13.6% did not specify the source of their information. When asked whether they believed that they received adequate education, 95.9% of students said “No” and only 4.1% said “Yes.” In answer to a question about the best time to learn about e-cigarettes, most students 43.2% said that it should be imparted in the basic science curriculum, while 38.4% said it should be in the clinical curriculum. The majority of students who received information about e-cigarettes outside medical school said they got the information from social media 74.7%, followed by 9.2% from online advertising, 4.4% from television advertisements, 0.4% each from radio advertisements, billboard and/or public signs. Other sources included newspapers or magazines 3.1% and other mediums 7.9% as shown in Figure 2.
Figure 2.
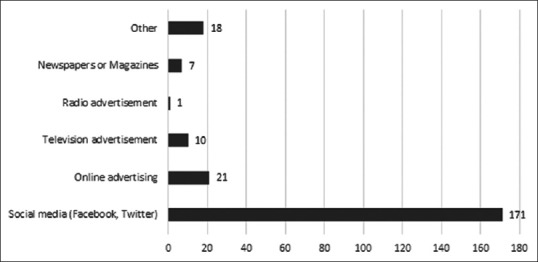
Sources of e-cigarettes knowledge
Discussion
In this study, we captured the knowledge, perception, and attitude of medical students toward e-cigarettes as well as the prevalence and frequency of e-cigarette smoking. There were few students 10.6% who said that they had tried e-cigarettes. In a comparison, a study on Polish university students reported a much higher 57% of such respondents.[17] Another study on health professional students in the US confirmed that 24.2% of the participants had tried e-cigarettes.[18]
A survey conducted on children of the 11th and 12th grades in California showed that gender, ethnic background, and grade had no relationship with e-cigarette smoking. However, an analysis at the Medical School of the University of Minnesota reported a correlation between gender and e-cigarette smoking, with a higher percentage of males smoking e-cigarettes.[12] Many participants in that study 22.7% admitted that they have an e-cigarette smoker among family members and friends. A similar outcome was recorded in the survey on US health professional students, where 53.1% of the participants had a family member or a friend using e-cigarettes.[18]
In our study, we established a correlation between trying e-cigarettes and having an e-cigarette smoker among close friends or family members. Similarly, the study in California concluded that participants with friends smoking tobacco had a higher chance of e-cigarette use.[6] The majority of our participants 71.1% were not sure whether e-cigarettes were approved by the FDA for smoking cessation and only 7.9% said “Yes.” In a comparable study, 35.8% of students stated that they were not sure whether e-cigarettes were approved by the FDA and only 4.1% said they were FDA-approved.[12]
Furthermore, many students 41.9% in our study did not consider e-cigarettes helpful in smoking cessation. A similar finding was recorded in the study at the University of Minnesota, where most students did not believe that e-cigarettes could help patients quit tobacco smoking.[12] Also, most students 55.9% said that they would not recommend e-cigarettes for smoking cessation, while only 11% of students were in favor of recommending such a step. Similarly, around 25.3% of the participants in the survey on US health professional students strongly agreed or agreed that e-cigarettes were a viable means for smoking cessation.[18] In the Canadian study, around 50.7% of smokers used e-cigarettes as an aid to quit smoking.[2] On the contrary, around half the respondents in the study on Polish University students considered e-cigarettes to be a safer option than traditional cigarettes, while only 23.2% in our study said so.[17] Many participants in a survey on medical students in New York City also agreed that nonconventional tobacco products had a lower causality than tobacco cigarettes for numerous illnesses.[19] However, 49.6% of the students believed that e-cigarettes are addictive. In comparison, the research on students in Minnesota showed that most participants believed e-cigarettes to be addictive.[12] Similarly, 83.5% of the participants in a medical school in Poland felt that e-cigarettes are addictive.[20] However, the majority of students reported that e-cigarettes are less addictive than traditional cigarettes.
With reference to the question on education about e-cigarettes, the vast majority of students denied having received any such education. Likewise, 84.7% in the study at the University of Minnesota reported receiving no education about e-cigarettes.[12] Moreover, 90% of students believed they had not received adequate information about e-cigarettes. On the contrary, most participants in the survey on US health professional students reported an average knowledge about e-cigarette.[18] Many of those students said that they received the information about e-cigarettes through social media. The same feedback was also recorded in the study at the University of Minnesota.[12] The majority of participants 63.5% in our study were confident about discussing the use of traditional cigarettes with their patients. However, fewer students 31.3% felt confident about discussing the use of e-cigarettes with their patients. Many primary health care physicians may encounter e-cigarette users,[14,15] and thus should be educated on e-cigarettes, their use, and their misconceptions. Many primary health care patients use e-cigarettes as a mean for smoking cessation. Thus, discussion regarding their use would be beneficial when conducted primary health care physicians.
Our research has shed light on the perception, knowledge, and attitude about e-cigarette smoking among medical students in Qassim University. A significant finding of the research is the relatively common use of e-cigarettes. Most students reported that they do not have adequate information about e-cigarettes, which necessitates more information on e-cigarettes in the curriculum. One of the limitations of our study was the scant literature available about e-cigarettes. Therefore, more studies are needed to better understand other aspects about e-cigarette use and knowledge among students and to assess the impact of those factors.
There is some inconsistency between the results obtained in this study and those recorded in other studies. Due to the limitations of this study, it might not be prudent to generalize our results and apply them to other colleges and universities. Nonetheless, our results provide a strong groundwork for e-cigarette use and associated perceptions among the medical students at Qassim University.
Limitations
The difficulties or limitations of the study included finding data collectors from each academic year and reaching the required sample size from such a small community. Moreover, the study questionnaire did not include items for traditional cigarette smokers.
Conclusion
Based on our survey, e-cigarette smoking seems to be relatively common among the medical students, with a significant correlation between-cigarette use and having a family member or a close friend who smokes e-cigarettes. Our evaluation of the students’ experience, attitude, and knowledge leads us to the conclusion that the medical students lack adequate knowledge about e-cigarettes. Therefore, more efforts are needed to educate healthcare professionals, and the community at large, about the risks associated with e-cigarettes. These efforts may eventually minimize the popularity of e-cigarettes.
Ethics approval and consent to participate
Ethical consent has been taken from the ethical committee at Qassim University.
Author Biographies
Abdullah Almutham is a medical intern at Qassim University, College of Medicine, Saudi Arabia.
Mohammed Altami is a medical intern at Qassim University, College of Medicine, Saudi Arabia.
Fawzy Sharaf is a Professor of family medicine at Qassim University, College of Medicine, Family and Community Department - KSA. He received the Jordanian and Saudi Board for Family Medicine and serves as a Professor/Consultant in Family Medicine. His research includes community-based and medical education studies.
Ali Alaraj is an Assistant Professor at Qassim University. He holds a specialty in pulmonary medicine and subspecialty in sleep medicine from Western University, Canada. His areas of interest are asthma and smoking-related pulmonary diseases.
Financial support and sponsorship
Nil.
Conflicts of interest
There is no conflict of interest.
Acknowledgements
We would like to acknowledge and thank the medical students and interns who helped us collect the data in this study: Ryan Ahmed Suliman Alaboodi (intern), Abdullah Abdulaziz Alkanan (intern), Meshal Sulaiman Alashgar (medical student), Ibrahim Saleh Algosair (medical student), Maram Ibrahim Altami (medical student), and Rawan Fahad AlSubaie (medical student).
References
- 1.Hawkins V. Smoking, drinking and drug use among young people in England in 2011. In: Fuller E, editor. London: Health and Social Care Information Centre; 2012. [Google Scholar]
- 2.Czoli CD, Reid JL, Rynard VL, Hammond D. E-cigarette in Canada-Tobacco Use in Canada: Patterns and Trends, Special Supplement. 2015 [Google Scholar]
- 3.CDC Tobacco Use among Middle and High School Students — United States, 2011–2014. Morb Mortal Wkly Rep. 2015;64:381–5. [PMC free article] [PubMed] [Google Scholar]
- 4.Wang M, Wang JW, Cao SS, Wang HQ, Hu RY. Cigarette smoking and electronic cigarettes use: A meta-analysis. Int J Environ Res Public Health. 2016;13 doi: 10.3390/ijerph13010120. doi: 10.3390/ijerph 13010120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leventhal AM, Strong DR, Kirkpatrick MG, Unger JB, Sussman S, Riggs NR, et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314:700–7. doi: 10.1001/jama.2015.8950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barrington-Trimis JL, Urman R, Berhane K, et al. E-Cigarettes and Future Cigarette Use. Pediatrics. 2016;138:e20160379. doi: 10.1542/peds.2016-0379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghobadi H, Sharghi A, Zh S. Epidemiology and Risk Factors for Lung Cancer in Ardabil, Iran. J Ardabil Univ Med Sci. 2013;13:220–8. Available from: http://jarums.arums.ac.ir/browse.php?a_code=A-10-27-95&slc_lang=en&sid=1 . [Google Scholar]
- 8.Furrukh M. Tobacco smoking and lung cancer: Perception-changing facts. Sultan Qaboos Univ Med J. 2013;13:345–58. doi: 10.12816/0003255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown J, West R, Beard E, Michie S, Shahab L, McNeill A. Prevalence and characteristics of e-cigarette users in Great Britain: Findings from a general population survey of smokers. Addict Behav. 2014;39:1120–5. doi: 10.1016/j.addbeh.2014.03.009. Available from: http://dx.doi.org/10.1016/j.addbeh.2014.03.009 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO. Electronic Nicotine Delivery Systems and Electronic Non-Nicotine Delivery Systems (ENDS/ENNDS) Report by WHO. 7–12, Conf Parties to WHO Framew Conv Tob Control. 2016 [Google Scholar]
- 11.Andrade MD, Hastings G, Angus K. Promotion of electronic cigarettes: Tobacco marketing reinvented? Bmj. 2013;347:f7473. doi: 10.1136/bmj.f7473. Available from: http://www.bmj.com/cgi/doi/10.1136/bmj.f7473 . [DOI] [PubMed] [Google Scholar]
- 12.Hinderaker K, Power DV, Allen S, Parker E, Okuyemi K. What do medical students know about e-cigarettes? A cross-sectional survey from one U.S. medical school. BMC Med Educ. 2018;18 doi: 10.1186/s12909-018-1134-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang X, Zhang X, Xu X, Gao Y. Perceptions and use of electronic cigarettes among young adults in China. Tob Induc Dis. 2019;17:1–9. doi: 10.18332/tid/102788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kalkhoran S, Alvarado N, Vijayaraghavan M, Lum PJ, Yuan P, Satterfield JM. Patterns of and reasons for electronic cigarette use in primary care patients. J Gen Intern Med. 2017;32:1122–9. doi: 10.1007/s11606-017-4123-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Access CA. Concurrent e-cigarette use during tobacco dependence treatment in primary care setttings: Association with smoking cessation at 3- and 6-months. Nicotine Tob Res. 2017;19:183–9. doi: 10.1093/ntr/ntw218. [DOI] [PubMed] [Google Scholar]
- 16.Lee Y, Lee K-S. Association of alcohol and drug use with use of electronic cigarettes and heat-not-burn tobacco products among Korean adolescents. PLoS One. 2019;14:e0220241. doi: 10.1371/journal.pone.0220241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zarobkiewicz MK, Wawryk-Gawda E, Wozniakowski MM, Slawinski MA, Jodlowska-Jedrych B. Tobacco smokers and electronic cigarettes users among Polish universities students. Rocz Panstw Zakl Hig. 2016;67:75–80. [PubMed] [Google Scholar]
- 18.Franks AM, Hawes WA, McCain KR, Payakachat N. Electronic cigarette use, knowledge, and perceptions among health professional students. Curr Pharm Teach Learn. 2017;9:1003–9. doi: 10.1016/j.cptl.2017.07.023. [DOI] [PubMed] [Google Scholar]
- 19.Castranova V, Asgharian B, Sayre P, Virginia W, Carolina N. A Study of the Use, Knowledge, and Beliefs About Cigarettes and Alternative Tobacco Products Among Students at One U.S. Medical School. HHS Public Access. 2016;90:1713–9. doi: 10.1097/ACM.0000000000000873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jankowski M, Zejda J, Idzik A. E-smoking among students of medicine — frequency, pattern and motivations. Adv Respir Med. 2017;85:8–14. doi: 10.5603/ARM.2017.0003. [DOI] [PubMed] [Google Scholar]


