Abstract
Background:
Stress is a psychophysiological phenomenon. Due to recent lifestyle modifications prevalence of stress is increasing among adults and adolescents. Adolescence is a period of storm and stress and any excess stress would have negative impact on their sleep and would ultimately affect their academic performance and health. Hence the current study proposes to evaluate the effect of stress on sleep hygiene among school going adolescents in Chennai.
Materials and Methods:
A cross-sectional study and participants were healthy male (84) and female (48) school going adolescents between the age group of 15-19 years (n = 132). Stress was assessed using Perceived Stress Scale (PSS) and sleep hygiene was assessed using Epworth Sleepiness Scale for Children and Adolescents (ESS-CHAD).
Results:
In all, 84.8% of the adolescents reported that they are academically overloaded. Both the genders were found to be moderately stressed (Males: 63.6%; females: 66.7%). Prevalence of sleep disturbances was found to be 23.5% and increase in stress was found to be associated with decrease in sleep quality.
Discussion:
The study shows that prevalence of stress is high among adolescents and it is negatively influencing their sleep hygiene. Hence, early identification and management of stress is required for school going late adolescents for better academic performance and wellbeing.
Keywords: Adolescents, sleep hygiene, stress
Introduction
Stress is an essential and inevitable part of life and is defined as “non-specific response to stimuli by the host due to internal or external factors.”[1] Stress is classified in to eustress and distress. Eustress is the positive form of stress which is required to carry out day-to-day activities of life. Distress is the unpleasant form of stress and prolonged existence of which acts as a threat to Homeostasis. Rapid increase in science and technology has increased the stress level among the general population.[2] Increased stress level activates neural system in a short-term basis and activates the neuro-endocrine system in long-term basis. Prolonged stress level repeatedly activates the Hypothalamo-pituitary axis and increases the level of stress hormones and other inflammatory mediators.[3] Increased circulation of stress hormones over a period of time increases the risk of developing lifestyle disorders such as Type 2 Diabetes Mellitus, Hypertension, Dyslipidemia, Early Coronary artery disease and Sleep disorders.[4]
Adolescence is critical phase of Human life where an enormous physical, emotional and social changes takes place. WHO has defined adolescence as “period between 10-19 yrs of life”.[5] Adolescents are exposed to various psycho-physiological stressors due to rapid changes in their body. Along with the pre-existing psycho-physiological stressors, in current era adolescents are exposed to increased academic pressure, peer pressure and pressures from other sources of society.[2]
Sleep is an essential part of life and required for a healthy living. A good sleep is divided in to NREM and REM sleep. NREM sleep is required for somatic well-being and REM sleep plays a vital role in memory consolidation,[6] which is required for good academic performance in adolescents. Increased level of stress compromises sleep hygiene of an individual by negatively influencing the psycho-physiological components of homeostasis.[2,7] Hence assessment of stress and its effect on sleep hygiene among adolescents is much needed and the current study proposes to study the effect of stress on sleep hygiene among school going adolescents in Chennai.
Materials and Methods
Study participants
The current study is a cross-sectional study. The study is initiated after obtaining permission from the Institutional Ethics committee. The school is chosen using random allocation software from list of schools obtained from the Urban Corporation. Participants are healthy school going adolescents between the age group of 15-19 years (n = 132). Participants with existing metabolic or neuro-psychiatric disorders were excluded and participants whose parents gave consent and participants who gave assent were included.
Study tools
General details, academic stress-related questions were collected using a questionnaire and stress was assessed using Perceived Stress Scale (PSS).[8] PSS is a self-report measure of an individual's stress. PSS is a 10-item questionnaire which contains questions asking feelings and thoughts of the individual in the last month. The questions have options like never, almost never, sometimes, fairly often and very often and the participants should choose their relevant option for the questions. For few questions, reverse scoring pattern is used and the total score is calculated. If the total score is ranged 0-13, it is mild stress; 14-26 is moderate stress; and 27-40 is considered as high stress.
Sleep hygiene is assessed used Epworth Sleepiness Scale (ESS) for children and adolescents.[9] ESS assesses Excessive Daytime Sleepiness (EDS) of an individual. EDS is defined as a condition where an ‘individual would be asleep during daytime when expected to be awake’. EDS remains as common symptom for most of the sleep disorders. Hence, assessment of EDS reveals sleep hygiene of an individual. ESS consists of eight questions and the adolescent should score chances of dozing from a scale of 0-3 where 0 indicates no chances of dozing, 1 indicates slight chances of dozing, 2 indicates moderate chances of dozing and 3 indicates severe chances of dozing. A total score of ≥10 indicates EDS indicating compromised sleep hygiene.
Study procedure
Study procedure is explained and written permission was obtained from the school authorities. Questionnaires were distributed to the students before the data collection day and informed consent was obtained from the parents and assent is obtained from the participants. General questionnaire, PSS and ESS is explained to the participants and they were asked to fill it individually without consulting with their classmates.
Statistical analysis
The data were tabulated in MS Excel sheet and analyzed using SPSS Software version 21.0. Descriptive statistics was calculated for background variables. Association between categorical variables was tested by Chi-square test. P < 0.0.5 was taken as statistically significant.
Results
Participants taken for analysis were 132 school going adolescents consisting of 84 males and 48 females. Among 132 participants, mean age was found to be 15.65 ± 0.75 years. Gender wise 63.6% were males and 36.4% were females. Highest percentage of study population (38.6%) was found in the board exam appearing students [Table 1]. Gender-wise prevalence of stress given in Table 2. The relation between stress and sleep given in Table 3.
Table 1.
Academic details of the study participants
| Questions | Frequency | Percentage | |
|---|---|---|---|
| Are you academically overloaded? | Yes | 112 | 84.8 |
| No | 20 | 15.2 | |
| Is ranking pattern stressful? | Yes | 107 | 81.1 |
| No | 25 | 18.9 | |
Table 2.
Gender wise prevalence of stress among study participants
| Gender | Mild stress | Moderate stress | Severe stress | P |
|---|---|---|---|---|
| Male | 22 (26.2%) | 84 (63.6%) | 14 (10.6%) | 0.782 |
| Female | 12 (25%) | 32 (66.7%) | 4 (8.3%) | |
| Total | 22 (26.2%) | 52 (61.9%) | 10 (11.9%) |
Table 3.
Stress and sleep quality among the study participants
| PSS Score | ESS ≥10 | P |
|---|---|---|
| Mild stress | 14.7% | 0.112 |
| Moderate stress | 23.8% | |
| Severe stress | 42.9% |
Prevalence of EDS
EDS among the study participants was found to be 23.5%. (total score ≥10). Gender difference in EDS was not analyzed due to uneven sample size distribution. Details given in Figure 1.
Figure 1.
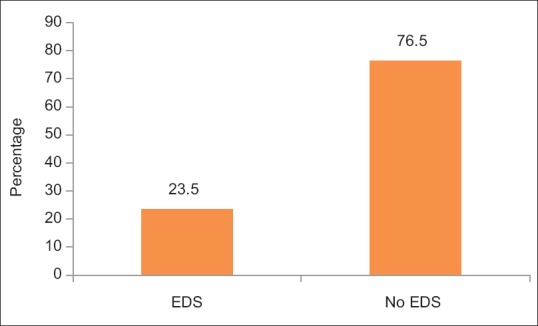
Prevalence of EDS among participants
Discussion
The current study aimed at assessing the effect of stress on sleep hygiene among school going adolescents in Chennai. Participants of the study belong to the age group 15-19 years which is academically and socially a stressful phase in an adolescent's life. Majority of the study participants belong to the board exam appearing class, which is a highly stressful period. Adolescents perceive that they are academically overloaded which acts as a main stressor.[10,11] Also, ranking pattern among students was found to be a stressful event among adolescents. Results have suggested that both male and female adolescents are moderately stressed. Academic stress, performance pressure, anxiety and fear of failure in school environment have been reported as major sources of stress in school among adolescents.[12] Family conflicts, body image,[13] and relationships[14] were also identified as potential stressors. All these factors trigger an increased level of stress among adolescents.
Statistical analysis of the effect of stress and sleep has shown that as stress level increases sleep quality decreases among adolescents,[2,7,15,16] though the P value was statistically insignificant which could be due to smaller sample size. Stress has been reported to reduce sleep quality in an individual.[2,7] Stress activates sympatho-adreno-medullary system (SAM) and Hypothalamo Pituitary axis (HPA). These system increases the level of stress hormones such as cortisol and catecholamines.[17] Decreased level of cortisol is required for initiation of sleep.[18] Increased level of cortisol decreases duration of REM sleep, increases superficial sleep.[19,20,21,22] and causes cognitive dysfunctions.[16] Experimental infusion of cortisol has been found to decrease REM sleep.[23] REM sleep is the phase where memory consolidation takes place, when REM sleep is disturbed it will affect the academic performance of adolescents. Also, increased amount of Growth hormone is released during sleep which produces physical growth in adolescents and compromise in sleep alters the Growth hormone level and physical growth in adolescents.[15] A disturbed sleep has been associated with increased levels of cortisol and other inflammatory mediators.[17] Cortisol affects the neural integrity of Hippocampus[24] which affects learning and memory. Elevated level of cortisol caused by stress and sleep disturbances increases sympathetic activity, increased level of inflammatory mediators and free radicals. Prolonged rise of inflammatory mediators and free radicals makes an individual more prone for lifestyle disorders, such as Diabetes Mellitus, hypertension, Dyslipidaemia and early cardiac disease.[25,26,27,28,29,30,31,32]
Conclusion
The current study shows that school going adolescents are moderately stressed and stress has a negative influence on their sleep hygiene. Stress is required in a minimal quantity for a positive life. But chronic stress makes an individual prone for psycho-somatic diseases and impairs quality of life. Adolescents are the pillars of a country and conditions like adolescent stress and adolescent sleep are not much considered or recognized. Family Physicians are the primary healthcare contact person of a family. They remain in close contact with family and will be aware of an adolescent's lifestyle, right from his childhood to his current adolescent phase.[33] So, it will be possible for family physician to identify and treat adolescent stress and sleep problem than any other healthcare professional. Hence, stress management and healthy lifestyle could be taught to adolescents by their family physician in their early life itself for a healthy future.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Self funding.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to acknowledge the participants and management of the school for permitting us to carry out the study.
References
- 1.Cohen S, Kessler RC, Underwood-Gordon L. Strategies for measuring stress in studies of psychiatric and physical disorders. In: Cohen S, Kessler RC, Underwood-Gordon L, editors. Measuring Stress. New York: Oxford University Press; 1995. pp. 3–28. [Google Scholar]
- 2.Larue DE, Herrman JW. Adolescent stress through the eyes of high-risk teens. Paed Nurs. 2008;34:375–80. [PubMed] [Google Scholar]
- 3.Weibel L, Follenius M, Spiegel K, Ehrhart J, Brandenberger G. Comparative effect of night and daytime sleep on the 24-hour cortisol secretory profile. Sleep. 1995;18:549–56. [PubMed] [Google Scholar]
- 4.Tajik E, Zulkefi LAM, Baharom A, Minhat HS, Lattiff LA. Contributing factors of obesity among stressed adolescents. Electron Physician. 2014;6:771–8. doi: 10.14661/2014.771-778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. New Delhi: Regional Office of the South East Asia; 1997. Adolescence: The Critical Phase: The Challenges and the Potential; p. 1. [Google Scholar]
- 6.Meldrum RC, Restivo E. The behavioral and health consequences of sleep deprivation among US high school students: Relative deprivation matters. Prev Med. 2014;6:24–8. doi: 10.1016/j.ypmed.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 7.Mesquita G, Reiamao R. Stress and sleep quality in highs chool Brazilian students. An Acad Bras Cienc. 2010;82:545–51. doi: 10.1590/s0001-37652010000200029. [DOI] [PubMed] [Google Scholar]
- 8.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:386–96. [PubMed] [Google Scholar]
- 9.Johns MW. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 10.Chandra A, Batada A. Exploring stress and coping among urban African-American adolescents: The shifting the lens study. Prev Chronic Dis. 2006;3:1–10. [PMC free article] [PubMed] [Google Scholar]
- 11.Green SE, Holohan E, Feldheim A. Stress in the family. 2003. [Last accessed on 2019 Jul 22]. Available from: http://www.ecb.org/guides/pdf/CE_68_05.pdf .
- 12.Lau BWK. Does the stress of childhood and adolescence matter? A psychological perspective. J R Soc Promot Health. 2002;122:238–44. doi: 10.1177/146642400212200411. [DOI] [PubMed] [Google Scholar]
- 13.Tarrant B, Woon A. Adolescent suicide: An overview. Aus J Emer Care. 1995;2:26–30. [Google Scholar]
- 14.Puskar KR, Rohay JM. School relocation and stress in teens. J School Nurs. 1999;5:16–22. doi: 10.1177/105984059901500103. [DOI] [PubMed] [Google Scholar]
- 15.Rogers NL, Szuba MP, Staab JP, Evans DL, Dinges DF. Neuroimmunologic aspects of sleep and sleep loss. Semin Clin Neuropsychiatry. 2001;6:295–307. doi: 10.1053/scnp.2001.27907. [DOI] [PubMed] [Google Scholar]
- 16.Harvey AG. A cognitive model of insomnia. Behav Res Ther. 2002;40:869–93. doi: 10.1016/s0005-7967(01)00061-4. [DOI] [PubMed] [Google Scholar]
- 17.Dunn AJ, Berridge CW. Physiological and behavioral responses to corticotropin-releasing factor administration: Is CRF a mediator of anxiety or stress responses? Brain Res Brain Res Rev. 1990;15:71–100. doi: 10.1016/0165-0173(90)90012-d. [DOI] [PubMed] [Google Scholar]
- 18.Vgontzas AN, Bixler EO, Lin HM, Prolo P, Mastorakos G, Vela-Bueno A, et al. Chronic insomnia is associated with nyctohemeral activation of the hypothalamic-pituitary-adrenal axis: Clinical implications. J Clin Endocrinol Metab. 2001;86:3787–94. doi: 10.1210/jcem.86.8.7778. [DOI] [PubMed] [Google Scholar]
- 19.Adam K, Tomney M, Oswald I. Physiological and psychological differences between good and poor sleepers. J Psychiatr Res. 1986;20:301–6. doi: 10.1016/0022-3956(86)90033-6. [DOI] [PubMed] [Google Scholar]
- 20.Steiger A. Sleep and the hypothalamo-pituitaryadrenocortical system. Sleep Med Rev. 2002;6:125–38. doi: 10.1053/smrv.2001.0159. [DOI] [PubMed] [Google Scholar]
- 21.Vgontzas AN, Zoumakis M, Bixler EO, Lin HM, Prolo P, Vela bueno A, et al. Impaired nighttime sleep in healthy old versus young adults is associated with elevated plasma interleukin-6 and cortisol levels: Physiologic and therapeutic implications. J Endocrinol Metab. 2003;88:2087–95. doi: 10.1210/jc.2002-021176. [DOI] [PubMed] [Google Scholar]
- 22.Capaldi VF, Handwerger K, Richardson E, Stroud LR. Associations between sleep and cortisol responses to stress in children and adolescents: A pilot study. Behav Sleep Med. 2005;3:177–82. doi: 10.1207/s15402010bsm0304_1. [DOI] [PubMed] [Google Scholar]
- 23.Verlander LA, Benedict JO, Hanson DP. Stress and sleep patterns of college students. Percept Mot Skills. 1999;88:893–8. doi: 10.2466/pms.1999.88.3.893. [DOI] [PubMed] [Google Scholar]
- 24.McEwen BS, Sapolsky RM. Stress and cognitive function. Curr Opin Neurobiol. 1995;5:205–16. doi: 10.1016/0959-4388(95)80028-x. [DOI] [PubMed] [Google Scholar]
- 25.Srihari R, Manikandan S, Semblingam P, Vimalarani S. Prevalence of excessive daytime sleepiness among medical students in Chennai. World J Pharm Sci. 2014;3:1819–26. [Google Scholar]
- 26.Srihari R, Mathangi DC, Sriteja Y, Remya K, Mathangi DC, Shyamala R. Second digit and fourth digit ratio – An adjunct tool to predict obstructive sleep apnea. Indian J Physiol Pharmacol. 2014;58:292–5. [PubMed] [Google Scholar]
- 27.Srihari R, Dilara K, Latha R, Manikandan S. Assessment of sleep hygiene among school going adolescents in Chennai. Ind J Public Heal Res Dev. 2019;10:17–21. [Google Scholar]
- 28.Srihari R, Mathangi DC, Shyamala R. OSA: An awaking disorder! IOSR J Pharm. 2014;4:4–7. [Google Scholar]
- 29.Pivonello R, Menafra D, Riccio E, Garifilos F, Mazzella M, de Angelis C, et al. Metabolic disorders and male hypogonadotrophic hypogonadism. Front Endocrinol. 2019;10:1–10. doi: 10.3389/fendo.2019.00345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Amin MN, Hussain MS, Sarwar MS, Rahman Moghal MM, Das A, Hossain MZ, et al. How the association between obesity and inflammation may lead to insulin resistance and cancer. Diabetes Metab Syndr. 2019;13:1213–24. doi: 10.1016/j.dsx.2019.01.041. [DOI] [PubMed] [Google Scholar]
- 31.Oguntibeju OO. Type 2 diabetes mellitus, oxidative stress and inflammation: Examining the links. Int J Physiol Pathophysiol Pharmacol. 2019;11:45–63. [PMC free article] [PubMed] [Google Scholar]
- 32.Afrisham R, Paknejad M, Soliemanifar O, Nejadi SS, Meshkani R, Larky DA. The influence of Psychological stress on initiation and progression of Diabetes and Cancer. Int J Endocrinol Metab. 2019;17:1–9. doi: 10.5812/ijem.67400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kulak JA, Griswold KM. Adolescent substance abuse and misuse; recognition and management. Am Fam Physician. 2019;99:689–96. [PubMed] [Google Scholar]


