Abstract
Background:
Rates of exclusive breastfeeding are exceedingly low in the Arabic world. This study aims to estimate the local prevalence of, and knowledge about, exclusive breastfeeding in Saudi Arabia.
Method:
This is a cross-sectional survey of mothers of infants aged 6–12 months who attended Taif-based “well-baby clinic.” A structured questionnaire was developed to explore predictors of, and participants’ knowledge about, exclusive breastfeeding.
Results:
Participants in the study were 202 mothers. The rate for initiation of breastfeeding in the first hour after childbirth was 13.9%. The prevalence of exclusive breastfeeding was 16.3%. Knowledge level was great among participating mothers as 65.3% of mothers scored over 75% of the total knowledge score and 95% got more than half of the questions right. Only having 3–6 children (P = 0.023) and 1-year interpregnancy interval (P = 0.005) were associated with the positive likelihood of exclusive breastfeeding. Baby age (P = 0.0218), birth in a private facility (P = 0.00843), and university education (P = 0.0131) were associated with better knowledge.
Discussion and Conclusion:
Rates of exclusive breastfeeding practice are low in Saudi Arabia despite adequate knowledge about its benefits and necessity.
Keywords: Exclusive breastfeeding, knowledge, Saudi Arabia
Introduction
Breastfeeding is the ideal, unique, and natural method for nourishing the developing infant. Breast milk provides all the first months’ energy and nutrients’ requirements, more than half of such requirements during the following 6 months, and up to one-third during the second year of life.[1] Prevalence of breastfeeding varies substantially across the globe, with highest rates are reported from low-income and middle-income countries.[2]
Exclusive breastfeeding is the provision of breast milk as the only nutrient received by babies. It reduces common childhood illnesses, strengthens immunity,[3] and improves infant survival.[4] World Health Organization (WHO) recommends exclusive breastfeeding for up to the first 6 months of life.[5] However, its rates are notoriously low across the Arabic world and in Saudi Arabia.[6] Worldwide, mothers struggle to keep a balance between prescribed social influence and personal, self-efficacious, view of parenting. This struggle can negatively affect their decision to exclusively breastfeed.[7] Enhancement of breastfeeding depends on societal norms that guide women's attitudes.[8] Regionally, breastfeeding behavior was also largely influenced by knowledge about the benefits associated with it.[9] Locally, in contrast, lack of support was cited as one of the important reasons for such low rates of exclusive breastfeeding among Saudi mothers, in addition to a multitude of biological (for instance, chronic diseases and obesity) and cultural factors.[10] Indeed, wider between-pregnancy intervals, husband and family support, and vaginal delivery are positive correlates with breastfeeding.[11] Certainly, very little is known about Saudi mothers’ awareness of exclusive breastfeeding and its practice.
The study aims to estimate the prevalence of exclusive breastfeeding in Saudi Arabia, the barriers against it, knowledge level about it, and the factors affecting it among mothers.
Methodology
This is a cross-sectional study on the basis of face-to-face interview for breastfeeding mothers of infants aged 6–12 months who attended “well-baby clinic.” We used convenience sampling in approaching participants.
The survey was conducted in Alhada Armed Forces Hospital—a modern facility with 569 beds. The study area, Taif, is in the mountains of Saudi Arabia in the Hejaz area, with generous rainfall.
The questionnaire was developed by the researchers to explore predictors of exclusive breastfeeding and participants’ knowledge about it. The items were adapted from recent standardized inventories exploring breastfeeding knowledge and attitudes in the Middle Eastern,[12] Asian,[13] and African regions.[14] It was adapted further by senior neonatologists, pediatricians, family physicians, and public health research experts. All agreed on the final version of the questionnaire in terms of content and face validity. Psychometric properties were evaluated during the conduct of this study. The questionnaire piloted the questionnaire on 20 mothers to ensure better understandability, readability, and time and cost-efficiency of its design. The final agreed version consisted of 12 questions with 3 possible answers: “correct,” “incorrect,” and “do not know.” Correct answers got a score of 1, and a score of 0 was awarded otherwise. Sum of correct answers constituted the final total score. As the total score is count data, its relationship with background covariates was tested using generalized regression binomial modeling to ensure robustness and good-fit to the data.
Statistical analysis was performed using R statistical software version 3.4.1.[15] Descriptive statistics were presented as count, percentages, range, medians, means, and standard deviation (SD). Inferential statistics were performed using generalized regression modeling as appropriate. Statistical significance level was set at a P value of <0.05.
Ethical approval number REC.T.2018-10-352 was granted from the Regional Research and Ethics committee in Taif and Alhada Armed Hospitals.
Results
The total number of participants interviewed was 202 mothers. The mean age was 23.4 years (SD = 4.89), ranging between 15 and 44 years, the median age was 31 years [Table 1].
Table 1.
Characteristics of study participants (n=202)
| Characteristic | Frequency (n) | Percentage (%) |
|---|---|---|
| Age categories (years) | ||
| 15-20 | 1 | 0.5 |
| 21-25 | 25 | 12.4 |
| 26-30 | 70 | 34.7 |
| 31-35 | 53 | 26.2 |
| >36 | 53 | 26.2 |
| Age (years) mean±SD (median) | 23.4±4.89 (31) | |
| Infant age (months) mean±SD (median) | 9.2±2.68 (9) | |
| Infant gender | ||
| Male | 105 | 52 |
| Female | 97 | 48 |
| Mother education | ||
| Illiterate | 5 | 2.5 |
| Primary | 13 | 6.4 |
| Preparatory | 11 | 5.4 |
| Secondary | 56 | 27.7 |
| University | 117 | 57.9 |
| Employment | ||
| Unemployed | 43 | 21.3 |
| Employed | 159 | 78.7 |
| Time with the baby | ||
| Always with baby | 151 | 74.8 |
| 1-2 hours separation | 12 | 5.9 |
| 3-6 hours separation | 11 | 5.4 |
| >6 hours separation | 28 | 13.9 |
| Parity | ||
| Once | 45 | 22.3 |
| More than once | 157 | 77.7 |
| No. of children | ||
| <3 | 110 | 54.5 |
| 3-6 | 76 | 37.6 |
| >6 | 16 | 7.9 |
| Planning future pregnancy | ||
| Yes | 88 | 43.6 |
| No | 114 | 56.4 |
| Between-pregnancy previous interval | ||
| <1 year | 8 | 4 |
| 1 year | 18 | 8.9 |
| 2 years | 35 | 17.3 |
| >2 years | 106 | 42.5 |
| No past pregnancy | 35 | 17.3 |
| Postpartum problems | ||
| Yes | 63 | 31.2 |
| No | 139 | 68.8 |
| Childbirth place | ||
| Public hospital | 194 | 96 |
| Private hospital | 8 | 4 |
| Husband support | ||
| Yes | 115 | 56.9 |
| Minimum | 60 | 29.7 |
| No | 27 | 13.4 |
The prevalence of breastfeeding among the participating mothers was 87.1% (n = 176), of whom 73.3% (n = 148) breastfed their babies after the first hour of birth and 13.9% (n = 28) breastfed during the first hour, whereas those who did not breastfeed were 12.9% (n = 26). Moreover, only 16.3% (n = 33) of mothers indicated that they engage in exclusive breastfeeding practice by giving supplementary food only after their baby reached 6 months, whereas the remaining 83.7% (n = 169) indicated otherwise, with 68.3% (n = 138) are willing to add supplementary food before the third month of age, and further 15.3% (n = 31) will give supplementary food at some point between the third and the sixth month of age [Figure 1].
Figure 1.
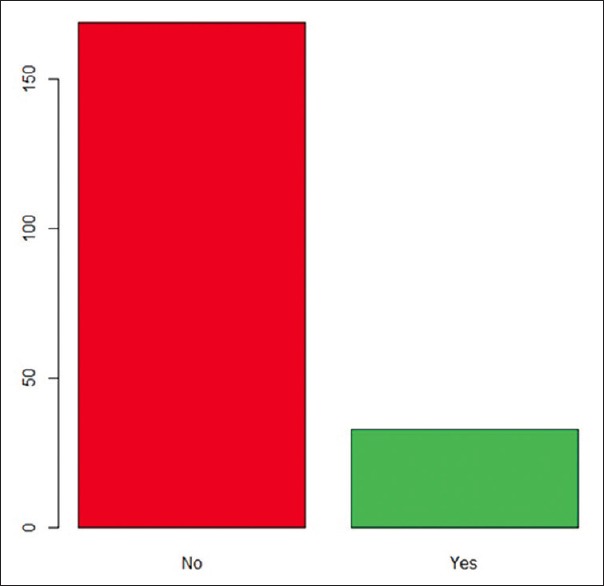
Prevalence of exclusive breastfeeding behavior among participating mothers
The majority of mothers scored over 75% of the total knowledge score (n = 132, 65.3%), with 29.7% (n = 60) who scored between 50% and 75% and a minority of 5% (n = 10) who scored below 50% [Table 2]. This is indicative of great knowledge among participating mothers. The mean overall score was 9.68 (SD = 1.78), ranging between 3 and 12, and the median score was 10.
Table 2.
Knowledge and opinions of study participants (n=202)
| No. | Item | Frequency (n) | Percentage (%) |
|---|---|---|---|
| 1 | Overall knowledge score: mean±SD | 9.86±1.78 | |
| 2 | Overall knowledge category | ||
| Good (score >9) | 132 | 65.3 | |
| Moderate (score between 6 and up to 9) | 60 | 29.7 | |
| Weak (score <6) | 10 | 5 | |
| 3 | Colostrum is full-nutrient food for neonates | ||
| Answered correctly | 172 | 85.1 | |
| Answered incorrectly | 2 | 1 | |
| Did not know | 28 | 13.9 | |
| 4 | Best to breastfeed during the first hour of birth | ||
| Answered correctly | 165 | 81.7 | |
| Answered incorrectly | 8 | 4 | |
| Did not know | 29 | 14.3 | |
| 5 | Continuous crying means thirst or hunger | ||
| Answered correctly | 111 | 55 | |
| Answered incorrectly | 85 | 42 | |
| Did not know | 6 | 3 | |
| 6 | The more you breastfeed the more milk you will have | ||
| Answered correctly | 182 | 90.1 | |
| Answered incorrectly | 9 | 4.5 | |
| Did not know | 11 | 5.4 | |
| 7 | It is possible to breast-bump and keep milk for later | ||
| Answered correctly | 132 | 65.3 | |
| Answered incorrectly | 41 | 20.3 | |
| Did not know | 29 | 14.4 | |
| 8 | Breast milk is clean, safe, and cheap | ||
| Answered correctly | 193 | 95.5 | |
| Answered incorrectly | 5 | 2.5 | |
| Did not know | 4 | 2 | |
| 9 | Breast milk is whole meal till the sixth month of age | ||
| Answered correctly | 166 | 82.2 | |
| Answered incorrectly | 27 | 13.4 | |
| Did not know | 9 | 4.5 | |
| 10 | Breast milk gives necessary fluids till the sixth month of age | ||
| Answered correctly | 136 | 67.3 | |
| Answered incorrectly | 36 | 17.8 | |
| Did not know | 30 | 14.9 | |
| 11 | Exclusive breastfeeding is better for baby’s health | ||
| Answered correctly | 194 | 96 | |
| Answered incorrectly | 4 | 2 | |
| Did not know | 4 | 2 | |
| 12 | Exclusive breastfeeding protects against infections | ||
| Answered correctly | 187 | 92.6 | |
| Answered incorrectly | 3 | 1.5 | |
| Did not know | 12 | 5.9 | |
| 13 | Exclusive breastfeeding reduces infant colic | ||
| Answered correctly | 169 | 83.7 | |
| Answered incorrectly | 12 | 5.9 | |
| Did not know | 21 | 10.4 | |
| 14 | Exclusive breastfeeding reduces breast cancer likelihood | ||
| Answered correctly | 185 | 91.6 | |
| Answered incorrectly | 0 | 0 | |
| Did not know | 17 | 8.4 | |
Only having 3–6 children (P = 0.023) and 1-year interpregnancy interval (P = 0.005) were associated with the positive likelihood of exclusive breastfeeding [Table 3].
Table 3.
Logistic regression model estimates for the effect of predictors on exclusive breastfeeding
| Covariate | Estimate | Standard Error | P |
|---|---|---|---|
| Infant age (months) | 0.100 | 0.074 | 0.176 |
| Infant gender: Male | -0.167 | 0.381 | 0.661 |
| Mother education | |||
| Illiterate | Reference | ||
| Primary | 16.36 | 1769 | 1.000 |
| Intermediate | 0 | 2134 | 0.993 |
| Secondary | 16.16 | 1769 | 0.993 |
| University | 15.93 | 1769 | 0.993 |
| Employment | |||
| Employed | - 0.232 | 0.488 | 0.634 |
| Time with the baby | |||
| Always with baby | 0.534 | 1.074 | 0.619 |
| 1-2 hours separation | 2.303 | 1.197 | 0.0544 |
| 3-6 hours separation | Reference | NA | NA |
| >6 hours separation | 0.511 | 1.180 | 0.665 |
| Parity | |||
| Once | - 1.961 | 0.631 | 0.058 |
| More than once | Reference | ||
| No. of children | |||
| <3 | Reference | 0.408 | 0.023 |
| 3-6 | 0.930 | 0.710 | 0.372 |
| >6 | 0.634 | ||
| Planning future pregnancy | -0.515 | 0.401 | 0.198 |
| Between-pregnancy | |||
| previous interval | |||
| <1 year | - 15.199 | 1398.7 | 0.991 |
| 1 year | 2.144 | 0.768 | 0.005 |
| 2 years | 0.792 | 0.752 | 0.293 |
| >2 years | 0.640 | 0.662 | 0.334 |
| No past pregnancy | Reference | NA | NA |
| Postpartum problems | 0.279 | 0.399 | 0.484 |
| Birthplace | |||
| Public hospital | - 0.561 | 0.840 | 0.504 |
| Husband support | |||
| Yes | 1.761 | 1.037 | 0.090 |
| Age categories (years) | |||
| 15-20 | Reference | NA | NA |
| 21-25 | 13.18 | 882.74 | 0.988 |
| 26-30 | 12.77 | 882.74 | 0.988 |
| 31-35 | 12.51 | 882.74 | 0.989 |
| >36 | 13.34 | 882.74 | 0.988 |
In terms of total knowledge score [Table 4], baby age (estimate = 0.045 indicative of an increase in knowledge score by 4.6% for every month increase in age; P = 0.0218), birth in private facility (estimate = 1.0436, translates into an increase of 183% in knowledge score for women giving birth in private hospitals; P = 0.00843), and university education (estimate = 0.7336, translates into an increase for university-educated mothers by 108% in total knowledge score; P = 0.0131) were associated with better knowledge among participating mothers. See Figures 2 and 3 for the visual representation of these significant associations.
Table 4.
Binomial regression model estimates for the effect of background factors on the total knowledge score
| Covariate | Estimate | Standard Error | P |
|---|---|---|---|
| Infant age (months) | 0.045 | 0.020 | 0.0218 |
| Infant gender: Male | -0.164 | 0.107 | 0.125 |
| Mother education | |||
| Illiterate | Reference | 0.354 | 0.0949 |
| Primary | 0.592 | 0.353 | 0.4726 |
| Intermediate | 0.253 | 0.303 | 0.1120 |
| Secondary | 0.481 | 0.296 | 0.0131 |
| University | 0.734 | ||
| Employment | |||
| Employed | 0.155 | 0.134 | 0.246 |
| Time with the baby | |||
| Always with baby | 0.227 | 0.222 | 0.305 |
| 1-2 hours separation | - 0.214 | 0.287 | 0.457 |
| 3-6 hours separation | Reference | NA | NA |
| >6 hours separation | 0.480 | 0.264 | 0.069 |
| Parity | |||
| Once | - 1.155 | 0.124 | 0.213 |
| More than once | Reference | NA | NA |
| No. of children | |||
| <3 | Reference | NA | NA |
| 3-6 | 0.166 | 0.115 | 0.148 |
| >6 | - 0.180 | 0.190 | 0.343 |
| Planning future pregnancy | -0.009 | 0.107 | 0.932 |
| Between-pregnancy previous interval | |||
| <1 year | - 0.371 | 0.271 | 0.171 |
| 1 year | - 0.352 | 0.205 | 0.086 |
| 2 years | 0.136 | 0.184 | 0.462 |
| >2 years | 0.061 | 0.148 | 0.680 |
| No past pregnancy | Reference | NA | NA |
| Postpartum problems | 0.103 | 0.116 | 0.376 |
| Birthplace | |||
| Public hospital | - 1.044 | 0.396 | 0.00843 |
| Husband support | |||
| Yes | - 0.093 | 0.160 | 0.560 |
| Age categories (years) | |||
| 15-20 | Reference | NA | NA |
| 21-25 | 0.460 | 0.627 | 0.464 |
| 26-30 | 0.882 | 0.619 | 0.154 |
| 31-35 | 0.916 | 0.622 | 0.140 |
| >36 | 0.916 | 0.622 | 0.140 |
Figure 2.
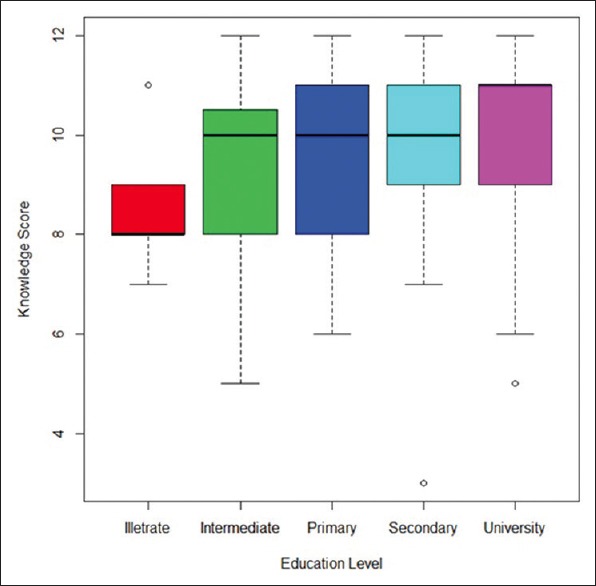
Association between education level and knowledge score
Figure 3.
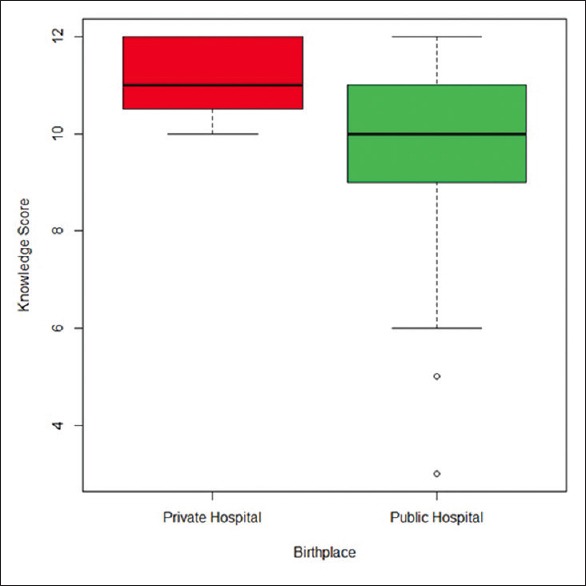
Association between place of childbirth and knowledge score
Cronbach's alpha value for the Knowledge questionnaire was 0.68 (95% confidence interval between 0.66 and 0.70), indicative of satisfactory internal consistency.[16]
Discussion
The results of this cross-sectional study revealed that the prevalence of exclusive breastfeeding among mothers in Taif is 16.3%, despite our finding that overall prevalence of breastfeeding is 87.1%. Our findings confirm the low rates of exclusive breastfeeding as practiced regionally, and globally. The current rate of exclusive breastfeeding in Taif, found by our survey, is lower than the 27.3% rate found by Saudi investigators some 15 years ago,[17] which dropped severely further in Saudi Arabia to a staggering 1.7% afterward.[18] Around the same time, a local survey estimated that 80.8% of below 6-month-old infants were not exclusively breastfed in Saudi Arabia.[19] A very recent improvement to a 31.4% exclusive breastfeeding rate was noted,[20] whereas another earlier study found only 8.3% of Saudi female teachers engage in exclusive breastfeeding.[21] This erratically worrying downhill trend in exclusive breastfeeding reflects the substantial variability in data across regions and time in Saudi Arabia, which makes interpretation difficult.[22] However, the 16.3% prevalence of exclusive breastfeeding, uncovered by our study, is almost equivalent to the 17% rate reported in Nigeria[23] and 12.5% in Egypt,[24] but clearly compares less favorably to results published from studies in Zanzibar (20.8%),[25] Ghana (38%),[26] Bangladesh (36%),[27] and Tanzania (24.1%).[28] Indeed, a lot will need to be done in terms of promoting exclusive breastfeeding to Saudi women, specifically in Taif region. Prioritization of the promotion of exclusive breastfeeding could be hypothesized to yield better maternal and child well-being and more efficient and cost-effective public health services.
One important finding from our investigation is the 13.9% rate for initiation of breastfeeding in the first hour after childbirth. This falls well below the 100% target of WHO,[1] or even the 65% rate found recently in Nepal.[29] Given its established effect on future exclusive breastfeeding practice,[30] his very low rate of the first-hour initiation of breastfeeding uncovered by this study could partly explain low rates of exclusive breastfeeding in Taif region. Very limited research was dedicated to early breastfeeding and skin-to-skin contact in the Middle East, despite its proven neonatal health benefits.[31]
On the contrary, the findings of this investigation revealed that knowledge about breastfeeding was not deficient among participating Saudi mothers. Of the sample, 65.3% scored above 75% of the knowledge questions and 95% scored more than half of the questions correctly in terms of questions related to awareness about benefits of breastfeeding. This is far better than the 47.8% knowledge level shown by Das et al.[32] and the 31% level reported by Ouchi et al.[33] or 42% among Nigerian women surveyed by Abasiattai et al.[34] At the local level, our results agree with the 78% knowledge level revealed by Elmougy et al's[35] survey in Dammam City in the Eastern Province of Saudi Arabia.
Knowledge about breastfeeding in our sample was significantly enhanced by university education, age of baby, and delivery in private health institute. Expectedly, higher education should improve popular science knowledge, including awareness of breastfeeding. This association between better education and higher knowledge was also observed by Hassan and Abdelwahed[24] in their survey of Egyptian mothers. Employment, in our sample, did not exert a substantial impact on knowledge score, in contrast to findings from regional studies.[24,36] The finding that private hospital birth coincided with improved breastfeeding-related knowledge is intriguing and warrants further investigation as what different educational (possibly midwives-led[37]) interventions are available in such health facilities.
This study showed clearly that only having 3–6 children and 1-year interpregnancy interval were strong predictors of exclusive breastfeeding. The current line of research into exclusive breastfeeding moved away from rigid demographic covariates and follows the important effect of mothers’ self-efficacy and planning.[38] Our local research policies should follow suit. Speculatively, such social cognitive qualities may have a role in limiting the number of children to between 3 and 6 and maintain regular well-planned pregnancy interval.
The results of our study capture an enormous gap between exclusive breastfeeding knowledge (as 95% of participants got more than half of the questions right) and practice (as only 16.3% of participants reported practicing it). This is counterintuitive and is against the tide of the international literature indicative of improvement in breastfeeding rates secondary to better health knowledge and education.[39,40] However, local studies conducted in Saudi Arabia have been consistent in terms of finding an inverse relationship between knowledge and practice of exclusive breastfeeding.[21,41,42] Careful consideration should be devoted to Saudi Arabia to behavioral and geosocial interventions if we want to match the 90% exclusive breastfeeding target endorsed by WHO.
The results of this paper have the potential to help policymakers in Primary Care device-focused educational interventions to improve rates of exclusive breastfeeding in Saudi Arabia. Primary Care physicians are usually the first point of contact for pregnant women and mothers to be. The advice in terms of exclusive breastfeeding from family physicians to this cohort of patients is crucial.
This study has uniquely contrasted knowledge and practices related to exclusive breastfeeding in Saudi Arabia. However, a couple of limitations need to be borne in mind before generalizing its results. Recall bias and social desirability could have played a part in shaping the results. Given the cross-sectional nature of the study, there was little to do to counteract their adverse impact.
Further research direction should implement a longitudinal design to explore the cognitive and social underpinnings of exclusive breastfeeding behavior.
Conclusion
In conclusion, findings indicated that low exclusive breastfeeding practice exists in Saudi Arabia despite adequate knowledge about its benefits and necessity. It is recommended that more research should focus on the social and cognitive determinants of exclusive breastfeeding in Saudi Arabia and the Middle Eastern region.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.WHO, Breastfeeding factsheet. [Last accessed on 2019 Jun 25]. Available from: https://www.who.int/nutrition/topics/exclusive_breastfeeding/en/
- 2.Sheehan A, Schmied V, Barclay L. Complex decisions: Theorizing women's infant feeding decisions in the first 6 weeks after birth. J Adv Nurs. 2010;66:371–80. doi: 10.1111/j.1365-2648.2009.05194.x. [DOI] [PubMed] [Google Scholar]
- 3.Hsu PS, Nanan R. Does breast milk nurture T lymphocytes in their cradle? Front Pediatr. 2018;6:268. doi: 10.3389/fped.2018.00268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Biks GA, Berhane Y, Worku A, Gete YK. Exclusive breast feeding is the strongest predictor of infant survival in Northwest Ethiopia: A longitudinal study. J Health Popul Nutr. 2015;34:9. doi: 10.1186/s41043-015-0007-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shohieb S, Nazer H. Springer: Textbook of Clinical Pediatrics. 2012 [Google Scholar]
- 6.Chehab R, Nasreddine L, Zgheib R, Forman M. C-section delivery is a barrier to and demographic-maternal-child factors have mixed effects on the length of exclusive breastfeeding under nutrition transition in Lebanon (P11-058-19) Curr Dev Nutr. 2019;3(Suppl 1) pii: nzz048.P11.058.19. [Google Scholar]
- 7.Wennberg AL, Jonsson S, Zadik Janke J, Hörnsten Š. Online perceptions of mothers about breastfeeding and introducing formula: Qualitative study. JMIR Public Health Surveill. 2017;3:e88. doi: 10.2196/publichealth.8197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.BouDiab S, Werle C. What motivates women to breastfeed in Lebanon: An exploratory qualitative analysis. Appetite. 2018;123:23–31. doi: 10.1016/j.appet.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Chopel A, Soto D, Joiner B, Benitez T, Konoff R, Rios L, et al. Multilevel factors influencing young mothers’ breastfeeding: A qualitative CBPR study. J Hum Lact. 2019;35:301–17. doi: 10.1177/0890334418812076. [DOI] [PubMed] [Google Scholar]
- 10.Batterjee, Modia Abd Almajeed. A phenomenology study examining partial breast - feeding in the Kingdom of Saudi Arabia.: ProQuest Dissertations and Theses, University of Phoenix. 2009 [Google Scholar]
- 11.Fehintola FO, Fehintola AO, Ogunlaja OA, Awotunde TO, Aworinde O, Ogunlaja IP. Patterns and predictors of exclusive breastfeeding among mothers in Ile Ife, Nigeria. Sudan J Med Sci. 2016;11:69–78. [Google Scholar]
- 12.Mohammed ES, Ghazawy ER, Hassan EE. Knowledge, attitude, and practices of breastfeeding and weaning among mothers of children up to 2 years old in a rural area in el-minia governorate, Egypt. J Family Med Prim Care. 2014;3:136–40. doi: 10.4103/2249-4863.137639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sultania P, Agrawal NR, Rani A, Dharel D, Charles R, Dudani R. Breastfeeding knowledge and behavior among women visiting a tertiary care center in India: A cross-sectional survey. Ann Glob Health. 2019;85 doi: 10.5334/aogh.2093. pii: 64. doi: 10.5334/aogh.2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Habibi M, Laamiri FZ, Aguenaou H, Doukkali L, Mrabet M, Barkat A. The impact of maternal socio-demographic characteristics on breastfeeding knowledge and practices: An experience from Casablanca, Morocco. Int J Pediatr Adolesc Med. 2018;5:39–48. doi: 10.1016/j.ijpam.2018.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.ARStud io Team. Boston, MA: RStudio, Inc.; 2016. [Last accessed on 2019 Jun 25]. RStudio: Integrated Development for R. Available from: http://www.rstudio.com/ [Google Scholar]
- 16.Bland JM, Altman DG. Cronbach's alpha. BMJ. 1997;314:572. doi: 10.1136/bmj.314.7080.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ogbeide DO, Siddiqui S, Al Khalifa IM, Karim A. Breast feeding in a Saudi Arabian community. Profile of parents and influencing factors. Saudi Med J. 2004;25:580–4. [PubMed] [Google Scholar]
- 18.Al-Hreashy FA, Tamim HM, Al-Baz N, Al-Kharji NH, Al-Amer A, Al-Ajmi H, et al. Patterns of breastfeeding practice during the first 6 months of life in Saudi Arabia. Saudi Med J. 2008;29:427–31. [PubMed] [Google Scholar]
- 19.El Mouzan MI, Al Omar AA, Al Salloum AA, Al Herbish AS, Qurachi MM. Trends in infant nutrition in Saudi Arabia: Compliance with WHO recommendations. Ann Saudi Med. 2009;29:20–3. doi: 10.4103/0256-4947.51812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alzaheb RA. Factors influencing exclusive breastfeeding in Tabuk, Saudi Arabia. Clin Med Insights Pediatr. 2017;11:1179556517698136. doi: 10.1177/1179556517698136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Binali AM. Breastfeeding knowledge, attitude and practice among school teachers in Abha female educational district, southwestern Saudi Arabia. Int Breastfeed J. 2012;7:10. doi: 10.1186/1746-4358-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Al Juaid DA, Binns CW, Giglia RC. Breastfeeding in Saudi Arabia: A review. Int Breastfeed J. 2014;9:1. doi: 10.1186/1746-4358-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Demographic Health Survey. 2013. [Last accessed on 2019 Jun 29]. Available from: https://dhsprogram.com/pubs/pdf/FR293/FR293.pdf .
- 24.Hassan S, Abdelwahed W. Knowledge and practices of exclusive breast feeding in Fayoum. Egypt J Community Med. 2015;33:61–77. [Google Scholar]
- 25.Khamis AG, Omar AM, Suleiman SA, Ali FS. Prevalence of exclusive breastfeeding and its predictors among mothers in Micheweni, Chake-Chake and North ‘A’ districts, Zanzibar. Clinics Mother Child Health. 2017;14:259. [Google Scholar]
- 26.Mogre V, Dery M, Gaa PK. Knowledge, attitudes and determinants of exclusive breastfeeding practice among Ghanaian rural lactating mothers. Int Breastfeed J. 2016;11:12. doi: 10.1186/s13006-016-0071-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Joshi PC, Angdembe MR, Das SK, Ahmed S, Faruque ASG, Ahmed T. Prevalence of exclusive breastfeeding and associated factors among mothers in rural Bangladesh: A cross-sectional study. Int Breastfeed J. 2014;9:7. doi: 10.1186/1746-4358-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maonga AR, Mahande MJ, Damian DJ, Msuya SE. Factors affecting exclusive breastfeeding among women in Muheza District Tanga Northeastern Tanzania: A mixed method community based study. Matern Child Health J. 2016;20:77–87. doi: 10.1007/s10995-015-1805-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sanjel K, Amatya A. Determinants of timely initiation of breastfeeding among disadvantaged ethnic groups in midwest Nepal. J Nepal Health Res Counc. 2019;16:385–91. [PubMed] [Google Scholar]
- 30.Ogbo FA, Ezeh OK, Khanlari S, Naz S, Senanayake P, Ahmed KY, et al. Determinants of exclusive breastfeeding cessation in the early postnatal period among culturally and linguistically diverse (CALD) Australian mothers. Nutrients. 2019:11. doi: 10.3390/nu11071611. pii: E1611. doi: 10.3390/nu11071611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Karim F, Khan ANS, Tasnim F, Chowdhury MAK, Billah SM, Karim T, et al. Prevalence and determinants of initiation of breastfeeding within one hour of birth: An analysis of the Bangladesh Demographic and Health Survey, 2014. PLoS One. 2019;14:e0220224. doi: 10.1371/journal.pone.0220224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Das BR, Bora PJ, Borah M. Awareness of exclusive breastfeeding among the women of reproductive age group in urban slums. J Med Sci Clin Res. 2018;6:93–9. [Google Scholar]
- 33.Oche MO, Umar AS, Ahmed H. Knowledge and practice of exclusive breastfeeding in Kware, Nigeria. Afr Health Sci. 2011;11:518–23. [PMC free article] [PubMed] [Google Scholar]
- 34.Abasiattai A, Etukumana E, Nyong E, Eyo U. Knowledge and practice of exclusive breastfeeding among antenatal attendees in Uyo, Southern Nigeria. Gaziantep Med J. 2014;20:130–5. [Google Scholar]
- 35.Elmougy AM, Matter MK, Shalaby NM, El-Regal ME, Abu Ali WH, Aldossary SS, et al. Knowledge, attitude and practice of breastfeeding among working and non-working mothers in Saudi Arabia. Egypt J Occup Med. 2018;42:133–50. [Google Scholar]
- 36.Chaudhary RN, Shah T, Raja S. Knowledge and practice of mothers regarding breast feeding: A hospital based study. BPKIHS Dharan. 2011;9:194–200. [Google Scholar]
- 37.McAllister H, Bradshaw S, Ross-Adjie G. A study of in-hospital midwifery practices that affect breastfeeding outcomes. Breastfeed Rev. 2009;17:11–5. [PubMed] [Google Scholar]
- 38.Martinez-Brockman JL, Shebl FM, Harari N, Pérez-Escamilla R. An assessment of the social cognitive predictors of exclusive breastfeeding behavior using the health action process approach. Soc Sci Med. 2017;182:106–16. doi: 10.1016/j.socscimed.2017.04.014. [DOI] [PubMed] [Google Scholar]
- 39.Suárez-Cotelo MDC, Movilla-Fernández MJ, Pita-García P, Arias BF, Novío S. Breastfeeding knowledge and relation to prevalence. Rev Esc Enferm USP. 2019;53:e03433. doi: 10.1590/S1980-220X2018004503433. [DOI] [PubMed] [Google Scholar]
- 40.Zielińska MA, Sobczak A, Hamułka J. Breastfeeding knowledge and exclusive breastfeeding of infants in first six months of life. Rocz Panstw Zakl Hig. 2017;68:51–9. [PubMed] [Google Scholar]
- 41.Alwelaie YA, Alsuhaibani EA, Al-Harthy AM, Radwan RH, Al-Mohammady RG, Almutairi AM. Breastfeeding knowledge and attitude among Saudi women in Central Saudi Arabia. Saudi Med J. 2010;31:193–8. [PubMed] [Google Scholar]
- 42.Hegazi MA, Allebdi M, Almohammadi M, Alnafie A, Al-Hazmi L, Alyoubi S. Factors associated with exclusive breastfeeding in relation to knowledge, attitude and practice of breastfeeding mothers in Rabigh community, Western Saudi Arabia. World J Pediatr. 2019 Jun;18 doi: 10.1007/s12519-019-00275-x. doi: 10.1007/s12519-019-00275-x. [DOI] [PubMed] [Google Scholar]


