Abstract
Nowadays one of the most frequent reasons of death in the world is coronary artery disease. CABG is a portion of a common revascularization mediation that is done to supervise CAD by applying vessels that are grafted to revascularize vessels distal from the blockage. Different sources of grafts are included veins (specifically saphenous) and arteries (include mammary and radial arteries). Multiple conduits are used to this end, but the most suitable is left internal mammary artery (LIMA) to the left anterior descending artery (LAD) as a golden standard. Saphenous vein grafts were the guiding approach applied by the vast majority of cardiac surgeons in the 1970s, even though all approaches were supported by doctors. Although the radial artery graft was introduced simultaneously, this approach due to its complications was not as prevalent. This article is aimed to define the pros and cons of applying each kind of grafts according to the results furnished by existent studies. It has also examined the benefits provided by total arterial coronary artery bypass graft against CABG including venous graft for patients with CAD from the perspective of surgeons.
Keywords: Arteries, coronary artery bypass grafting, coronary disease, multiple conduits, myocardial revascularization, veins
Introduction
The prevalence rate of coronary artery disease (CAD), prevalently brought out by atherosclerosis, has noticeably lower within populations that have lower life expectation.[1] Coronary artery bypass graft surgery (CABG) has still known as the main approach carried out by cardiac surgeons. Due to the advancements in intraoperative technique and post-operative care, CABG being suggested to a more patients with less adverse occurrences and complications.[2] CABG is a kind of open-heart surgery during which a section of a blood vessel from the aorta to the coronary artery is grafted in order to bypassing the blocked section of the coronary artery and expanding the blood delivery to the heart. According to successful using of the left internal mammary artery to bypass the left anterior descending coronary artery, it is thought that arterial grafts to be better conduits compared to saphenous vein grafts for CABG.[3] Parasca et al.,[4] cited that percutaneous coronary intervention (PCI) is a non-surgical approach that supplies a less intrusive interference of CAD in patients who are stable and used in also is patients who the coronary arteries of the heart get narrowing.
Olearchyk[5] was who performed the first prosperous internal mammary artery-coronary artery anastomosis. Afterward, Captur et al.[6] related using of saphenous vein in 171 patients to restore the blood circulation of coronary artery. Duhaylongsod et al.[7] reported thoracoscopic approach as a medical procedure involving internal examination or biopsy of collecting the left internal mammary artery (IMA). Weintraub et al.[8] reported that the number of CABG is rapidly reduced in 2012. Totally, it is supposed that arterial conduits have superior patency over saphenous vein grafts (SVG), but the existing data on radial artery grafts is imperfect. Jolly et al.[9] showed that radial has higher patency rates than SVG (92% against 86%). Anyway, it is thought that arterial grafts to be better conduits compared to saphenous vein grafts for CABG.[10]
By implementing grafted vessels to revascularization vessels distal from the narrowed or blockage, CABG is known as a section of revascularization mediation that is usually applied to manage CAD. Various sources of grafts are included veins (specifically saphenous) and arteries (include mammary and radial arteries).[11] In such clinical operations, left anterior descending is regularly grafted with an arterial conduit, in most situations with the left internal thoracic artery. By using of arterial and venous conduits, other types of grafts could be performed, including single grafts, sequential grafts, or composite grafts. According to successful using of the left internal mammary artery to bypass the left anterior descending coronary artery, it is thought that arterial grafts to be better conduits compared to saphenous vein grafts for CABG.[12] This article is aimed to define the pros and cons of applying each kind of grafts according to the findings accomplished by related studies. Authors in this study tried to compare the consequences of coronary artery revascularization and the data based on if CABG done in the study is TACABG or VCABG.
Various Applications of Arterial and Venous Graft
Problems with graft surgery
According to previous studies and more specially, the case study of Al-Sabti et al.,[13] about ongoing challenges of searching the most successfully second coronary artery bypass graft, the evaluation of each graft can be performed by the procedure preparation requirements, time required to do the surgery, and surgery skills requirements. According to Andrew Foreman et al.,[14] Allen's test, also called the Allen test works like a medical sign that can be used in physical examination of arterial blood flow. This test was named for Edgar Van Nuys Allen, the first one who described the original version of the test [Figure 1].
Figure 1.
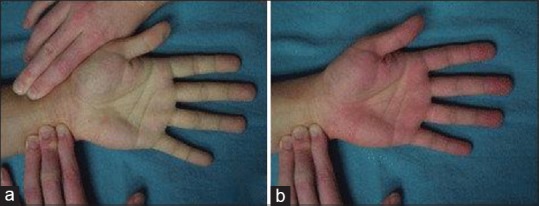
The Allen test. (Derived from: Andrew Foreman et al.,[14]). (a) The paleness of hand due to occlusion of both radial and ulnar artery inflow to the hand. (b) The redness of the hand is quickly return after releasing of the radial artery pressure that confirms flow through the radial artery
Median sternotomy for the open-heart surgery is the standard procedure of operation in all patients. At the first, when internal thoracic arteries (ITAs) that are better called as internal mammary arteries (IMAs) is needed, the method of surgery is the internal thoracic artery skeletonization. Second, when there is need to radial arteries (RAs), the surgery is performed by providing an open atraumatic entry using harmonic scalpel or cautery with lower power. Eventually, when saphenous vein grafts (SVGs) are needed, the chosen technique would be lower leg open entry. In this case, the surgery ream should avoid the thigh vein.[15,16] In their study about the total arterial revascularization analysis, Tatoulis et al.,[15] reported the mean of aortic cross-clamping time for total arterial revascularization (TAR) and non-total arterial revascularization (n-TAR) equals to 60.6 and 63.8 min correspondingly. They also reported that the perfusion times taken by each approach are 80.2 and 90.7, respectively. The longer the duration of the open surgery, the greater the risk of infection, even in patient who receive prophylaxis antibiotics.
Clinical benefits and natural restrictions of radial artery
The studies of Samak et al.,[16] has demonstrated that condition of ulnar flow must be satisfied to guarantee provide the needed blood. It should be noted that arteries with their inner diameter less than 2 millimeters or calcified radial arteries shouldn’t be chosen for harvesting. The patients who their radial arteries are removed may undergo weakness in their forearm or feel sensory abnormalities after removal. When patients positioning to face such a condition, using of vasodilators as radial arteries is essential for their noticeable spasmodic reactions to hypothermia and vasoconstrictors. According to the study of Gaudino et al.,[17] the use of radial-artery grafts for CABG during a follow-up period of 5 years, leads to smaller rates of opposed cardiac events and a bigger rates of patency, when comparing with the use of saphenous-vein grafts. Moreover, they reported that using of radial-artery grafts is related to considerably lower risk of occlusion, lower occurrence of myocardial infarction and halve the repetition of revascularization at follow-up angiography.
Outcomes of Operation
Comparing the patency of vein/artery
In their studies, Goldman et al.,[3] compared saphenous vein grafts (SVG) and interior thoracic artery (ITA) when they are functioned as conduits. Through the 10-year angiogram obtained in their studies, they concluded that ITA had better patency. According to the recent studies, the range of patients throughout recent 10 years has decreased, demonstrating that the rate number of patent grafts is constantly lower in SVG than ITA.[3] Domanski et al.,[18] reported that, arterial grafts are better conduits compared to saphenous vein grafts that are vulnerable to atherosclerosis development. This factor can limit the proper prognosis of revascularization. In a more recently study, Tatoulis et al.,[15] attempted to assess right ITA (RITA) patency in comparison with other conduit vessels at a period of 10 years, and derived the patency rates of 90%, 70%, and 50% for RITA, RA, and SVG, respectively. Finally, they acknowledged the potency of saphenous venous conduits are lower than arterial conduits.
TACABG and VCABG Clinical Outcomes
The most important factors in comparing VCABG with TACABG are their adverse consequences and rate of death known as mortality. Mäkikallio et al.,[19] reported that main disease remained in all patients with 66.2 years old in average, the death rate of patients according to the 5-year Kaplan-Meier outcome estimation was 9%, 18 percentage of patients experienced main adverse cardiovascular and cerebrovascular events (MACE), incidence of stroke and total rate of revascularization was 2% and 10%, respectively. In order to minimize orientation bias, the Kaplan-Meier judgements were arranged in groups based on SYNTAX tool that score complexity of coronary artery disease. Parasca et al.,[4] estimated secondary arterial graft effect on a 5-years period outcomes after coronary artery bypass grafting and cooperative interaction between cardiac surgery trial and percutaneous coronary intervention with TAXUS. Their study indicated that mortality rate due to the all causes was 8.4%, stroke incidence was 3.2% and total revascularization rate was 6.6%. From the other side, comparing the post-hoc analysis of the SYNTAX examination in patients received a second arterial conduit with those experienced single ITA grafting with extra vein grafts depicted that MACCE in venous and arterial groups were 21.4% and 23.3%, respectively. Furthermore, they reported the mortality of 9.1% and 9.5% in the arterial and venous groups, respectively. From the results of the previous studies it could be concluded that the MACCE outcome of single ITA with supplementary vein graft is better than total arterial revascularization.[4]
Left main coronary artery disease (LMCA)
Left main coronary artery (LMCA) as a subtype of ischemic heart disease, has highest risk among the others. It has conventionally considered as an indication for coronary artery bypass grafting (CABG). LMCA disease would been detected within four to six% of patients those receive coronary arteriography, that is generally related to multivessel coronary artery disease (MVCAD). Buxton et al.,[20] collected more detailed information about the effect of total arterial CABG on left main disease and successfully gathered the most relative data from the studies about radial artery patency and clinical outcomes (RAPCO). According to Buxton et al.,[20] research, it could be concluded that RAPCO study is a type of experiment that is the ability to reduce bias when testing new treatments, monitoring outcomes and connected it to other factors such as protection or suspected risk factors and also providing a strong single-center trial. Accordingly, the outcomes of VCABG and TACABG for patients who suffer from left main coronary artery disease (LMCA) are shown in Table 1. Tatoulis et al.,[15] represented that TACABG resulted in higher perioperative as well as long-term survival. Although, the difference between these two percentages was not significant, but by increasing the time period of study to 10 years, this difference enhanced too.
Table 1.
The outcomes of VCABG and TACABG for patients who suffer from left main coronary artery disease. Derived from[20]
| Studied Cases | TACABG | VCABG | |
|---|---|---|---|
| TAR Group | RAPCO | ART (single graft group) | |
| No. of patients | 6232 | 140 | 1554 |
| Average of age (years) | 64.4 | 60.1 | 63.5 |
| Death rate (from all causes) | n/a | 3 | 130 |
| Sudden cardiac death (SCD) | n/a | n/a | n/a |
| Vascular death (sudden cardiac death) | n/a | n/a | n/a |
| non-procedural myocardial blockage (nPMB) | n/a | n/a | n/a |
| Revascularization (total) | n/a | n/a | 103 |
| CABG revascularization | n/a | n/a | n/a |
| PCI revascularization | n/a | 3 | n/a |
| Revascularization in LMCA disease | n/a | n/a | n/a |
| Surgical revascularization for a lesion | n/a | n/a | n/a |
| De novo lesion revascularization | n/a | n/a | n/a |
| Definite stent thrombosis | n/a | n/a | n/a |
| Stroke | n/a | n/a | 49 |
CABG: coronary artery bypass grafting; PCI: percutaneous coronary intervention; TACABG: total arterial coronary artery bypass graft; VCABG: venous coronary artery bypass graft; LMCA: left main coronary artery; TAR: total arterial revascularization; RAPCO/ART: clinical trials names (RA was the only conduit used by RAPCO)
Discussion
Nowadays the most frequent cardiac surgery operation carried out all around the world is CABG. This comprehensive revascularization method is proved to be the most successful method among most of patients that suffer from coronary artery disease. The main factor for successfulness of a procedure is its long-term conduit patency.[21] The application of arterial conduits in the revascularization of coronary arteries has better outcomes than using venous conduits.[22] Applying a second arterial graft to patients with high-risk, for example those suffer from unstable angina or reduced ventricular function has some advantages that become obvious within the first decade after operation. But unfortunately the secondary arterial conduit location and utilizing the subsequent strategy don’t enhance the survival advantage.[23] Selection of Conduits for CABG as a Novel Coronary Artery Surgery is shown in Figure 2. To provide the best outcome from CABG, the surgeon should assure that the used vessels are intact and has sufficient quality. It is also important to investigate the ulnar artery patency while using radial artery, but that is not required for saphenous vein collateral circulation. However, Luckraz et al.[22] asserted that investigating saphenous vein by application of Doppler ultrasonography helps in improving diagnosis of SVG.
Figure 2.
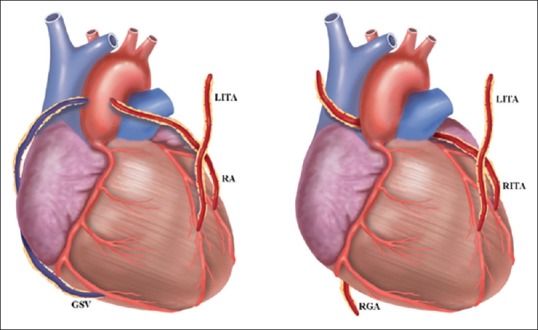
Graft configurations that could be selected by multiple arterial conduits.[15] CABG; Coronary artery bypass graft, GSV; Great saphenous vein, LITA; Left internal thoracic artery, RA; Radial artery, RGA; Right gastroepiploic artery, RITA; Right internal thoracic artery
The total of perfusion time and cross-clamp time is longer in the VCABG than in TACABG. Operation time is another important factor. Tatoulis et al.[24] declared that the entire of perfusion time and cross clamp time needed in VCABG is longer than in TACABG. Di Mauro et al.[25] stated that, graft configuration can influence the long-term outcomes by the use of a propensity-score approach. They also found that, the rate of MACCES and sudden mortality was not difference between studied groups, and also, configuration of the surgery doesn’t affect BIMA grafting. Furthermore, they argued that using new technique that is made up of a right Y-graft intensify the BIMA grafting flexibility and is the best method to use in surgical approaches for laser revascularization that also called myocardial revascularization.
Buxton and Hayward[26] declared that the short-term outcomes of the post-operative is the third important factor to be considered while CABG operation. Taggart et al.[27] reported that through accurate graft harvesting and keeping the integrity of pleural cavities, it's possible to reduce the postoperative complications as well as hospital costs. Tranbaugh et al.[11] stated that deep sternal wound infection (DSWI) is among the most hazardous complications of TACABG. Deo et al.[28] found that harvesting internal thoracic arteries in old people may enhance the incidence of DSWI. Accordingly, they concluded that pedicled harvesting results in a considerable increase in the risk of DSWI after operation and should be discouraged when using both ITA.
Suzuki et al.[29] reported that the rate of morbidity postoperative SWI is less for skeletonized ITA compared to pedicled ITA after CABG. Deo et al.,[30] introduced the main approaches for minimizing deep sternal wound infection (DSWI) after BIMA grafting, that are included appropriate antibiotic prophylaxis, microbiological factors, and tight glycemic control. They also presented surgical techniques to reduce deep sternal wound infection (DSWI) after BIMA harvest, involving moderated pedicle harvest accompanied by larger protection of sternal closure and sternal blood supply, IMA harvesting using skeletonized and semiskeletonized with fewer devascularization of sternum and stability techniques.
The forth important factor when choosing a procedure is long-term outcome.[31] The risk of death in 10 years after operation is 1.61 times greater when using SVG rather ITA that further indicates superiority of arterial conduits.[32] On the other hand, using off-pump coronary artery bypass is preferable and results in reducing the risk of death, morbidity or mortality, stroke and hospitalization time. Anyway, enough training and investment should be allocated by both the patients and healthcare system to achieve the desired benefits.[29]
Another determinant that strongly influences the outcome of graft is difficulty of target vessel stenosis in relation to its location and using an arterial revascularization approach it is of great importance to specify functional character description of the target vessel injury. The use of fractional flow supply instead of angiography to plan the configuration of conduits in the future allows for better physiological combination of graft and coronary flow and is likely to enhance the long-term patency and clinical effective results. From the above-mentioned studies, it can be concluded that TACABG method has generally more advantages than VCABG, but increasing the usage cases of this method firstly requires to assure surgeons of priority of this method.
Conclusion
The best performing arterial-coronary conduit in patients with MVCAD in term of patency and in clinical outcome is LIMA. It worth noting that preparation time in TACABG is longer than in non-total arterial CABG. The use of TACABG, whenever possible, had associated with better outcomes in term of short- and long-term survival than using VCABG. Moreover, as compared to venous conduits, arterial conduits have been approved to have longer durability patency and are more protective. Although, 30-day effectiveness for two of TACABG and VCABG was exactly alike, but the rate of death in long-term was higher in VCABG. So far, internal thoracic arteries have been the best arteries available to be used as conduits and provided the best outcomes among others, even for those exposed to higher risk of complications. If heart surgical team look at the graft selection as a strategic issue, more appropriate applications of arterial grafts can be found.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Stone GW, Sabik JF, Serruys PW, Simonton CA, Généreux P, Puskas J, et al. EXCEL Trial Investigators. Everolimus-eluting stents or bypass surgery for left main coronary artery disease. N Engl J Med. 2016;375:2223–35. doi: 10.1056/NEJMoa1610227. [DOI] [PubMed] [Google Scholar]
- 2.Mackay J, Mensah GA, Greenlund K. The atlas of heart disease and stroke. World Health Organization. 2004 [Google Scholar]
- 3.Goldman S, Zadina K, Moritz T, Ovitt T, Sethi G, Copeland JG, et al. Longterm patency of saphenous vein and left internal mammary artery grafts after coronary artery bypass surgery: Results from a department of veteran's affairs cooperative study. J Am Coll Cardiol. 2004;44:2149–56. doi: 10.1016/j.jacc.2004.08.064. [DOI] [PubMed] [Google Scholar]
- 4.Parasca CA, Head SJ, Mohr FW, Mack MJ, Morice MC, Holmes DR, Jr, et al. SYNTAX Investigators. The impact of a second arterial graft on 5-year outcomes after coronary artery bypass grafting in the synergy between percutaneous coronary intervention with TAXUS and cardiac surgery trial and registry. J Thorac Cardiovasc Surg. 2015;150:597–606. doi: 10.1016/j.jtcvs.2015.05.010. e592. [DOI] [PubMed] [Google Scholar]
- 5.Olearchyk AS, Vasilii I, Kolesov A pioneer of coronary revascularization by internal mammary-coronary artery grafting. J Thorac Cardiovasc Surg. 96:13–8. [PubMed] [Google Scholar]
- 6.Captur G. Memento for René Favaloro. Tex Heart Inst J. 31:47–60. [PMC free article] [PubMed] [Google Scholar]
- 7.Duhaylongsod FG, Mayfield WR, Wolf RK. Thoracoscopic harvest of the internal thoracic artery: A multicenter experience in 218 cases. Ann Thorac Surg. 9;66:1012–7. doi: 10.1016/s0003-4975(98)00731-0. [DOI] [PubMed] [Google Scholar]
- 8.Weintraub WS, Grau-Sepulveda MV, Weiss JM, O’Brien SM, Peterson ED, Kolm P, et al. Comparative effectiveness of revascularization strategies. N Engl J Med. 366:1467–76. doi: 10.1056/NEJMoa1110717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jolly SS, Yusuf S, Cairns J, Niemelä K, Xavier D, Widimsky P, et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): A randomised, parallel group, multicentre trial. Lancet. 377:1409–20. doi: 10.1016/S0140-6736(11)60404-2. [DOI] [PubMed] [Google Scholar]
- 10.Athanasiou T, Saso S, Rao C, Vecht J, Grapsa J, Dunning J, et al. Radial artery versus saphenous vein conduits for coronary artery bypass surgery: Forty years of competition-which conduit offers better patency? A systematic review and meta-analysis. Eur J Cardiothorac Surg. 40:208–20. doi: 10.1016/j.ejcts.2010.11.012. [DOI] [PubMed] [Google Scholar]
- 11.Tranbaugh RF, Dimitrova KR, Lucido DJ, Hoffman DM, Dincheva GR, Geller CM, et al. The second best arterial graft: A propensity analysis of the radial artery versus the free right internal thoracic artery to bypass the circumflex coronary artery. J Thorac Cardiovasc Surg. 147:133–40. doi: 10.1016/j.jtcvs.2013.08.040. [DOI] [PubMed] [Google Scholar]
- 12.Glineur D, Kuschner CE, Grau JB. Bilateral internal thoracic artery graft configuration and coronary artery bypass grafting conduits. Curr Opin Cardiol. 31:625–34. doi: 10.1097/HCO.0000000000000342. [DOI] [PubMed] [Google Scholar]
- 13.Al-Sabti HA, Al Kindi A, Al-Rasadi K, Banerjee Y, Al-Hashmi K, Al-Hinai A. Saphenous vein graft vs. radial artery graft searching for the best second coronary artery bypass graft. J Saudi Heart Assoc. 25:247–54. doi: 10.1016/j.jsha.2013.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foreman A, de Almeida JR, Gilbert R, Goldstein DP. The Allen's test: Revisiting the importance of bidirectional testing to determine candidacy and design of radial forearm free flap harvest in the era of trans radial endovascular access procedures. J Otolaryngol Head Neck Surg. 44:47. doi: 10.1186/s40463-015-0096-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tatoulis J, Wynne R, Skillington PD, Buxton BF. Total arterial revascularization: Achievable and prognostically effective-a multicenter analysis. Ann Thorac Surg. 100:1268–75. doi: 10.1016/j.athoracsur.2015.03.107. [DOI] [PubMed] [Google Scholar]
- 16.Samak M, Fatullayev J, Sabashnikov A, Zeriouh M, Schmack B, Ruhparwar A, et al. Total arterial revascularization: Bypassing antiquated notions to better alternatives for coronary artery disease. Med Sci Monit Basic Res. 22:107–14. doi: 10.12659/MSMBR.901508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gaudino M, Benedetto U, Fremes S, Biondi-Zoccai G, Sedrakyan A, Puskas JD, et al. Radial-artery or saphenous-vein grafts in coronary-artery bypass surgery. N Engl J Med. 378:2069–77. doi: 10.1056/NEJMoa1716026. [DOI] [PubMed] [Google Scholar]
- 18.Domanski MJ, Borkowf CB, Campeau L, Knatterud GL, White C, Hoogwerf B, et al. Prognostic factors for atherosclerosis progression in saphenous vein grafts: The postcoronary artery bypass graft (Post-CABG) trial. Post-CABG Trial Investigators. J Am Coll Cardiol. 36:1877–83. doi: 10.1016/s0735-1097(00)00973-6. [DOI] [PubMed] [Google Scholar]
- 19.Mäkikallio T, Holm NR, Lindsay M, Spence MS, Erglis A, Menown IB, et al. NOBLE study investigators. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): A prospective, randomised, open-label, non-inferiority trial. Lancet. 388:2743–52. doi: 10.1016/S0140-6736(16)32052-9. [DOI] [PubMed] [Google Scholar]
- 20.Buxton BF, Raman JS, Ruengsakulrach P, Gordon I, Rosalion A, Bellomo R, et al. Radial artery patency and clinical outcomes: Five-year interim results of a randomized trial. J Thorac Cardiovasc Surg. 125:1363–71. doi: 10.1016/s0022-5223(02)73241-8. [DOI] [PubMed] [Google Scholar]
- 21.Lopes RD, Mehta RH, Hafley GE, Williams JB, Mack MJ, Peterson ED, et al. Project of Ex Vivo Vein Graft Engineering via Transfection IV (PREVENT IV) Investigators. Relationship between vein graft failure and subsequent clinical outcomes after coronary artery bypass surgery. Circulation. 125:749–56. doi: 10.1161/CIRCULATIONAHA.111.040311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luckraz H, Lowe J, Pugh N, Azzu AA. Pre-operative long saphenous vein mapping predicts vein anatomy and quality leading to improved post-operative leg morbidity. Interact Cardiovasc Thorac Surg. 7:188–91. doi: 10.1510/icvts.2007.166645. [DOI] [PubMed] [Google Scholar]
- 23.Gagné K, Deschamps A, Cartier R. Sequential internal thoracic artery bypass is safe but does not improve survival. Ann Thorac Surg. 98:23–9. doi: 10.1016/j.athoracsur.2014.03.036. [DOI] [PubMed] [Google Scholar]
- 24.Tatoulis J, Wynne R, Skillington PD, Buxton BF. Total arterial revascularization: A superior strategy for diabetic patients who recoronary surgery. Ann Thorac Surg. 102:1948–55. doi: 10.1016/j.athoracsur.2016.05.062. [DOI] [PubMed] [Google Scholar]
- 25.Di Mauro M, Iacò AL, Allam A, Awadi MO, Osman AA, Clemente D, et al. Bilateral internal mammary artery grafting: In situ versus Y-graft. Similar 20-year outcome. Eur J Cardiothorac Surg. 50:729–34. doi: 10.1093/ejcts/ezw100. [DOI] [PubMed] [Google Scholar]
- 26.Buxton BF, Hayward PA. The art of arterial revascularization-total arterial revascularization in patients with triple vessel coronary artery disease. Ann Cardiothorac Surg. 2:543–51. doi: 10.3978/j.issn.2225-319X.2013.07.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taggart DP, Altman DG, Gray AM, Lees B, Nugara F, Yu LM, et al. for the ART Investigators. Randomized trial to compare bilateral vs. single internal mammary coronary artery bypass grafting: 1-year results of the Arterial Revascularisation Trial (ART) Eur Heart J. 31:2470–81. doi: 10.1093/eurheartj/ehq318. [DOI] [PubMed] [Google Scholar]
- 28.Deo SV, Altarabsheh SE, Shah IK, Cho YH, McGraw M, Sarayyepoglu B, et al. Are two really always better than one.Results, concerns and controversies in the use of bilateral internal thoracic arteries for coronary artery bypass grafting in the elderly: A systematic review and meta-analysis? Int J Surg. 16:163–70. doi: 10.1016/j.ijsu.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 29.Suzuki T, Asai T, Nota H, Kuroyanagi S, Kinoshita T, Takashima N, et al. Early and longterm patency of in situ skeletonized gastroepiploic artery after off-pump coronary artery bypass graft surgery. Ann Thorac Surg. 96:90–5. doi: 10.1016/j.athoracsur.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 30.Deo SV, Shah IK, Dunlay SM, Erwin PJ, Locker C, Altarabsheh SE, et al. Bilateral internal thoracic artery harvest and deep sternal wound infection in diabetic patients. Ann Thorac Surg. 95:862–9. doi: 10.1016/j.athoracsur.2012.11.068. [DOI] [PubMed] [Google Scholar]
- 31.Gaudino M, Puskas JD, Di Franco A, Ohmes LB, Iannaccone M, Barbero U, et al. Three arterial grafts improve late survival: A meta-analysis of propensity-matched studies. Circulation. 135:1036–44. doi: 10.1161/CIRCULATIONAHA.116.025453. [DOI] [PubMed] [Google Scholar]
- 32.Glineur D, D’hoore W, Price J, Dorméus S, de Kerchove L, Dion R, et al. Survival benefit of multiple arterial grafting in a 25-year single-institutional experience: The importance of the third arterial graft. Eur J Cardiothorac Surg. 42:284–90. doi: 10.1093/ejcts/ezr302. [DOI] [PubMed] [Google Scholar]


