Abstract
Warfarin is the commonest anticoagulant used in today's practice; it has a very narrow therapeutics window. Under and overdosing results in various life-threatening complications. Warfarin-related nephropathy (WRN) is a rare cause of acute kidney injury (AKI) in patients on long-term anticoagulation, as a result of supratherapeutic anticoagulation. Warfarin causes AKI by inducing glomerular hemorrhage with subsequent tubular obstruction by red blood cell (RBC) casts. WRN has been associated with irreversible kidney injury and increased risk of mortality. Despite a better understanding of pathophysiology and histopathology of WRN, its preventive measures and clinical outcome are not well known. We report here the case of a 62-year-old male, who was on a long-term warfarin therapy due to chronic atrial fibrillation with a history of old ischemic stroke and dilated cardiomyopathy. He was presented with AKI and his renal biopsy was suggestive of WRN. He was managed by withholding warfarin for a few days until the therapeutic range of international normalized ratio was achieved and steroids and N-acetylcysteine (NAC) recovered. WRN is a diagnosis of exclusion; other causes of AKI must be ruled out. Renal biopsy is the gold standard for diagnosis. Patients on chronic anticoagulant therapy should be monitored periodically for the therapeutic range of anticoagulants, deterioration of renal function, and hematuria.
Keywords: Acute kidney injury, warfarin, warfarin-related nephropathy
Background
Warfarin is the commonly used anticoagulant for preventing thrombosis in a different subset of patients. Supratherapeutic dose of warfarin results in side effects like hematuria, vasculitis, interstitial nephritis, and hemorrhage.[1,2] Patients on chronic warfarin therapy are at increased risk of acute kidney injury (AKI) due to many reasons such as associated comorbidities, increased risk of hemorrhage, renal ischemia, atheroembolism, and allergic acute interstitial nephritis.[1] We are reporting here a case of warfarin-related nephropathy (WRN), biopsy-proven in a 62-year-old man with chronic atrial fibrillation on long-term warfarin therapy with a history of ischemic stroke and dilated cardiomyopathy, where warfarin cannot be withheld.
Case Report
A 62-year-old male was admitted with pain in abdomen as well as decreased appetite, vomiting, and red-colored urine. He was a known case of coronary artery disease post-percutaneous transluminal coronary angioplasty (PTCA)/stent with old ischemic stroke, chronic atrial fibrillation, dilated cardiomyopathy, and type 2 diabetes mellitus. He was kept on acenocoumarol 1 mg, aspirin 75 mg, atorvastatin 10 mg, and metoprolol 25 mg twice daily. He was on regular follow-up, and his acenocoumarol was recently increased to 1 and 2 mg alternate day to achieve the therapeutic international normalized ratio (INR). His baseline creatinine was 1.2 mg/dl. There was no history of exertional dyspnea, chest pain, palpitations, skin rash, decreased urine output, burning micturition, or pyuria. On physical examination, he was well nourished, no pallor and icterus was noticed, pulse rate was 80/min, and blood pressure was 130/80 mmHg. His serum creatinine was 5.35 mg/dl and INR was 5.4, with dysmorphic red blood cell (RBC) casts in the urine [Table 1]. A provisional diagnosis of AKI was made in the background of anticoagulation and was investigated further.
Table 1.
Laboratory investigations
| Investigations | 04/04/2018 | 03/06/2018 Warfarin dose increased | 05/07/2018 On admission | 10/07/2018 Heparin switch over | 21/07/2018 Discharge |
|---|---|---|---|---|---|
| Hb (g/dl) | 13.7 | 13.4 | 13.1 | 11.0 | 10.1 |
| TLC (cells/mm3) | 7900 | 7000 | 8600 | 7200 | 6800 |
| Platelets (lakh/mm3) | 1.25 | 1.6 | 1.79 | 1.89 | 2.1 |
| Creatinine (mg/dl) | 1.40 | 1.3 | 5.35 | 3.2 | 1.8 |
| Bilirubin (mg/dl) | 0.8 | 0.9 | 1.08 | 1.0 | 0.91 |
| Urine routine and microscopy | Albumin - nil RBC and pus cell - nil | Albumin - nil RBC and pus cell - nil | Albumin - 1+RBC - plenty and dysmorphic, RBC cast+Pus cell-6-8/hpf | Albumin - 1+RBC - 20-25/hpf Pus - 5-6/hpf | Albumin - nil RBC - 6-8/hpf Pus - 3-4/hpf |
| PT INR | 1.61 | 1.3 | 5.4 | 1.4 | 1.8 |
| ANA/DSDNA | Negative | ||||
| ANCA | Negative | ||||
| C3/C4 | Normal |
HB: Hemoglobin, TLC: Total leucocyte count, PT: Prothrombin time, INR: International normalized ratio, ANA: Anti nuclear antibody, ANCA: Antineutrophilic cytoplasmic antibodies, RBC: Red blood cells, DSDNA: Double-stranded DNA
The autoimmune markers were negative. 2D echocardiography showed global hypokinesia with ejection fraction of 35%. The ultrasonography showed bilateral normal-sized kidneys. Renal biopsy was planned in view of unexplained AKI after stopping acenocoumarol, suggestive of acute tubular necrosis with RBC casts and immunofluorescence studies were negative [Figure 1]. Oral N-acetylcysteine (NAC) 1200 mg twice daily as well as oral prednisolone 30 mg/day was started. The serum creatinine started improving with the above treatment; meanwhile, he was managed with low molecular heparin before being restarted back with warfarin, with target INR of 1.5–2. The serum creatinine and INR 3-month postdischarge were 1.3 and 1.8, respectively.
Figure 1.
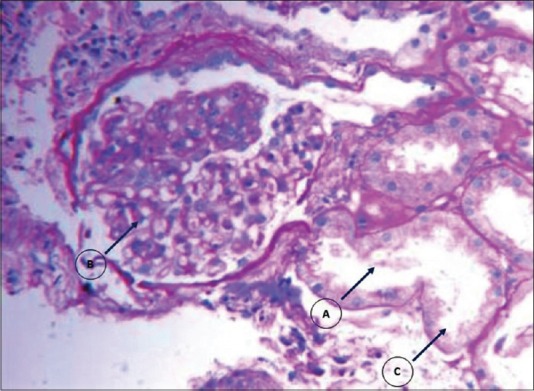
Sections stained with H and E (A). RBC casts in tubules (B). Normal glomerulus (C). Acute tubular necrosis
Discussion
Warfarin is a commonly used anticoagulant in clinical practice, used for both treatment as well as prophylaxis for prevention of arterial and venous thrombosis. WRN is defined as an increase in serum creatinine >0.3 mg/dl, occurred within 1 week of an INR >3.0 in patients on chronic warfarin therapy.[3]
Kapoor et al. in 2008 described the entity called WRN as a cause of AKI in patients with hematuria while on warfarin therapy.[2] Brodsky et al. described an association between anticoagulation with warfarin and INR (>3.0) and worsening renal function.[3] They published a series of nine patients who received renal biopsies over a 5-year period for unexplained AKI and hematuria during warfarin therapy.[4] They retrospectively analyzed the biopsies and found extensive erythrocytes in Bowmen's space and tubules, and occlusive RBC casts in distal tubules without Tamm–Horsfall protein and active glomerulonephritis.[4] WRN was a rare cause of AKI <1% of the total kidney biopsies reviewed by them.[4] Preexisting chronic kidney disease (CKD) doubles the incidence of WRN, 33% in CKD and 16.5% in non-CKD population.[5,6] Out of nine patients analyzed by them, four patients had a complete renal recovery, four became dialysis-dependent, and one developed CKD with no improvement in kidney function 2 months after biopsy.[4]
Mendonca et al., Golla et al., and Conjeevaram et al. reported cases of WRN from India; we are reporting here a similar case.[7,8,9]
Management of WRN in patients requiring long-term anticoagulation is ambiguous. Alternative to warfarin, other anticoagulants such as dabigatran, rivaroxaban, apixaban, and edoxaban are being increasingly used. However, their renal safety is not established. In the literature, dabigatran-related nephropathy was also reported.[10] The best way to prevent WRN is to avoid excessive anticoagulation, drug interactions particularly with vitamin K antagonist and antibiotics, which interferes with warfarin metabolism and increases its drug level. In our case, patient had baseline serum creatinine of 1.2 mg/dl, and after 3 months of follow-up, his creatinine was 1.3 mg/dl, that is almost complete recovery occurred.[4] Beneficial effects of steroid in WRN are not documented in studies; it may be useful due to its anti-inflammatory and antifibrotic action. Withholding of warfarin till therapeutic level attained reduces the glomerular hemorrhage and prevents further damage to renal tubules and hasten recovery of renal failure.[8]
Conclusion
AKI resulting from glomerular hemorrhage and tubular obstruction by RBC cast in patients on chronic warfarin therapy is a rare but serious complication. The supratherapeutic dose of warfarin increases the risk of AKI due to glomerular hematuria. Renal biopsy may be required for confirmation of diagnosis. Elderly patients, overanticoagulation, and underlying kidney diseases are the greatest risk factors. The treatment of biopsy-proven WRN is not clear; anticoagulants should be withdrawn and its effects should be reversed by using vitamin K. There is insufficient evidence regarding additional treatment with NAC or oral glucocorticoids. Clinical outcome in these patients is worst leading to the development of CKD and dialysis requirement. Care providers involved in the clinical care of patients on long-term anticoagulation should be aware of WRN and such patients should be monitored regularly for deterioration of renal function, change in coagulation profiles, and hematuria. Better understanding of WRN, though underdiagnosed, helps clinicians in early diagnosis, prognostication, timely therapy, and prevention from developing AKI, CKD, or dialysis dependence.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Oliver T, Ciaudelli B, Cohen DA. Anticoagulation-related nephropathy: The most common diagnosis you’ve never heard of. Am J Med. 2019 doi: 10.1016/j.amjmed.2019.02.038. pii: S0002-9343(19)30233-5. doi: 10.1016/j.amjmed. 2019.02.038. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 2.Kapoor K, Bekaii-Saab J. Warfarin-induced allergic interstitial nephritis and leucocytoclastic vasculitis. Intern Med J. 2008;38:281–3. doi: 10.1111/j.1445-5994.2008.01646.x. [DOI] [PubMed] [Google Scholar]
- 3.Brodsky S, Eikelboom J, Hebert LA. Anticoagulant-related nephropathy. J Am Soc Nephrol. 2018;29:2787–93. doi: 10.1681/ASN.2018070741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brodsky SV, Satoskar A, Chen J, Nadasdy G, Eagen JW, Hamirani M, et al. Acute kidney injury during warfarin therapy associated with obstructive tubular red blood cell casts: A report of 9 cases. Am J Kidney Dis. 2009;54:1121–6. doi: 10.1053/j.ajkd.2009.04.024. [DOI] [PubMed] [Google Scholar]
- 5.Brodsky SV, Satoskar A, Hemminger J, Rovin B, Hebert L, Ryan MS, et al. Anticoagulant-related nephropathy in kidney biopsy: A single-center report of 41 cases. Kidney Med. 2019;1:51–6. doi: 10.1016/j.xkme.2019.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.An JN, Ahn SY, Yoon C-H, Youn TJ, Han M-K, Kim S, et al. The occurrence of warfarin-related nephropathy and effects on renal and patient outcomes in Korean patients. PLoS One. 2013;8:e57661. doi: 10.1371/journal.pone.0057661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mendonca S, Gupta D, Valsan A, Tewari R. Warfarin related acute kidney injury: A case report. Indian J Nephrol. 2017;27:78–80. doi: 10.4103/0971-4065.177142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Golla A, Goli R, Nagalla VK, Kiran BV, Raju DS, Uppin MS. Warfarin-related nephropathy. Indian J Nephrol. 2018;28:378–81. doi: 10.4103/ijn.IJN_3_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conjeevaram A, Lohia P, Ravishankar GS, Vankalakunti M. Double whammy: Pigment nephropathy and warfarin-related nephropathy as aetiology for acute kidney injury in a patient with mechanical heart valves. Open Urol Nephrol J. 2019;12:41–4. [Google Scholar]
- 10.Ikeda M, Tanaka M, Shimoda S, Saita H, Nishikawa S, Shimada H, et al. Dabigatran-induced anticoagulant-related nephropathy with undiagnosed IgA nephropathy in a patient with normal baseline renal function. CEN Case Rep. 2019:1–5. doi: 10.1007/s13730-019-00410-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


