Abstract
Less than half of US adults and two-thirds of US high school students do not meet current US guidelines for physical activity. We examined which factors promoted physicians’ and medical students’ confidence in counseling patients about physical activity. We established an online exercise survey targeting attending physicians, resident and fellow physicians, and medical students to determine their current level of physical activity and confidence in counseling patients about physical activity. We compared their personal level of physical activity with the 2008 Physical Activity Guidelines of the US Department of Health and Human Services (US-DHHS). We administered a survey in 2009 and 2010 that used the short form of the International Physical Activity Questionnaire. A total of 1,949 individuals responded to the survey, of whom 1,751 (i.e., 566 attending physicians, 138 fellow physicians, 806 resident physicians, and 215 medical students) were included in this analysis. After adjusting for their BMI, the odds that physicians and medical students who met USDHHS guidelines for vigorous activity would express confidence in their ability to provide exercise counseling were more than twice that of physicians who did not meet these guidelines. Individuals who were overweight were less likely to be confident than those with normal BMI, after adjusting for whether they met the vigorous exercise guidelines. Physicians with obesity were even less likely to express confidence in regards to exercise counseling. We conclude that physicians and medical students who had a normal BMI and met vigorous USDHHS guidelines were more likely to feel confident about counseling their patients about physical activity. Our findings suggest that graduate medical school education should focus on health promotion in their students, as this will likely lead to improved health behaviors in their students’ patient populations.
Keywords: Physicians, Exercise, Medical students, Physician’s role, United States Department of Health and Human Services, Healthy people programs
Introduction
In 2008, the US Department of Health and Human Services (USDHHS) released its first national guidelines for physical activity (USDHHS, 2008). This comprehensive set of recommendations was developed as a blueprint for persons of all ages and diverse ethnic and racial groups, and with varied physical abilities. These guidelines were developed based upon research that indicates that children benefit from at least 1 h of physical activity daily, whereas adults gain substantial benefits from 150 min of moderate physical activity, or 75 min of vigorous physical activity, a week. Highly active adults, who engage in moderate intensity activity for more than 300 min or vigorous activity more than 2.5 h/week, will achieve greater health benefits such as prevention of weight gain and reduction of chronic diseases. USDHHS disseminated these guidelines to encourage people to incorporate physical activity into their daily lives.
Recent studies have indicated that <44 % of U.S. adults are aerobically active (Carlson, Fulton, Schoenborn, & Loustalot, 2010) and a nationally representative sample of adolescents suggested that only 18 % of high school students engaged in at least 60 min of physical activity per day on five or more days during the week preceding the administration of the 2009 Youth Risk Behavior Surveillance Survey. There are numerous factors that influence physical activity. In the pediatric population, several socioeconomic and behavioral characteristics have been identified that suggest that older, female, non-English speaking, metropolitan children, and those with lower socioeconomic status (SES) and neighborhood social capital, have lower physical activity levels (Singh, Kogan, Siahpush, & van Dyck, 2008). Adults’ physical activity levels appear to be influenced by additional factors such as the availability of physical activity equipment and connectivity of trails with active commuting (Wendel-Vos, Droomers, Kremers, Brug, & van Lenthe, 2007).
There are now several studies that indicate that physicians’ physical activity levels are related to the likelihood that they will counsel patients about physical activity (Bazargan, Makar, Bazargan-Hejazi, Ani, & Wolf, 2009; Frank, Carrera, Elon, & Hertzberg, 2007; Howe et al., 2010; Rogers et al., 2005; Wendel-Vos et al., 2007). Unfortunately, many physicians do not assess their patient populations’ physical activity (Wee, McCarthy, Davis, & Phillips, 1999; Winzenberg, Reid, & Shaw, 2009). Using data from a nationally representative sample of the 2001–2007 Medical Expenditure Panel, Liang, Meyerhoefer, & Wang (2012) investigated the frequency with which adolescents received advice from their physicians about physical activity and nutrition. They found that only 36 % received pertinent counseling from their pediatrician.
Evidence suggests that intensive and repeated counseling by health care professionals can increase their patients’ physical activity (Chakravarthy, Joyner, & Booth, 2002; WGACTRG, 2001; Petrella, Koval, Cunningham, & Paterson, 2003). Because of their regular patient contact, primary care physicians (PCPs) are more likely than physicians of other specialties to have an opportunity to promote their patients’ levels of physical activity. Grandes and colleagues demonstrated that family physicians were effective at increasing physical activity levels of primary care patients within a 6-month time frame (Grandes et al., 2009). Previous studies suggest that PCPs are more likely to counsel patients as to their need for physical activity than for diet or weight control (Smith et al., 2011).
We reported earlier that physicians and medical students had a higher likelihood of being physically active than the general US adult population (Stanford et al., 2012). Our findings also demonstrated that physicians who were Caucasian and those with a normal BMI had the highest levels of physical activity. In a subsequent study, we demonstrated that geographic differences in physical activity in the general US adult population are reflected in physicians and medical students as well (Stanford, Durkin, Stallworth, & Blair, 2013). In this study, we sought to determine whether physicians’ and medical students’ adherence to the 2008 USDHHS guidelines for moderate and vigorous physical activity, BMI, racial or ethnic background, or designation as a primary care physician affected their confidence in counseling patients about physical activity. We hypothesized that physicians and medical students who met the US-DHHS guidelines for moderate or vigorous physical activity, have a normal BMI, are Caucasian, and are primary care providers would have a higher likelihood of counseling patients about physical activity.
Methods
Participants and Data Collection
We established an online exercise survey with the goal of surveying a total of 2,100 individuals, including 700 attending physicians and equal numbers of resident and fellow physicians and medical students. Individuals in each group completed a 3–4 min survey. Initially, we advertised the survey through the online newsletter of the American Medical Association online (AMA® e-Voice) in order to secure an adequate sample from each of the groups studied. We also distributed fliers at the American Medical Association Annual Meeting held in June 2009. These strategies yielded approximately 450 completed surveys.
In order to increase our sample size, we used other efforts to gather survey responses. Using the website of the American College of Graduate Medical Education (ACGME), we sent individual emails to each designated institutional official for all residency and fellowship programs in the United States. In addition to the ACGME directed emails, we sent individual emails to the leaders of the Aerospace Medical Association, American Academy of Pediatrics, American College of Physicians, and the American Association of Public Health Physicians. Data collection lasted approximately eight months, from June of 2009 through January of 2010. Because we distributed the survey through numerous sources, we were unable to document the number of surveys actually received by each of our groups of interest. We provided no incentives for participation in the study, and the study was considered exempt by the institutional review board of Palmetto Health Richland Hospital in Columbia, SC.
Survey Instrument
We developed an anonymous survey to secure respondents’ self reported physical activity level, body mass index, age, gender, race/ethnicity, specialty, practice setting, the frequency with which they encourage their patients to be physically active their comfort level with providing physical activity counseling, and their assessment of whether or not they participated in an adequate amount of physical activity. We used the short form of the International Physical Activity Questionnaire (IPAQ) to quantify respondents’ level of physical activity. The IPAQ has undergone rigorous testing in numerous countries and has demonstrated adequate reliability and validity as a means to assess physical activity (Craig et al., 2003). We used the short form of the IPAQ to encourage completion of the survey. The short form of the IPAQ, in which respondents recall their physical activity over the last 7 days, has been used for national monitoring, whereas the long form is useful for more detailed assessments.
Respondents answered questions concerning their stage of training (medical student, resident physician, fellow physician, or attending physician), specialty of training, state (where they practiced or attended medical school), setting (urban, rural, suburban), practice type (academic, hospital based, non-clinical, private practice, retired), average number of work hours per week, confidence with regards to physical activity counseling (e.g. Do you feel confident about counseling patients on physical activity?), belief of the adequacy of their personal level of physical activity (e.g. Do you feel you get enough physical activity?), age, gender, racial/ethnic background, weight, height, marital status, and number of children in their household. Geographic distribution (i.e. where respondents practice or attend medical school) was determined by US Census Bureau regions (i.e. Midwest, Northeast, South, West). The survey took approximately three minutes to complete.
Data Analysis
We downloaded data from Survey Monkey® into a Microsoft Excel® spreadsheet, and then converted survey responses into variables for analysis in the R statistical program (R Development Core Team, 2011). We created a dichotomous variable from responses concerning the number of hours and days per week respondents engaged in vigorous, moderate, or walking exercise, to indicate whether or not USDHHS guidelines were met. We also compared PCPs to all other respondents. We used descriptive statistics and simple statistical tests to compare these two groups on a number of factors, including: level of training, weight class, confidence in counseling about physical activity, and whether they met the UDHHS guidelines for moderate or vigorous physical activity. We built logistic regression models using confidence about counseling patients on physical activity as the outcome and specialty (“Primary Care” or “Non-Primary Care”) with regards to level of training as the major predictor variable. We adjusted this model for whether the physician met the moderate or vigorous USDHHS guidelines for physical activity and for BMI.
Measures
Respondents had the option to select their specialty or combined specialty from 50 denoted on the AMA FREIDA website (AMA, 2013). We classified respondents as “Primary Care” if they selected the following specialties: Family Medicine, Internal Medicine, Pediatrics, Internal Medicine/Family Medicine, Internal Medicine/Pediatrics, General Preventive Medicine, and Internal Medicine/Preventive Medicine. We classified other respondents as “Non-Primary Care” or as medical students, and we further characterized physician respondents by level of training (i.e. attending, resident, or fellow).
Results
Survey respondents represented a diverse subset of the physician and medical student populations throughout the United States. A total of 1,949 persons responded to the survey, of whom 1,687 were physicians and 262 were medical students. We provide survey respondent demographics in Table 1. Survey respondents were more likely to be characterized as: (1) a primary care attending, resident, or fellow, (2) young (< age of 40), (3) Caucasian, (4) work between 50–80 h per week, (5) from the South, (6) practice in urban settings, (7) practice academic medicine, and (8) in a normal weight class.
Table 1.
Survey respondents demographics
| Number (%) | |
|---|---|
| Survey respondents demographics | |
| Medical specialty and level of training | |
| Primary care attendings | 406 (20.8) |
| Primary care residents | 427 (21.9) |
| Primary care fellows | 97 (5.0) |
| Non-primary care attendings | 207 (10.6) |
| Non-primary care residents | 505 (25.9) |
| Non-primary care fellows | 45 (2.3) |
| Medical students | 262 (13.4) |
| Age in years (missing = 1) | |
| 20–29 | 738 (37.9) |
| 30–39 | 691 (35.5) |
| 40–49 | 227 (11.7) |
| 50–59 | 202 (10.4) |
| 60–79 | 90 (4.6) |
| Race | |
| African American | 96 (4.9) |
| Asian | 283 (14.5) |
| Caucasian | 1,368 (70.1) |
| Hispanic | 60 (3.1) |
| Other | 85 (4.4) |
| Did not respond | 57 (2.9) |
| Hours worked per week | |
| < 40 | 103 (5.3) |
| 40–49 | 320 (16.4) |
| 50–59 | 433 (22.2) |
| 60–69 | 453 (23.2) |
| 70–79 | 440 (22.6) |
| > 80 | 200 (10.3) |
| Geographic region | |
| Midwest | 417 (21.4) |
| Northeast | 467 (24.0) |
| South | 731 (37.5) |
| West | 311 (16.0) |
| Did not respond | 23 (1.1) |
| Community type | |
| Rural | 55 (2.8) |
| Suburban | 536 (27.5) |
| Urban | 1,358 (69.7) |
| Practice type | |
| Academic | 1,318 (67.6) |
| Non-academic | 631 (32.4) |
| Body mass index categories | |
| Underweight | 30 (1.5) |
| Normal | 1,157 (59.4) |
| Overweight | 560 (28.7) |
| Obese | 196 (10.1) |
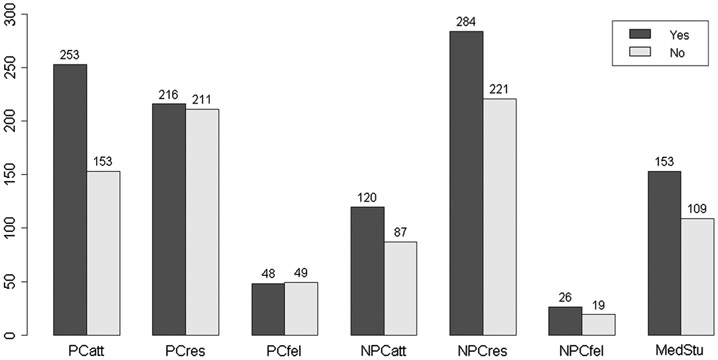
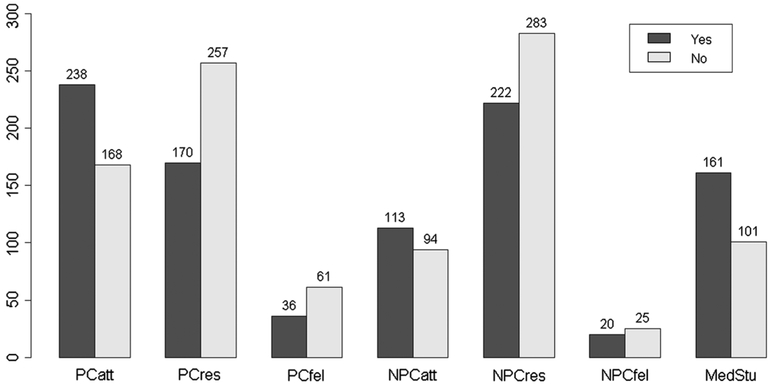
Figures 1 and 2 specify the number of respondents who met moderate and vigorous USDHHS physical activity guidelines, as disaggregated by primary care status and level of training. Figure 1 describes survey respondents who met the USDHHS for moderate physical activity by primary care status and level of training. Primary care attending physicians had the largest percentage (~62 %) of persons who met the moderate guidelines. However, primary care resident and fellows were least likely to meet USDHHS moderate guidelines, with only 51 and 49 % of survey respondents who met this criterion, respectively. Figure 2 reveals that medical students (61 %) and primary care attending physicians (58 %) were most likely to meet USDHHS vigorous physical activity guidelines.
Fig. 1.
Survey respondents who meet moderate USDHHS guidelines. PCatt Primary Care attendings, PCres Primary Care residents, PCfel Primary Care fellows, NPCatt Non-Primary Care attendings, NPCres Non-Primary Care residents, NPCfel Non-Primary Care fellows, MedStu Medical Students
Fig. 2.
Survey respondents who meet vigorous USDHHS guidelines. PCatt Primary Care attendings, PCres Primary Care residents, PCfel Primary Care fellows, NPCatt Non-Primary Care attendings, NPCres Non-Primary Care residents, NPCfel Non-Primary Care fellows, MedStu Medical Students
In Table 2, physicians’ BMI was associated with their confidence in counseling. Physicians and medical students with obesity were less likely to feel confident about physical activity counseling, despite meeting UDHSS guidelines for moderate physical activity (OR 0.484, 95 % CI 0.31, 0.76).Based on the model forTable 2, we computed odds ratios to determine the association of being a primary care physician and confidence in counseling about physical activity. The OR for counseling for non-primary care attendings compared to primary care attendings was 0.34 (95 % CI 0.20, 0.58), the OR for non-primary care residents compared to primary care residents was 0.90 (95 % CI 0.57, 1.40), and the OR for non-primary care fellows compared to primary care fellows was 1.19 (95 % CI 0.43, 3.33).
Table 2.
Counseling confidence by USDHHS moderate guidelines
| Odds ratio |
95 % Confidence interval |
|
|---|---|---|
| Meet USDHHS moderate guidelines | 1.57 | (1.17, 2.13) |
| Levels of specialty/training variable | ||
| Primary care residents | 0.70 | (0.42, 1.16) |
| Reference: primary care attendings | ||
| Primary care fellows | 0.39 | (0.20, 0.78) |
| Non-primary care attendings | 0.34 | (0.21, 0.58) |
| Non-primary care residents | 0.62 | (0.38, 1.02) |
| Non-primary care fellows | 0.47 | (0.18, 1.20) |
| Medical students | 0.51 | (0.29, 0.90) |
| Levels of body mass index variable | ||
| BMI-Obese | 0.48 | (0.31, 0.76) |
| Reference: BMI-Normal | ||
| BMI-Overweight | 0.67 | (0.48, 0.93) |
| BMI-Underweight | 2.71 | (0.36, 20.30) |
These findings suggest that there is an interaction between specialty and training with regards to physical activity counseling. To investigate this possibility, we ran logistic models without medical students and with separate specialty and training variables. The specialty by training interaction term was significant when we used the likelihood ratio test. When we computed odds ratios for the comparisons above, the values were essentially the same. Because of the interaction between specialty and level of training, a summary measure for specialty (primary care versus non primary-care) is not appropriate. We derived similar results when we completed this analysis for survey respondents’ ethnic background and whether they met USDHHS vigorous activity guidelines.
Table 3 shows physician confidence in counseling patients with regards to survey respondents who met the USDHHS vigorous guidelines for physical activity. Table 3 demonstrates that physicians who meet the vigorous USDHHS guidelines and have a normal BMI are more confident about physical activity counseling. Physicians who met USDHHS vigorous physical activity guidelines were significantly more likely than those who did not meet these guidelines to feel confident in counseling a patient about physical activity (OR 2.41, 95 % CI 1.74, 3.34).
Table 3.
Counseling confidence by USDHHS vigorous guidelines
| Odds ratio |
95 % Confidence interval |
|
|---|---|---|
| Meet USDHHS vigorous guidelines | 2.41 | (1.73, 3.34) |
| Levels of specialty/training variable | ||
| Primary care residents | 0.76 | (0.46, 1.27) |
| Reference: primary care attendings | ||
| Primary care fellows | 0.43 | (0.22, 0.86) |
| Non-primary care attendings | 0.34 | (0.20, 0.58) |
| Non-primary care residents | 0.70 | (0.42, 1.15) |
| Non-primary care fellows | 0.52 | (0.20, 1.34) |
| Medical students | 0.48 | (0.27, 0.84) |
| Levels of body mass index variable | ||
| BMI-Obese | 0.55 | (0.35, 0.87) |
| Reference: BMI-Normal | ||
| BMI-Overweight | 0.65 | (0.47, 0.91) |
| BMI-Underweight | 2.49 | (0.33, 18.73) |
Table 4 displays findings related to confidence in counseling about physical activity by race/ethnic background. We found that non-Caucasian physicians are less likely than Caucasian physicians to feel confident about physical activity counseling (OR 0.68, 95 % CI 0.49, 0.95). Weight status as denoted by BMI category also appears to play a large role in confidence about physical activity counseling, insofar as non-Caucasian physicians with obesity were less likely than their counterparts of normal weight to feel confident about physical activity counseling (OR 0.45, 95 % CI 0.28, 0.71)
Table 4.
Counseling confidence by ethnic background
| Odds ratio |
95 % Confidence interval |
|
|---|---|---|
| Race-not caucasian | 0.68 | (0.49, 0.95) |
| Reference: Caucasian | ||
| Levels of specialty/training variable | ||
| Primary care residents | 0.74 | (0.44, 1.26) |
| Reference: primary care attendings | ||
| Primary care fellows | 0.44 | (0.22, 0.91) |
| Non-primary care attendings | 0.33 | (0.20, 0.57) |
| Non-primary care residents | 0.64 | (0.38, 1.05) |
| Non-primary care fellows | 0.57 | (0.21, 1.58) |
| Medical students | 0.52 | (0.29, 0.93) |
| Levels of body mass index variable | ||
| BMI-Obese | 0.45 | (0.28, 0.71) |
| Reference: BMI-Normal | ||
| BMI-Overweight | 0.66 | (0.47, 0.94) |
| BMI-Underweight | 2.46 | (0.32, 18.43) |
Discussion
To our knowledge, our study is the first to categorize the physical activity of physicians according to the USDHHS guidelines for physical activity. Our study indicates that meeting 2008 USDHHS guidelines for moderate and vigorous activity is a strong predictor of a physician’s confidence in their ability to counsel patients about physical activity. However, physician providers that had BMIs in the overweight or obese range were less confident about physical activity counseling, even if they met current moderate or vigorous USDHHS guidelines. We presumed that primary care physicians would be more confident than other physician providers due to their higher level of patient contact and more predominant focus on preventive measures to improve overall patient health. However, we were unable to discern whether primary care attending physicians were more confident about physical activity counseling than physicians from other specialties.
Prior studies have sought to determine if patients are more likely to trust advice with regards to health related behaviors (e.g. diet, physical activity) from physicians of normal weight as compared to those with obesity (Hash, Munna, Vogel, & Bason, 2003; Puhl, Gold, Luedicke, & Depierre, 2013). In agreement with the results in our study, which demonstrates that physicians who are overweight or obese are less likely to feel confident about counseling patients about physical activity, Bleich et al. demonstrated that normal weight physicians were more likely to provide obesity related care to their patients and felt confident doing so (Bleich, Bennett, Gudzune, & Cooper, 2012). However, a more recent study by Bleich et al. found that patients who are overweight or obese were more likely to trust diet advice from overweight PCPs than normal BMI PCPs (Bleich, Gudzune, Bennett, Jarlenski, & Cooper, 2013).
Many studies conducted in the pediatric and adult population indicate that only a small percentage of patients are counseled about physical activity. However, Klein et al. report more optimistic results in their study of 8,384 adolescents. In their study, more than 80 % of all adolescents received information from their pediatrician or family physician about exercise. Their results vary significantly from other studies, especially those in the adult population. Barnes et al. report than only 32.4 % of adult patients seen in 2010 were advised by their physician to begin or continue exercise (Barnes & Schoenborn, 2012). While the percentage of counseling in the adult population is low, there is a trend towards an increase in physical activity counseling, as these investigators noted an increase of 10 percent between 2000 and 2010 in the proportion of adults who received advice to exercise.
Our study results reinforce data from previous studies that have determined that physicians who perform aerobic and strength training exercise regularly are more likely to counsel their patients on the benefits of exercise (Abramson, Stein, Schaufele, Frates, & Rogan, 2000; Bazargan et al., 2009; Frank, Breyan, & Elon, 2000a; Frank et al., 2007; Frank, Rothenberg, Lewis, & Belodoff, 2000b; Lobelo, Duperly, & Frank, 2009; Rogers et al., 2006; Smith et al., 2011). Kosteva et al. conducted a survey to ascertain physician variation in perceived barriers to their personal health (Kosteva et al., 2012). Respondents cited work schedules and family commitments as barriers to a healthy lifestyle. Lobelo et al. state that while doctors are well positioned to provide physical activity, they often do not. They conclude that medical schools need to increase the proportion of students adopting and maintaining regular PA habits to increase the rates and quality of future physical counseling delivered by doctors (Lobelo et al., 2009). Several barriers have been identified for physicians’ lack of physical activity counseling which includes: insufficient training, motivation, time, and knowledge (Abramson et al., 2000; Lobelo et al., 2009; McKenna, Naylor, & McDowell, 1998). Doctor-prescribed exercise has been shown to improve the quality of life of patients. Martin et al. performed a randomized controlled trial which determined that exercise-induced quality of life was dose dependent and independent of weight change (Martin, Church, Thompson, Earnest, & Blair, 2009).
While our study does offer evidence of the importance of a physicians’ activity level on the likelihood on their confidence in counseling patients, it does have some limitations. First, while we have a large sample size, we were unable to determine the response rate as there was no mechanism to monitor the number of persons who accessed the online survey. Secondly, as with any self-reported survey, there are likely over-estimates of activity level and inaccurate BMI levels. Finally, even though our data represent physicians from diverse geographic, training level, medical specialty, and ethnic background, we cannot be sure if this survey is a true representation of all physicians in the US.
Due to the relative paucity of physical activity in the patient population in the US, future studies should seek to discern methods that clinicians may utilize to encourage physical activity in their patient population. As previous studies have demonstrated that providers with motivational interview training feel more confident in their ability to provide guidance regarding topics such as nutrition (Cox et al., 2011), future studies might investigate whether training in motivational interviewing techniques might increase physicians’ level of confidence in regards to counseling patients about physical activity. Another potential future study would be to determine whether physicians who have a personal history of bring overweight or obese, and who now have a normal weight status, are more confident in counseling about physical activity, diet, and other health behaviors, and whether patients are more receptive to their advice than that of physicians who have always maintained a normal weight.
Conclusion
Physicians and medical students with a normal BMI, and who met moderate and vigorous USDHHS guidelines, were more likely to feel confident about counseling their patients about physical activity than those who did not meet the guidelines or those who are overweight or obese. Non-Caucasian physicians were less likely than Caucasians to feel confident about counseling patients on physical activity. Physicians should strive to meet USDHHS guidelines and aim for a normal BMI, as this will likely improve the likelihood that they can confidently counsel their patients about physical activity.
Acknowledgments
This study was supported by the Richland Memorial Hospital Research and Education Foundation.
Abbreviations
- IPAQ
International Physical Activity Questionnaire
- USDHHS
United States Department of Health and Human Services
Footnotes
Conflict of interests There are no conflicts of interest.
Contributor Information
Fatima Cody Stanford, Massachusetts General Hospital, Harvard Medical School, 50 Staniford Street, 4th Floor, Boston, MA 02114, USA.
Martin W. Durkin, Palmetto Health Richland Research Administration, Columbia, SC, USA
James Rast Stallworth, Palmetto Health Richland, University of South Carolina, School of Medicine, Columbia, SC, USA.
Caroline Keller Powell, Palmetto Health Richland, University of South Carolina, School of Medicine, Columbia, SC, USA.
Mary Beth Poston, Palmetto Health Richland, University of South Carolina, School of Medicine, Columbia, SC, USA.
Steven N. Blair, Arnold School of Public Health, University of South Carolina, Columbia, SC, USA
References
- Abramson S, Stein J, Schaufele M, Frates E, & Rogan S (2000). Personal exercise habits and counseling practices of primary care physicians: A national survey. Clinical Journal of Sport Medicine, 10(1), 40–48. [DOI] [PubMed] [Google Scholar]
- American Medical Association (AMA). (2013). FREIDA Online Retrieved October 7, 2013, from https://freida.amaassn.org/Freida/user/programSearchDispatch.do?method=viewSpec.
- Barnes PM, & Schoenborn CA (2012). Trends in adults receiving a recommendation for exercise or other physical activity from a physician or other health professional. NCHS Data Brief, 86, 1–8. [PubMed] [Google Scholar]
- Bazargan M, Makar M, Bazargan-Hejazi S, Ani C, & Wolf KE (2009). Preventive, lifestyle, and personal health behaviors among physicians. Academic Psychiatry, 33(4), 289–295. [DOI] [PubMed] [Google Scholar]
- Bleich SN, Bennett WL, Gudzune KA, & Cooper LA (2012). Impact of physician BMI on obesity care and beliefs. Obesity (Silver Spring, Md.),20(5), 999–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleich SN, Gudzune KA, Bennett WL, Jarlenski MP, & Cooper LA (2013). How does physician BMI impact patient trust and perceived stigma? Preventive Medicine, 57(2), 120–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson SA, Fulton JE, Schoenborn CA, & Loustalot F (2010). Trend and prevalence estimates based on the 2008 Physical Activity Guidelines for Americans. American Journal of Preventive Medicine, 39(4), 305–313. [DOI] [PubMed] [Google Scholar]
- Chakravarthy M, Joyner M, & Booth F (2002). An obligation for primary care physicians to prescribe physical activity to sedentary patients to reduce the risk of chronic health conditions. Mayo Clinic Proceedings, 77(2), 165–173. [DOI] [PubMed] [Google Scholar]
- Cox ME, Yancy WS Jr, Coffman CJ, Ostbye T, Tulsky JA, Alexander S, et al. (2011). Effects of counseling techniques on patients’ weight-related attitudes and behaviors in a primary care clinic. Patient Education and Counseling, 85(3), 363–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. (2003). International physical activity questionnaire: 12-country reliability and validity. Medicine and Science in Sports and Exercise, 35(8), 1381–1395. [DOI] [PubMed] [Google Scholar]
- Frank E, Breyan J, & Elon L (2000a). Physician disclosure of healthy personal behaviors improves credibility and ability to motivate. Archives of Family Medicine, 9(3), 287–290. [DOI] [PubMed] [Google Scholar]
- Frank E, Carrera JS, Elon L, & Hertzberg VS (2007). Predictors of US medical students’ prevention counseling practices. Preventive Medicine, 44(1), 76–81. [DOI] [PubMed] [Google Scholar]
- Frank E, Rothenberg R, Lewis C, & Belodoff BF (2000b). Correlates of physicians’ prevention-related practices. Findings from the Women Physicians’ Health Study. Archives of Family Medicine, 9(4), 359–367. [DOI] [PubMed] [Google Scholar]
- Grandes G, Sanchez A, Sanchez-Pinilla RO, Torcal J, Montoya I, Lizarraga K, et al. (2009). Effectiveness of physical activity advice and prescription by physicians in routine primary care: A cluster randomized trial. Archives of Internal Medicine, 169(7), 694–701. [DOI] [PubMed] [Google Scholar]
- Hash RB, Munna RK, Vogel RL, & Bason JJ (2003). Does physician weight affect perception of health advice? Preventive Medicine, 36(1), 41–44. [DOI] [PubMed] [Google Scholar]
- Howe M, Leidel A, Krishnan SM, Weber A, Rubenfire M, & Jackson EA (2010). Patient-related diet and exercise counseling: Do providers’ own lifestyle habits matter? Preventive Cardiology, 13(4), 180–185. [DOI] [PubMed] [Google Scholar]
- Kosteva AR, Salata BM, Krishnan SM, Howe M, Weber A, Rubenfire M, et al. (2012). Physician variation in perceived barriers to personal health. International Journal of General Medicine, 5, 53–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang L, Meyerhoefer C, & Wang J (2012). Obesity counseling by pediatric health professionals: An assessment using nationally representative data. Pediatrics, 130(1), 67–77. [DOI] [PubMed] [Google Scholar]
- Lobelo F, Duperly J, & Frank E (2009). Physical activity habits of doctors and medical students influence their counselling practices. British Journal of Sports Medicine, 43(2), 89–92. [DOI] [PubMed] [Google Scholar]
- Martin CK, Church TS, Thompson AM, Earnest CP, & Blair SN (2009). Exercise dose and quality of life: A-randomized controlled trial. Archives of Internal Medicine, 169(3), 269–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenna J, Naylor PJ, & McDowell N (1998). Barriers to physical activity promotion by general practitioners and practice nurses. British Journal of Sports Medicine, 32(3), 242–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrella RJ, Koval JJ, Cunningham DA, & Paterson DH (2003). Can primary care doctors prescribe exercise to improve fitness? The Step Test Exercise Prescription (STEP) project. American Journal of Preventive Medicine, 24(4), 316–322. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Gold JA, Luedicke J, & Depierre JA (2013). The effect of physicians’ body weight on patient attitudes: Implications for physician selection, trust and adherence to medical advice. International Journal of Obesity, 37(11), 1415–1421. [DOI] [PubMed] [Google Scholar]
- R Development Core Team (2011). R: A language and environment for statistical computing. R Foundation for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing. [Google Scholar]
- Rogers LQ, Gutin B, Humphries MC, Lemmon CR, Waller JL, Baranowski T, et al. (2005). A physician fitness program: Enhancing the physician as an “exercise” role model for patients. Teaching and Learning in Medicine, 17(1), 27–35. [DOI] [PubMed] [Google Scholar]
- Rogers LQ, Gutin B, Humphries MC, Lemmon CR, Waller JL, Baranowski T, et al. (2006). Evaluation of internal medicine residents as exercise role models and associations with self-reported counseling behavior, confidence, and perceived success. Teaching and Learning in Medicine, 18(3), 215–221. [DOI] [PubMed] [Google Scholar]
- Singh GK, Kogan MD, Siahpush M, & van Dyck PC (2008). Independent and joint effects of socioeconomic, behavioral, and neighborhood characteristics on physical inactivity and activity levels among US children and adolescents. Journal of Community Health, 33(4), 206–216. [DOI] [PubMed] [Google Scholar]
- Smith AW, Borowski LA, Liu B, Galuska DA, Signore C, Klabunde C, et al. (2011). U.S. primary care physicians’ diet-, physical activity-, and weight-related care of adult patients. American Journal of Preventive Medicine, 41(1), 33–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanford FC, Durkin MW, Blair SN, Powell CK, Poston MB, & Stallworth JR (2012). Determining levels of physical activity in attending physicians, resident and fellow physicians and medical students in the USA. British Journal of Sports Medicine, 46(5), 360–364. [DOI] [PubMed] [Google Scholar]
- Stanford FC, Durkin MW, Stallworth JR, & Blair SN (2013). Comparison of physical activity levels in physicians and medical students to the general adult population in the US. The Physician and Sports Medicine, 41(4), 86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Health and Human Services (USDHHS). (2008). 2008 Physical activity guidelines for Americans. Washington, DC: United States Department of Health and Human Services. [Google Scholar]
- Wee CC, McCarthy EP, Davis RB, & Phillips RS (1999). Physician counseling about exercise. Journal of the American Medical Association, 282(16), 1583–1588. [DOI] [PubMed] [Google Scholar]
- Wendel-Vos W, Droomers M, Kremers S, Brug J, & van Lenthe F (2007). Potential environmental determinants of physical activity in adults: Asystematic review. Obesity Reviews, 8(5), 425–440. [DOI] [PubMed] [Google Scholar]
- Winzenberg T, Reid P, & Shaw K (2009). Assessing physical activity in general practice: A disconnect between clinical practice and public health? British Journal of General Practice, 59(568), e359–e367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Writing Group for the Activity Counseling Trial Research Group (WGACTRG). (2001). Effects of physical activity counseling in primary care: The Activity Counseling Trial: A randomized controlled trial. Journal of the American Medical Association, 286(6), 677–687. [DOI] [PubMed] [Google Scholar]