Abstract
Statements about building walls, deportation and denying services to undocumented immigrants made during President Trump’s presidential campaign and presidency may induce fear in Latino populations and create barriers to their health care access. To assess how these statements relate to undocumented Latino immigrants’ (UDLI) and Latino legal residents/citizens’ (LLRC) perceptions of safety and their presentations for emergency care, we conducted surveys of adult patients at three county emergency departments (EDs) in California from June 2017 to December 2018. Of 1,684 patients approached, 1,337 (79.4%) agreed to participate: 34.3% UDLI, 36.9% LLRC, and 29.8% non-Latino legal residents/citizens (NLRC). The vast majority of UDLI (95%), LLRC (94%) and NLRC (85%) had heard statements about immigrants. Most UDLI (89%), LLRC (88%) and NLRC (87%) either thought that these measures were being enacted now or will be enacted in the future. Most UDLI and half of LLRC reported that these statements made them feel unsafe living in the US, 75% (95% CI 70–80%) and 51% (95% CI 47–56%), respectively. More UDLI reported that these statements made them afraid to come to the ED (24%, 95% CI 20–28%) vs LLRC (4.4%, 95% CI 3–7%) and NLRC (3.5%, 95% CI 2–6%); 55% of UDLI with this fear stated it caused them to delay coming to the ED (median delay 2–3 days). The vast majority of patients in our California EDs have heard statements during the 2016 presidential campaign or from President Trump about measures against undocumented immigrants, which have induced worry and safety concerns in both UDLI and LLRC patients. Exposure to these statements was also associated with fear of accessing emergency care in some UDLIs. Given California’s sanctuary state status, these safety concerns and ED access fears may be greater in a nationwide population of Latinos.
Introduction
The Pew Research Center estimates that approximately 8 million undocumented Latino immigrants (UDLI) lived in the United States in 2016 [1]. Given the lack of availability of other health care options including primary care, emergency departments (EDs) serve as the primary health care access point and safety net for UDLI [2–4]. Even though unfettered access to emergency care—regardless of citizenship or ability to pay—is protected by law under the Emergency Medical Treatment and Active Labor Act (EMTALA) of 1986 [5], UDLI face a number of obstacles when coming to EDs. In a 2013 study, we demonstrated that fear of discovery and deportation deters some UDLI from presenting for emergency care [6]. Since that time, US policy toward immigrants has evolved considerably, and immigration has become a heated topic across the US. Most notably, President Trump made deportation of “illegal” immigrants—particularly those from Latin America—a cornerstone of his 2016 campaign [7–9], and he has continued to promote a hardline stance toward immigrants throughout his presidency [10–12]. Although the effects of the president’s statements and policy shift on attitudes of US citizens and voters have been well documented by traditional news media surveys and polling organizations [13,14], very little is known about the impact on immigrants themselves. Threats of deportation may induce safety concerns, anxiety and other mental health problems in UDLI. Statements about denying health care (and other) services may generate misconceptions that increase their fear of emergency care access and thereby compromise the public health and safety net function of EDs.
Beyond the possible impact on UDLI, the president’s statements about immigrants may also affect the 58 million Latino legal residents/citizens (LLRC) of the US, many of whom have undocumented immigrant family and friends. Almost 6 million US citizen children live with an undocumented family member [15]. With these issues in mind, we conducted this multicenter survey study to examine whether statements about immigrants made during the 2016 presidential campaign or by President Trump affected Californian UDLI’s and LLRC’s perceptions of safety and fear of accessing emergency care. Specifically, we sought to determine 1) the proportion of UDLI and LLRC who had heard statements about deportation and denying services to undocumented immigrants from the president or during the campaign; 2) whether these statements affected their feelings of safety living in the US; and 3) whether these statements made them afraid to come to the ED for care.
Methods
Ethics statement
We obtained institutional review board (IRB) approval from the University of California of San Francisco Committee on Human Research, the Olive-View UCLA Medical Center IRB and the Highland Hospital—Alameda Health System IRB to conduct this survey study. Because the surveys were anonymous with no identifying information, a signed consent would unnecessarily add identifying information and add risk of discovery for these UDLI. The IRBs therefore recommended scripted, verbal consent. We recorded whether patients agreed to participate as a yes/no field at the initiation of the surveys.
Study design and setting
From mid-June 2017 to mid-December 2018, we conducted this survey study at three urban county hospitals in California (Zuckerberg San Francisco General Hospital [San Francisco, CA], Olive View-UCLA Medical Center [Sylmar, CA] and Highland Hospital—Alameda Health System [Oakland, CA]) with annual ED censuses of 77,000, 60,000 and 73,000 patients, respectively. At these EDs, 45.3% of visits were by patients of self-declared Latino ethnicity in 2017. We obtained IRB approval from each institution to conduct this anonymous survey study with scripted, verbal consent.
Survey development
After consultation with health literacy experts with expertise in survey design, we adapted our 2013 survey instrument to include questions assessing the following primary outcome variables: 1) whether respondents had heard statements about measures against undocumented immigrants during the presidential campaign or from President Trump; 2) whether these statements had affected their feelings of safety living in the US; and 3) whether these statements had induced fear in accessing emergency care. We pilot tested the final instrument, consisting of yes/no, multiple choice, free text response, and numerical analog questions, on ten UDLI and LLRC to ensure brevity and comprehension of questions with consistent responses. We found excellent understanding and response consistency and that the survey took less than eight minutes on average to administer (S1 Fig and S2 Fig).
Participants and enrollment
Using a convenience sampling method consisting of enrollment when study personnel were available (typically four- to six-hour time blocks on weekdays), we screened ED tracking boards for eligible adult patients. We excluded patients with any of the following characteristics: 1) trauma; 2) transfer from another facility; 3) inability to participate in an interview because of intoxication, altered mental status or critical illness; 4) incarceration; and 5) on psychiatric hold. In order to enroll similar numbers of our three groups (UDLI, LLRC and non-Latino legal residents/citizens [NLRC]), we examined our central database tally of the participant group assignments monthly. When the total number of participants in one group fell to 20% lower than the other groups, we shifted toward approaching more patients in that group. We excluded patients after interviews if they were vacationing or were non-Latino undocumented immigrants.
Survey administration
Physicians, students and other research personnel, most of whom were fluent Spanish speakers, received orientation sessions and shadowed the principal investigators during initial surveys to ensure standard survey technique. After scripted verbal consent, these study personnel read survey questions to participants directly from data collection forms in their preferred language (fluent Spanish speakers only for Spanish-speaking participants) in private ED areas. Without recording any numbers or identifying information, we reviewed ED registration records to determine whether respondents had a social security number (SS#). After the surveys, interviewers assured subjects that EDs maintain confidentiality regarding immigration status and provided information sheets about local resources for primary medical care and social services support.
Data management and analysis
Using double checks on entry, we entered data into REDCap hosted by the University of California, San Francisco [16]. We used STATA v 15.1 (StataCorp, College Station, TX) for analyses, summarizing patient characteristics as raw counts and frequency percent and key survey questions as percentages (proportions) with 95% confidence intervals (CIs). Non-responses to individual questions were not included in the denominators of these proportions.
We categorized participants after the surveys into UDLI, LLRC, and NLRC groups by the following direct questions: Do you identify as being of Latino origin? Are you a legal resident/citizen of the United States? Our three primary outcomes were 1) the proportions of UDLI, LLRC and NLRC who had heard statements about measures against immigrants from the president or during the campaign; 2) whether these statements made them worry or feel unsafe living in the US; and 3) whether these statements made them afraid to come to the ED for care.
To assess differences between groups, we compared 95% CIs around differences in proportions. We calculated odds ratios (ORs) to describe the association of patient characteristics (age, sex, identification as Latino, legal US resident status, having health insurance, having a doctor/clinic for regular care, having housing, and belief that the statements about immigrants are being/will be enacted) with the primary outcomes of feeling unsafe in the US and being afraid to come to the ED. Additionally, we estimated adjusted odds ratios (aORs) of characteristics that showed OR significance, while adjusting for interactions, using logistic regression to examine which factors continued to demonstrate independent association with these two outcomes. To have no more than a 5% CI around the point estimates for prevalence of safety concerns and fear of coming to the ED, we calculated a priori that we would need to enroll at least 384 patients in each group.
We conducted two secondary analyses of the two primary outcomes of feeling unsafe in the US and being afraid to come to the ED on the UDLI sub-group of patients. We compared 1) recent immigrants (< 5 years) versus non-recent immigrants (> 5 years), and 2) immigrants surveyed in the first 12 months (late June 2017 –June 2018) versus the last six months (July–December 2018) of the study time period.
Results
Of 1,684 patients approached, 1,337 (79.4%) agreed to participate. We excluded 16 patients because they were non-Latino undocumented immigrants and three because they were just visiting the US. Of the remaining 1,318 patients, 452 (34.3%) were UDLI, 473 (35.9%) LLRC, and 393 (29.8%) NLRC. Enrollment and categorization of participants at the three sites was (501: 34% UDLI, 38% LLRC and 28% NLRC); (418: 36% UDLI, 37% LLRC and 27% NLRC); and (399: 33% UDLI, 32% LLRC and 35% NLRC).
On review of ED registration records, 15% of UDLI, 89% of LLRC and 93% of NLRC had SS#s. Compared to LLRC and NLRC, UDLI were younger, more often female, less likely to have health insurance, and less likely to have primary care. Most UDLI (93%) had seen a doctor in the US previously. Spanish was the primary language of 97% of UDLI with 78% of them reporting little to no English proficiency; 22% stated that they were brought to the US as children. UDLI without primary care were more likely to get their usual medical care in an ED (Table 1).
Table 1. Patient characteristics sorted according to study groups.
| UDLI | LLRC | NLRC | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Total Number | 452 (34) | 473 (36) | 393 (30) |
| Male | 200 (44) | 260 (55) | 221 (56) |
| Median age in years (IQR) | 40 (32, 51) | 45 (28, 58) | 48 (33, 60) |
| Primary Language* | |||
| English | 17 (4) | 201 (42) | 349 (89) |
| Spanish | 437 (97) | 308 (65) | 3 (1) |
| Other | 6 (1) | 7 (1) | 60 (15) |
| English Proficiency | |||
| Not at all | 104 (23) | 27 (6) | 2 (0.5) |
| A little | 247 (55) | 117 (25) | 10 (3) |
| Most of it | 68 (15) | 81 (17) | 33 (8) |
| Completely | 38 (8) | 249 (53) | 349 (89) |
| Have Health Insurance | 315 (70) | 384 (81) | 332 (84) |
| Private | 15 (3) | 41 (9) | 43 (11) |
| Medicare/Medi-Cal | 177 (39) | 328 (69) | 285 (73) |
| Healthy SF/My Health LA/HealthPAC** | 133 (29) | 39 (8) | 17 (4) |
| Have Housing | 437 (97) | 448 (95) | 346 (88) |
| Have PCP | 271 (60) | 312 (66) | 253 (64) |
| If no PCP, where do you get care? | |||
| Clinic | 24 (17) | 41 (30) | 33 (31) |
| Emergency Department | 117 (83) | 96 (70) | 75 (69) |
PCP–primary care provider; IQR–interquartile range; UDLI–Undocumented Latino Immigrant; LLRC–Latino legal resident/citizen; NLRC–Non-Latino resident/citizen.
*Patients could declare more than one primary language
**Healthy SF, My Health LA and HealthPAC are Department of Public Health programs in San Francisco, Los Angeles and Alameda counties that provide free or affordable health services to those who are not eligible for public insurance (Medi-Cal and Medicare) and are below a certain income threshold.
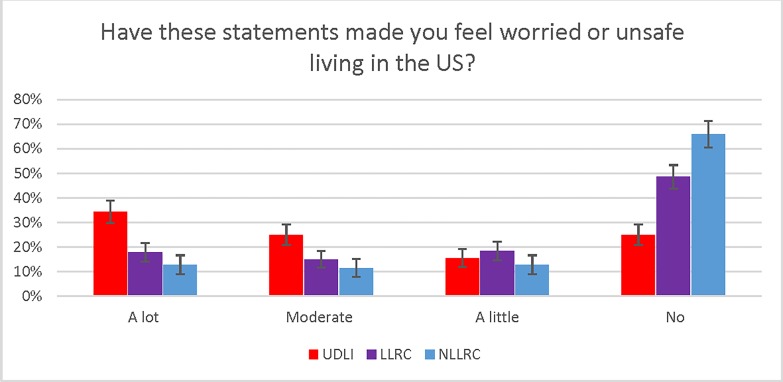
Nearly all UDLI (99.3%), LLRC (99.8%), and NLRC (97.4%) knew the name of the US president (President Trump). Greater percentages of UDLI (95%, 95% CI 92–96%) and LLRC (94%, 95% CI 91–96%) had heard statements about measures against immigrants than NLRC (85%, 95% CI 81–88%). High percentages of UDLI respondents had heard that President Trump wants to deport immigrants (92%), deny immigrants services (87%) and prevent immigrants from getting health care in the US (79%). Of those who had heard these statements, most UDLI (89%), LLRC (88%) and NLRC (87%) thought that these measures were being enacted now or will be enacted in the future. When asked whether these statements made them feel worried or unsafe living in the US, most UDLI (75%; 95% CI 71–79%) and approximately half of LLRC (51%; 95% CI 47–56%) responded Yes “a little”, “somewhat”, or “a lot” (Table 2 and Fig 1).
Table 2. Responses to key questions sorted according to study groups.
| UDLI | LLRC | NLRC | |
|---|---|---|---|
| % (95% CI) | % (95% CI) | % (95% CI) | |
| Believe that providers treat US citizens different than non-US citizens? | |||
| Yes | 11 (8–14) | 11 (8–14) | 12 (9–16) |
| No | 81 (77–85) | 75 (7–78) | 60 (55–65) |
| Unsure | 8 (6–11) | 15 (12–18) | 30 (26–35) |
| Believe that hospital staff report illegal immigrants to the authorities? | |||
| Yes | 4 (2–6) | 4 (3–7) | 7 (5–10) |
| No | 81 (77–84) | 76 (71–79) | 60 (55–65) |
| Unsure | 15 (12–19) | 20 (17–24) | 33 (28–38) |
| Did anyone ask about your citizenship? | |||
| Yes | 5 (3–8) | 7 (5–10) | 6 (4–9) |
| No | 93 (90–95) | 81 (77–84) | 89 (85–92) |
| Unsure | 2 (1–4) | 2 (1–4) | 6 (4–9) |
| Do you know someone (friends or family) that did not come to the ED out of fear of being discovered as undocumented? | |||
| Yes | 24 (21–28) | 26 (22–30) | 15 (11–19) |
| Have you heard any of these statements? The president wants to: | |||
| Build a wall | 92 (89–95) | 92 (89–94) | 77 (73–81) |
| Deport immigrants | 92 (89–95) | 91 (88–94) | 77 (72–81) |
| Deny services | 87 (83–90) | 80 (76–83) | 63 (58–68) |
| Prevent immigrant from working | 86 (83–89) | 81 (77–85) | 59 (53–63) |
| Prevent immigrants from getting health care | 79 (74–82) | 73 (68–76) | 53 (48–58) |
| Do you believe any of these are currently occurring or will happen? | |||
| No, not now and will never happen | 11 (8–14) | 12 (10–16) | 13 (1–17) |
| Not right now, but will happen in the future | 31 (26–35) | 29 (25–33) | 19 (16–24) |
| Some are occurring now | 43 (38–48) | 41 (37–46) | 33 (28–38) |
| All are occurring now | 10 (7–13) | 12 (10–16) | 8 (6–11) |
| Have these statements made you feel worried or unsafe living in the US? | |||
| No, they have not affected me at all | 25 (21–30) | 49 (44–53) | 66 (60–71) |
| Yes, little worried or unsafe | 16 (12–20) | 18 (15–22) | 13 (9–17) |
| Yes, somewhat (moderate) worried or unsafe | 25 (21–30) | 15 (12–19) | 12 (8–16) |
| Yes, they've affected me a lot | 34 (30–40) | 18 (14–19) | 13 (9–17) |
| Did any of these statements make you afraid to come to the ED? | |||
| No, not at all | 76 (72–81) | 96 (93–97) | 96 (94–98) |
| Yes, a little | 11 (8–14) | 2 (1–4) | 1 (0–3) |
| Yes, a moderate amount | 8 (6–11) | 2 (1–3) | 1 (0–3) |
| Yes, a lot | 5 (3–7) | 1 (0–2) | 1 (0–3) |
UDLI–Undocumented Latino immigrant; LLRC–Latino legal resident/citizen; NLRC–Non-Latino resident/citizen; CI–confidence interval
Fig 1. Perceived impact of the president’s statements about immigrants on feelings of safety.
UDLI–Undocumented Latino immigrant; LLRC–Latino legal resident/citizen; NLRC–Non-Latino resident/citizen; US–United States. Error bars represent 95% confidence intervals.
When asked whether these statements about immigrants made them afraid to come to the ED, a greater percentage of UDLI as compared to LLRC and NLRC reported Yes “a little”, “a moderate amount”, or “a lot” (UDLI 24%, 95% CI 20–28%; LLRC 4%, 95% CI 3–7%; and NLRC 4%, 95% CI 2–6%). Of the UDLI who had this fear, 55% stated that they delayed coming to the ED (median delay of 2–3 days). Similar percentages of UDLI (24%, 95% CI 21–28%) and LLRC (26%, 95% CI 22–30%) reported that they had friends or family members who had not come to the ED because of fear of discovery, greater than the 15% (95% CI 11–19%) of NLRC who reported having friends/family who had not come to the ED (Table 2).
Only undocumented status (aOR 2.8; 95% CI 2.1–3.9), belief that the president’s immigrant statements are being/will be enacted (aOR 2.4; 95% CI 1.6–3.5), and identification as Latino (aOR 1.5; 95% CI 1.1–2.1) were independently associated with feeling unsafe in the US. Only undocumented status (aOR 7.4; 95% CI 4.4–13.3) and belief that the president’s immigrant statements are being/will be enacted (aOR 2.1; 95% CI 1.0 to 4.8) were independently associated with fear of coming to the ED (Table 3).
Table 3. Association of characteristics with primary outcomes of feeling unsafe in the US and feeling afraid to come to the ED because of the president’s anti-immigrant statements: ORs and aORs.
| Characteristic | Feel unsafe living in US because of statements OR (95% CI) |
Afraid to come to ED because of statements OR (95% CI) |
|---|---|---|
| Age (unit = 10 years) | 0.9 (0.8–0.9)* | 0.9 (0.8–1.1) |
| Female | 2.3 (1.8–2.9)* | 1.2 (0.8–1.7) |
| Identify as Latino | 2.6 (2.0–3.5)* | 4.7 (2.5–10.2)* |
| Non-insured | 1.1 (0.8–1.5) | 1.4 (0.9–2.2) |
| No regular clinic or doctor for care | 0.9 (0.7–1.2) | 1.4 (0.9–2.0) |
| Not housed | 0.6 (0.4–1.1) | 1.5 (0.7–2.9) |
| Not legal US resident | 3.7 (2.8–4.9)* | 8.2 (5.2–13.3)* |
| Believe actions in anti-immigrant statements are being done or will be done | 2.5 (1.8–3.6)* | 2.3 (1.1–5.3)* |
| Characteristic | aOR (95% CI) | aOR (95% CI) |
| Age (unit = 10 years) | 0.9 (0.8–1.0) | 1.0 (0.9–1.2) |
| Female | 2.1 (1.6–2.8)* | 0.9 (0.6–1.4) |
| Identify as Latino | 1.5 (1.1–2.1)* | 1.2 (0.5–3.0) |
| Not legal US resident | 2.8 (2.1–3.9)* | 7.4 (4.4–13.3)* |
| Believe actions in anti-immigrant statements are being done or will be done | 2.4 (1.6–3.5)* | 2.1 (1.0–4.8)* |
OR = odds ratio; aOR = adjusted odds ratio; CI = confidence interval; US = United States; ED = emergency department
*significant at p < .05
In terms of the secondary analyses of the perceived effects of these statements, UDLI living in the US for > 5 years had similar prevalence of safety concerns as UDLI who had recently immigrated (82% vs 74% [difference 8%, 95% CI -5 to 18%]) and similar rates of fear of coming to the ED (23% vs 32% [difference -10%, 95% CI -23 to 2%]). We found a higher rate of safety concerns in the last six months of sampling (July–December 2018) as compared to the first year (83.1% vs 72.8% [difference 10.3%, 95% CI 0 to 19%]), but similar rates of fear coming to the ED (23.3% vs 24.2% [difference -0.9%, 95% CI -10 to 10%]).
Discussion
Excluded from the Affordability Care Act (ACA) and with limited options for regular health care, UDLI in the US report worse health and less health care utilization compared to US-born Latinos [17–19]. Given that the ED serves as the sole health care access point for many UDLI, efforts to improve UDLI health must begin with minimization of barriers (both true and perceived) to ED utilization. In this study we sought to assess whether statements about immigrants made during the 2016 presidential campaign or by President Trump have generated another barrier to UDLI access to EDs. We found that the vast majority of UDLI had heard statements about President Trump’s intended measures against undocumented immigrants and that most believed that these measures are being or will be enacted. According to responses in this survey, UDLIs reported that these statements have affected their feelings of safety living in the US and have induced fear of accessing the ED for health care.
Our UDLI population was not a medically naïve group—the vast majority had seen a doctor in the US previously and were aware that health care workers do not report patients to immigration authorities; few believed that doctors and nurses treat them differently. That nearly a quarter of them still had fear in coming to the ED attests to the potential power and threat of statements about deportation and denial of services coming from the president or being used during a presidential campaign. Notably, rates of safety concerns and fear of accessing the ED were similar in recent and non-recent immigrants, indicating a pervasiveness that does not appear to wane over time living in the US. The reasons for a higher prevalence of safety concerns in the latter part of the study are unclear, but it is possible that it arises from later statements and policy changes by the presidential administration, including narrowing asylum eligibility and changing the definition of “Public Charge,” such that immigration officials may consider a much broader range of public benefits when determining who is likely to become dependent on government benefits. These changes have the potential to lead to the disenrollment of millions of children from benefits that support their health and nutrition [20–22].
Beyond effects on the UDLI population, we have additionally demonstrated that the statements made by the president or during the campaign also correlate with perceptions held by LLRC, half of whom replied that these statements made them feel unsafe living in the US. Self-identification as Latino was independently associated with this feeling of being unsafe. These findings about safety are in line with reports that hate crimes against Latinos in California increased over 50% from 2016 to 2017 [23]. Although our NLRC enrollment group was intended to serve primarily as a control, a third of these patients replied that they had personal safety concerns arising from these statements about immigrants as well.
Undocumented immigrant populations in the US are a difficult group to study, and it is not surprising that little original research has been published regarding their barriers to accessing health care. Beyond the standard barriers of language difficulties and lack of financial resources, investigators have more recently reported that spikes in immigration enforcement were associated with decreased Medicaid enrollment [24,25]. This “chilling effect” on enrollment extends beyond UDLIs to their legal resident family members, as immigration raids have been linked to worse self-reported health and increased stress levels among legal residents of Latino communities [25,26].
Outside of efforts in the political arena, what can be done to reduce undocumented immigrants’ fear of accessing emergency care? The most obvious measure is to spread the message that US law guarantees everyone—regardless of citizenship—the right to emergency care. Many EDs promote Know Your Rights education initiatives with multiple language signs in waiting rooms and verbal reassurance at triage [27,28], but these messages may not reach those in greatest need of this information—immigrants who completely avoid coming to the hospital. Other measures to engage this hard-to-reach group include public awareness campaigns on Spanish media and forging community alliances through churches and neighborhood immigrant centers. Given that most UDLI knew that hospital staff do not report immigrants, merely spreading this message of safety in the ED may be insufficient. Addressing health disparities requires consideration of traditional social determinants of health (housing instability, food insecurity and limited English proficiency), as well as exploration of how other newly recognized factors, such as “racialized legal status,” may disproportionately affect their health [29–32].
Beyond the ED, tempering the rise in personal safety concerns in Latino populations may be even more difficult. A statement released by the Los Angeles Police Department in early 2018 showed substantial drops in the reporting of sexual assaults and domestic violence by the Hispanic community after the president’s inauguration [33]. According to a number of media reports, the mass shooting that targeted Latinos in El Paso, Texas, in August 2019 may have made UDLIs apprehensive about their personal safety and reluctant to report crimes because of their immigration status [34,35]. Similar to the message that everyone can safely receive care in the ED, initiatives assuring safety when seeking police assistance should also be considered. Our finding that LLRC and NLRC also had safety concerns rooted in the president’s statements about immigrants may signal the potential mental health benefit of such interventions for the broader US citizen population as well.
Limitations
Although we optimized survey content with health literacy experts and pilot tested our survey instrument to ensure comprehension and response consistency, we did not specifically address other elements of instrument validity. Confidentiality constraints limited formal review of citizenship and use of self-reports for categorization of citizenship status may have led to misclassification of undocumented immigrants who may have been afraid to respond candidly. However, on review of ED registration records, we found similar rates of social security numbers in the LLRC and NLRC groups and low rates of social security numbers in UDLI, bolstering the face validity of this method of participant classification. Furthermore, self-report is the generally accepted standard for determination of citizenship in studies of this vulnerable population [26,32]. Our convenience sampling during weekday hours may have introduced spectrum bias.
Perhaps the greatest limitation of our work is that we surveyed patients in only one state and in communities that are generally considered to be safe for undocumented immigrants; UDLI in other states or communities may have higher or lower levels of fear. Similarly, because we only examined Latinos, our findings may not generalize to other immigrant populations. Another major limitation is that we only surveyed immigrants who actually came to the ED for health care—a quarter of UDLI and LLRC stated they had friends or family members who had not come to the ED because of fear, and we were unable to interview this group. These limitations all likely lead to an underestimation of the true levels of UDLI safety concerns and fear of accessing emergency care, and our study therefore likely provides lower-bound point estimates of what would be seen in a national sample of undocumented immigrants.
Finally, we must acknowledge that this topic is emotionally charged and that simply asking these questions may have paradoxically triggered fear in respondents. Social desirability may also have induced patients to answer in ways that they thought we wanted them to respond [36]. We attempted to mitigate these effects by training our interviewers to read the questions directly off the survey template in a standardized fashion with neutral tones and without insertion of other leading statements. Although we included IRB-mandated language in the scripted consent assuring patients that the study would not affect their care and that they would receive information about health care access, we avoided other language that would induce positive responses to our primary outcome questions. To diminish primacy bias (the tendency for respondents to choose the first option in surveys) toward finding greater effect, we placed neutral responses, e.g. “No, these statements have not affected me at all”, as the first choice in all of our queries. Our tiered decreasing rates of safety concerns from highest in UDLI to lowest in NLRC (as evident in Fig 1) logically support the validity of our central finding that the two Latino groups truly have heightened fear.
Conclusions
The vast majority of patients in our California EDs have heard statements about deporting and denying services to undocumented immigrants from President Trump or during the 2016 presidential campaign. Latino patients (both UDLI and LLRC) responded that such statements made them feel unsafe living in the US. Some UDLI also indicated that these statements made them afraid to come to the ED and thus represent a potential psychological barrier to emergency care access.
Supporting information
(DOCX)
(DOCX)
Data Availability
All relevant data are within the manuscript and its Supporting Information files. Our data will be deposited at the UCSF Library's open access repository Dash: https://datashare.ucsf.edu/stash. Per university rules, we cannot provide the full link until we receive notice that the manuscript is accepted for publication.
Funding Statement
This study was supported in part by a grant (RMR) from the University of California Institute for Mexico and the United States (UC MEXUS- https://ucmexus.ucr.edu/). The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The contents of the article are solely the responsibility of the authors and do not necessarily represent the official views of the sponsors.
References
- 1.Passel JS, Cohn D. U.S. Unauthorized Immigrant Total Dips to Lowest Level in a Decade. Pew Hispanic Center; http://www.pewhispanic.org/2018/11/27/u-s-unauthorized-immigrant-total-dips-to-lowest-level-in-a-decade/. Published November 27, 2018. Accessed January 14, 2019. [Google Scholar]
- 2.Tarraf W, Vega W, Gonzalez HM. Emergency Department Services Use among Immigrant and Non-Immigrant Groups in the United States. J Immigr Minor Health. 2014;16(4):595–606. 10.1007/s10903-013-9802-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gusmano MK. Lack of Coverage for Undocumented Patients Puts Pressure on the Health Care Safety Net. https://www.rwjf.org/en/blog/2014/09/lack_of_coveragefor.html. Robert Wood Johnson Foundation Culture of Health Blog. Published September 26, 2014. Accessed January 14, 2019.
- 4.Derose KP, Bahney BW, Lurie N, Escarce JJ. Review: immigrants and health care access, quality, and cost. Med Care Res Rev. 2009;66(4):355–408. 10.1177/1077558708330425 [DOI] [PubMed] [Google Scholar]
- 5.Zibulewsky J. The Emergency Medical Treatment and Active Labor Act (EMTALA): What it is and what it means for physicians. Proc (Bayl Univ Med Cent). 2001. October; 14(4):339–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maldonado CZ, Rodriguez RM, Torres JR, Flores YS, Lovato LM. Fear of discovery among Latino immigrants presenting to the emergency department. Acad Emerg Med. 2013. February;20(2):155–61. 10.1111/acem.12079 [DOI] [PubMed] [Google Scholar]
- 7.Gamboa S. Donald Trump Announces Presidential Bid By Trashing Mexico, Mexicans. NBC News. https://www.nbcnews.com/news/latino/donald-trump-announces-presidential-bid-trashing-mexico-mexicans-n376521. Published June 16, 2015. Updated June 16, 2015. Accessed January 14, 2019.
- 8.Desjardins L. What is Donald Trump’s 10-Point immigration plan? PBS NewsHour. https://www.pbs.org/newshour/politics/donald-trumps-10-point-immigration-plan. Published September 1, 2016. Accessed January 14, 2019.
- 9.Osnos E. President Trump’s First Term. The New Yorker. https://www.newyorker.com/magazine/2016/09/26/president-trumps-first-term. Published September 26, 2016. Accessed January 14, 2019.
- 10.Trump DJ. Executive Order 13768: Enhancing Public Safety in the Interior of the United States. The White House, Office of the Press Secretary; https://www.whitehouse.gov/presidential-actions/executive-order-enhancing-public-safety-interior-united-states/. Published January 25, 2017. Accessed January 14, 2019. [Google Scholar]
- 11.Gamboa S, Soto VD, Nuño SA. Trump Ends Convention as He Started Campaign: Linking Immigrants to Crime. NBC News. https://www.nbcnews.com/storyline/2016-conventions/trump-ends-convention-he-started-campaign-linking-immigrants-crime-n614551. Published July 21, 2016. Updated July 22, 2016. Accessed January 14, 2019.
- 12.Bialik K. ICE Arrests went up in 2017, with biggest increases in Florida, northern Texas, Oklahoma. Pew Research Center; http://www.pewresearch.org/fact-tank/2018/02/08/ice-arrests-went-up-in-2017-with-biggest-increases-in-florida-northern-texas-oklahoma/. Published February 8, 2018. Accessed January 14, 2019. [Google Scholar]
- 13.McCarthy J. Immigration Up Sharply as Most Important U.S. Problem. Gallup; https://news.gallup.com/poll/244925/immigration-sharply-important-problem.aspx. Published November 20, 2018. Accessed January 14, 2019. [Google Scholar]
- 14.Tinney D, Quinlan S. Explaining the Trump Victory: Populist Sentiments and the 2016 Presidential Election. Comparative Study of Electoral Systems (CSES). Published May 3, 2017. Accessed January 14, 2019. [Google Scholar]
- 15.American Immigration Council. US Citizen Children Impacted by Immigration Enforcement. https://www.americanimmigrationcouncil.org/research/us-citizen-children-impacted-immigration-enforcement. Published May 23, 2018. Accessed January 31, 2019.
- 16.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009. April;42(2):377–81. Epub 2008 Sep 30. 10.1016/j.jbi.2008.08.010 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ortega AN, McKenna RM, Kemmick Pintor J, Langellier BA, Roby DH, Pourat N, et al. Health Care Access and Physical and Behavioral Health Among Undocumented Latinos in California. Med Care. 2018. November;56(11):919–26. 10.1097/MLR.0000000000000985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hacker K, Anies M, Folb BL, Zallman L. Barriers to health care for undocumented immigrants: a literature review. Risk Manag Healthc Policy 2015;8:175–83. 10.2147/RMHP.S70173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sommers BD. Stuck between Health and Immigration Reform—Care for Undocumented Immigrants. New Engl J Med 2013;369:593–5. 10.1056/NEJMp1306636 [DOI] [PubMed] [Google Scholar]
- 20.Zallman L, Finnegan KE, Himmelstein DU, Touw S, Woolhandler S. Implications of Changing Public Charge Immigration Rules for Children Who Need Medical Care. JAMA Pediatr [Internet]. 2019. July 1 [cited 2019 Oct 10];173(9):e191744 10.1001/jamapediatrics.2019.1744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Katz MH, Chokshi DA. The "Public Charge" Proposal and Public Health: Implications for Patients and Clinicians. JAMA 2018;320:2075–6. 10.1001/jama.2018.16391 [DOI] [PubMed] [Google Scholar]
- 22.Inadmissibility on Public Charge Grounds: A Proposed Rule by the Homeland Security Department on 10/10/2018. 83 FR 51114. https://www.federalregister.gov/documents/2018/10/10/2018-21106/inadmissibility-on-public-charge-grounds
- 23.State of California Department of Justice, Office of the Attorney General. Hate Crime in California 2017. OpenJustice. https://openjustice.doj.ca.gov/resources/publications. Published July 9, 2018. Accessed January 29, 2019.
- 24.Watson T. Inside the Refrigerator: Immigration Enforcement and Chilling Effects in Medicaid Participation. Am Econ J: Economic Policy 2014;6:313–38. [Google Scholar]
- 25.Batalova J, Fix M, Greenberg M. Chilling Effects: The Expected Public Charge Rule and Its Impact on Legal Immigrant Families’ Public Benefits Use. https://www.migrationpolicy.org/research/chilling-effects-expected-public-charge-rule-impact-legal-immigrant-families. Published June 2018. Accessed January 31, 2019
- 26.Lopez WD, Kruger DJ, Delva J, Llanes M, Ledón C, Waller A, et al. Health Implications of an Immigration Raid: Findings from a Latino Community in the Midwestern United States. J Immigr Minor Health 2017;19:702–8. 10.1007/s10903-016-0390-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Immigration Law Center. Rights: Immigration Enforcement at Health Care Facilities [Internet]. National Immigration Law Center; 2019. [cited 27 August 2019]. Available from:https://www.nilc.org/get-involved/community-education-resources/know-your-rights/health-provider-patient-rights-imm-enf/ [Google Scholar]
- 28.LA County Office of Immigrant Affairs. Your Rights [Internet]. LA County Office of Immigrant Affairs; 2019. [cited 27 August 2019]. Available from: http://oia.lacounty.gov/know-your-rights/ [Google Scholar]
- 29.Asad AL, Clair M. Racialized legal status as a social determinant of health. Soc Sci Med 2018;199:19–28. 10.1016/j.socscimed.2017.03.010 [DOI] [PubMed] [Google Scholar]
- 30.Samra S, Taira BR, Pinheiro E, Trotzky-Sirr R, Schneberk T. Undocumented Patients in the Emergency Department: Challenges and Opportunities. West J Emerg Med. 2019. August 12 10.5811/westjem.2019.7.41489 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Castaneda H, Holmes SM, Madrigal DS, Young ME, Beyeler N, Quesada J. Immigration as a social determinant of health. Annu Rev Public Health 2015;36:375–92. 10.1146/annurev-publhealth-032013-182419 [DOI] [PubMed] [Google Scholar]
- 32.Cavazos-Rehg PA, Zayas LH, Spitznagel EL. Legal status, emotional well-being and subjective health status of Latino immigrants. J Natl Med Assoc. 2007;99:1126–31. [PMC free article] [PubMed] [Google Scholar]
- 33.Statement on Sexual Assault and Domestic Violence Reporting in Immigrant Communities NR18122ra [Internet]. Los Angeles (CA): Los Angeles Police Department; 2019. April 27 [cited 2019 Oct 10]. Available from: http://www.lapdonline.org/central_news/news_view/63831 [Google Scholar]
- 34.Fetters A. When Fear of Deportation Keeps Families From Help After a Shooting [Internet]. The Atlantic; 2019. [updated 2019 Aug 4; cited 27 Aug 2019]. Available from: https://amp.theatlantic.com/amp/article/595441/ [Google Scholar]
- 35.Náñez DM, Moroti K, Warnock S, Hawthorne T, Alvarado M, Yasukawa M, et al. After El Paso, Latinos across America voice a new kind of fear [Internet]. Mclean (VA): USA Today Network, azcentral; 2019. August 16 [updated 2019 Aug 17; cited 2019 Aug 26]. Available from: https://www.azcentral.com/in-depth/news/nation/2019/08/16/el-paso-texas-mass-shooting-latino-hispanic-reaction-fears/1992555001/. [Google Scholar]
- 36.Kimberlin CL, Winterstein AG. Validity and reliability of measurement instruments used in research. Am J Health Syst Pharm. 2008;65:2276–84. 10.2146/ajhp070364 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files. Our data will be deposited at the UCSF Library's open access repository Dash: https://datashare.ucsf.edu/stash. Per university rules, we cannot provide the full link until we receive notice that the manuscript is accepted for publication.