Inflammation is incriminated in the pathogenesis of atherosclerosis.1 The Canakinumab Anti-inflammatory Thrombosis Outcomes Study (CANTOS) established inflammation as a therapeutic target in atherosclerosis,2 especially, in patients with residual inflammatory risk.
Psoriasis is a chronic inflammatory skin disease associated with increased risk for both clinical3 and subclinical coronary artery disease.4 Observational studies have suggested decreased risk for myocardial infarction over 8 years in psoriasis patients treated with biologic therapy.5
In a recent article,6 using 1-year follow-up visits in a large ongoing cohort study of psoriasis patients, coronary computed tomography angiography was performed at baseline and at 1 year. The authors asked whether treating psoriasis with biologic therapy compared to not taking biologic therapy was associated with reduction in coronary plaque burden at 1-year follow-up.
First, patients treated with biologic agents had significant reductions in psoriasis skin disease severity and high-sensitivity C-reactive protein, which were not seen in those treated with non-biologic therapy. Furthermore, patients treated with biologic agents had improvement in total and non-calcified coronary plaque burden. When all biologic therapy was analysed as a group, there was improvement in fibro-fatty plaque burden, necrotic core with no significant changes in fibrous or dense-calcified burden. Although no significant changes in plaque burdens were seen in the non-biologic group, the burden of the fibro-fatty plaque subcomponent increased significantly.
Finally, exploratory analyses revealed that the change in coronary plaque burden in the biologic group was driven by those on anti-interleukin 17 treatment. This group also had the largest reduction in the necrotic core, however, these patients also started with higher total coronary plaque burden. Thus, the authors noted that direct comparisons between biologics were exploratory, and results should be interpreted with caution.
These results add to the growing body of literature demonstrating potential value of treating inflammation to reduce cardiovascular risk. These treatment options have already proven their utility in treatment of psoriasis skin disease.7 Future research should focus on analysing the impact of biologic therapy on coronary artery disease over longer period of times with deeper immune phenotyping including cell populations and secreted proteins (Figure 1). The authors provide interesting protein levels (interferon gamma, tumour necrosis factor alpha, interleukin 6, and interleukin 1 beta) before and after therapy hinting that these immune-based studies will greatly inform the biology of coronary plaque modulation, a much needed area of research to reduce the risk of inflammatory-driven cardiovascular disease risk.
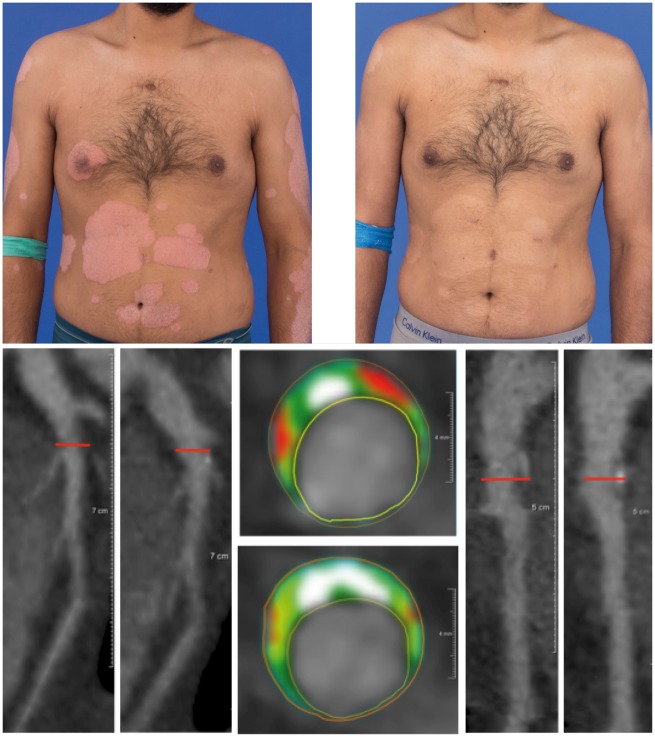
Figure 1.
Impact of biologic treatment on psoriasis and coronary artery disease. (Upper panel) Psoriasis patient before (left) and after (right) treatment with biologic agent demonstrates resolution of skin disease. (Lower panel) Representative coronary computed tomography angiography images of left anterior descending artery in a psoriasis patient. This patient had a low attenuation high-risk lipid-rich coronary plaque in the mid-left anterior descending artery before treatment with biologic treatment (left two images and upper image in the middle panel). Low attenuation plaque improves post-biologic therapy as seen in the lower image in the middle panel along with the two images on the right.
Conflict of interest: none declared.
References
References are available as supplementary material at European Heart Journal online.
Supplementary Material
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.