Abstract
Zika virus (ZIKV) has emerged as a globally important arbovirus and has been reported from all states of Brazil. The virus is primarily transmitted to humans through the bite of an infective Aedes aegypti (Linnaeus, 1762) or Aedes albopictus (Skuse, 1895). However, it is important to know if ZIKV transmission also occurs from Ae. aegypti through infected eggs to her offspring. Therefore, a ZIKV and dengue virus (DENV) free colony was established from eggs collected in Manaus and maintained until the third–fourth generation in order to conduct ZIKV vertical transmission (VT) experiments which used an infectious bloodmeal as the route of virus exposure. The eggs from ZIKV-infected females were allowed to hatch. The resulting F1 progeny (larvae, pupae, and adults) were quantitative polymerase chain reaction (qPCR) assayed for ZIKV. The viability of ZIKV vertically transmitted to F1 progeny was evaluated by cultivation in C6/36 cells. The effects of ZIKV on immature development of Ae. aegypti was assessed and compared with noninfected mosquitoes. AmazonianAe. aegypti were highly susceptible to ZIKV infection (96.7%), and viable virus passed to their progeny via VT. Moreover, eggs from the ZIKV-infected mosquitoes had a significantly lower hatch rate and the slowest hatching. In addition, the larval development period was slower when compared to noninfected, control mosquitoes. This is the first study to illustrate VT initiated by oral infection of the parental population by using mosquitoes, which originated from the field and a ZIKV strain that is naturally circulating in-country. Additionally, this study suggests that ZIKV present in the Ae. aegypti can modify the mosquito life cycle. The data reported here suggest that VT of ZIKV to progeny from naturally infected females may have a critical epidemiological role in the dissemination and maintenance of the virus circulating in the vector.
Keywords: Zika virus, vertical transmission, Aedes aegypti, fitness cost
Zika virus (ZIKV) was first isolated in 1947 and until 2007, the only reported outbreak had been in Micronesia (Kindhauser et al. 2016). In early 2015, Brazil reported the first case of ZIKV in a Northeastern state (Zanluca et al. 2015) with rapid expansion to all regions of the country. By 2017, 3,754 probable cases of ZIKV had been registered with an incidence rate of 1.8 cases/1,000 inhabitants (Brazilian Ministry of Health 2017a). Between November 2015 and May 2017, there were more than 13,000 suspected cases associated with changes in growth and development in newborns, with 2,722 cases confirmed and 3,245 cases still under investigation (Brazilian Ministry of Health 2017b). Currently, ZIKV is circulating in all Brazilian states.
ZIKV is transmissible primarily by mosquitoes, but other types of transmission have already been described, such as by sexual routes (McCarthy 2016). In mosquitoes, a mechanism that may contribute to virus survival through adverse conditions is vertical transmission (VT), when infected females pass the virus to her eggs/embryos and the resulting offspring (Ferreira-de-brito et al. 2016, Smartt et al. 2017). ZIKV is a member of the Flaviviridae family related to arboviruses such as West Nile virus, yellow fever virus and dengue virus (DENV) that can be transmitted from one mosquito generation to the next via VT (Rosen et al. 1983, Fontenille et al. 1997, Nelms et al. 2013).
The most important mechanism for the spread of ZIKV, and the resulting human disease, is the typical horizontal transmission via the bite of an infected Aedes aegypti, the primary vector (Kindhauser et al. 2016). However, it is essential to understand if infected Ae. aegypti are capable of VT of ZIKV. This may serve as a mechanism for maintaining ZIKV in the vectors in the absence of available or susceptible vertebrate hosts. In this report, we utilized newly colonized Brazilian Ae. aegypti and demonstrated the VT of ZIKV from orally infected female mosquitoes to their progeny, and illustrated that ZIKV infection also constrains the normal mosquito development.
Materials and Methods
Ethic Approval
This study was conducted in accordance with recommendations from the Manual for the Use of Animals (FIOCRUZ, Ministry of Health of Brazil, National decree, Nr. 3179) and approved by the Ethics Committee for the Use of Animals of Fundação Oswaldo Cruz (FIOCRUZ, Ministry of Health of Brazil, Nr. L-1715). This protocol was authorized by the Ethics in Animal Use Committee of Tropical Medicine Foundation Dr. Heitor Vieira Dourado, Manaus – AM, Brazil (protocol number 002380/2016).
Ae. aegypti Collection
Two thousand five hundred eggs were collected in the field using ovitraps in a ZIKV endemic area of Manaus, the capital city of the state of Amazonas, and allowed to hatch, all larvae were identified as Ae. aegypti. A subsample of 100 randomly chosen larvae was verified to be ZIKV and DENV-free by quantitative polymerase chain reaction (qPCR). The resulting virus-free adult mosquitoes were reared as described previously (Gonçalves et al. 2014) and used to establish a third–fourth generation to conduct ZIKV infection experiments.
ZIKV and Mosquito Infection
A human isolate of ZIKV from the State of São Paulo, Brazil (ZIKV/H. sapiens/Brazil/SPH/2015) was used to infect the mosquitoes (Cunha et al. 2016). Virus stocks were passaged and maintained in an Aedes albopictus clone C6/36 cell line (ATCC - CRL-1660) as previously described (Gonçalves et al. 2014). Virus titration followed the TCID50 method (Reed and Muench 1938). Two hundred, 3–5 d old, inseminated Ae. aegypti females were infected orally via glass feeding devices filled with ZIKV-infected C6/36 cell culture supernatant re-suspended in 2:1 fresh mouse blood with heparin (Gonçalves et al. 2014). The ZIKV titer of 5 × 105 PFU/ml was determined using Vero cell line by plaque assay. A control group of Ae. aegypti females was treated using the same conditions as the tested ZIKV-infected female group, but fed with a normal bloodmeal. Mosquitoes were allowed to feed for 1 h and 150 fully engorged females from each group were separated and maintained on 10% glucose solution ad libitum.
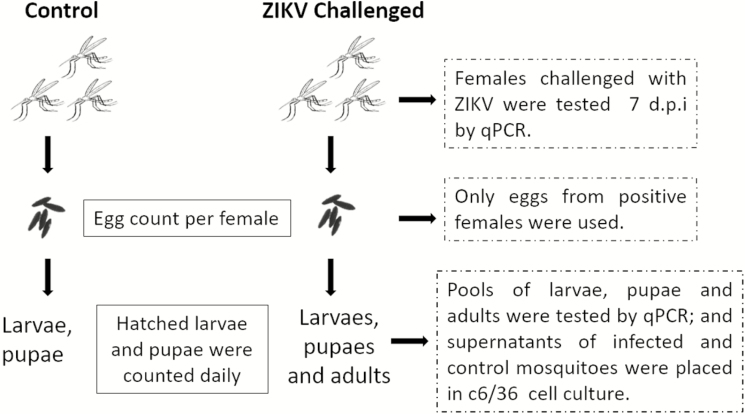
VT of ZIKV to the Ae. aegypti Progeny
Four days post infection (4 d.p.i.), 30 mosquitoes were randomly selected from the two experimental groups. Each mosquito was placed into a small individual cage and allowed to oviposit over the following 3 d. On the 7 d.p.i., the parental infected mosquitoes were individually evaluated for ZIKV by qPCR (Secundino et al. 2017). Four days after the oviposition, eggs from positive females (ZIKV-infected) and control mosquitoes were separated into two groups and placed in small cups to observe individual hatching. The resulting F1 larvae (L3–L4) were randomly placed into sixty groups of 10 (n = 600). Twenty individuals at each distinct developmental stage (larvae, pupae, and adults, n = 200) of these two groups were assayed for ZIKV by qPCR as 10 single pools. Individuals of each stage were chosen randomly regardless of sex.
Effect of VT-ZIKV on Ae. aegypti Developmental Stages
Thirty parentally ZIKV-infected Ae. aegypti were randomly selected and allowed to oviposit in order for us to evaluate the number of laid eggs, time to hatch, and period of larval development until pupation of the infected F1 progeny. Larvae and pupae were counted every day since the eggs hatched. The data were compared with the control group. The two groups were kept in the same room, and in the identical controlled conditions (temperature [28°C], humidity [80%], food availability, and breeding container).
Viability of VT-ZIKV to the Progeny
Fifteen F1 VT-ZIKV Ae. aegypti adults were grouped into three pools of five individuals and macerated in L-15 medium with 1% Penicillin/Streptomycin (10,000 U/ml), 2.5 g/ml Amphotericin B and 2% FBS, cultivated in C6/36 cells for 5 d as described above for observation of ZIKV growth and cytopathic effect (CPE; Contreras and Arumugaswami 2016).The ZIKV-free mosquitoes were used as negative control and inoculated in cell culture at the same time as test mosquitoes.
VT-ZIKV Detection and Quantification by qPCR
Samples were processed for RNA extraction (QIAamp viral RNA Mini kit, Qiagen, Hilden, Germany) (Lanciotti et al. 2008). Reverse transcription with cDNA production was carried out using a random primer and M-MLV enzyme, and subsequent TaqMan-based qPCR assay for ZIKV (primers set ZIKV 1086 and ZIKV 1162c) (Lanciotti et al. 2008, Secundino et al. 2017). Standard curve used was from gBlocks Gene Fragments dilutions, range 30,000 to 3 copies.
Statistical Analyses
Shapiro Wilk and two-tailed Student’s t-tests were used to evaluate significance among the groups in relation to mean numbers of laid eggs. Differences in numbers of hatched eggs among groups were evaluated using two-tailed χ 2 or Fisher’s tests. Period of time to egg hatching and development time of the larvae until pupation were analyzed using a Kaplan-Meier (log-rank) analysis, P values ≤ 0.05 were considered significant. Statistical analysis was performed in GraphPad Prism, version 5.00 (San Diego, CA) and Stata (Stata Statistical Software, version 13.0).
Results
ZIKV Infection of the Amazonian Ae. aegypti and Vertical and Trans-stadial Transmission in the Progeny
The Amazonian Ae. aegypti were very susceptible to ZIKV infection. Individual qPCR analysis of the 7 d.p.i mosquitoes revealed an infection rate (IR) of 96.7% (29/30) with a median (md) = 1.3 × 106 ZIKV cDNA copies/mosquito. The analysis of a total of 600 F1 individuals in 20 pools per life stage demonstrated high filial infection rates (FIR) due to VT of ZIKV as follows: 55% in larvae (11 out of 20 pools) md = 2.5 × 102 ZIKV cDNA copies, 50% in pupae (10 out 20 pools) md = 1.9 × 102 ZIKV cDNA copies and 70% in adults (14 out of 20 pools) md = 1.7 × 102 ZIKV cDNA copies. Trans-stadial transmission (i.e., presence of ZIKV from one life stage to the next), showed the minimum filial infection rates (MFIR) to be 1:18 in larvae, 1:20 in pupae, and 1:14.3 in adults (Table 1 and Fig. 1).
Table 1.
ZIKV infection of Aedes aegypti and F1 progeny
| Parental | F1 progeny | |||||
|---|---|---|---|---|---|---|
| IR (%) | Median cDNA copies ± SD | Stage | Nº pools (10 individuals) | FIRa (%) | MFIRb | Median cDNA copies ± SD |
| Larvae | 20 | 11/20 (55) | 1:18.2 | 2.5 × 102 ± 2.1 × 103 | ||
| 29/30 (96.7) | 1.3 × 106 ± 1.4 × 107 | Pupae | 20 | 10/20 (50) | 1:20.0 | 1.9 × 102 ± 8.3 × 102 |
| Adult | 20 | 14/20 (70) | 1:14.3 | 1.7 × 102 ± 2.9 × 102 |
aFilial infection rate.
bMinimum filial infection rate.
Fig. 1.
Schematic representation of the experimental design.
Effect of VT-ZIKV and Trans-stadial Infection in the Development of Amazonian Ae. aegypti
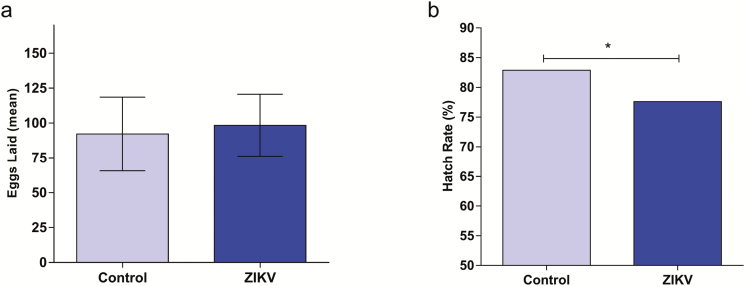
Out of the 30 selected parental ZIKV-infected Ae. aegypti, 29 of these laid 2,853 eggs while the same number of the control mosquitoes laid 2,672 eggs (one female in each group died before laying eggs), of these 2,215 and 2,214 hatched, respectively. The mean number of laid eggs by each ZIKV-infected and control mosquitoes were 98.36 (±22.20) and 92.14 (±26.44), respectively, with no significant difference in oviposition rates (Fig. 2a). The eclosion rates (number of eggs hatched/number of eggs laid) were 82.9% for control and 77.6% for VT-ZIKV-infected mosquitoes, which was statically significant (P < 0.001) (Fig. 2b).
Fig. 2.
Evaluation of number of eggs laid and hatched for Ae. aegypti infected with ZIKV. (a) Mean number of eggs laid; (b) Egg hatch rate.
Fitness Costs of VT-ZIKV-infected Ae. aegypti Progeny
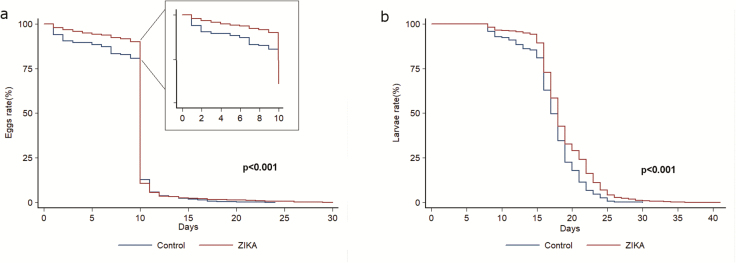
The fitness costs of the VT-ZIKV-infected F1 Ae. aegypti progeny were measured using survivorship curves following the Kaplan-Meier method and tested for significance by Log-rank test (P < 0.05). The number of eggs hatched daily and the period of larval development to pupae was compared between the VT-ZIKV-infected and control mosquitoes. Differences in the hatch rate occurred in the first 10 d. The VT-ZIKV group had the slowest hatching and the larval development period (eclosion to pupation) compared with control group (P < 0.001; Fig. 3a and b).
Fig. 3.
The fitness cost of Ae. aegypti progeny derived from ZIKV-infected mosquitoes compared with the control. (a) Analysis of number of eggs hatched daily illustrates difference in the hatch rate happened in the first 10 d, ZIKV group has the slowest hatching. (b) Larval development time from hatching to pupation was longer for ZIKV-infected individuals. (Kaplan-Meier [log-rank] analysis, P values ≤ 0.05 were considered significant).
Viability of VT-ZIKV of the Ae. aegypti Progeny
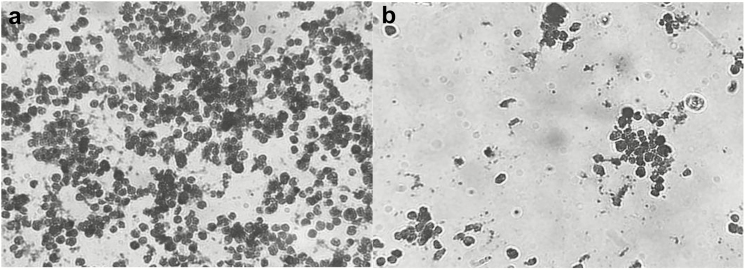
The supernatant of macerated F1 adult mosquitoes was evaluated for viable ZIKV by cell cultures. Orally infected VT-ZIKV Ae. aegypti F1 of the progeny was able to infect C6/36 cell cultures and CPE was observed at 5 d.p.i. (Fig. 4).
Fig. 4.
Light microscopy of uninfected and ZIKV-infected C6/36 cell monolayers, 5 days post inoculum. (a) Uninfected C6/36 cells in a typical monolayer. (b) C6/36 cultivated with the supernatants of the adult F1 progeny derived from the ZIKV-infected parental mosquitoes reveal significant cytopathic effect with the formation of large syncytia.
Discussion
The first two cases of ZIKV were confirmed in Manaus, State of Amazonas, in January 2016. In 2017, 1 yr later, the city confirmed 4,418 Zika cases including 500 pregnant women and five microcephaly cases in newborns (Semsa 2017). It is astonishing how quickly ZIKV spread through the city and improving our understanding of ZIKV dispersal and transmission is critical. Today, it is well known that ZIKV behaves differently from other Flaviviruses since it is capable of being transmitted sexually between humans via its presence in body fluids such as semen and urine, and in the female genital tract (Baud et al. 2017).
In cities like Manaus, several factors such as unplanned urban expansion, irregular or absence of waste collection, and poor socioeconomic conditions contribute to the development of breeding sites and subsequent increases in the Ae. aegypti populations. Previously, only two studies, using mosquitoes from Rio de Janeiro, a Southeastern city, described the susceptibility of Brazilian Ae. aegypti to ZIKV. The first study reports a high infection and disseminated IR (Dutra et al. 2016), which is similar to our findings. The second study reports a high IR, but with low levels of disseminated infection in recently colonized Ae. aegypti (Chouin-Carneiro et al. 2016). Since we worked with a mosquito population from Manaus, a Northern city, these differences may reflect the genetic or physiological variability in the permissiveness of these geographically different Ae. aegypti populations.
The Amazonian Ae. aegypti mosquitoes are highly susceptible to oral ZIKV infection and we verified the VT to their progeny. The MFIR of the larvae and adults of the Ae. aegypti was greater than other studies describing VT in other populations (Thangamani et al. 2016, Ciota et al. 2017). It is worth noting that, in the previous VT studies, the infections were artificially initiated via intra-thoracic injection by syringe, however, our study was the first one to demonstrate the VT-ZIKV by natural oral infection of the parental mosquitoes. Additionally, this study used third and fourth generations of Ae. aegypti from eggs collected in the field, infected with a ZIKV strain that is naturally circulating in the country. In 2016, a study in Rio de Janeiro Brazil showed for the first time that among 963 Ae. aegypti males only one was naturally infected with ZIKV by venereal and/or VT (Ferreira-de-Brito et al. 2016). Certainly, this experimental model is a more accurate reflection of how efficiently VT-ZIKV mosquitoes occur in an endemic region.
Many studies have shown that pathogens, including arboviruses transmitted by insects, can affect vector fitness mainly related to their physiology (Power 1992, Keating et al. 2013). Decreased fecundity and fertility of DENV infected parental Ae. aegypti and lengthening of the larval development period of VT-DENV infected progeny have been reported (Joshi et al. 2002, Maciel-de-Freitas et al. 2011). In addition, our study shows that ZIKV infection also alters Ae. aegypti’s physiology, e.g., by delaying hatching of the eggs and by changing the larvae stage. Essentially, there is no significant difference in the number of laid eggs by ZIKV-infected parental Ae. aegypti compared to the noninfected mosquitoes, but a decrease in egg eclosion rate occurred, and the larval development period of the VT-ZIKV-infected progeny increased.
Our results show that ZIKV infection in Ae. aegypti has the potential to modify the mosquito life cycle by increasing the time of two major life stages: egg eclosion and larval development. The data reported here suggest that VT of ZIKV to progeny from naturally infected females may have a critical role in the dissemination and maintenance of the virus circulating in the vector.
VT occurs, but with a small number of cDNA viral copies in VT-ZIKV-infected progeny, similar to a study with VT-DENV-1 in Ae. aegypti and Ae. albopictus (Buckner et al. 2013). These are important aspects that need to be explored further in the context of urban vector-borne disease dispersal since they can have a significant epidemiological impact. The developmental delays in immature vector mosquitoes and the decrease in the eggs hatching rate induced by ZIKV infection may make the mosquito more vulnerable to vector control of immature stages. This kind of information about vector biology is important for directing interventions in vector control; and this can influence the dispersion and incidence of the disease. If Ae. aegypti mosquitoes emerge already infected and are capable of transmitting ZIKV to humans, the potential risk is dramatically increased, especially for populations already bearing the brunt of ongoing epidemics. Thus, it is necessary to develop complementary studies to evaluate vector competence of ZIKV-infected progeny, as well as gaining a better understanding of how many generations ZIKV can be maintained for via VT in field populations of permissive vectors.
Acknowledgments
This study was partially funded by the following Brazilian agencies: Foundation of the Institute Oswaldo Cruz (FIOCRUZ), Strategic Program for Supporting Health Research (PAPES VI), Brazilian Council for Scientific and Technological Development (CNPq/MS/CAPES/DECIT), Program Science without Borders, INCT-Instituto Nacional de Ciencia e Tecnologia - Entomologia Molecular, Minas Gerais State Research Support Foundation (FAPEMIG), and Amazonas State Research Support Foundation (FAPEAM). Support Program to Young Ph.D. Professors – Federal University of Bahia (PROPESQ/UFBA). N.F.C.S., M.V.G.L., M.G.V.B.G., and P.F.P.P. are research fellows, supported by CNPq. B.A.C., T.B.C., A.S.O., E.B.C.V., and N.B.R. are student fellows supported by CAPES and K.R.D.S., L.E.M.V., and R.N.P. are supported by CNPq; A.C.P. and A.B.V.J. are supported by FAPEAM.
References Cited
- Baud D., Gubler D. J., Schaub B., Lanteri M. C., and Musso D.. . 2017. An update on Zika virus infection. Lancet. 390: 2099–2109. [DOI] [PubMed] [Google Scholar]
- Brazilian Ministry of Health 2017a. Monitoramento dos casos de dengue, febre de chikungunya e febre pelo vírus Zika até a Semana Epidemiológica 4, 2017 (Portuguese) http://combateaedes.saude.gov.br/images/pdf/2017-Dengue_Zika_Chikungunya-SE4.pdf.
- Brazilian Ministry of Health 2017b. Monitoramento integrado de alterações no crescimento e desenvolvimento relacionadas à infecção pelo vírus Zika e outras etiologias infecciosas, até a Semana Epidemiológica 18/2017 (Portuguese) http://portalarquivos.saude.gov.br/images/pdf/2017/junho/01/BE-2017-015-Monitoramento-integrado-de-alteracoes-no-crescimento-e-desenvolvimento.pdf.
- Buckner E. A., Alto B. W., and Lounibos L. P.. . 2013. Vertical transmission of key West dengue-1 virus by Aedes aegypti and Aedes albopictus (Diptera: Culicidae) mosquitoes from Florida. J. Med. Entomol. 50: 1291–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chouin-Carneiro T., Vega-Rua A., Vazeille M., Yebakima A., Girod R., Goindin D., Dupont-Rouzeyrol M., Lourenço-de-Oliveira R., and Failloux A. B.. . 2016. Differential susceptibilities of Aedes aegypti and Aedes albopictus from the Americas to Zika virus. Plos Negl. Trop. Dis. 10: e0004543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciota A. T., Bialosuknia S. M., Ehrbar D. J., and Kramer L. D.. . 2017. Vertical transmission of Zika virus by Aedes aegypti and Ae. albopictus mosquitoes. Emerg. Infect. Dis. 23: 880–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contreras, D., and V. Arumugaswami. 2016. Zika Virus Infectious Cell Culture System and the In Vitro Prophylactic Effect of Interferons. JoVE. (114), 54767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunha M. S., Esposito D. L. A., Rocco I. M., Maeda A. Y., Vasami F. G. S., Nogueira J. S., de Souza R. P., Suzuki A., Addas-Carvalho M., Barjas-Castro M. de L., . et al. 2016. First complete genome sequence of Zika virus (Flaviviridae, Flavivirus) from an autochthonous transmission in Brazil. Genome Announc. 4: e00032–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutra H. L., Rocha M. N., Dias F. B., Mansur S. B., Caragata E. P., and Moreira L. A.. . 2016. Wolbachia blocks currently circulating Zika Virus Isolates in Brazilian Aedes aegypti Mosquitoes. Cell Host Microbe 19: 771–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira-de-brito A., Ribeiro I. P., De Miranda R. M., Fernandes R. S., Campos S. S., Antunes K., De Castro M. G., Bonaldo M. C., Brasil P., and Lourenço-de-oliveira R.. . 2016. First detection of natural infection of Aedes aegypti with Zika virus in Brazil and throughout South America. Mem. Inst. Oswaldo Cruz. 111: 655–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontenille D., Diallo M., Mondo M., Ndiaye M., and Thonnon J.. . 1997. First evidence of natural vertical transmission of yellow fever virus in Aedes aegypti, its epidemic vector. Trans. R. Soc. Trop. Med. Hyg. 91: 533–535. [DOI] [PubMed] [Google Scholar]
- Gonçalves C. M., Melo F. F., Bezerra J. M., Chaves B. A., Silva B. M., Silva L. D., Pessanha J. E., Arias J. R., Secundino N. F., Norris D. E., . et al. 2014. Distinct variation in vector competence among nine field populations of Aedes aegypti from a Brazilian dengue-endemic risk city. Parasit. Vectors. 7: 320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi V., Mourya D. T., and Sharma R. C.. . 2002. Persistence of dengue-3 virus through transovarial transmission passage in successive generations of Aedes aegypti mosquitoes. Am. J. Trop. Med. Hyg. 67: 158–161. [DOI] [PubMed] [Google Scholar]
- Keating J. A., Bhattacharya D., Rund S. S., Hoover S., Dasgupta R., Lee S. J., Duffield G. E., and Striker R.. . 2013. Mosquito protein kinase G phosphorylates flavivirus NS5 and alters flight behavior in Aedes aegypti and Anopheles gambiae. Vector Borne Zoonotic Dis. 13: 590–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindhauser M. K., Allen T., Frank V., Santhana R. S., and Dye C.. . 2016. Zika: the origin and spread of a mosquito-borne virus. Bull. World Health Organ. 94: 675–686C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanciotti R. S., Kosoy O. L., Laven J. J., Velez J. O., Lambert A. J., Johnson A. J., Stanfield S. M., and Duffy M. R.. . 2008. Genetic and serologic properties of Zika virus associated with an epidemic, Yap State, Micronesia, 2007. Emerg. Infect. Dis. 14: 1232–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maciel-de-Freitas R., Koella J. C., Lourenço-de-Oliveira R., Lourenc R., and Lourenço-de-Oliveira R.. . 2011. Lower survival rate, longevity and fecundity of Aedes aegypti (Diptera: Culicidae) females orally challenged with dengue virus serotype 2. Trans. R. Soc. Trop. Med. Hyg. 105: 452–458. [DOI] [PubMed] [Google Scholar]
- McCarthy M. 2016. Zika virus was transmitted by sexual contact in Texas, health officials report. BMJ. 352: i720. [DOI] [PubMed] [Google Scholar]
- Municipal Health Secretariat (Semsa) Manaus City Hall. 2017. 68o Informe Epidemiologico (In Portuguese). https://semsa.manaus.am.gov.br/semsa-divulga-68o-informe-epidemiologico-do-zika-virus/ [Google Scholar]
- Nelms B. M., Fechter-Leggett E., Carroll B. D., Macedo P., Kluh S., and Reisen W. K.. . 2013. Experimental and natural vertical transmission of West Nile virus by California Culex (Diptera: Culicidae) mosquitoes. J. Med. Entomol. 50: 371–378. [DOI] [PubMed] [Google Scholar]
- Power A. G. 1992. Patterns of virulence and benevolence in insect-borne pathogens of plants. CRC. Crit. Rev. Plant Sci. 11: 351–372. [Google Scholar]
- Reed, L. J. and H. Muench. 1938. Muench H: A simple method of estimating fifty percent endpoints. Am. J. Hyg. 27: 493–497. [Google Scholar]
- Rosen L., D. A. Shroyer, R. B. Tesh, J. E. Freier and J. C. Lien. 1983. Transovarial transmission of dengue viruses by mosquitoes: Aedes albopictus and Aedes aegypti. Am. J. of Trop. Med. Hyg. 32: 1108–1119 [DOI] [PubMed] [Google Scholar]
- Secundino N. F. C., Chaves B. A., Orfano A. S., Silveira K. R. D., Rodrigues N. B., Campolina T. B., Nacif-Pimenta R., Villegas L. E. M., Silva B. M., Lacerda M. V. G., . et al. 2017. Zika virus transmission to mouse ear by mosquito bite: a laboratory model that replicates the natural transmission process. Parasit. Vectors. 10: 346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smartt C. T., Stenn T. M. S., Chen T. Y., Teixeira M. G., Queiroz E. P., Souza Dos Santos L., Queiroz G. A. N., Ribeiro Souza K., Kalabric Silva L., Shin D., . et al. 2017. Evidence of Zika virus RNA fragments in Aedes albopictus (Diptera: Culicidae) field-collected eggs from Camaçari, Bahia, Brazil. J. Med. Entomol. 54: 1085–1087. [DOI] [PubMed] [Google Scholar]
- Thangamani S., Huang J., Hart C. E., Guzman H., and Tesh R. B.. . 2016. Vertical Transmission of Zika Virus in Aedes aegypti Mosquitoes. Am. J. Trop. Med. Hyg. 95: 1169–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanluca C., Melo V. C., Mosimann A. L., Santos G. I., Santos C. N., and Luz K.. . 2015. First report of autochthonous transmission of Zika virus in Brazil. Mem. Inst. Oswaldo Cruz. 110: 569–572. [DOI] [PMC free article] [PubMed] [Google Scholar]