Abstract
Background/Objectives
Bariatric surgery is helpful in enabling sustained weight loss, but effects on depression are unclear. Reductions in depression-related symptoms and increases in suicide rate have both been observed after bariatric surgery, but these observations are confounded by the presence of pre-existing depression. The goal of this study is to evaluate the effect of bariatric surgery on subsequent depression diagnosis.
Subjects/Methods
In this observational study, a prospective cohort study was simulated by evaluating depression risk based on diagnostic codes. An administrative database was utilized for this study, containing records and observations between 1 January 2008 through 29 February 2016 of enrolled patients in the United States. Individuals considered in this analysis were enrolled in a commercial health insurance program, observed for at least 6 months prior to surgery, and met the eligibility criteria for bariatric surgery. In all, 777,140 individuals were considered in total.
Results
Bariatric surgery was found to be significantly associated with subsequent depression relative to both non-surgery controls (HR = 1.31, 95% CI, 1.27–1.34, P < 2e–32) and non-bariatric abdominal surgery controls (HR = 2.15, 95% CI, 2.09–2.22, P < 2e–32). Patients with pre-surgical psychiatric screening had a reduced depression hazard ratio with respect to patients without (HR = 0.85, 95% CI, 0.81–0.89, P = 3.208e–12). Men were found to be more susceptible to post-bariatric surgery depression compared with women. Pre-surgical psychiatric evaluations reduced the magnitude of this effect. Relative to bariatric surgeries as a whole, vertical sleeve gastrectomy had a lower incidence of depression, while Roux-en Y Gastric Bypass and revision/removal surgeries had higher rates.
Conclusions
In individuals without a history of depression, bariatric surgery is associated with subsequent diagnosis of depression. This study provides guidance for patients considering bariatric surgery and their clinicians in terms of evaluating potential risks and benefits of surgery.
Introduction
Bariatric surgery is recognized as an effective treatment for severe obesity, resulting in large, sustained weight loss and improved quality of life [1]. Post-operative depression has been implicated as a predictor of poor overall weight loss after surgery. As a result, evaluating the relationship between bariatric surgery and depression is important in ensuring the success of the procedure [2]. However, it is difficult to separate the potential of bariatric surgery to reduce pre-existing depressive symptoms from reduction of depression after surgery at the population level due to confounding by the presence/absence of pre-existing mood disorders. This analysis is further complicated by the bidirectional associations between depression and obesity [3]. Previous studies have tended to focus on the reduction in depressive symptoms in the same individuals before and after bariatric surgery, generally reporting a reduction in depression rates between 55 and 65% over 2 years [4-6]. The Swedish Obese Subjects (SOS) study reported long-term reductions in depression among bariatric surgery patients relative to conventionally treated patients, but the studied individuals seeking surgery had higher baseline incidence of depression relative to the control population [7]. In contrast, an increase in suicide among gastric bypass surgery patients relative to matched non-surgical controls has been reported [8], but this observation was similarly attributed to the presence of preoperative depression [9]. A separate study of patients in Pennsylvania implicated both disappointment with weight regain and lack of follow-up appointments with the association between bariatric surgery and suicide [10].
A clear understanding of the influence of bariatric surgery on post-surgical depression risk will assist the determination of ideal candidates for weight loss surgery from a psychological standpoint, and inform surgical follow-up standards of care. We performed a causal-inference analysis of post-surgical rates of depression in populations undergoing and eligible for bariatric surgery (body mass index (BMI) ≥ 40 kg/m2 or BMI ≥ 35 kg/m2 with a comorbid condition) [11], and without a history of depression. To our knowledge, our utilization of health insurance claims data for this analysis represents the largest such study to date.
Methods
Using un-identifiable member claims data from Aetna, a prospective cohort study was simulated. The claims dataset contained diagnosis and intervention records for >63 million individuals in the United States between 2008 and 2016. Race, ethnicity, and socioeconomic data were not present in the database. International Classification of Diseases, Ninth Revision (ICD-9) codes were used to define diagnoses, while ICD-9 and Current Procedural Terminology (CPT) codes were used to define procedures and interventions. Phenome-wide association study [12] (PheWAS) codes were used to map ICD-9 codes according to phenotype. All calculations were conducted using Microsoft SQL Server and R statistical software, version 3.4.3 [13]. R packages survival and data.table were also used. The Harvard Medical School Institutional Review Board waived the approval requirement, as it determined this analysis of the dataset not to be human subjects research.
Using annotations of diagnoses and procedures, all individuals who were eligible for and who underwent bariatric surgery were identified, with relevant codes and criteria defined using published UnitedHealthcare Commercial Medical Policy [14]. Patients undergoing non-bariatric abdominal surgery were identified using CPT codes for anesthesia for abdominal surgeries. For patients with multiple surgeries, the earliest date available was used. Non-surgical groups were assigned a placeholder surgery date to enable comparisons with surgical groups. These dates were calculated by identifying the earliest eligibility date and adding the median eligibility-to-surgery time observed in the bariatric surgery cohort. A similar process was conducted for comparisons against non-bariatric abdominal surgeries, identified using anesthesia codes. Some of the most common surgeries in this category included cholecystectomies, appendectomies, and hernia repairs. Individuals were required to have at least 6 months of observations prior to their surgery/placeholder date to be included in the study. An analysis of all depression diagnoses in our dataset found that the mean number of days between depression diagnoses was 58 days, and that 93% of all depression diagnoses were separated by fewer than 6 months, indicating that it was unlikely that unobserved depression diagnoses prior to the observation period were frequent. Subsequent diagnoses of depression were identified using phenotype-level codes corresponding to “Depression” or “Major Depressive Disorder” (Supplementary Table 3). Individuals with codes corresponding to diagnoses of depression prior to their surgery/placeholder date were excluded from the analysis.
To examine the effect of bariatric surgery on subsequent depression diagnosis, Cox proportional hazard models and Kaplan-Meier cumulative incidence estimates were used to evaluate hazard ratios for depression between three pairs of groups (Table 1):
Table 1.
Study cohort distribution
| Number (%) | |||
|---|---|---|---|
| Bariatric surgery patients | Bariatric surgery patients | ||
| Prior psych evaluation | No prior psych evaluation | ||
| Total | 64,090 | 25,861 | 38,229 |
| Men | 18,403 (28.7) | 6983 (27) | 11,420 (29.87) |
| Age, years, mean (SD) | 46.19 (13.59) | 43.86 (11.52) | 47.76 (14.63) |
| Post-surgical depression diagnosis (≥1) | 7421 (11.57) | 2647 (10.24) | 4774 (12.49) |
| Protracted post-surgical depression occurrences (≥3 diagnoses/6 months) | 2550 (3.98) | 951 (3.68) | 1599 (4.18) |
| BMI, mean (SD) | 44.76 (7.08) | 45.37 (7.13) | 44.12 (6.98) |
| 6-Month code count, mean (SD) | 120.63 (123.64) | 121.71 (92) | 119.9 (141.07) |
| 6-Month diagnosis count, mean (SD) | 56.21 (55.04) | 58.84 (41.96) | 54.44 (62.29) |
| 6-Month procedure count, mean (SD) | 64.42 (71.64) | 62.87 (52.99) | 65.47 (81.87) |
| Follow-up time, days, mean (SD) | 748.78 (665.53) | 716.38 (647.54) | 770.71 (676.56) |
| Number (%) | |||
| Bariatric eligible individuals | Bariatric eligible individuals | ||
| Other abdominal surgery patients | Non-surgery individuals | ||
| Total | 713,050 | 220,706 | 492,344 |
| Men | 327,413 (45.92) | 97,702 (44.26) | 229,711 (46.65) |
| Age, years, mean (SD) | 53.22 (15.59) | 57.69 (12.63) | 51.62 (16.66) |
| Post-surgical depression diagnosis (≥1) | 64,932 (9.11) | 13,843 (6.27) | 51,089 (10.38) |
| Protracted post-surgical depression occurrences (≥3 diagnoses/6 months) | 20,051 (2.81) | 3991 (1.8) | 16,070 (3.26) |
| BMI, mean (SD) | 41.58 (7.06) | 41.15 (6.95) | 41.8 (7.11) |
| 6-Month code count, mean (SD) | 53.43 (83.12) | 103.06 (132.03) | 46.52 (74.16) |
| 6-Month diagnosis count, mean (SD) | 24.77 (36.93) | 48.07 (60.34) | 24.86 (42.86) |
| 6-Month procedure count, mean (SD) | 28.67 (48.28) | 54.99 (74.7) | 24.86 (33.20) |
| Follow-up time, days, mean (SD) | 892.33 (654.27) | 857.24 (646.68) | 985.22 (640.32) |
All individuals considered are either bariatric surgery patients or eligible for bariatric surgery. While bariatric surgery patients are also eligible for bariatric surgery, the term “surgery eligible” refers to individuals who did not receive bariatric surgery in this analysis
Bariatric surgery patients vs. bariatric surgery eligible individuals who did not receive bariatric surgery (referred to here as “surgery eligible individuals”). Note that while bariatric surgery patients are also technically eligible for surgery, the phrase “surgery eligible individuals” will refer to those who did not receive bariatric surgery.
Bariatric surgery patients vs. surgery eligible individuals who received non-bariatric abdominal surgery (referred to as “other abdominal surgery patients”). Patients with both bariatric surgeries and non-bariatric abdominal surgeries were placed in the bariatric surgery cohort.
Other abdominal surgery patients vs. surgery eligible individuals who received no abdominal surgeries, bariatric or otherwise (referred to as “non-surgery individuals”).
Sex, age, and pre-surgical ICD code count (6 months) were treated as covariates in all hazard ratio models, and sex-stratified multivariate analyses were conducted. Analyses were further stratified by bariatric surgery type and whether bariatric surgery patients had annotations of psychiatric evaluation 6 months prior to the surgery.
To identify what phenotypes were associated with post-bariatric surgery depression risk, matched case–control groups were created, using both surgery eligible and other abdominal surgery patient cohorts as controls. Patients were matched based on sex, age, pre-surgical ICD code count (6 months), and ZIP code. Pre- and post-surgical phenotypes were examined separately. Phenotype counts and depression status were recorded for all patients in all cohorts, and phenotype-specific risk ratios for depression were computed. Only phenotypes that (i) were found to be significantly associated with depression in the bariatric surgery cohort, (ii) were not found to be significantly associated with depression in either of the control cohorts, and (iii) had at least 100 co-occurring depression diagnoses were examined. Bonferroni correction was used to correct for multiple hypothesis testing.
Results
In total, 777,140 individuals were considered, including 64,090 bariatric surgery patients (Table 1). Among all considered individuals, there were 72,353 individuals diagnosed with depression (PheWAS code in 296.2 group), for a population incidence of 9.3%. This is lower than previous estimates [15] of depression prevalence among individuals with obesity, but can be rationalized by the exclusion of individuals with histories of depression prior to surgery from the analysis. Among bariatric surgery patients, 7421 subsequent depression diagnoses were recorded, for a population incidence of 11.57%. The mean follow-up time for bariatric surgery patients was 748 days, compared with 892 days for bariatric eligible individuals and 985 days for non-bariatric abdominal surgery patients.
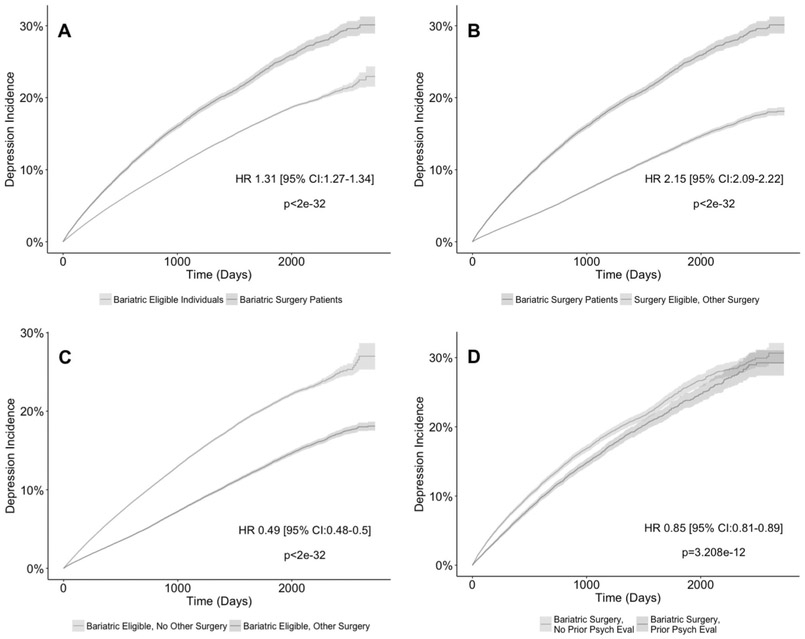
Figure 1 summarizes the results of Cox regression models over the patient cohorts. Bariatric surgery was found to have a hazard ratio of 1.31 (95% confidence interval (CI), 1.27–1.34, P < 2e–32) toward subsequent depression when compared with surgery eligible individuals. Furthermore, bariatric surgery was found to have a hazard ratio of 2.15 (95% CI, 2.09–2.22, P < 2e–32) compared with other abdominal surgery patients. Other abdominal surgery patients had a hazard ratio of 0.49 (95% CI, 0.48–0.50, P < 2e–32) relative to non-surgery individuals. Age and code count 6 months prior to surgery were found to have minor effects (hazard ratios between 0.98 and 1.02, all P < 2e–32) on the hazard ratio. Pre-surgical BMI measurements were available for a subset of patients examined (n = 132,000). Within this cohort, BMI was observed to have a small but statistically significant hazard ratio (1.01, P = 6.1e–12) with respect to depression (Supplementary Fig. 2). As an additional point of comparison, the depression hazard ratio for patients undergoing laparoscopic bariatric surgeries (n = 58,536) compared with bariatric eligible individuals undergoing non-bariatric laparoscopic surgeries of the stomach and esophagus (n = 2679) was found to be 1.39 (95% CI, 1.30–1.50, P < 2e–32), consistent with the finding that the non-bariatric laparoscopic surgery cohort had no elevated risk of depression relative to the non-surgical group (HR = 1.03, 95% CI, 0.98–1.09, P < 2e–32) (Supplementary Table 2).
Fig. 1.
Incidence of post-surgical depression. Text represents the hazard ratio and confidence interval between the two plotted cohorts. a Time-to-depression curve for bariatric surgery patients compared with bariatric eligible individuals. b Time-to depression curve for bariatric surgery patients compared with bariatric eligible individuals with other abdominal surgeries. c Time-to-depression curve for bariatric eligible individuals with other abdominal surgeries compared with non-surgery individuals. d Time-to-depression curve for bariatric surgery patients with pre-surgical psychiatric evaluations compared with bariatric surgery patients without pre-surgical psychiatric evaluations. All hazard ratios are adjusted for sex, age, and 6-month claim count
Psychiatric evaluation prior to bariatric surgery is commonly recommended [16, 17]. The effect of psychiatric evaluations or testing 6 months prior to bariatric surgery on the risk of subsequent depression was examined. Relative to bariatric surgery patients without pre-surgical psychiatric evaluations/tests, patients who received them (n = 25,861) prior to bariatric surgery had a hazard ratio of 0.85 (95% CI, 0.81–0.89, P = 3.208e–12). For this study, depression was defined as a single observation of a depression code patient’s record. These annotations do not make reference to the severity or degree of diagnosis. The prevalence of protracted depression, defined as three or more diagnoses of depression within a 6-month period, was examined with respect to bariatric surgery. Although the absolute incidence of protracted depression was lower compared with standard depression, similar trends in hazard ratio were observed (Supplementary Fig. 1).
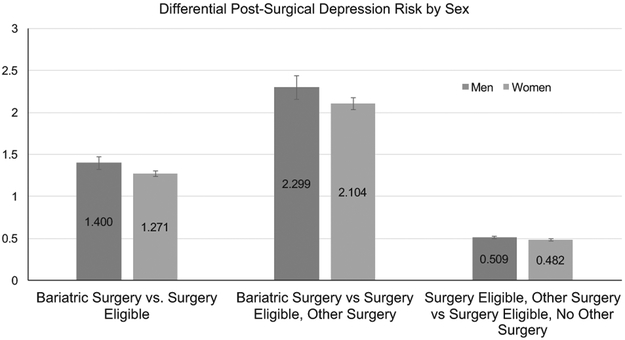
Figure 2 shows the hazard ratios for the bariatric surgery comparisons stratified by sex. Consistent with previous studies [18], the rate of depression was found to be higher among female individuals, but men were typically more susceptible to a post-bariatric surgery depression effect. With respect to surgery eligible patients, male patients undergoing bariatric surgery had a hazard ratio of 1.40 (95% CI, 1.329–1.475, P < 2e–32), whereas female patients had a hazard ratio of 1.271 (95% CI, 1.236–1.307, P < 2e–32) (Supplementary Figs. 3, 4). Compared with the other abdominal surgery cohort, male patients undergoing bariatric surgery had a hazard ratio of 2.299 (95% CI, 2.165–2.442, P < 2e–32), whereas female patients had a hazard ratio of 2.104 (95% CI, 2.031–2.178, P < 2e–32). The effect of sex on post-surgical depression diagnosis risk was significantly smaller in magnitude when considering non-bariatric surgeries. When evaluating the hazard ratios for other abdominal surgery patients compared with non-surgery individuals, the hazard ratio for men was 0.509 (95% CI, 0.492–0.526, P < 2e–32) compared with 0.482 (95% CI, 0.471–0.494, P < 2e–32) for women. The difference in hazard ratios between men and women for all comparisons was found to be significant with P < 0.0001 based on bootstrap analysis.
Fig. 2.
Sex-stratified time-to-depression diagnosis curves. Red bars represent the case groups in each plot (bariatric surgery or other abdominal surgery patients), whereas blue bars represent the control groups (surgery eligible individuals, other abdominal surgery patients, non-surgery individuals, respectively). Error bars represent 95% confidence intervals. (color figure online)
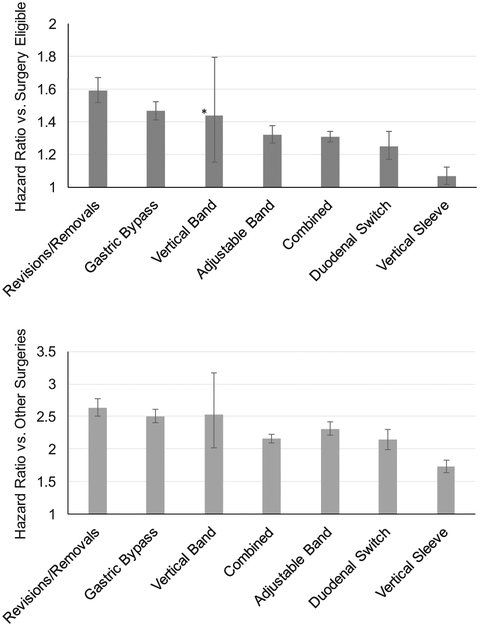
Figure 3 describes the hazard ratios of post-surgical depression stratified by surgery type. Individuals with more than one surgery were classified based on the last annotated surgery present in their record. The individual surgical cohorts are summarized in Supplementary Table 1. Vertical sleeve gastrectomy (VSG) surgical patients (n = 19,852) had significantly lower rates of post-surgical depression compared with the overall population, while Roux-en Y Gastric Bypass (RYGB) surgical patients (n = 18,877) and patients who underwent revision/reversal surgeries (n = 12,319) had significantly higher rates. Other surgical groups included adjustable bands (n = 15,799), vertical bands (n = 506), and duodenal switches (n = 6686). Consistent with the group-level sex-stratified analysis, in every examined surgery type, men had higher hazard ratios than women. In particular, a significant hazard ratio for depression was not observed for female VSG patients relative to female bariatric eligible individuals (Supplementary Figs. 5-8).
Fig. 3.
Procedure-stratified time-to-depression hazard ratios. The error bars represent 95% confidence intervals. Blue bars represent hazard ratios relative to surgery eligible individuals, whereas red bars represent hazard ratios relative to other abdominal surgery patients. The asterisk represents a non-statistically significant hazard ratio. (color figure online)
Table 2 summarizes the results of PheWAS analysis of post-surgical bariatric surgery, split between pre- and post-surgical phenotypes. Phenotypes were only included in these lists if they were not found to have significant associations with depression in surgery eligible and other abdominal surgery cohorts. Post-surgical phenotypes related to infections and surgical complications were significantly associated with depression in the bariatric surgery group but not in the cohort who underwent other abdominal surgeries, implying a specific association with the specific bariatric surgeries undergone by the patients with subsequent depression.
Table 2.
Phenotypes associated with depression in bariatric surgery patients only
| Depression risk ratio |
P-value | |
|---|---|---|
| Pre-surgical phenotype | ||
| Memory loss | 1.997 | 8.11E–08 |
| Chronic airway obstruction | 1.408 | 6.58E–07 |
| Post-surgical phenotype | ||
| Sleep disorders | 2.043 | 1.95E–12 |
| Peritonitis and retroperitoneal infections | 1.783 | 8.42E–10 |
| Post-operative infection | 1.638 | 4.83E–09 |
| Complications of medical procedures NOS | 1.71 | 4.58E–08 |
| Pleurisy; pleural effusion | 1.484 | 4.58E–08 |
| Cellulitis and abscess of trunk | 1.496 | 1.58E–05 |
Phenotypes are grouped by PheWAS code. Depression risk ratio is observed in the bariatric patient cohort. A P-value threshold of 3E–05 was used to account for multiple hypothesis testing
Discussion
We report a robust association between bariatric surgery and subsequent depression. Because the follow-up times in the control cohorts were longer than those in the cases, it is unlikely that the observed association is due to early censoring. This observation is likely an artifact of utilizing insurance claims records: the case group was significantly younger than the controls, and were consequently more likely to experience changes in employment. We, however, note that age was not found to be significant covariate in our analysis. This also implies that the presented risk ratios are conservative, due to the possibility of missed instances of depression among the cases. The observed trends were also found to be robust to the definition of depression used (protracted or not). Two findings suggest that the specific processes and impacts unique to bariatric surgery may be responsible for our observations: (i) non-bariatric abdominal surgery patients have reduced depression risk ratios, likely due to the therapeutic value of the surgery itself, and (ii) laparoscopic bariatric surgeries also have an elevated hazard ratio against depression relative to esophageal/stomach laparoscopic surgery patients. Differential susceptibility toward this effect based on sex was also observed. Despite a higher population incidence of depression among female individuals, the post-surgical effect size was found to be higher among men. Among the subset of patients with pre-surgical BMI measurements, we observed only a very small effect size of BMI with respect to depression risk, implying that our observations are unlikely to be driven by higher BMI measurements in the bariatric surgery group. Previous studies reported more significant effect sizes [19] or a U-shaped relationship [20] between BMI and depression. We hypothesize that the lack of observed effect in our cohort is due to our study design: all patients were eligible for bariatric surgery, and had significantly elevated BMI and baseline depression risk as a result. Therefore, trends observed over a wider BMI range might not be applicable to our cohorts.
A survey of 81 bariatric surgery programs found that only half required formal psychiatric assessment prior to surgery [21]. Our finding that post-surgical depression was less common in patient populations with these screenings reinforce the value of these evaluations even in populations without histories of depression. These screenings may be interpreted as indicators of programs with greater priority on mental health care or stricter patient selection mechanisms.
Based on our control of confounders and the temporal control, we applied to cohort selection, our results lead us to hypothesize a potential causal relationship between the surgery and subsequent depression in a subset of patients, relating to the success and frequency of surgery. Post-surgical phenotypes related to infection and surgical complications were strongly associated with depression among patients undergoing bariatric surgery, and revision/removal surgeries had some of the highest hazard ratios for subsequent depression. Crucially, post-operative surgical complications and infections were only associated with depression in bariatric surgery patients, and not in other abdominal surgery patients. These associations could provide hints at the mechanism and time-scale of post-bariatric surgical depression, such as perturbations of the gut microbiome or disappointment at the outcome of the surgery, though further study would be needed to investigate any of these hypotheses. Previous reports of post-surgical depression often implicated long-term weight loss as a primary factor [6, 22], while our phenotype association data provides evidence for a shorter-term mechanism as well. Similarly, we observe a higher risk of post-surgical depression among RYGB patients relative to other surgeries, which could be attributed to the fact that patients undergoing it typically have more severe baseline conditions [23, 24].
We were able to achieve a significantly higher sample size than comparable clinical studies through our use of clinical insurance records, allowing us to focus on a specific subset of the population (those without histories of depression) and compute comparable placeholder surgery dates for comparisons with non-surgery populations, which emulated a prospective clinical trial and were able to control potential confounders not addressed in previous studies. Furthermore, we were able to utilize matched diagnosis data for our patient population to uncover new phenotypic associations with post-surgical depression.
Our study contains several limitations. First, although we enforced similar inclusion criteria on our cases and controls, based on the inclusion criteria for consideration for bariatric surgery, our cases still had higher pre-surgery claims counts relative to the controls, raising the possibility that they had poorer baseline health. Second, although we removed individuals with pre-existing diagnoses of depression, other comorbid conditions present among the population who received bariatric surgery could contribute to the observations noted. The limited demographic and sociological information present in the insurance claims dataset restricted the pool of covariates that could be controlled or adjusted for in the analysis. Features that we were unable to measure include ethnicity, marital status, and socioeconomic status. Furthermore, the population of individuals with health insurance may not be representative of the population at large. Annotations of procedures and interventions required the presence of billed procedure codes. Discrepancies between procedures billed for and procedures actually carried out, as well as differences between when a procedure occurs and is billed for exist. Finally, we were unable to completely eliminate the possibility that the observed association results from a hypothetical association between the decision to undergo bariatric surgery and subsequent depression, as opposed to the surgery itself.
Conclusions
This study examined the frequency of depression diagnoses after bariatric surgery in individuals without a prior history of depression, relative to both non-surgical and non-bariatric surgery controls. We report an increased risk of depression following bariatric surgery that is amplified in men and reduced in patient cohorts with pre-surgical psychiatric evaluations. Our findings also show that this effect is comparatively larger in patients undergoing gastric bypass, and smaller among patients undergoing vertical sleeve surgeries. Furthermore, we find that this effect is most pronounced in the presence of post-surgical infections or complications, as well as in patients with pre-surgical histories of memory loss or chronic airway obstruction. For patients considering bariatric surgery and their physicians, this research provides a clearer estimate of post-surgical depression risk and associated exacerbating and mitigating factors.
Supplementary Material
Acknowledgements
We thank Aetna Inc. for the data used in this study and Dr. Gabriel Brat for his suggestions on this work. K-HY is a Harvard Data Science Fellow, and WY is supported by NIH Ruth L. Kirschstein National Research Service Award #4TL1TR001101-04 and 5TL1TR001101-05.
Footnotes
Data availability
The data that support the findings of this study are available from Aetna Inc. but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of Aetna Inc.
Conflict of interest The authors declare that they have no conflict of interest.
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information The online version of this article (https://doi.org/10.1038/s41366-019-0364-6) contains supplementary material, which is available to authorized users.
References
- 1.Nguyen NT, Esteban Varela J. Bariatric surgery for obesity and metabolic disorders: state of the art. Nat Publ Gr. 2016. 10.1038/nrgastro.2016.170. [DOI] [PubMed] [Google Scholar]
- 2.Sheets CS, Peat CM, Berg KC, White EK, Bocchieri-Ricciardi L, Chen EY, et al. Post-operative psychosocial predictors of outcome in bariatric surgery. Obes Surg. 2015;25:330–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luppino FS, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–9. [DOI] [PubMed] [Google Scholar]
- 4.Burgmer R, et al. Psychological outcome 4 years after restrictive bariatric surgery. Obes Surg. 2014;24:1670–8. [DOI] [PubMed] [Google Scholar]
- 5.Mitchell JE, et al. Course of depressive symptoms and treatment in the longitudinal assessment of bariatric surgery (LABS-2) study. Obesity. 2014;22:1799–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ivezaj V, Grilo CM. When mood worsens after gastric bypass surgery: characterization of bariatric patients with increases in depressive symptoms following surgery. Obes Surg. 2015;25:423–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rydén A, Torgerson JS. The Swedish Obese Subjects Study-what has been accomplished to date? Surg Obes Relat Dis. 2006;2:549–60. [DOI] [PubMed] [Google Scholar]
- 8.Adams TD, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357:753–61. [DOI] [PubMed] [Google Scholar]
- 9.J-C LR, W TA. Risk of depression and suicide in patients with extreme obesity who seek bariatric surgery. Obes Manage. 2007;3:255–60. [Google Scholar]
- 10.Tindle HA, et al. Risk of suicide after long-term follow-up from bariatric surgery. Am J Med. 2010;123:1036–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hedley AA, et al. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291:2847–50. [DOI] [PubMed] [Google Scholar]
- 12.Denny JC, et al. PheWAS: demonstrating the feasibility of a phenome-wide scan to discover gene-disease associations. Bioinformatics. 2010;26:1205–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.R Development Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. http://www.R-project.org/. [Google Scholar]
- 14.UnitedHealthcare. Bariatric Surgery, Policy Number 2018T0362AA.
- 15.Roberts RE, Kaplan Ga, Shema SJ, Strawbridge WJ. Are the obese at greater risk for depression? Am J Epidemiol. 2000;152:163–70. [DOI] [PubMed] [Google Scholar]
- 16.Panel CDC. Gastrointestinal surgery for severe obesity. Ann Intern Med. 1991;115:956. [PubMed] [Google Scholar]
- 17.Mechanick JI, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient--2013 update. Surg Obes Relat Dis. 2013;9:159–91. [DOI] [PubMed] [Google Scholar]
- 18.Ford DE, Erlinger TP. Depression and C-reactive protein in US adults: data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2004;164:1010–4. [DOI] [PubMed] [Google Scholar]
- 19.Bjerkeset O, Romundstad P, Evans J, Gunnell D. Association of adult body mass index and height with anxiety, depression, and suicide in the general population: the HUNT study. Am J Epidemiol. 2008;167:193–202. [DOI] [PubMed] [Google Scholar]
- 20.De Wit LM, Van Straten A, Van Herten M, Penninx BW, Cuijpers P. Depression and body mass index, a u-shaped association. BMC Public Health. 2009. January 13,9:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bauchowitz AU, et al. Psychosocial evaluation of bariatric surgery candidates: a survey of present practices. Psychosomatic Med. 2005;67:825–32. [DOI] [PubMed] [Google Scholar]
- 22.McGuire MT, Wing RR, Klem ML, Lang W, Hill JO. What predicts weight regain in a group of successful weight losers? J Consult Clin Psychol. 1999;67:177–85. [DOI] [PubMed] [Google Scholar]
- 23.English WJ, et al. American Society for Metabolic and Bariatric Surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. Surg Obes Relat Dis. 2018. 10.1016/j.soard.2017.12.013. [DOI] [PubMed] [Google Scholar]
- 24.Griggs CL, et al. National trends in the use of metabolic and bariatric surgery among pediatric patients with severe obesity. JAMA Pediatr. 2018;172:1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.