Abstract
Distinguishing essential thrombocythemia JAK2V617F from polycythemia vera is difficult because of shared mutation and phenotypic characteristics. The World Health Organization suggested hemoglobin and hematocrit values to diagnose polycythemia vera (PV), but their sensitivity and specificity were not tested. Moreover, red cell values do not accurately predict red cell mass, which we use to discriminate essential thrombocythemia JAK2V617F from PV. Eighty-three PV and 39 essential thrombocythemia JAK2V617F patients were diagnosed based on JAK2V617F positivity, chromium-51 red cell mass, and marrow biopsy findings. Red cell values used to construct a receiver operating characteristic analysis determined optimal thresholds for distinguishing essential thrombocythemia JAK2V617F from PV. Red cell value frequencies were plotted determining if overlap existed. Chromium-51 red cell mass separated PV from essential thrombocythemia JAK2V617F, but red cell values overlapped in 25.0-54.7%. Our data indicate that a significant proportion of PV patients may be underdiagnosed by using only red cell values. A bone marrow biopsy was performed in 199 of 410 (48.5%) and a serum erythropoietin value was measured in 225 of 410 (54.9%) of potential PV patients at our institution. Without isotope studies, marrow biopsies and serum erythropoietin values should improve diagnostic accuracy and become mandatory, but clinical data suggest these tests have not been routinely performed. Therefore, the clinical hematologist must be aware of imperfect accuracy when using only red cell values for distinguishing essential thrombocythemia JAK2V617F from PV.
Introduction
The JAK2V617F and exon 12 mutations are critical for the diagnosis of polycythemia vera (PV); JAK2V617F is also the molecular marker of 50-60% of patients with essential thrombocythemia (ETJAK2V617F).1 Distinguishing these illnesses in their early stages remains a clinical problem because of their shared mutation and phenotypic characteristics.2,3
In clinical situations when the hematocrit (HCT), hemoglobin (HGB), or red blood cell (RBC) count are relatively increased, we distinguish ETJAK2V617F from PV using chromium-51 (Cr-51) labeled RBC and iodine-135 (I135) to measure red cell mass (RCM) and plasma volume, respectively.4 We include the latter to determine if an elevated HCT is attributed to reduced plasma volume when the Cr-51 determined RCM is normal. The distinction of these diagnoses has clinical significance: if a presumptive ETJAK2V617F patient in fact has PV, a significant risk for thrombosis may incur because therapeutic phlebotomy is not performed. Conversely, if a patient is misdiagnosed with PV, inappropriate phlebotomy treatment may cause significant iron deficiency and other related complications.5 In addition, a misdiagnosis may also affect prognostic models comparing ETJAK2V617F with PV, ETCALR, or ETMPL.
The majority of hematology centers worldwide do not use isotope techniques but instead rely on arbitrarily defined World Health Organization (WHO) 2016 HCT and HGB threshold values6 as surrogates for RCM to help diagnose and distinguish these diseases.7 These unconfirmed values were derived from a retrospective study and do not discriminate all cases of ETJAK2V617F from PV.2,7 For this reason, the WHO has advocated marrow biopsy and serum erythropoietin values (SEV), although it is not clear how frequently these tests are actually performed in clinical practices.
Since red cell values in ETJAK2V617F and PV can overlap, a proportion of both diseases may be misdiagnosed. Therefore, we decided to systematically study the sensitivity and specificity of distinguishing ETJAK2V617F with relatively high-normal red blood values from PV in patients when the RCM had been confirmed by isotope studies. Using a newly devised database-querying tool, we also determined the frequency of marrow biopsy and SEV testing, both of which we use at our own intuition.
Methods
The Institutional Review Board of Weill Cornell Medicine (WCM) approved this study. Signed informed consent was obtained in accordance with the Declaration of Helsinki.
The diagnosis of PV in our patients was established according to our previously published criteria which included JAK2V617F positivity, a Cr-51 isotope measured RCM≥125% of expected volume, and a marrow biopsy consistent with PV.4,8 The diagnosis of ETJAK2V617F in our patients was established using JAK2V617F positivity, a Cr-51 isotope measured RCM<125% of expected volume, WHO 2007 criteria,1 and a marrow biopsy consistent with ET.8 ETJAK2V617F patients presenting with “high-normal” blood values (women: HCT>42.0%, HGB>14.0 g/dL; men: HCT>45.0%, HGB>15.0 g/dL) prompted an RCM study and were selected for this review.
We used a bioinformatics tool developed at WCM to search our electronic medical records for patients with an International Classification of Diseases (ICD) 9 or 10 code for PV or ET who had an RCM study performed from 2004-2017.9
Utilizing a receiver operating characteristic (ROC) analysis, we then determined threshold values for HCT, HGB, and RBC to establish limits of specificity and sensitivity. The ROC analysis calculates the optimal combination of sensitivity and specificity thresholds within a range of values to determine which one is the most accurate for diagnosis. We then plotted these ROC-derived threshold values and the frequencies of red cell values obtained at the time of isotope studies to ascertain whether there was any overlap between ETJAK2V617F and PV.
Results
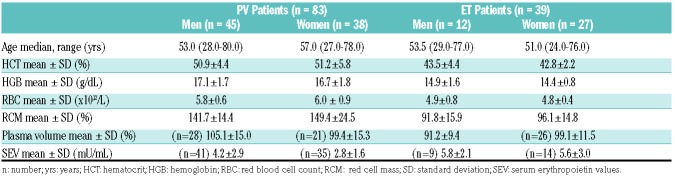
Of 157 patients who had an RCM study performed, 35 were excluded because of JAK2V617F and exon 12 negativity; of the remaining 122 patients, 83 PV and 39 ETJAK2V617F patients met study requirements. Relevant demographic and hematologic data of these patients, including age, HCT, HGB, RBC, RCM, and plasma volume are shown in Table 1. The blood values were recorded at the time of isotope study and prior to any treatment, including phlebotomy. The median age for male and female PV patients was 53.0 (28.0-80.0) and 57.0 (27.0-78.0) years, respectively. The median age for male and female ETJAK2V617F patients was 53.5 (29.0-77.0) and 51.0 (24.0-76.0) years, respectively. For male PV patients, the mean HCT was 50.9±4.4%, the mean HGB 17.1±1.7 g/dL, and the mean RBC count 5.8±0.6x1012/L. For female PV patients, the mean HCT was 51.2±5.8%, the mean HGB 16.7±1.8 g/dL, and the mean RBC count 6.0±0.9x1012/L. For male ETJAK2V617F patients, the mean HCT was 43.5±4.4%, the mean HGB 15.4±1.6 g/dL, and the mean RBC count 4.9±0.8x1012/L. For female ETJAK2V617F patients, the mean HCT was 42.8±2.2%, the mean HGB 14.4±0.8 g/dL, and the mean RBC count 4.8±0.4x1012/L. The mean Cr-51 RCM of all 83 PV patients was 145.3±20.1%, greater than 125% above the expected value and thus establishing polycythemia;4 it was measured in 39 presumptive ETJAK2V617F and it was normal in all of them (mean: 94.8±15.3%). These RCM values show a clear distinction because unlike in red cell values, there was no overlap in values. The mean plasma volume was measured in 49 of 83 PV patients and it was 102.7±15.4%. The mean plasma volume was measured in 38 of 39 ETJAK2V617F patients and was 96.6±11.5%. The difference in plasma volume for all patients with PV and ETJAK2V617F was statistically significant (P=0.04) due to differences for male patients (P=0.01), but not for female patients (P=0.94). In addition, there was a weak correlation between HCT and plasma volume (r=-0.05). The mean serum erythropoietin value (SEV) was measured in 76 of 83 PV patients and was 3.5±2.5 mU/mL. The mean SEV was measured in 23 of 40 ETJAK2V617F patients and was 5.7±2.7 mU/mL.
Table 1.
Demographic and hematologic data of polycythemia vera (PV) and essential thrombocythemia (ETJAK2V617F) patients at diagnosis.
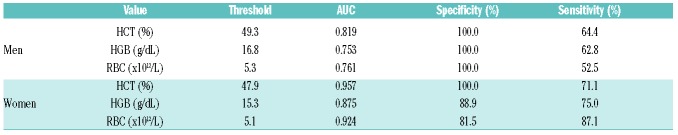
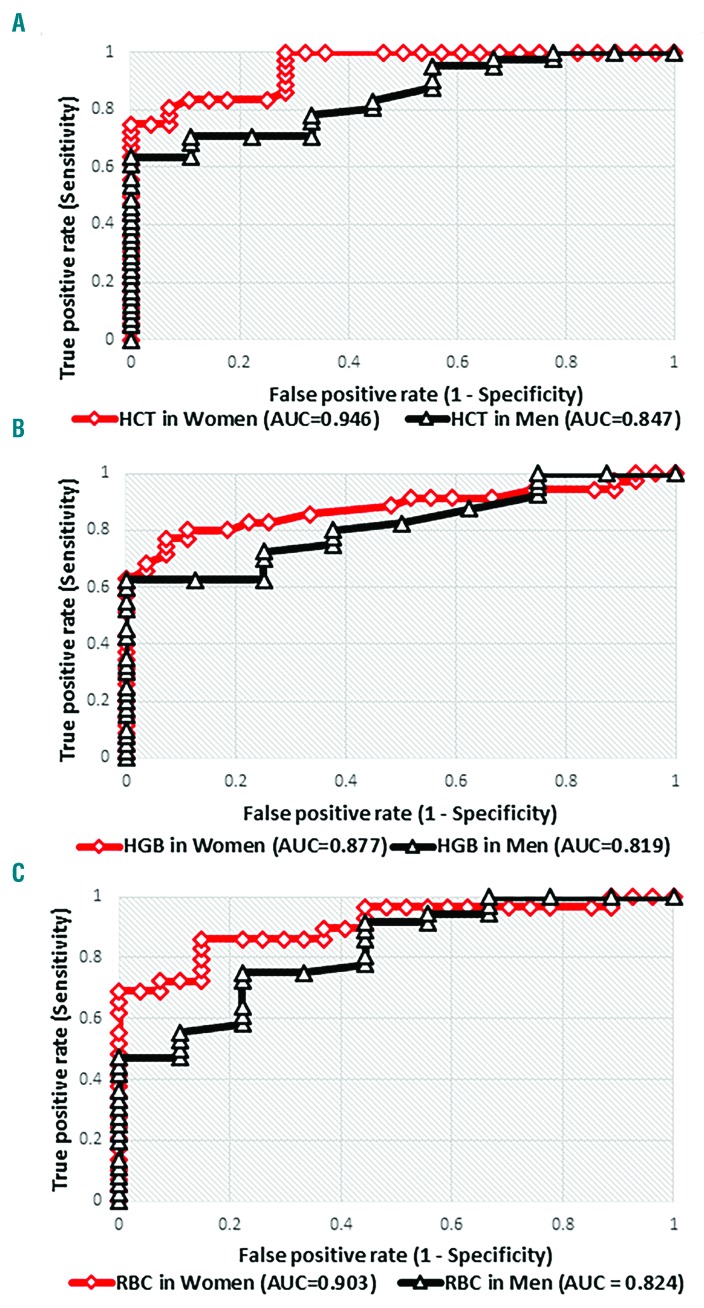
Receiver operating characteristic (ROC) analyses were performed to determine optimal threshold values of HCT, HGB, and RBC to discriminate ETJAK2V617F from PV. The threshold values for distinguishing ETJAK2V617F from PV in men and women, respectively, are HCT: 49.3 and 47.9%, HGB: 16.8 and 15.3 g/dL, and RBC: 5.8 and 5.1x1012/L (Table 2). Figure 1A shows ROC curves for HCT in men and women with ETJAK2V617F and PV; Figure 1B shows this for HGB concentration and Figure 1C shows this for RBC counts. The computer-calculated area under the curve (AUC) measures how well ETJAK2V617F and PV patients are distinguished using HCT, HGB, or RBC. AUC ranges from 0 to 1, inclusive, with 1 representing a perfectly specific and sensitive test. For men, the AUC for HCT is 0.819 (specificity=100.0%, sensitivity=64.4%) indicating that by using this sole criterion, 100.0% of male ETJAK2V617F patients, but only 64.4% of male PV patients, would be correctly diagnosed. For men, the AUC for HGB is 0.753 (specificity=100.0%, sensitivity=62.8%) indicating that 100.0% of male ETJAK2V617F patients, but only 62.8% of male PV patients, would be correctly diagnosed. For men, the AUC for RBC is 0.761 (specificity=100.0%, sensitivity=52.5%) indicating that 100.0% of male ETJAK2V617F and 52.5% of male PV patients would be correctly diagnosed. For women, the AUC for HCT is 0.957 (specificity=100.0%, sensitivity=71.1%), for HGB 0.875 (specificity=88.9%, sensitivity=75.0%), and for RBC 0.924 (specificity=81.5%, sensitivity=87.1%). The implications of these varying specificities and sensitivities are as previously noted above for men.
Table 2.
Threshold values of hematocrit (HCT), hemoglobin (HGB), or red blood cell (RBC) count for men and women with associated area under the curve (AUC), specificity, and sensitivity.
Figure 1.
Receiver operating characteristic (ROC) analysis curves of red cell values in men with polycythemia vera (PV) versus men with essential thrombocythemia (ETJAK2V617F) (triangle markers) and women with PV versus women with ETJAK2V617F (diamond markers). (A) For hematocrit (HCT), (B) for hemoglobin (HGB), and (C) for red blood cells (RBC).
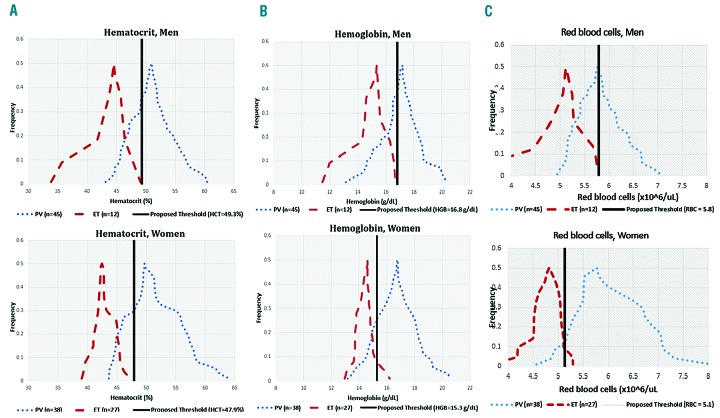
For patients with either ETJAK2V617F or PV, the HCT values overlap in 36.0% of men and 25.0% of women (Figure 2A), the HGB values overlap in 40.0% of men and 54.7% of women (Figure 2B), and the RBC values overlap in 44.0% of men and 35.9% of women (data not shown). In these figures, the threshold values are shown in vertical, solid lines.
Figure 2.
Frequencies of red cell values in men and women with polycythemia vera (PV) (dotted curve) and essential thrombocythemia (ETJAK2V617F) (dashed curve). Proposed thresholds shown in black, vertical line. (A) For hematocrit (HCT), (B) for hemoglobin (HGB), and (C) for red blood cells (RBC).
Querying our outpatient and inpatient electronic medical records with a bioinformatics tool provisioned by WCM showed that of 410 presumptive PV patients, 199 (48.5%) and 225 (54.9%) had a marrow biopsy performed and a SEV measured, respectively.
Discussion
For more than half a century, it has been emphasized that a single HCT or HGB determination cannot be used as a surrogate for RCM.4,10,11 Additional errors in blood count values are compounded by poor techniques of obtaining blood samples and other issues affecting plasma volume. We attempt to minimize these errors by collecting blood samples at the same time of the day insofar as possible and by using a standardized blood collection technique.12 To attain an accurate RCM and plasma volume, we employ a dual isotope technique, using Cr-51 and I135 to measure these values simultaneously. In this study, as expected, the plasma volume was increased in PV.4,10 We have no explanation for the gender differences, but insights may be learned from a larger sample size. The normal RCM and reduced plasma volume found in ETJAK2V617F patients accounted for the increased red cell values at the time of diagnosis.
An insufficient number of matched Cr-51 RCM and marrow results from our patients precluded comparison or correlation, which we plan to carry out as a future study. Discriminating ETJAK2V617F from PV is hierarchal with a dual isotope RCM study remaining the “gold standard”. We recognize that many institutions cannot perform the standard dual isotope technique;13 in this situation, we espouse the use of marrow biopsy, which is now performed in all potential MPN patients at our institution at diagnosis, even in patients with a measured Cr-51 RCM to evaluate baseline fibrosis and cellularity to assess subsequent response to treatment.14 It would be of interest to correlate marrow biopsy and Cr-51 RCM findings in the future. Despite the usefulness of a diagnostic marrow findings, as reported by us and others,4,8 such findings have not been universally accepted15–17 and even the value of marrow examination in general has been questioned.18
Although the SEV is a WHO 2016 minor criterion for the diagnosis of PV,6 we emphasize that approximately 15% of PV patients have a normal SEV (4-27 mU/mL).19,20 This fact and the availability of isotope studies may account for the relatively infrequent use of this test at our institution in the past. However, this laboratory value may be used in combination with abnormal red cell values to distinguish ETJAK2V617F from PV with higher accuracy than using red cell values exclusively.
There are no published data regarding the frequency with which marrow biopsy and SEV are currently performed in patients with PV at diagnosis by general hematologists. We reviewed marrow performance at our institution over the past decade and found that marrow biopsies were performed in 199 of 410 (48.5%) and an SEV was measured in 225 of 410 (54.9%) PV patients. Of those that did not have a marrow biopsy, the majority had been encountered for only a single visit so that a marrow biopsy was not temporally feasible or the patient was advised to have it performed with their primary hematologist.
In the absence of isotope studies and an initial marrow biopsy or SEV, it is important to evaluate the accuracy, as defined statistically, of the HCT, HGB, and RBC threshold values that are advocated to distinguish ETJAK2V617F from PV. We found overlap in HCT, HGB, and RBC values ranging from 25.0-54.7% indicating that a single red cell value will not effectively distinguish ETJAK2V617F from PV.
Such considerations have been overlooked in other studies. For example, it has been suggested that ETJAK2V617F patients are at higher risk for thrombosis than those with a CALR mutation.21 However, those patients diagnosed with ETJAK2V617F had a median SEV of 4.7 mU/mL (range: 0-47 mU/mL) compared with CALR+ ET patients who had a median SEV of 9.4 mU/mL (range: 1.2-27 mU/mL). An unspecified number of ETJAK2V617F patients had a SEV below normal (i.e. <4 mU/mL)22 suggesting the possibility of PV. Since neither all red cell values, isotope studies, nor systematic marrow biopsies were reported, some of these ETJAK2V617F patients might have, in fact, had a higher risk of thrombotic events because they actually had PV.23 Thus, they were incorrectly assigned to a disease with a decreased expected survival.24 Of course, these issues do not occur in JAK2V617F wild-type, CALR+, or MPL+ patients because these mutations, with very rare exceptions, do not occur in PV.18
It is of interest that our threshold values are coincidentally similar to the WHO 2016 criteria,6 which did not address the important topic of imperfect specificity and sensitivity. Although marrow biopsy and SEV are advantageous for distinguishing ETJAK2V617F from PV, it is unclear how frequently these examinations are being performed in actual clinical practice. Our data support their use even despite the discussed limitations. In the absence of resolving these discrepancies, isotope RCM studies remain the gold standard for discriminating ETJAK2V617F from PV.
In summary, the clinical hematologist must be warned of the varying specificity and sensitivity and the considerable limitations of discriminating ETJAK2V617F from PV solely when using red cell values, and the importance of isotope, marrow, and SEV studies as outlined by WHO 2016 criteria.6 It remains undetermined how frequently any of these tests are performed in clinical practice.
Acknowledgments
We thank Dr. Paul Christos for statistical review. He was partially supported by the Clinical and Translational Science Center, Weill Cornell Medical College (UL1-TR000457-06).
Footnotes
Check the online version for the most updated information on this article, online supplements, and information on authorship & disclosures: www.haematologica.org/content/104/11/2200
Funding
This study was supported in part by the William and Judy Higgins Trust and the Johns Family Foundation of the Cancer Research and Treatment Fund Inc., New York, NY, USA.
References
- 1.Tefferi A, Thiele J, Orazi A, et al. Proposals and rationale for revision of the World Health Organization diagnostic criteria for polycythemia vera, essential thrombocythemia, and primary myelofibrosis: recommendations from an ad hoc international expert panel. Blood. 2007;110(4):1092–1097. [DOI] [PubMed] [Google Scholar]
- 2.Barbui T, Thiele J, Kvasnicka HM, Carobbio A, Vannucchi AM, Tefferi A. Essential thrombocythemia with high hemoglobin levels according to the revised WHO classification. Leukemia. 2014: 28(10):2092–2094. [DOI] [PubMed] [Google Scholar]
- 3.Spivak JL. Myeloproliferative Neoplasms. N Engl J Med. 2017;377(9):895–896. [DOI] [PubMed] [Google Scholar]
- 4.Silver RT, Chow W, Orazi A, Arles SP, Goldsmith SJ. Evaluation of WHO Criteria for Diagnosis of Polycythemia Vera: A Prospective Analysis. Blood. 2013; 22(11):1881–1886. [DOI] [PubMed] [Google Scholar]
- 5.Silver RT, Kiladjian JJ, Hasselbalch HC. Interferon and the treatment of polycythemia vera, essential thrombocythemia and myelofibrosis. Exp Rev Hematol. 2013;6(1):49–58. [DOI] [PubMed] [Google Scholar]
- 6.Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–2405. [DOI] [PubMed] [Google Scholar]
- 7.Barbui T, Thiele J, Gisslinger H, et al. Masked polycythemia vera (mPV): Results of an international study. Am J Hematol. 2014;89(1):52–54. [DOI] [PubMed] [Google Scholar]
- 8.Kvasnicka HM, Orazi A, Thiele J, Barosi G, Bueso-Ramos CE, Vannucchi AM. European LeukemiaNet study on the reproducibility of bone marrow features in masked polycythemia vera and differentia tion from essential thrombocythemia. Am J Hematol. 2017;92(1):1062–1067. [DOI] [PubMed] [Google Scholar]
- 9.Overhage JM, Ryan PB, Reich CG, Hartzema AG, Stang PE. Validation of a common data model for active safety surveillance research. J Am Med Inform Assoc. 2012;19(1):54–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alvarez-Larran A, Ancochea A, Angona A, et al. Red cell mass measurement in patients with clinically suspected diagnosis of polycythemia vera or essential thrombocythemia. Haematologica. 2012; 97(11): 1704–1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johansson PL, Safai-Kutti S, Kutti J. An elevated haemoglobin concentration cannot be used as a surrogate marker for absolute erythrocytosis: a study of patients with polcythaemia vera and appartent polycythaemia. Br J Haematol. 2005;129(5):701–705. [DOI] [PubMed] [Google Scholar]
- 12.Silver RT, Gjoni S. The hematocrit value in polycythemia vera: caveat utilitor. Leuk Lymphoma. 2015;56(6):1540–1541. [DOI] [PubMed] [Google Scholar]
- 13.Margolskee E, Orazi A, Krichevsky S, Silver RT. Evaluation of bone marrow morphology is essential for assessing disease status in interferon-treated polycythemia vera patients. Haematologica. 2017;102(3):e97–e99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alvarez-Larran A, Ancochea A, Garcia M, et al. WHO-histological criteria for myeloproliferative neoplasms: reproducibility, diagnostic accuracy and correlation with gene mutations and clinical outcomes. Br J Haematol. 2014;166(6):911–919. [DOI] [PubMed] [Google Scholar]
- 15.Ellis JT, Silver RT, Coleman M, Geller SA. The bone marrow in polycythemia vera. Semin Hematol. 1975;12(4):433–444. [PubMed] [Google Scholar]
- 16.Wilkins BS, Erber WN, Bareford D, et al. Bone marrow pathology in essential thrombocythemia: interobserver reliability and utility for identifying disease subtypes. Blood. 2008:111(1):60–70. [DOI] [PubMed] [Google Scholar]
- 17.Spivak J. Polycythemia Vera. Curr Treat Options Oncol. 2018;19(2):12. [DOI] [PubMed] [Google Scholar]
- 18.Silver RT, Krichevsky S, Cross NCP. Evaluation of serum erythropoietin values as defined by 2016 World Health Organization criteria for the diagnosis of polycythemia vera. Leuk Lymphoma. 2017;58(11):2768–2769. [DOI] [PubMed] [Google Scholar]
- 19.Ancochea A, Alvarez-Larran A, Morales-Indiano C, et al. The role of serum erythropoietin level and JAK2 v617f allele burden in the diagnosis of polycythemia vera. Br J Haematol. 2014;167(3):411–417. [DOI] [PubMed] [Google Scholar]
- 20.Rumi E, Pietra D, Ferretti V, et al. JAK2 or CALR mutation status defines subtypes of essential thrombocythemia with substantially different clinical course and outcomes. Blood. 2014;123(10):1544–1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.“Laboratory Testing Information-Erythropoietin.” RSS 20 In Focus. ARUP Laboratories, Web. 28 Feb. 2013 http://www.aruplab.com/guides/ug/tests/0050227.jsp>. [Google Scholar]
- 22.Price GL, Davis KL, Karve S, Pohl G, Walgren RA. Survival Patterns in United States (US) Medicare Enrollees with Non-CML Myeloproliferative Neoplasms (MPN). PLoS One. 2014;9(3):e90299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Michiels JJ, Medinger M, Raeve HD, et al. Increased erythrocyte count on top of bone marrow histology but not serum EPO level or JAK2 mutation load discriminates between JAK2V617F mutated essential thrombocythemia and polycythemia vera. J Hematol Thromb Dis. 3:S1–001. [Google Scholar]
- 24.Pearson TC, Guthrie DL, Simpson J, et al. Interpretation of measured red cell mass and plasma volume in adults: Expert Panel on Radionuclides of the International Council for Standardization in Haematology. Br J Hematol. 1995;89(4): 745–756. [DOI] [PubMed] [Google Scholar]