Abstract
Urinary tract infection (UTI) is one of the most common bacterial infections in infants less than age 1 year. UTIs frequently recur and result in long-term effects include sepsis and renal scarring. Uropathogenic Escherichia coli (UPEC), the most prevalent organism found in UTIs, can cause host inflammation via various virulence factors including hemolysin and cytotoxic necrotizing factors by inducing inflammatory cytokines such as interleukin (IL)-1β. However, the ability of each UPEC organism to induce IL-1β production may differ by strain. Furthermore, the correlation between differential IL-1β induction and its relevance in pathology has not been well studied. In this study, we isolated UPEC from children under age 24 months and infected bone-marrow derived macrophages with the isolates to investigate secretion of IL-1β. We found that children with higher concentrations of C-reactive protein (CRP) were more likely to harbor phylotype B2 UPEC strains that induced more IL-1β production than phylotype D. We also observed a significant correlation between serum CRP level and in vitro IL-1β induction by phylotype B2 UPEC bacteria. Our results highlight the diversity of UPEC in terms of IL-1β induction capacity in macrophages and suggest a potential pathogenic role in UTIs by inducing inflammation in infants.
Subject terms: Infectious-disease epidemiology, Bacteriology, Urinary tract infection
Introduction
Urinary tract infection (UTI) is one of the most common bacterial infections and occurs in approximately 150 million people a year1. Infants under age 1 year are more susceptible to UTIs. In general, UTIs are more common in girls, although before age 1 year boys have more UTIs than girls2. A previous study found that 18% of infants under age 12 months who experience UTIs have recurrences within a few months3. Moreover, depending on when a UTI is diagnosed and treated after occurrence, the outcome may include sepsis, renal scarring, and hypertension4.
Among bacteria that can lead to UTI, uropathogenic Escherichia coli (UPEC) is the most common and is found in 80~90% of UTI patients1. As the urinary tract is a harsh environment for bacteria due to continuous flow of urine, UPECs can replicate in the form of intracellular bacterial communities (IBCs) as a strategy to survive5. Various virulence factors such as fimbriae/adhesins, pore-forming toxins, and iron-uptake molecules contribute to this survival strategy6. UPEC make use of fimbriae and adhesins, including type 1 fimbriae, P fimbriae, and Afa adhesins, to adhere to host cell surfaces7,8 while pore-forming toxins such as cytotoxic necrotizing factors (CNF) and hemolysin of UPEC can make pores in host cell membranes for invasion9,10.
Inflammation often accompanies UTIs and is associated with renal scarring and disease severity11. Several cytokines, including TNF-α, interleukin (IL)−1β, IL-6, and IL-8, are involved in the inflammation that accompanies UTIs12. IL-1β, which is often detected in serum samples of children with UTIs, has been used as a marker for acute pyelonephritis13. IL-1β is primarily secreted by monocytes and macrophages. It induces tissue damage and infiltration of neutrophils. To avoid uncontrolled inflammation, secretion of the active-form of IL-1β is tightly regulated and modulated by a molecular complex called inflammasome14. Several UPEC virulence factors can activate inflammasome and directly influence IL-1β secretion. Pore-forming toxin, especially hemolysin, is known to induce IL-1β secretion and cell death in bladder tissue15. Hemolysin of Proteus mirabilis and group B Streptococcus can also induce IL-1β secretion via NLRP3 inflammasome and enhance inflammation16,17. In UTI and meningitis animal models, E. coli CNF exacerbates inflammation18,19. CNF can synergistically promote IL-1β secretion with lipopolysaccharide in a caspase-1/caspase-11-dependent manner20.
Macrophages in the urinary tract have various roles in host defense against invading UPEC. At an early infection time point, the absence of macrophage results in a higher bacterial burden and alteration of innate immune signaling21. Macrophages in urinary tissue can recruit neutrophils to the uroepithelium during UPEC infection and depletion of these tissue macrophages results in ablation of neutrophil migration and bacteria clearance22. Moreover, there is evidence that some UPEC strains can directly infect macrophages, reside in intracellular vesicles, and make IBCs23,24. Invasion of macrophages by UPEC can result in prolonged survival of UPEC and recurrent infection25. From these results, we can consider macrophages in the urinary tract to be both sensor and reservoir of UPEC.
Much research about inflammation in UTI has focused on host responses at the tissue level or interactions between UPEC and epithelial cells26–28. However, myeloid cells recruited to the site of infection also play an immediate role in innate immune responses21,29. Macrophages are not only target cells for primary UPEC infection but they also play key roles in inflammatory response23. Inflammation is considered a double-edged sword in many diseases because it is essential for controlling infection while it is hazardous to the host when exacerbated in the acute phase30–32. To investigate the relationship between different characteristics of UPEC and a patient’s inflammatory responses, we recruited patients under age 24 months and measured serum C-reactive protein (CRP) concentration, which is known to rise in response to inflammation. We chose this age group because infants are highly susceptible to severe progression including renal scarring upon UTI33. In parallel, we isolated UPEC strains from child patients to analyzed phylotype, virulence gene expression, and IL-1β induction potential. Integrative analyses were made from a data series obtained from patient’s blood and UPEC isolates.
Results
Subject characteristics
We analyzed 40 E. coli isolates from individual children. The median age of the participants was 4.7 months (range, 0.4–16.7) and 27% (11/40) were girls. The mean white blood cell (WBC) count of these patients was 15,279/mm³. All had fever ≥38 °C, pyuria, and E. coli identified in urine cultures. Mean CRP levels were 44.5 mg/L (range, 0.9–189.5). Twenty-two children had CRP levels ≥30 mg/L. A DMSA (dimercaptosuccinic acid) scan showed cortical defects in 8 of the 40 patients. Children with CRP levels ≥30 mg/L were more likely to have defects shown by DMSA (36.3% vs. 0%, p = 0.005). Vesicoureteral reflux (VUR) was found in 5 of 23 patients who underwent a voiding cystourethrogram (VCUG). Ultrasonography (USG) revealed 5 patients with hydronephrosis, 9 with cystitis, and 2 with acute pyelonephritis (Table 1).
Table 1.
Characteristics of study population with urinary tract infections.
| CRP < 30 (n = 18) | CRP ≥ 30 (n = 22) | All (n = 40) | p-value | |
|---|---|---|---|---|
| Median age, mo (Max-Min) | 3.7 (0.5–7.9) | 5.5 (0.4–18.0) | 4.7 (0.4–18.0) | 0.004 |
| Girls, n (%) | 6 (33.3) | 5 (22.7) | 11 (27.5) | 0.498 |
| WBC, /mm³ (Max-Min) | 13927 (4470–24580) | 16438 (7610–25090) | 15279 (4470–25090) | 0.235 |
| CRP, mg/L (Max-Min) | 12.5 (0.9–29.4) | 70.7 (32.8–189.5) | 44.5 (0.9–189.5) | 0.000 |
| Cortical defect in DMSA, n (%) | 0/18 (0.0) | 8/22 (36.3) | 8/40 (20.0) | 0.005 |
| VUR, n (%) | 2/13 (15.5%) | 3/10 (30.0) | 5/23 (21.7) | 0.39 |
| Abnormal findings on sonography | ||||
| Hydro, n | 2/18 | 3/20 | 5/38 | 1.00 |
| APN, n | 2/18 | 0/20 | 2/38 | 0.21 |
| Cystitis, n | 4/18 | 5/20 | 9/38 | 1.00 |
Note: APN, acute pyelonephritis; CRP, C-reactive protein; DMSA, dimercaptosuccinic acid; Hydro, hydronephrosis D; Max, maximum; Min, minimum; VUR, vesicoureteral reflux; WBC, white blood cells.
Phylotype and pathotypic distribution of UPEC isolates
All isolates were identified as E. coli by phoA gene-specific amplification (Supplementary Table 1). Confirmed strains were used to infect bone marrow-derived macrophage (BMDM) for further studies, including phylotypic and pathotypic analysis. When phylotyping was performed34, among 40 isolates, 28 (70%) were group B2 E. coli while 12 (30%) were group D. No group A or B1 strains were isolated (Table 2).
Table 2.
Phylotypic and virulence gene distribution of UTI bacteria in 40 children.
| Distribution of virulence genes | Phylogenetic group | Total (n = 40), % | |
|---|---|---|---|
| Group B2 (n = 28), % | Group D (n = 12), % | ||
| papC | 18 (64.3) | 7 (58.3) | 25 (62.5) |
| sfa/foc (sfa) | 6 (21.4) | — | 6 (15) |
| afaC | 6 (21.4) | 1 (8.3) | 7 (17.5) |
| fimH | 20 (71.4) | 11 (91.7) | 31 (77.5) |
| cnf | 3 (10.7) | — | 3 (7.5) |
| hly | 4 (14.3) | — | 4 (10) |
| aer | 15 (53.6) | 10 (83.3) | 25 (62.5) |
Note: No Group A or B1 genes were found.
To determine pathotypic characteristics of UPEC isolates, we investigated the presence of seven virulence genes by polymerase chain reaction (PCR). Of these, papC were found in 25 (62.5%), sfa/focDE in 6 (15%), afaC in 7 (17.5%), fimH in 31 (44.5%), cnf in 3 (7.5%), hlyCA in 4 (10%), and iucC in 25 (62.5%). All virulence genes were more prevalent in group B2 E. coli. Six of 7 afaC-positive strains were group B2 while sfa/focDE, cnf, hlyCA genes were only detected from group B2 (Table 2).
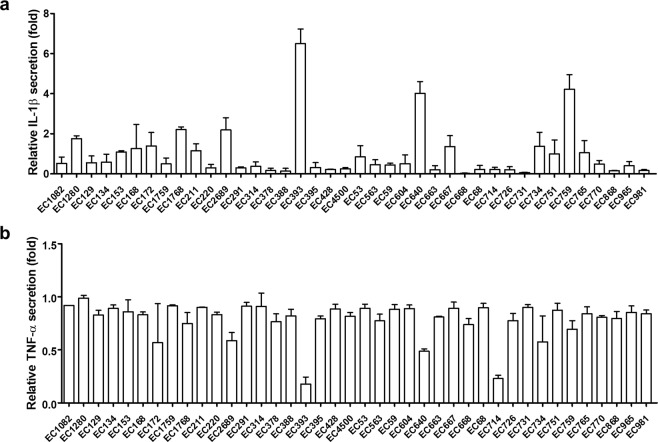
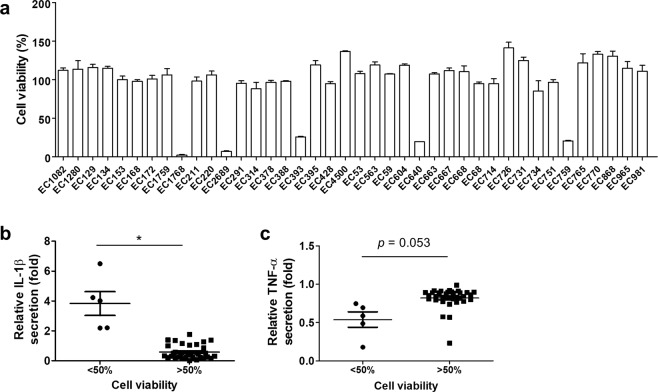
Cytokine secretion profile and viability of BMDM upon infection of UPEC strains
To examine cytokine secretion by BMDM co-cultured with UPEC isolates, we performed ELISA on culture medium 12 h after stimulation. Because P. mirabilis can efficiently induce IL-1β and TNF-α production in BMDM17, we used this strain as a positive control. Among 40 isolates, 5 exhibited more than two-fold higher IL-1β secretion than P. mirabilis (Fig. 1a). In many instances, TNF-α levels did not differ significantly among isolates. However, three strains were reduced by more than half compared with P. mirabilis (Fig. 1b). IL-1β can induce pyroptosis, a type of cell death that results in membrane rupture and release of inflammatory components35. Therefore, we investigated cell viability of infected BMDMs to examine cell death (Fig. 2a). Co-culture of BMDM with five isolates resulted in reduced cell viability. When we assessed the correlation between cytokine production and cell viability, the top five IL-1β-secreting isolates had obvious reduction (p = 0.015) in cell viability (Fig. 2b). These five strains also showed reduced production of TNF-α (Fig. 1a,b). However, the correlation between TNF-α and cell viability did not reach statistical significance (Fig. 2c). These data suggest that UPEC strains with more cytotoxicity can induce more IL-1β secretion in vitro.
Figure 1.
UPEC isolates induce IL-1β from BMDM at different levels. BMDMs were co-cultured with UPEC isolates for 12 h. Levels of (a) IL-1β and (b) TNF-α in culture supernatants were measured. Amounts of cytokines induced by UPEC isolates were normalized against cytokines produced by P. mirabilis stimulation. Values represent mean ± SD from six samples from two separate experiments.
Figure 2.
Cytotoxic UPEC induces higher IL-1β and lower TNF-α levels than other UPEC strains. (a) BMDMs were co-cultured with UPEC isolates for 12 h and cell viability was measured. Isolates were divided into lower and higher viability groups (<50% and >50%, respectively) and their induced secretion of (b) IL-1β and (c) TNF-α from BMDM after co-culture was compared. Cytokine levels were normalized against those of a P. mirabilis stimulated group. Each dot represents a mean of six samples from two independent experiments. *p < 0.05.
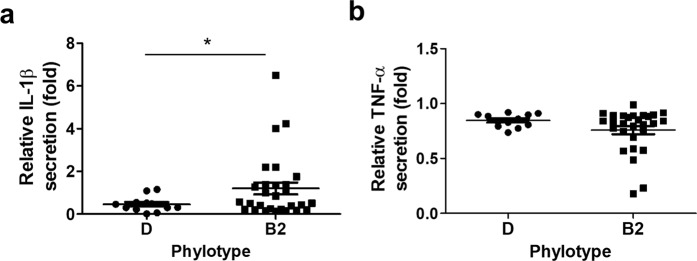
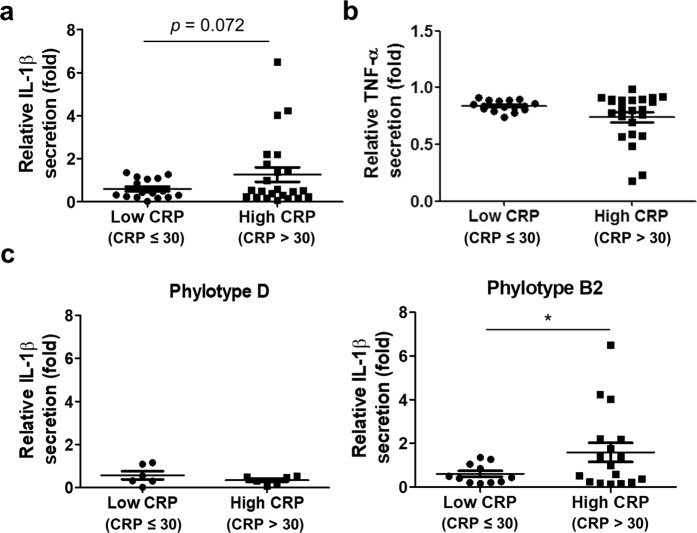
Group B2 UPEC is associated with IL-1β induction in vitro and patient’s serum CRP level
We then sought to determine which UPEC group might be more associated with IL-1β induction. We also tried to determine the relationship between IL-1β induction potential and patient inflammatory status using the serum CRP level. When the amount of IL-1β secreted by UPEC-treated BMDM was compared between groups B2 and D, group B2 induced significantly more IL-1β secretion (p = 0.018) than group D (Fig. 3a). However, we could not detect any significant difference in TNF-α secretion (Fig. 3b). We then divided patients into “high” and “low” inflammation groups (CRP > 30 and <30 mg/L, respectively). UPEC isolates from the high inflammation group induced more IL-1β secretion in vitro (Fig. 4a; not statistically significant). Likewise, we found no significant correlation between TNF-α secretion and CRP level (Fig. 4b). We then further analyzed IL-1β secretion between UPECs isolated from the high and low CRP groups after subdividing patients by phylotype. The group B2 UPECs from patients in the high CRP group had significantly more IL-1β induction (p = 0.045); however, there was no significant difference in group D UPECs from high and low CRP patients (Fig. 4c). These data suggest that some group B2 UPEC, but not group D UPEC, can augment inflammation, probably by enhancing IL-1β induction during infection.
Figure 3.
Group B2 UPECs are more likely to induce IL-1β from BMDM than are group D UPECs. Phylotypes of UPEC isolates were determined. (a) IL-1β and (b) TNF-α induction data were re-grouped and analyzed based on phylotypes. Each dot represents a mean of six samples from two independent experiments. *p < 0.05.
Figure 4.
IL-1β induction by group B2 UPEC strains is correlated with patient serum CRP level. (a) IL-1β and (b) TNF-α induction levels by UPEC isolates were grouped by patient CRP values. (c) Two CRP groups were subdivided by phylotype to compare IL-1β induction by UPEC isolates. Each dot represents a mean of six samples pooled from two independent experiments. *p < 0.05.
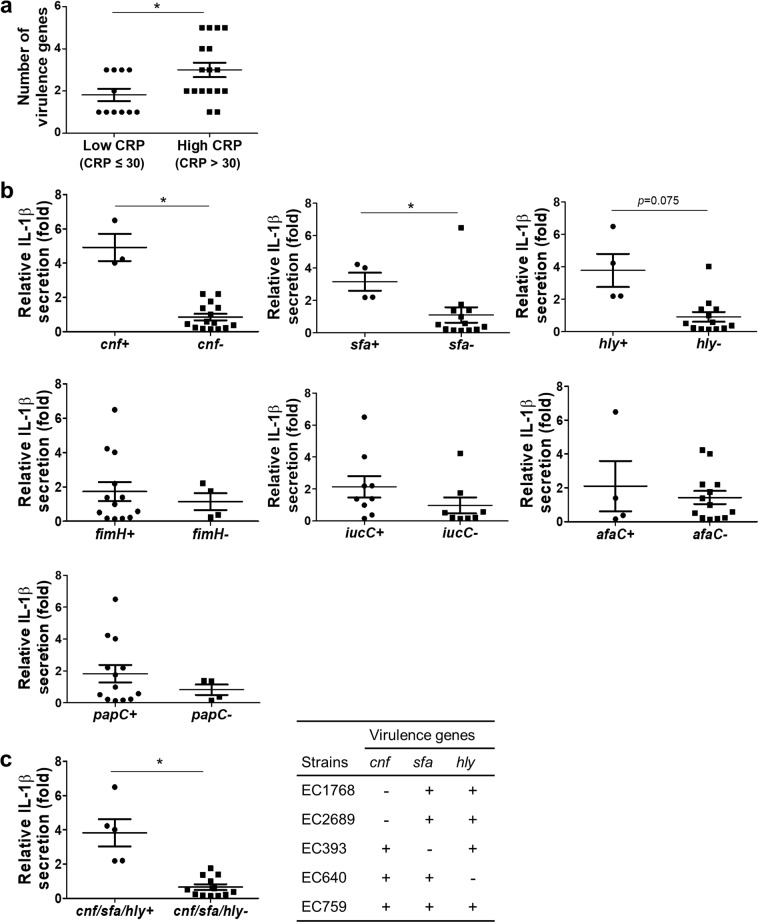
Selective virulence genes are involved in IL-1β induction by group B2 UPEC
It is clear that group B2 UPECs have greater ability to induce IL-1β in macrophages than group D UPECs. However, the amount of IL-1β secretion varied within group B2 (Fig. 4c). We hypothesized that genetic differences in this group might be linked to the observed variation and performed experiments to detect virulence genes from group B2 UPEC isolates. We tested the presence of seven virulence genes by PCR and counted the number of positive genes for each isolate. When group B2 UPECs were divided into high (CRP > 30 mg/L) and low inflammation groups, more virulence genes were detected (p = 0.015) in the patients with high CRP levels (Fig. 5a). To further define the virulence gene directly involved in IL-1β induction, we divided UPEC isolates from patients with CRP >30 mg/L based on the presence of each virulence gene and compared in vitro IL-1β secretion. Statistical analysis revealed that five isolates (EC1768, EC2689, EC393, EC640, EC759) that possessed at least one cnf (p = 0.038), hlyCA (p = 0.075), or sfa/focDE (p = 0.026) gene induced higher IL-1β secretion than the other isolates (Fig. 5b). However, the presence of the afaC, fimH, iucC, or papC genes did not significantly affect the amount of IL-1β secreted by macrophages (Fig. 5b). Of note, all five isolates were dual or triple positive for cnf, hlyCA, and sfa/focDE genes. In addition, they induced significantly higher levels of IL-1β secretion (p = 0.017) than the other isolates (Fig. 5c). Overall, our data suggest that patients infected with group B2 UPECs that express hemolysin (hly), cytotoxic necrotizing factor (cnf), S fimbrial adhesion (sfa), and F1C fimbriae (foc) have stronger inflammatory potential.
Figure 5.
Multiple virulence genes in group B2 UPEC contribute to IL-1β induction in BMDM. (a) Virulence gene numbers of UPEC isolates were grouped based on serum CRP level. (b) Seven virulence genes were examined in UPECs isolated from patients with serum CRP concentration >30 mg/L (high CRP). (c) Strains that possessed hlyCA, cnf, and sfa/focDE were grouped and compared with other isolates from the high CRP group (CRP > 30 mg/L) for IL-1β induction. Each dot represents a mean of six samples from two independent experiments. *p < 0.05.
Discussion
Previous research mainly investigated the correlation between cytokine profile and clinical findings, including CRP to assess the contribution of inflammatory components (i.e., inflammatory cytokines) during UTI pathogenesis36–38. Although UPECs are the most frequent causative agents of UTI and therefore closely related to disease outcome, most studies did not examine the genetic characteristics of UPECs to link their viral properties with the host’s inflammatory responses. We believe our study is the first to identify genes associated with IL-1β induction in UPECs isolated from young children with UTIs (age < 24 months) and to phylotypically characterize genetic correlation with each child’s serum CRP level. E. coli strains belonging to groups B2 and D are considered to be more pathogenic34,39. Group B2 UPECs are known to more prevalent than group D UPECs in different age groups and harbor virulence genes including hlyCA, cnf, and sfa/focDE39–42. These virulence genes were exclusively found in group B2 isolates in our study. Our data suggest that phylotypic distribution and pathotypic characteristics of UPEC isolated from Korean patients are similar to those of previous reports39–42.
We also pathotyped DH5α, a non-pathogenic group A E. coil strain that is commonly used in the laboratory (data not shown). Although DH5α contained fimH, it failed to induce IL-1β production by BMDM. However, similar levels of TNF-α were detected upon stimulation, comparable to that of TNF-α induced by group B2 UPEC isolates (data not shown). Consistent with a previous report17, IL-1β induction in macrophages was more selective and virulence factor-dependent compared to TNF-α induction. IL-1β, but not TNF-α, showed significant correlation with patient CRP levels. Thus, increased inflammation by group B2 UPEC might be partially attributed to virulence genes related to IL-1β.
Production of IL-1β via caspase-1 signaling can induce a unique type of cell death called ‘pyroptosis’43. Pyroptosis can stimulate exfoliation of epithelial cells in urinary tract tissue and possibly give UPECs a chance to reach the inner part of the urothelial layer44. During in vitro stimulation of BMDM by a UPEC isolate, IL-1β production induces pyroptosis, which may lead to reduced cell survival. Indeed, BMDM treated with group B2 UPEC isolates that expressed hlyCA, cnf, and sfa/focDE genes showed markedly reduced cell survival. Generally, severe UTI results in overall elevation of inflammatory cytokines12,28. However, we observed reduced TNF-α production by BMDM in response to UPECs that induced higher levels of IL-1β. This was probably due to rapid cell death by pyroptosis of BMDM, limiting TNF-α accumulation in culture medium.
Results of our study suggest that UPECs harboring multiple IL-1β-inducible genes are more inflammatory and pathogenic. Three specific genes (i.e., hlyCA, cnf, sfa/focDE) were found in the five most IL-1β-inducible strains. Many previous studies have shown the important role of hemolysin and CNF in IL-1β secretion by macrophages upon infection via pathways that include activation of Rho GTPase, NF-κB, inflammasomes, and pyroptosis20,45–48. Hemolysin encoded by various organisms is well known to activate NLRP3 inflammasome to produce the active form of IL-1β49. However, we could not rule out other virulence genes associated with IL-1β induction because minor differences were observed in IL-1β levels from the other 35 UPEC isolates.
We also found that S and F1C fimbriae were associated with IL-1β induction by macrophages. S and F1C fimbriae are known to recognize and bind to sialic acid moieties or gangliotriaosylceramide present on the cell surface of macrophages50–52. Bacterial interaction with the urinary tract is an important step to colonization in the bladder. Such interaction is mediated by different types of fimbriae53. Some studies have highlighted a pro-inflammatory role of fimbriae27,54. Further study is needed to determine the role of S and F1C fimbriae in inflammatory modulation.
Collection bag specimen urine is associated with higher contamination than clean-catch urine or catheter specimen urine55. The specimens used in this study were collected between 2010 and 2014 before our laboratory discontinued this practice in 201656. Therefore, some samples were collected with sterile and sealed urine collection bags from febrile infants. Because collection bags have increased contamination risk, the samples used in this study all had a single uropathogenic organism isolated with a colony-forming unit (cfu) count >100,000. We believe this selection criteria helped us to exclude contaminated specimens.
Overall, our results indicate that group B2 UPECs have a greater potential to induce IL-1β. Our data also suggest that IL-1β-inducible genes may play a significant role in the pathogenesis of UTI. However, some patients with group B2 or group D UPECs without noticeable induction of IL-1β in vitro also had CRP levels of >30 mg/L. Moreover, many E. coli in urinary organs are avirulent57. Thus, we suggest that virulence genes need to be examined in addition to detection of bacteria. As multiple virulence factors may synergistically affect disease prognosis, we cannot easily define which virulence factors are important for the pathogenesis of UTI58,59. Further studies are required to understand the relationship between underlying mechanisms and the interactions of multiple viral pathways.
Methods
Mice
Six- to ten-week-old female WT C57BL/6 (B6) mice were bred and kept under specific pathogen-free conditions in the animal facility of Wide River Institute of Immunology, Seoul National University College of Medicine (Hongcheon, Korea). Animal studies were conducted under protocols approved by the Seoul National University Institutional Animal Care and Use Committee (approval No. SNU-180108-2). All experiments were performed in accordance with relevant guidelines and regulations.
Subjects and bacterial strains
P. mirabilis was kindly provided by Dr. Harry Mobley, University of Michigan, Ann Arbor, USA. E. coli strains were isolated from patient urine samples and susceptibility to antimicrobials was tested by Vitek-2 system (BioMérieux, Durham, NC, USA). The clinical samples were then collected and banked at Gyeongsang National University Hospital Branch of the National Culture Collection for Pathogens (GNUH-NCCP, Jinju, Korea). The GNUH Institutional Review Board approved this study (2018-09-012). We retrospectively analyzed data for the 40 pediatric patients under age 24 months with febrile UTI. All had been admitted to Gyeongsang National University Hospital between January 2010 and December 2014. The criteria for diagnosis of a first-time febrile UTI for inclusion in this study have been described60. In brief, each child had the following findings: (1) temperature ≥ 38 °C, (2) pyuria (≥5 WBC/high-power field), (3) bacteria-positive urine culture, and (4) no previous history of UTI, kidney, or bladder disease. Renal USG, VCUG, or DMSA scan were used for patient evaluation. Clinical data including age, gender, and WBC counts were recorded. Peripheral venous blood was collected to measure CRP levels by the latex-enhanced turbidimetric assay method (cobas 8000 analyzer; Roche, Indianapolis, IN, USA). Urinary examinations were performed at hospital admission before antibiotic administration or fluid therapies. UTI, USG, and DMSA scan data were collected within 5 days of hospitalization, and VCUG was performed within 4 weeks following antibiotics therapy. The 40 non-duplicate E. coli isolates studied were obtained from the GNUH-NCCP and the E. coli was identified using PCR with primers specific for E. coli alkaline phosphatase gene61. Bacteria count was determined by CFU assay on Luria-Bertani (LB) agar plates; optical density (OD) was measured by Epoch spectrophotometer (Bio-Tek, Winooski, VT, USA).
Bacterial DNA extraction
E. coli strains were grown in Müller’s LB broth (BD Difco, Franklin Lakes, NJ, USA) at 37 °C for 18 h. DNA extraction was performed by optimized heat shock method. Bacteria were pelleted from 200 μl of broth, suspended in 200 μl of sterile distilled water, and incubated at 95 °C for 5 min followed by 10 min on ice and centrifugation. We stored 150 μl of the supernatant at −20 °C as a template DNA stock.
Identification of phylotype and virulence gene distribution by PCR
Specific primers were used to amplify phoA61, chuA, yjaC, and TSPE4.C2 genes34 and fimH, papC, sfa/focDE, afaC, hlyCA, cnf, and iucC operons62. Additional information on PCR primers and conditions is summarized in Table 3. For phylotyping, three genes (chuA, yjaC, TSPE4.C2) were amplified by multiplex PCR. Phylotype group was categorized according to the combination of these three genes: phylogenetic group A (−/−/+; −/+/−), group B1 (−/−/+), group B2(+/+/−; +/+/+), and group D (+/−/−; +/−/+)34. All PCR reactions were carried out by using a 20-μl mixture containing 2 μl of DNA, 10 μl of Topsimple nTaq-Hot premix (Enzynomics, Daejeon, Korea), and 50 pmol of the selected primers in a Veriti thermal cycler (Applied Biosystems, Foster City, CA, USA). The PCR conditions for phylotyping, phoA identification, and pathotyping were as follows: (1) for phylotyping, denaturation for 10 min at 94 °C; 35 cycles of 30 s at 94 °C, 30 s at 55 °C, and 30 s at 72 °C; and a final extension step of 10 min at 72 °C; (2) for phoA identification, denaturation for 10 min at 94 °C; 35 cycles of 60 s at 94 °C, 60 s at 56 °C, and 60 s at 72 °C; and a final extension step of 10 min at 72 °C; (3) for pathotyping, denaturation for 10 min at 94 °C; 35 cycles of 120 s at 94 °C, annealing s shown in Table 3, and 60 s at 72 °C; and a final extension step of 10 min at 72 °C. Then 10 μl of PCR product was mixed with 1 μl of Midori Green Direct (Nippon Genetics Europe, Dueren, Germany) and followed by 2% agarose gel electrophoresis. Imaging was performed using a Gel-doc XR+ gel documentation system (Bio-Rad, Hercules, CA, USA). Sizes of amplicons were assessed by comparing them with a 1 kb plus DNA ladder (Enzynomics, Daejeon, Korea) on the same gel.
Table 3.
List of primers and PCR conditions used in this study.
| Purpose | Target | Primer | Sequence (5’ to 3’) | Annealing (°C/sec) | Denaturation (sec) | Extension (sec) | Size (bp) | Reference |
|---|---|---|---|---|---|---|---|---|
| E. coli identification | E. coli alkaline phosphatase (PhoA) | PhoA-F | GTCACAAAAGCCCGGACACCATAAATGCCT | 56/60 | 60 | 60 | 903 | 61 |
| PhoA-R | TACACTGTCATTACGTTGCGGATTTGGCGT | |||||||
| Phylotyping | Outer membrane hemin receptor (chuA) | ChuA-F | GACGAACCAACGGTCAGGAT | 55/30 | 30 | 30 | 279 | 34 |
| ChuA-R | TGCCGCCAGTACCAAAGACA | |||||||
| Conserved stress-induced protein (yjaA) | YjaA-F | TGAAGTGTCAGGAGACGCTG | 55/30 | 30 | 30 | 211 | 34 | |
| YjaA-R | ATGGAGAATGCGTTCCTCAAC | |||||||
| TspE4.C2 fragment | TspE4.C2-F | GAGTAATGTCGGGGCATTCA | 55/30 | 30 | 30 | 152 | 34 | |
| TspE4.C2-R | CGCGCCAACAAAGTATTACG | |||||||
| UPEC pathotyping | Type 1 fimbriae (fimH) | FimH-F | AACAGCGATGATTTCCAGTTTGTGTG | 65/30 | 120 | 60 | 465 | 63 |
| FimH-R | ATTGCGTACCAGCATTAGCAATGTCC | |||||||
| P fimbriae (papC) | PapC-F | GACGGCTGTACTGCAGGGTGTGGCG | 65/30 | 120 | 60 | 328 | 64 | |
| PapC-R | ATATCCTTTCTGCAGGGATGCAATA | |||||||
| S and FIC fimbriae (sfa/focDE) | Sfa-F | CTCCGGAGAACTGGGTGCATCTTAC | 65/30 | 120 | 60 | 410 | 64 | |
| Sfa-R | CGGAGGAGTAATTACAAACCTGGCA | |||||||
| Afa adhesins (afaC) | Afa-F | CGGCTTTTCTGCTGAACTGGCAGGC | 65/30 | 120 | 60 | 672 | 64 | |
| Afa-R | CCGTCAGCCCCCACGGCAGACC | |||||||
| Hemolysin (hlyCA) | Hly-F | AGATTCTTGGGCATGTATCCT | 65/30 | 120 | 60 | 556 | 65 | |
| Hly-R | TTGCTTTGCAGACTGTAGTGT | |||||||
| Cytotoxic necrotizing factor (cnf) | Cnf-F | TTATATAGTCGTCAAGATGGA | 58/30 | 120 | 60 | 693 | 66 | |
| Cnf-R | CACTAAGCTTTACAATATTGA | |||||||
| Aerobactin (iucC) | Aer-F | AAACCTGGCTTACGCAACTGT | 60/30 | 120 | 60 | 269 | 65 | |
| Aer-R | ACCCGTCTGCAAATCATGGAT |
In vitro BMDM stimulation
Bone marrow cells were isolated from femurs and tibias of 6- to 10-week-old female B6 mice and cultured for 7 days with macrophage differentiation medium containing RPMI 1640 (Hyclone, South Logan, UT, USA) supplemented with 80 ng/ml M-CSF (BioLegend, San Diego, CA, USA), glutamine, sodium pyruvate, 10% heat-inactivated FBS (Hyclone), 1% 100 × penicillin-streptomycin and 15 mM HEPES (Gibco BRL, Gaithersburg, MD, USA). Differentiated macrophages were detached by cell lifter and 2.0 × 105 of BMDMs were seeded into a 48-well plate followed by incubation overnight for attachment. Cells were then treated with P. mirabilis or E. coli isolates in RPMI 1640 without antibiotics at an MOI of 1 for 3 h followed by the addition of 100 µg/ml gentamicin (Gibco BRL) and additional culture for 9 h. Culture supernatants of infected cells were harvested and stored in −80 °C until use in an ELISA.
ELISA
Levels of IL-1β and TNF-α in culture supernatants were measured using Duoset mouse ELISA kits (R&D Systems, Minneapolis, MN, USA) according to the manufacturer’s directions. The amounts of cytokine produced by E. coli stimulation were normalized to the same cytokine produced by P. mirabilis (positive control) and shown as relative cytokine induction.
Cell viability assay
BMDMs were washed twice with DPBS supplemented with penicillin-streptomycin and 100 µg/ml gentamicin (Gibco BRL) and then treated with EZ-Cytox Enhanced Cell Viability Assay reagent (Daeil Lab Service, Seoul, Korea) at 37 °C for 30 min. Cell culture supernatants were then placed on 96-well plates and absorbance was measured at a wavelength of 450 nm by Epoch microplate spectrophotometer (Bio-Tek).
Statistical analysis
Data were analyzed using prism 5 software (GraphPad Software, La Jolla, CA, USA). Student’s t-test was performed to determine significance for most data, including experiments investigating any relationship between IL-1β and patient clinical data. We used the Chi-square test to investigate relationships between CRP value in patient serum and patient VUR, DMSA, and sonography data. Significance was defined as a p value < 0.05.
Supplementary information
Acknowledgements
Forty clinical isolates were kindly provided by GNUH (Gyeongsang National University Hospital) Branch of NCCP (National Culture Collection for Pathogens). This work was supported by a National Research Foundation of Korea (NRF) grant (2016R1C1B2008089) funded by the Ministry of Science and ICT and Creative-Pioneering Researchers Program through Seoul National University (SUS). This work was also supported by Biomedical Research Institute fund ‘GNUHRIF-2016-0008’ from Gyeongsang National University Hospital. It was also supported by development fund foundation, Gyeongsang National University, 2015 (JL).
Author contributions
A.G., J.L. and S.U.S. designed and coordinated this study. H.H. and J.C. collected samples and interpreted clinical data. J.J. performed most experiments and analyzed data. B.B. and Y.H. assisted in completing the experiments. B.K., D.K., S.Y.S. and S.U.S. contributed analytic tools and interpreted the results. J.J., H.H., J.L., and S.U.S. wrote the manuscript.
Data availability
All data generated or analyzed during this study are included in this published article (and its Supplementary Information Files).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Jong-Hyeok Jung and Hyun Jung Hong.
Contributor Information
Jae-Young Lim, Email: pedneu@gnu.ac.kr.
Sang-Uk Seo, Email: suseo@ulsan.ac.kr.
Supplementary information
is available for this paper at 10.1038/s41598-019-52070-3.
References
- 1.Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13:269–284. doi: 10.1038/nrmicro3432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chang SL, Shortliffe LD. Pediatric urinary tract infections. Pediatr Clin North Am. 2006;53:379–400, vi. doi: 10.1016/j.pcl.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 3.Winberg J, Bergstrom T, Jacobsson B. Morbidity, age and sex distribution, recurrences and renal scarring in symptomatic urinary tract infection in childhood. Kidney Int Suppl. 1975;4:S101–106. [PubMed] [Google Scholar]
- 4.Bhat RG, Katy TA, Place FC. Pediatric Urinary Tract Infections. Emergency Medicine Clinics of North America. 2011;29:637-+. doi: 10.1016/j.emc.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 5.Bower JM, Eto DS, Mulvey MA. Covert operations of uropathogenic Escherichia coli within the urinary tract. Traffic. 2005;6:18–31. doi: 10.1111/j.1600-0854.2004.00251.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Totsika M, et al. Uropathogenic Escherichia coli mediated urinary tract infection. Curr Drug Targets. 2012;13:1386–1399. doi: 10.2174/138945012803530206. [DOI] [PubMed] [Google Scholar]
- 7.Selvarangan R, et al. Interaction of Dr adhesin with collagen type IV is a critical step in Escherichia coli renal persistence. Infect Immun. 2004;72:4827–4835. doi: 10.1128/IAI.72.8.4827-4835.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sokurenko EV, Courtney HS, Maslow J, Siitonen A, Hasty DL. Quantitative differences in adhesiveness of type 1 fimbriated Escherichia coli due to structural differences in fimH genes. J Bacteriol. 1995;177:3680–3686. doi: 10.1128/jb.177.13.3680-3686.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garcia TA, Ventura CL, Smith MA, Merrell DS, O’Brien AD. Cytotoxic necrotizing factor 1 and hemolysin from uropathogenic Escherichia coli elicit different host responses in the murine bladder. Infect Immun. 2013;81:99–109. doi: 10.1128/IAI.00605-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sugawara T, et al. Structural basis for pore-forming mechanism of staphylococcal alpha-hemolysin. Toxicon. 2015;108:226–231. doi: 10.1016/j.toxicon.2015.09.033. [DOI] [PubMed] [Google Scholar]
- 11.Li B, et al. Inflammation drives renal scarring in experimental pyelonephritis. Am J Physiol Renal Physiol. 2017;312:F43–F53. doi: 10.1152/ajprenal.00471.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sundac Lana, Dando Samantha J., Sullivan Matthew J., Derrington Petra, Gerrard John, Ulett Glen C. Protein-based profiling of the immune response to uropathogenicEscherichia coliin adult patients immediately following hospital admission for acute cystitis. Pathogens and Disease. 2016;74(6):ftw062. doi: 10.1093/femspd/ftw062. [DOI] [PubMed] [Google Scholar]
- 13.Sheu JN, et al. Urine interleukin-1beta in children with acute pyelonephritis and renal scarring. Nephrology (Carlton) 2007;12:487–493. doi: 10.1111/j.1440-1797.2007.00819.x. [DOI] [PubMed] [Google Scholar]
- 14.Ambite I, et al. Molecular Basis of Acute Cystitis Reveals Susceptibility Genes and Immunotherapeutic Targets. PLoS Pathog. 2016;12:e1005848. doi: 10.1371/journal.ppat.1005848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nagamatsu K, et al. Dysregulation of Escherichia coli alpha-hemolysin expression alters the course of acute and persistent urinary tract infection. Proc Natl Acad Sci USA. 2015;112:E871–880. doi: 10.1073/pnas.1500374112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gupta R, et al. RNA and beta-hemolysin of group B Streptococcus induce interleukin-1beta (IL-1beta) by activating NLRP3 inflammasomes in mouse macrophages. J Biol Chem. 2014;289:13701–13705. doi: 10.1074/jbc.C114.548982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seo SU, et al. Distinct Commensals Induce Interleukin-1beta via NLRP3 Inflammasome in Inflammatory Monocytes to Promote Intestinal Inflammation in Response to Injury. Immunity. 2015;42:744–755. doi: 10.1016/j.immuni.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chang AC, Krishnan S, Prasadarao NV. The effects of cytotoxic necrotizing factor 1 expression in the uptake of Escherichia coli K1 by macrophages and the onset of meningitis in newborn mice. Virulence. 2016;7:806–818. doi: 10.1080/21505594.2016.1192730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang H, et al. Cytotoxic Necrotizing Factor 1 Downregulates CD36 Transcription in Macrophages to Induce Inflammation During Acute Urinary Tract Infections. Front Immunol. 2018;9:1987. doi: 10.3389/fimmu.2018.01987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Diabate M, et al. Escherichia coli alpha-hemolysin counteracts the anti-virulence innate immune response triggered by the Rho GTPase activating toxin CNF1 during bacteremia. PLoS Pathog. 2015;11:e1004732. doi: 10.1371/journal.ppat.1004732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carey AJ, et al. Uropathogenic Escherichia coli Engages CD14-Dependent Signaling to Enable Bladder-Macrophage-Dependent Control of Acute Urinary Tract Infection. J Infect Dis. 2016;213:659–668. doi: 10.1093/infdis/jiv424. [DOI] [PubMed] [Google Scholar]
- 22.Schiwon M, et al. Crosstalk between sentinel and helper macrophages permits neutrophil migration into infected uroepithelium. Cell. 2014;156:456–468. doi: 10.1016/j.cell.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bokil NJ, et al. Intramacrophage survival of uropathogenic Escherichia coli: differences between diverse clinical isolates and between mouse and human macrophages. Immunobiology. 2011;216:1164–1171. doi: 10.1016/j.imbio.2011.05.011. [DOI] [PubMed] [Google Scholar]
- 24.Mavromatis CH, et al. The co-transcriptome of uropathogenic Escherichia coli-infected mouse macrophages reveals new insights into host-pathogen interactions. Cell Microbiol. 2015;17:730–746. doi: 10.1111/cmi.12397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baorto DM, et al. Survival of FimH-expressing enterobacteria in macrophages relies on glycolipid traffic. Nature. 1997;389:636–639. doi: 10.1038/39376. [DOI] [PubMed] [Google Scholar]
- 26.Bens M, et al. Flagellin/TLR5 signalling activates renal collecting duct cells and facilitates invasion and cellular translocation of uropathogenic Escherichia coli. Cell Microbiol. 2014;16:1503–1517. doi: 10.1111/cmi.12306. [DOI] [PubMed] [Google Scholar]
- 27.Demirel I, et al. Activation of the NLRP3 Inflammasome Pathway by Uropathogenic Escherichia coli Is Virulence Factor-Dependent and Influences Colonization of Bladder Epithelial Cells. Front Cell Infect Microbiol. 2018;8:81. doi: 10.3389/fcimb.2018.00081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ingersoll MA, Kline KA, Nielsen HV, Hultgren SJ. G-CSF induction early in uropathogenic Escherichia coli infection of the urinary tract modulates host immunity. Cell Microbiol. 2008;10:2568–2578. doi: 10.1111/j.1462-5822.2008.01230.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hayes, B. W. & Abraham, S. N. Innate Immune Responses to Bladder Infection. Microbiol Spectr4, 10.1128/microbiolspec.UTI-0024-2016 (2016). [DOI] [PMC free article] [PubMed]
- 30.Godaly G, et al. Neutrophil recruitment, chemokine receptors, and resistance to mucosal infection. J Leukoc Biol. 2001;69:899–906. [PubMed] [Google Scholar]
- 31.Hagberg L, et al. Difference in susceptibility to gram-negative urinary tract infection between C3H/HeJ and C3H/HeN mice. Infect Immun. 1984;46:839–844. doi: 10.1128/iai.46.3.839-844.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hannan TJ, Mysorekar IU, Hung CS, Isaacson-Schmid ML, Hultgren SJ. Early severe inflammatory responses to uropathogenic E. coli predispose to chronic and recurrent urinary tract infection. PLoS Pathog. 2010;6:e1001042. doi: 10.1371/journal.ppat.1001042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee YJ, Lee JH, Park YS. Risk factors for renal scar formation in infants with first episode of acute pyelonephritis: a prospective clinical study. J Urol. 2012;187:1032–1036. doi: 10.1016/j.juro.2011.10.164. [DOI] [PubMed] [Google Scholar]
- 34.Clermont O, Bonacorsi S, Bingen E. Rapid and simple determination of the Escherichia coli phylogenetic group. Appl Environ Microbiol. 2000;66:4555–4558. doi: 10.1128/AEM.66.10.4555-4558.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fink SL, Cookson BT. Caspase-1-dependent pore formation during pyroptosis leads to osmotic lysis of infected host macrophages. Cell Microbiol. 2006;8:1812–1825. doi: 10.1111/j.1462-5822.2006.00751.x. [DOI] [PubMed] [Google Scholar]
- 36.Jiang YH, Peng CH, Liu HT, Kuo HC. Increased pro-inflammatory cytokines, C-reactive protein and nerve growth factor expressions in serum of patients with interstitial cystitis/bladder pain syndrome. PLoS One. 2013;8:e76779. doi: 10.1371/journal.pone.0076779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin SJ, Huang JL. Circulating interleukin (IL)−1 beta, IL-6 and tumor necrosis factor-alpha in children with febrile infection–a comparison with C-reactive protein. Asian Pac J Allergy Immunol. 1998;16:105–109. [PubMed] [Google Scholar]
- 38.Mahyar A, et al. Are serum procalcitonin and interleukin-1 beta suitable markers for diagnosis of acute pyelonephritis in children? Prague Med Rep. 2014;115:16–23. doi: 10.14712/23362936.2014.2. [DOI] [PubMed] [Google Scholar]
- 39.Lee JH, et al. Phylogenetic group distributions, virulence factors and antimicrobial resistance properties of uropathogenic Escherichia coli strains isolated from patients with urinary tract infections in South Korea. Lett Appl Microbiol. 2016;62:84–90. doi: 10.1111/lam.12517. [DOI] [PubMed] [Google Scholar]
- 40.Campos ACC, et al. Comprehensive Molecular Characterization of Escherichia coli Isolates from Urine Samples of Hospitalized Patients in Rio de Janeiro, Brazil. Front Microbiol. 2018;9:243. doi: 10.3389/fmicb.2018.00243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lavigne JP, et al. Resistance and virulence potential of uropathogenic Escherichia coli strains isolated from patients hospitalized in urology departments: a French prospective multicentre study. J Med Microbiol. 2016;65:530–537. doi: 10.1099/jmm.0.000247. [DOI] [PubMed] [Google Scholar]
- 42.Sabate M, Moreno E, Perez T, Andreu A, Prats G. Pathogenicity island markers in commensal and uropathogenic Escherichia coli isolates. Clin Microbiol Infect. 2006;12:880–886. doi: 10.1111/j.1469-0691.2006.01461.x. [DOI] [PubMed] [Google Scholar]
- 43.Franchi L, Munoz-Planillo R, Nunez G. Sensing and reacting to microbes through the inflammasomes. Nat Immunol. 2012;13:325–332. doi: 10.1038/ni.2231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hamilton C, Tan L, Miethke T, Anand PK. Immunity to uropathogens: the emerging roles of inflammasomes. Nat Rev Urol. 2017;14:284–295. doi: 10.1038/nrurol.2017.25. [DOI] [PubMed] [Google Scholar]
- 45.Boyer L, Lemichez E. Switching Rho GTPase activation into effective antibacterial defenses requires the caspase-1/IL-1beta signaling axis. Small GTPases. 2015;6:186–188. doi: 10.1080/21541248.2015.1095698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.M V Murthy A, et al. Regulation of hemolysin in uropathogenic Escherichia coli fine-tunes killing of human macrophages. Virulence. 2018;9:967–980. doi: 10.1080/21505594.2018.1465786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ristow LC, Welch RA. Hemolysin of uropathogenic Escherichia coli: A cloak or a dagger? Biochim Biophys Acta. 2016;1858:538–545. doi: 10.1016/j.bbamem.2015.08.015. [DOI] [PubMed] [Google Scholar]
- 48.Schaale K, et al. Strain- and host species-specific inflammasome activation, IL-1beta release, and cell death in macrophages infected with uropathogenic Escherichia coli. Mucosal Immunol. 2016;9:124–136. doi: 10.1038/mi.2015.44. [DOI] [PubMed] [Google Scholar]
- 49.Koizumi Y, et al. Inflammasome activation via intracellular NLRs triggered by bacterial infection. Cell Microbiol. 2012;14:149–154. doi: 10.1111/j.1462-5822.2011.01707.x. [DOI] [PubMed] [Google Scholar]
- 50.Khan AS, et al. Receptor structure for F1C fimbriae of uropathogenic Escherichia coli. Infect Immun. 2000;68:3541–3547. doi: 10.1128/IAI.68.6.3541-3547.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Varki A, Gagneux P. Multifarious roles of sialic acids in immunity. Ann N Y Acad Sci. 2012;1253:16–36. doi: 10.1111/j.1749-6632.2012.06517.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Monner DA, Muhlradt PF. Surface expression of Forssman glycosphingolipid antigen on murine bone marrow-derived macrophages is subject to both temporal and population-specific regulation and is modulated by IL-4 and IL-6. Immunobiology. 1993;188:82–98. doi: 10.1016/S0171-2985(11)80489-4. [DOI] [PubMed] [Google Scholar]
- 53.Hull RA, et al. Role of type 1 fimbria- and P fimbria-specific adherence in colonization of the neurogenic human bladder by Escherichia coli. Infect Immun. 2002;70:6481–6484. doi: 10.1128/IAI.70.11.6481-6484.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hedlund M, et al. Type 1 fimbriae deliver an LPS- and TLR4-dependent activation signal to CD14-negative cells. Mol Microbiol. 2001;39:542–552. doi: 10.1046/j.1365-2958.2001.02205.x. [DOI] [PubMed] [Google Scholar]
- 55.Tosif S, Baker A, Oakley E, Donath S, Babl FE. Contamination rates of different urine collection methods for the diagnosis of urinary tract infections in young children: an observational cohort study. J Paediatr Child Health. 2012;48:659–664. doi: 10.1111/j.1440-1754.2012.02449.x. [DOI] [PubMed] [Google Scholar]
- 56.Kliegman, R., Behrman, R. E. & Nelson, W. E. Nelson textbook of pediatrics. Edition 20/edn, (Elsevier, 2016:2559).
- 57.Thomas-White K, Brady M, Wolfe AJ, Mueller ER. The bladder is not sterile: History and current discoveries on the urinary microbiome. Curr Bladder Dysfunct Rep. 2016;11:18–24. doi: 10.1007/s11884-016-0345-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Abe CM, et al. Uropathogenic Escherichia coli (UPEC) strains may carry virulence properties of diarrhoeagenic E. coli. FEMS Immunol Med Microbiol. 2008;52:397–406. doi: 10.1111/j.1574-695X.2008.00388.x. [DOI] [PubMed] [Google Scholar]
- 59.Terlizzi ME, Gribaudo G, Maffei ME. UroPathogenic Escherichia coli (UPEC) Infections: Virulence Factors, Bladder Responses, Antibiotic, and Non-antibiotic Antimicrobial Strategies. Front Microbiol. 2017;8:1566. doi: 10.3389/fmicb.2017.01566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Han SY, Lee IR, Park SJ, Kim JH, Shin JI. Usefulness of neutrophil-lymphocyte ratio in young children with febrile urinary tract infection. Korean J Pediatr. 2016;59:139–144. doi: 10.3345/kjp.2016.59.3.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yu Ke xin, Thong Kwai Lin. Multiplex PCR for Simultaneous Detection of Virulence Genes in Escherichia coli. Malaysian Journal of Science. 2009;28(1):1–14. doi: 10.22452/mjs.vol28no1.1. [DOI] [Google Scholar]
- 62.Tarchouna M, Ferjani A, Ben-Selma W, Boukadida J. Distribution of uropathogenic virulence genes in Escherichia coli isolated from patients with urinary tract infection. Int J Infect Dis. 2013;17:e450–453. doi: 10.1016/j.ijid.2013.01.025. [DOI] [PubMed] [Google Scholar]
- 63.Murray, P. R. & Baron, E. J. Manual of clinical microbiology. 9th edn, (ASM Press, 2007).
- 64.Soto SM, Zuniga S, Ulleryd P, Vila J. Acquisition of a pathogenicity island in an Escherichia coli clinical isolate causing febrile urinary tract infection. Eur J Clin Microbiol Infect Dis. 2011;30:1543–1550. doi: 10.1007/s10096-011-1258-2. [DOI] [PubMed] [Google Scholar]
- 65.Usein CR, et al. Prevalence of virulence genes in Escherichia coli strains isolated from Romanian adult urinary tract infection cases. J Cell Mol Med. 2001;5:303–310. doi: 10.1111/j.1582-4934.2001.tb00164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Licznar P, et al. Revised prevalence of afa+ Escherichia coli strains in acute pyelonephritis of children. Pathol Biol (Paris) 2003;51:512–515. doi: 10.1016/S0369-8114(03)00153-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article (and its Supplementary Information Files).