Abstract
The authors present two cases in which the ruptured popliteal (Baker’s) cysts remained undetected and were diagnosed only during an isotope investigation. The aim was to describe a specific imaging sign, the “arch sign”, that is indicative of ruptured Baker’s cysts. In both cases, the whole-body imaging was performed 2 hours after injection of 706.7 MBq of Tc-99m-MDP. Single-photon emission computed tomography (SPECT) imaging was performed to localize an accumulation of the radiopharmaceutical. An analysis of literature was performed to connect these cases with previously reported data and to detect the pathognomonic radio image sign of ruptured popliteal cysts. The arch-shaped distribution of the radiopharmaceutical below the knee joints was seen already on the whole-body bone scan image in both cases. An anterior view of SPECT MIP images showed the arched accumulation of the Tc-99m-MDP bone tracer along the postero-medial aspect of the right calf secondary to synovial fluid leak from a ruptured Baker’s cyst. The similar arthroscintigrams were published since 1971 without recognizing this sign as pathognomonic. Tc-99m-MDP bone scanning is sensitive for a Baker’s cyst with synovial effusion, and distribution of a radiopharmaceutical in the medial posterior calf in a shape of an arch, the arch sign, may serve as an indicator of a ruptured popliteal cyst.
Keywords: Popliteal cysts, Ruptured Baker’s cysts, Tc-99m-MDP, SPECT
Introduction
Cysts in the popliteal region (Baker’s cysts) are benign lesions filled with synovial fluid that frequently communicates with the semimembranosus-gastrocnemius bursa. They may be associated with osteoarthritis, rheumatoid arthritis, or cartilage tears, but in many cases, they remain asymptomatic [1, 2]. In addition to the habit of mimicking thrombophlebitis and deep vein thrombosis or coexisting with them, the cysts should be differentiated from liposarcoma, popliteal aneurysm or hematoma, popliteal varices, cellulitis, xanthoma, fibrosarcoma, and other soft tissue tumors [2–4]. A physical examination is confusing in most such cases, and certain imaging techniques were introduced in the process of diagnosis already in the middle of the previous century.
Popliteal cysts were examined radiographically by arthrography of the knee, ultrasonography, and MRI and CT scan images that permitted visualization of a well-defined cyst wall and fluid density contents [5, 6]. While intact cysts became well detectable, the diagnostic precision in cases of the ruptured or dissecting cysts was less impressive because in such cases the cyst actually disappears and the synovial fluid escapes into the calf and may widely spread over its superficial posterior compartment. That is why nuclear medicine imaging procedures were also added to the diagnostic armamentarium for Baker’s cysts.
Rarely published articles on the use of isotopes for diagnostic purposes in cases of the suspected Baker’s cyst indicated high potential of radionuclide-involving investigations in cases of the popliteal cysts [7, 8]. Whatever isotope was used, it was demonstrated that in the case of a ruptured Baker’s cyst, radioactivity extends far below the knee joint into the posterior and sometimes medial calf [9, 10]. Despite these promising results, diagnostic nuclear medicine was completely ignored in the review articles on the imaging spectrum of Baker’s (popliteal) cysts and diagnostic approaches to popliteal fossa masses [11, 12].
To stress the importance of diagnostic nuclear medicine in cases of ruptured popliteal cysts, we present two cases in which the ruptured cysts remained undetected and were diagnosed only during an isotope investigation. The second aim of the current paper was to describe a specific imaging sign, the “arch sign,” that is indicative of ruptured Baker’s cysts. Our analysis of literature connects these cases with previously reported data to confirm that the “arch sign” is a pathognomonic sign of ruptured popliteal cysts.
Case Reports
Case 1
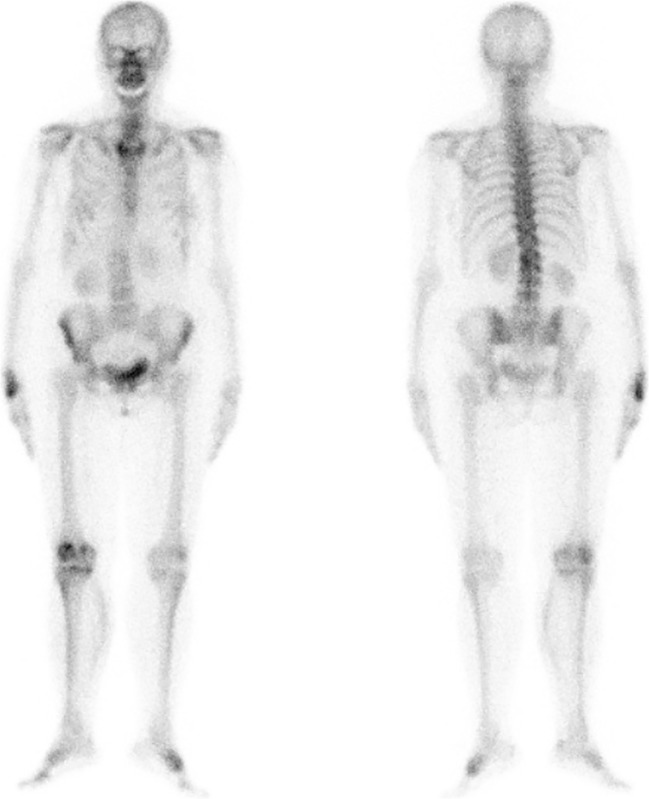
A 68-year-old female patient was presented for the whole-body bone scan to evaluate her complaints of idiopathic pains in various joints of the extremities. The patient did not have the history of rheumatoid arthritis, thrombophlebitis, synovitis of the knee, and traumas of the low extremities. No acute inflammatory disorder was detected. She was administered with 706.7 MBq (19.1 mCi) of 99m-technetium methylene diphosphonate (Tc-99m-MDP). The whole-body imaging was performed 2 hours after the radiopharmaceutical was injected. The arch-shaped distribution of the radiopharmaceutical below the right knee was seen already on the whole-body bone scan image (Fig. 1).
Fig. 1.
The whole-body Tc-99m-MDP bone scan (case 1), demonstrating diffuse tracer accumulation in the right calf with arched linear increased tracer activity along the postero-medial aspect indicative of synovial fluid accumulation due to a ruptured Baker’s cyst
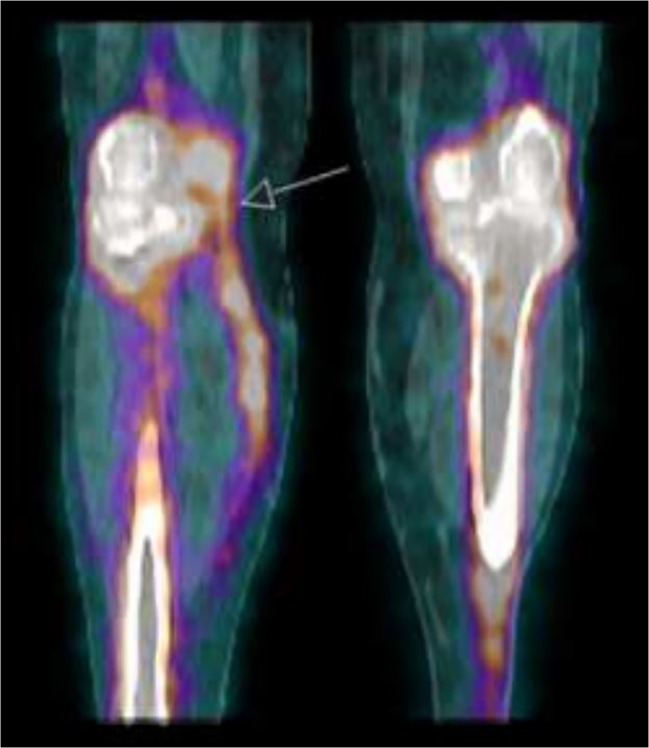
A diffuse intense accumulation of Tc-99m-MDP was noted in all joint surfaces of the right knee. In addition, an accumulation of the tracer was also seen in the synovial effusion of the same knee. It should be noted that the tracer uptake runs along distally and medial-posteriorly to the right calf. Single-photon emission computed tomography (SPECT) with low-dose computed tomography (CT) imaging was performed and demonstrated the localized accumulation of the radiopharmaceutical in the effusion between the semimembranosus tendon and the medial head of the gastrocnemius (Fig. 2). The ruptured Baker’s cyst was detected, and an MRI-based confirmation of the diagnosis was suggested. The findings were confirmed by MR examination performed later on. A surgical opinion also confirmed the diagnosis, but due to the age and general condition of the patient, a conservative treatment was chosen.
Fig. 2.
Fused coronal SPECT-CT image of a 99m-Tc-MDP bone scan of case 1 knees, presenting synovial fluid leak from the ruptured Baker’s cyst and the connection, at the arrow level, between the knee and the arched tracer accumulation
Case 2
A 74-year-old woman was admitted to the Department of Nuclear Medicine with complaints of pain in the left knee and suspected osteonecrosis. There was no history of multiple joint pains, rheumatoid arthritis, thrombophlebitis, and any pathology in the left knee prior to the pain episode. The patients suffered from obesity, atrial fibrillation, and hypertension. On physical examination of the knee, no soft mass was palpable in the popliteal fossa and deep vein thrombosis was suspected. No anteroposterior or lateral instability of the joint was observed. The duplex scan of the left knee and calf showed edema and swelling of the left calf and popliteal fossa without any evidence for thrombosis at the femoral or popliteal veins.
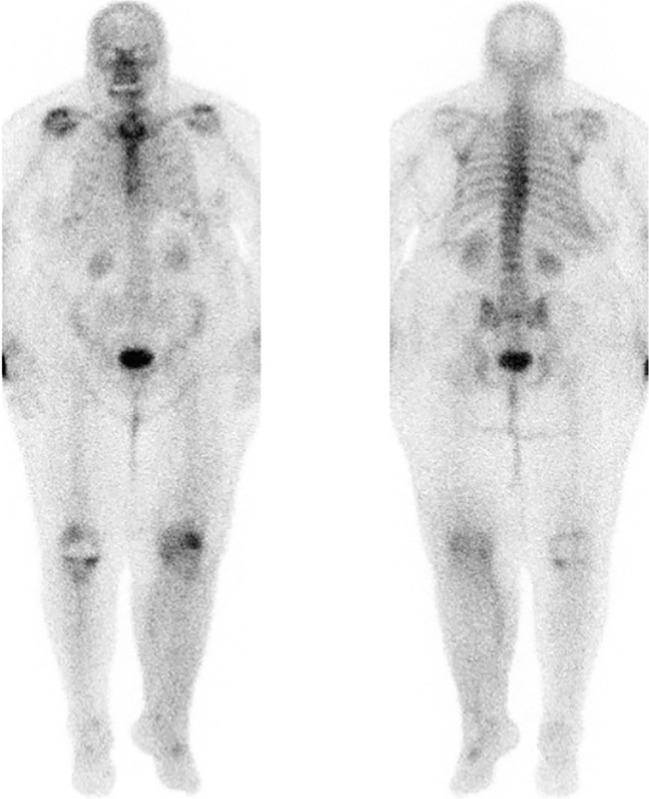
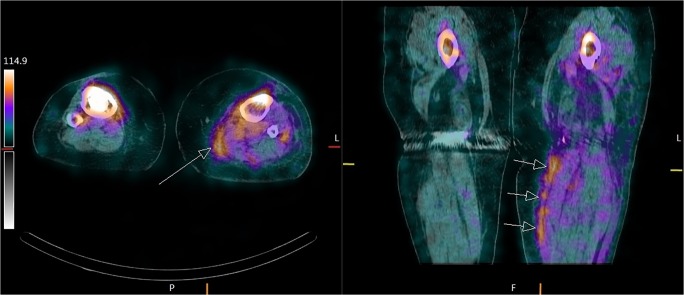
On a 3-phase bone scan image, hyperemia and increased blood pool around the left knee were detected with uptake on the late scan in the patellofemoral and medial aspect of the knee. It was accompanied with intra-articular knee effusion on a SPECT-CT image compatible with degenerative changes. As in case 1, the arch-shaped distribution of the radiopharmaceutical (706.7 MBq) below the left knee was seen already on the whole-body bone scan image (Fig. 3). The accumulation of Tc-99m-MDP in the postero-medial aspect of the calf due to a leak of synovial fluid was clearly observed (Fig. 4). In addition, there was a swelling of the left calf and an increased accumulation of Tc-99m-MDP on the medial aspect of the popliteal fossa space between the semimembranosus tendon and the medial head of the gastrocnemius. The patient was diagnosed with a ruptured Baker’s cyst. A surgical opinion also confirmed the diagnosis, but due to the age and general condition of the patient, a conservative treatment was chosen.
Fig. 3.
The whole-body Tc-99m-MDP bone scan of case 2, demonstrating diffuse tracer accumulation in the left calf with arched linear increased tracer activity along the postero-medial aspect indicative of synovial fluid accumulation due to a ruptured Baker’s cyst
Fig. 4.
SPECT-CT axial (left image) and coronal (right side) images of case 2 left knee, demonstrating Tc-99m-MDP tracer and synovial fluid accumulation at the superficial posterior compartment of the left calf due to a ruptured Baker’s cyst
Discussion
Our cases demonstrate the usefulness of nuclear medicine in diagnosing previously undetected ruptured Baker’s cysts. When the above-described patients were sent for radionuclide scintigraphy, the presence of Baker’s cysts and their rupture were not suspected. In addition to asymptomatic behavior of the majority of such cysts before the rupture [1, 2, 13], Baker’s cysts may develop and rupture in normal knee joints [14] and rupture itself can remain asymptomatic [13]. Therefore, to whatever reason the whole-body scanning or a specific investigation of the knee joints is performed, nuclear medicine practitioners should be aware of the imaging sign indicating a ruptured Baker’s cyst. The arch sign, the visible distribution of a radiopharmaceutical in the medial posterior calf in a shape of an arch, is indeed the pathognomonic sign of ruptured popliteal cysts. To our knowledge, the first images of the arch sign were published in the article of Levin et al. in 1971 (Figs. 3 and 4 of that article) [9]. The authors used I-131-labeled human serum albumin being injected intra-articularly to visualize the ruptured cyst. The first image of the arch sign obtained with the help of 99m-technetium-containing radiopharmaceutical (Tc-99m-labeled human serum albumin) was published in 1975 (arthroscintigrams) [15]. The authors of the 1970s, with their technical devices and limited previously collected data, did not recognize the shape of the radioisotope shadow as pathognomonic. The following publications of 99m-technetium-involving investigations of Baker’s cysts were extremely sporadic. For example, the last research on the subject, in which specifically Tc-99m-MDP was used, was published in 2006 [16]. Twelve years later, combining all the data from 1969 to 2019, we are inclined to believe that (1) the bone scanning can be sensitive for a Baker’s cyst with synovial effusion and that (2) the above-described arch sign may serve as an indicator of a ruptured cyst (Fig. 5). There were case reports describing anterolateral rupture of a Baker’s cyst or even proximal dissection and rupture of the cyst into the thigh [17, 18]. Such cases are extremely rare while the absolute majority of Baker’s cysts rupture towards the superficial posterior compartment of the calf [1, 2, 19] thus presenting the arch sign. The reason for appearance of this sign is that before Tc-99m-MDP will concentrate in the bones, it is distributed in various body fluids including the synovial fluid. Accumulation of the tracer in the synovial fluid may be even enhanced due to the increased regional perfusion and permeability in cases of chronically inflamed arthritic joints causing extravasation of Tc-99m-MDP into the expanded synovial interstitium. After that, Tc-99m-MDP is successfully washed out from the blood through the kidneys but remains “trapped” in the leaked synovial fluid for a longer time that permits the observation of the indicated arch-shaped uptake.
Fig. 5.
The “arch sign,” the arched accumulation of the Tc-99m-MDP bone tracer along the postero-medial aspect of the right calf secondary to synovial fluid leak from a ruptured Baker’s cyst as seen on the anterior view of SPECT maximum intensity projection image (case 1)
The usefulness of SPECT investigations for cases of Baker’s cysts was recognized long ago [20]. A PET/CT scan investigation of the Baker’s cyst was also reported [21]. The beneficial cooperation between SPECT-CT and ultrasonography and MRI studies is evident. Ultrasonography presents clear results if “a large hypoechoic space” is seen behind the calf muscles after the rupture [19]. The results will be less convincing in cases with insignificant leaks, and in such cases, Tc-99m-MDP may clearly indicate the leak of the synovial fluid. As for MRI, it is the best option to diagnose the intact cyst by analysis of its walls, content, and signal intensity similar to those of the synovial fluid. Yet, in some cases, even MRI data may not be fully convincing especially in cases when no underlying knee pathology was detected or the leak of the synovial fluid is insignificant. In such cases, MRI and SPECT-CT data may reinforce each other.
Conclusion
Tc-99m-MDP bone scanning is sensitive for a Baker’s cyst with synovial effusion, and distribution of a radiopharmaceutical in the medial posterior calf in a shape of an arch, the arch sign, may serve as an indicator of a ruptured popliteal cyst. SPECT-CT investigation findings may confirm soft tissue abnormalities detected by MRI.
Acknowledgments
The authors thank Michael Shterenshis for editing assistance.
Compliance with Ethical Standards
Conflict of Interest
Haim Golan and Evgeniya Fridburg declare that they have no conflict of interest.
Ethical Approval
The research did not involve human participants and/or animals because only images and previously obtained data from the charts were analyzed. No personal details of patients appear in the article as in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
The institutional review board of our institute approved this retrospective study, and the requirement to obtain informed consent was waived.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Labropoulos N, Shifrin DA, Paxinos O. New insights into the development of popliteal cysts. Br J Surg. 2004;91:1313–1318. doi: 10.1002/bjs.4635. [DOI] [PubMed] [Google Scholar]
- 2.Herman AM, Marzo JM. Popliteal cysts: a current review. Orthopedics. 2014;37:e678–e684. doi: 10.3928/01477447-20140728-52. [DOI] [PubMed] [Google Scholar]
- 3.Lee KR, Tines SC, Price HI, De Smet AA, Neff JR. The computed tomographic findings of popliteal cysts. Skelet Radiol. 1983;10:26–29. doi: 10.1007/BF00355387. [DOI] [PubMed] [Google Scholar]
- 4.Chong VF. Calf pain and swelling: Baker’s cyst mimicking deep vein thrombosis. Singap Med J. 1996;37:175–180. [PubMed] [Google Scholar]
- 5.McCarthy CL, McNally EG. The MRI appearance of cystic lesions around the knee. Skelet Radiol. 2004;33:187–209. doi: 10.1007/s00256-003-0741-y. [DOI] [PubMed] [Google Scholar]
- 6.Ward EE, Jacobson JA, Fessell DP, Hayes CW, van Holsbeeck M. Sonographic detection of Baker’s cysts: comparison with MR imaging. AJR Am J Roentgenol. 2001;176:373–380. doi: 10.2214/ajr.176.2.1760373. [DOI] [PubMed] [Google Scholar]
- 7.Wallner RJ, Dadparvar S, Croll MN, Brady LW. Demonstration of an infected popliteal (Baker’s) cyst with three-phase skeletal scintigraphy. Clin Nucl Med. 1985;10:153–155. doi: 10.1097/00003072-198503000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Lamki L. Baker’s cyst. Radionuclide arthrographic findings. Clin Nucl Med. 1985;10:147–152. doi: 10.1097/00003072-198503000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Levin MH, Nordyke RA, Ball JJ. Demonstration of dissecting popliteal cysts by joint scans after intra-articular isotope injections. Arthritis Rheum. 1971;14:591–598. doi: 10.1002/art.1780140506. [DOI] [PubMed] [Google Scholar]
- 10.Lin WY, Wang SJ. Rupture of a popliteal cyst visualized by radionuclide venography and confirmed by radionuclide arthrography. Clin Nucl Med. 1997;22:326. doi: 10.1097/00003072-199705000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Torreggiani WC, Al-Ismail K, Munk PL, Roche C, Keogh C, Nicolaou S, Marchinkow LP. The imaging spectrum of Baker’s (popliteal) cysts. Clin Radiol. 2002;57:681–691. doi: 10.1053/crad.2001.0917. [DOI] [PubMed] [Google Scholar]
- 12.Shah A, James SL, Davies AM, Botchu R. A diagnostic approach to popliteal fossa masses. Clin Radiol. 2017;72:323–337. doi: 10.1016/j.crad.2016.11.010. [DOI] [PubMed] [Google Scholar]
- 13.Mollá Olmos E, Martí-Bonmatí L, Llombart Aís R, Dosdá Muñoz R. Prevalence and characteristics of complications of Baker cysts by MRI. Rev Clin Esp. 2001;201:179–183. doi: 10.1016/S0014-2565(01)70788-6. [DOI] [PubMed] [Google Scholar]
- 14.Macfarlane DG, Bacon PA. Popliteal cyst rupture in normal knee joints. Br Med J. 1980;281(6249):1203–1204. doi: 10.1136/bmj.281.6249.1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Watkins AE, Poulose KP, Reba RC. Arthroscintigraphy with technetium albumin in diagnosis of pseudophlebitis (Baker’s) cyst. Br Med J. 1975;4:86. doi: 10.1136/bmj.4.5988.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chatzopoulos D, Markou P, Iakovou I. Scintigraphic imaging of knee synovitis in osteoarthritis after intra-articular injection of technetium-99m pertechnetate in the unilateral knee. Hell J Nucl Med. 2006;9:69–71. [PubMed] [Google Scholar]
- 17.Ushiyama T, Kawasaki T, Matsusue Y. Anterior tibial compartment syndrome following rupture of a popliteal cyst. Mod Rheumatol. 2003;13:189–190. doi: 10.3109/s10165-002-0222-5. [DOI] [PubMed] [Google Scholar]
- 18.Abdelrahman MH, Tubeishat S, Hammoudeh M. Proximal dissection and rupture of a popliteal cyst: a case report. Case Rep Radiol. 2012;2012:292414. doi: 10.1155/2012/292414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sato O, Kondoh K, Iyori K, Kimura H. Midcalf ultrasonography for the diagnosis of ruptured Baker’s cysts. Surg Today. 2001;31:410–413. doi: 10.1007/s005950170131. [DOI] [PubMed] [Google Scholar]
- 20.Smith T, Shawe DJ, Crawley JC, Gumpel JM. Use of single photon emission computed tomography (SPECT) to study the distribution of 90Y in patients with Baker's cysts and persistent synovitis of the knee. Ann Rheum Dis. 1988;47:553–558. doi: 10.1136/ard.47.7.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bagga S. Baker cyst as seen on a PET/CT scan. Clin Nucl Med. 2008;33:64–65. doi: 10.1097/RLU.0b013e31815c4f7b. [DOI] [PubMed] [Google Scholar]