Abstract
BACKGROUND
There is still large debate on feasibility and advantages of fast-track protocols in elderly population after colorectal surgery.
AIM
To investigate the impact of age on feasibility and short-term results of enhanced recovery protocol (ERP) after laparoscopic colorectal resection.
METHODS
Data from 225 patients undergoing laparoscopic colorectal resection and ERP between March 2014 and July 2018 were retrospectively analyzed. Three groups were considered according to patients’ age: Group A, 65 years old or less, Group B, 66 to 75 years old and Group C, 76 years old or more. Clinic and pathological data were compared amongst groups together with post-operative outcomes including post-operative overall and surgery-specific complications, mortality and readmission rate. Differences in post-operative length of stay and adherence to ERP’s items were evaluated in the three study groups.
RESULTS
Among the 225 patients, 112 belonged to Group A, 57 to Group B and 56 to Group C. Thirty-day overall morbidity was 32.9% whilst mortality was nihil. Though the percentage of complications progressively increased with age (25.9% vs 36.8% vs 42.9%), no differences were observed in the rate of major complications (4.5% vs 3.5% vs 1.8%), prolonged post-operative ileus (6.2% vs 12.2% vs 10.7%) and anastomotic leak (2.7% vs 1.8% vs 1.8%). Significant differences in recovery outcomes between groups were observed such as delayed urinary catheter removal (P = 0.032) and autonomous deambulation (P = 0.013) in elderly patients. Although discharge criteria were achieved later in older patients (3 d vs 3 d vs 4 d, P = 0.040), post-operative length of stay was similar in the 3 groups (5 d vs 6 d vs 6 d).
CONCLUSION
ERPs can be successfully and safely applied in elderly undergoing laparoscopic colorectal resection.
Keywords: Colorectal surgery, Laparoscopic surgery, Enhanced recovery protocol, Age, Elderly
Core tip: Feasibility and safety of enhanced recovery protocols in elderly populations undergoing minimally invasive colorectal surgery have been questioned by recent literature. Age has been considered an obstacle for enhanced recovery and a risk factor for surgical outcomes. Our study investigated the impact of age on fast-track after laparoscopic colorectal resection. Early removal of urinary catheter and walking resumption were the most difficult goals achieved by the elderly. Nevertheless, general compliance to fast-track items was good and, although discharge criteria were fulfilled later in older patients, no differences in length of stay and major complications rate were observed.
INTRODUCTION
Laparoscopy and enhanced recovery protocols (ERPs) represent two major innovations in colorectal surgery. ERP is a multi-disciplinary model of peri-operative care for patients undergoing different types of major surgery[1] and it is considered the gold standard for patients undergoing colorectal surgery[2]. The purpose of these protocols is to minimize the response to surgical related stress and promote faster restoration of homeostasis. Many studies have proved that fast-track programs are safe and effective in reducing post-operative morbidity and length of hospital stay (LOS) after colorectal surgery[3-5]. The association of minimally invasive techniques and ERPs leads to a faster recovery and definitively produces an improvement of short-term outcomes[6,7].
Early ERPs excluded elderly patients from enrollment since their frailty was considered a contraindication to fast-track pathways. Recent experiences show that elderly patients may benefit from ERP though critics have argued that successful programs are difficult to be achieved due to a lower adherence to many fast-track components[8,9]. Although the elderly have higher levels of comorbidity, frailty and social care requirements[10,11], it is not proven that they may not be able to complete an ERP or that they have different outcomes with such management[12]. The aim of this retrospective observational study was to assess the safety, feasibility and efficacy of ERP according to patients’ age after laparoscopic colorectal surgery.
MATERIALS AND METHODS
Inclusion criteria and population under study
Enhanced recovery after surgery program was introduced at the Division of General and Hepatobiliary Surgery, University of Verona Hospital Trust, in March 2014. Between March 2014 and July 2018 patients undergoing elective laparoscopic colorectal resection, with or without stoma formation, were preferentially enrolled in the ERP. All patients aged 18 years or more, undergoing elective surgery for tumor of the colon and rectum or diverticular disease were offered to enter the protocol. Exclusion criteria were: inflammatory bowel disease (IBD), familial adenomatous polyposis (FAP), palliative surgery, body mass index above 35 kg/m2, American Society of Anaesthesiologists (ASA) physical status above 3, coagulopathy, impaired kidney function, uncontrolled diabetes, severe cardiovascular impairment or chronic obstructive pulmonary disease, psychiatric disorders, drug and alcohol addiction, duration of anesthesia above 6 h and denied consent. Reasons for pre-operative and intra-operative exclusion criteria have been previously described in detail[13]. Informed consent was obtained from all the patients for the surgical procedure proposed and the protocol was approved by the local Ethics Committee.
ERAS protocol and outcome measures
The protocol was devised in accordance to the recommendations of the ERAS Society[1]. The objective of the ERP was to provide all the items to all patients as far as possible. Surgical approach, anesthesiologic management, post-operative analgesia and post-operative care according to ERAS items were previously described in detail[13,14].
Post-operative morbidity was defined as any deviation from the expected course and complications were graded according to the Clavien-Dindo Classification[15]. Thirty-day readmission rate and mortality were registered. During hospital stay, patients were clinically reviewed at least twice a day by a trained member of the surgical team and adherence to ERP items was registered together with the presence of nausea, vomiting, passage of flatus and stools, tolerance to liquid and solid diet and level of pain according to a Visual Analog Scale (VAS). Diet was considered tolerated when patient’s oral intake would be deemed enough to avoid starvation and be independent of intravenous fluids. Out of bed mobilization was considered as patient sitting on chair for at least 2 h per day while active mobilization was considered as assisted or autonomous walking or sitting on chair for more than 6 h per day.
LOS was measured from the date of surgery to the date of discharge from hospital. Time to readiness for discharge (TRD) was defined as the number of days needed to fulfill discharge criteria[16]: Patients were considered fit for discharge when bowel function was restored (stool or repeated flatus), adequate amount of food and liquid intake was tolerated, normal mobilization restored, pain well controlled with oral analgesics (VAS < 4) and CRP < 120 mg/dL on the third post-operative day (POD)[17]. Discharge delay (DD) was defined as the difference between TRD and the actual discharge from hospital. Since the aim of our ERAS protocol was not to pursue very early discharge, the TRD was considered as an indicator of how comfortable patient felt with returning home and effective presence of post-hospitalization assistance.
Data analysis
All demographic and clinical data, after treatment consent acquisition, were anonymously collected in a PC dataset. Statistical analysis was performed using IBM SPSS software version 21.0. Descriptive variables were reported as frequencies and continuous variables were reported as mean (± SD) or median (range).
Short-term outcomes and adherence to ERP items were compared in 3 groups according to patients’ age: Group A, 65 years old or less, Group B, 66 to 75 years old and Group C, 76 years old or more. These cut-off values defining elderly and old elderly patients were defined according to the World Health Organization definition[18].
Adherence to ERP items and clinical outcomes were analyzed as a binary outcome (yes/no). Discrete variables were compared with the chi-square test. For continuous outcomes, Student’s t-test, ANOVA and Mann-Whitney tests were used when indicated. All statistical tests were two-sided with statistical significance expressed as aP < 0.05 and bP < 0.01.
RESULTS
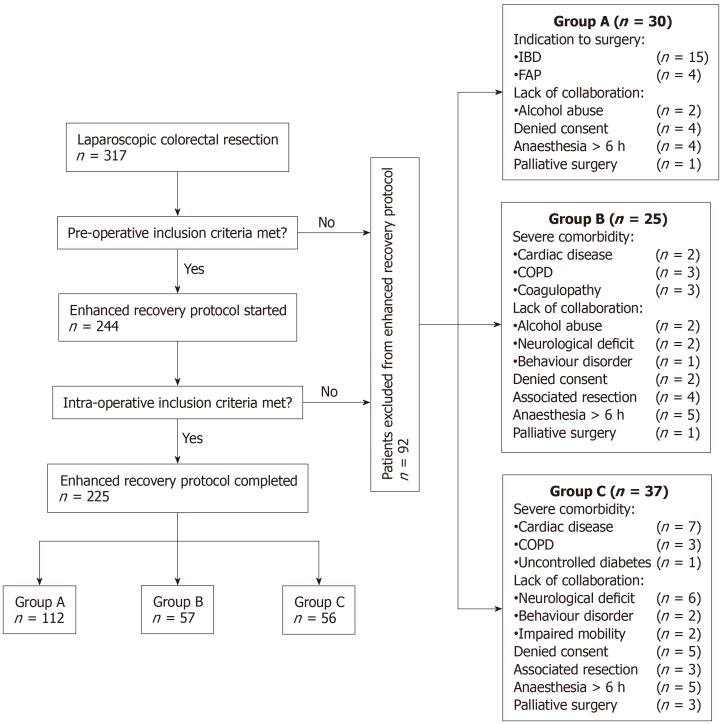
During the study period, a total of 317 patients underwent laparoscopic colorectal resection at our institution; among these, 73 patients did not meet pre-operative inclusion criteria while 19 patients were excluded due to post-operative exclusion criteria. Younger patients (Group A) were most frequently excluded due to surgical indication and refusal to participate in ERP whilst, in Group B and C the most frequent causes for exclusion were the presence of severe comorbidities and lack of collaboration (Figure 1). The final cohort was represented by 225 patients: 112 patients belonged to Group A, 57 patients to Group B and 56 patients to Group C.
Figure 1.
Exclusion criteria among the 317 patients undergoing laparoscopic colorectal resection from March 2014 to July 2018. IBD: Inflammatory bowel disease; FAP: Familial adenomatous polyposis; COPD: Chronic obstructive pulmonary disease.
Patients’ demographics and clinical characteristics according to age grouping are reported in Table 1. In Group A, most patients were classified as ASA ≤ 2 while, in Group B and Group C, the number of patients classified as ASA 3 was significantly higher (4.5% vs 24.6% vs 33.9%; P < 0.001). Similarly, a significantly higher rate of patients with comorbidities ≥ 2 was observed in Group B and C (20.5% vs 47.4% vs 58.9%; P < 0.001). Colonic cancer was the main indication for surgery in the three groups although, rectal cancer was more frequent in younger patients (28.6% vs 8.8% vs 14.3%; P = 0.007). The three groups did not differ in terms of extent of surgery, surgical procedure duration, blood loss and new stoma formation. Conversion to open surgery was comparably low in the subgroups (2% vs 7% vs 3.6%).
Table 1.
Clinic-pathological characteristics and operative data according to age grouping for the 225 patients under study, n (%)
| Age group | ||||
| Group A | Group B | Group C | P value | |
| (n = 112) | (n = 57) | (n = 56) | ||
| Age, yrb | 57.1 (18-65) | 68.9 (65.5-74.2) | 80 (75-91.6) | |
| Male sex | 62 (55.4) | 35 (61.4) | 24 (42.9) | NS |
| BMI, Kg/m2 | 25 (3.8) | 25.6 (3.7) | 24.9 (3.2) | NS |
| ASA classificationb | < 0.001 | |||
| I | 23 (20.5) | 2 (3.5) | 1 (1.8) | |
| II | 84 (75) | 41 (71.9) | 36 (64.3) | |
| III | 5 (4.5) | 14 (24.6) | 19 (33.9) | |
| Indication for surgeryb | 0.007 | |||
| Colon cancer | 46 (41.1) | 37 (64.9) | 37 (66.1) | |
| Rectal cancer | 32 (28.6) | 5 (8.8) | 8 (14.3) | |
| Benign | 34 (29.4) | 15 (26.4) | 11 (19.7) | |
| Presence of comorbiditiesb | < 0.001 | |||
| None | 48 (42.9) | 12 (21.1) | 8 (14.3) | |
| 1 | 41 (36.6) | 18 (31.6) | 15 (26.8) | |
| ≥ 2 | 23 (20.5) | 27 (47.4) | 33 (58.9) | |
| Previous surgery | 49 (43.7) | 33 (57.9) | 31 (55.4) | NS |
| R0 resection | 75 (96.2) | 42 (100) | 45 (100) | NS |
| TNM Stage | NS | |||
| Stage ≤ II | 53 (67.9) | 28 (66.7) | 36 (80) | |
| Stage III | 23 (29.5) | 11 (26.2) | 19 (20) | |
| Stage IV | 2 (2.6) | 3 (7.1) | - | |
| Extent of surgery | NS | |||
| Right hemicolectomy | 26 (23.2) | 19 (33.3) | 23 (41.1) | |
| Left hemicolectomy | 46 (41) | 28 (49.2) | 21 (37.5) | |
| Rectal resections1 | 32 (28.6) | 5 (8.8) | 8 (14.3) | |
| Abdominoperineal resection | 6 (5.4) | 1 (1.7) | - | |
| Others | 2 (1.8) | 4 (7) | 4 (7.1) | |
| Stoma formation | NS | |||
| Ileostomy | 20 (17.9) | 2 (3.6) | 5 (8.9) | |
| Colostomy | 6 (5.4) | 1 (1.8) | 1 (1.8) | |
| Time of surgery, min | 235 (125-360) | 216 (145-340) | 220 (125-320) | NS |
| Estimated blood loss, mL | 50 (20-400) | 40 (10-400) | 50 (20-250) | NS |
| Conversion to open surgery | 2 (1.8) | 4 (7) | 2 (3.6) | NS |
Includes extended resections to the upper rectum, anterior resection, low anterior resection and intersphincteric resection. Data are expressed as number of patients (%), mean (standard deviation) or median (range).
P < 0.01. BMI: Body mass index; ASA: American Society of Anaesthesiologists.
Compliance outcomes
Adherence to the 14 ERP items selected for this study is summarized in Table 2. Respiratory training, routine antiemetic therapy, nasogastric tube removal immediately after surgery, TAP block administration were equally dispensed in almost all the patients independently from age.
Table 2.
Adherence to the enhanced recovery protocol’s items according to age grouping for the 225 patients under study, n (%)
| Age group | ||||
| Group A | Group B | Group C | P value | |
| (n = 112) | (n = 57) | (n = 56) | ||
| Laparoscopy (no conversion) | 110 (98.2) | 53 (93) | 53 (94.6) | NS |
| Carbohydrate rich drinka | 48 (42.9) | 26 (45.6) | 13 (23.2) | 0.022 |
| Respiratory training | 106 (94.6) | 54 (94.7) | 55 (98.2) | NS |
| Prophylactic antiemetics | 109 (97.3) | 52 (91.2) | 52 (92.9) | NS |
| Intra-operative warming | 108 (96.4) | 52 (91.2) | 55 (98.2) | NS |
| No nasogastric tube | 101 (90.2) | 53 (93) | 48 (85.7) | NS |
| TAP block | 62 (55.4) | 29 (50.9) | 37 (66.1) | NS |
| Oral liquids POD0 | 31 (27.7) | 14 (24.6) | 9 (16.1) | NS |
| Solid food POD1 | 46 (41.1) | 18 (31.6) | 16 (28.6) | NS |
| Early mobilization | 101 (90.2) | 51 (89.5) | 50 (89.3) | NS |
| Walking POD1a | 57 (50.9) | 23 (40.4) | 21 (37.5) | 0.032 |
| Early UC removala | 66 (58.9) | 40 (70.2) | 24 (42.9) | 0.013 |
| Stop iv fluids POD2a | 67 (59.8) | 36 (63.2) | 23 (41.1) | 0.032 |
| Opiates avoidancea | 56 (50) | 22 (38.6) | 38 (67.9) | 0.007 |
| GC, % | 70.3 (36-100) | 64.3 (21-100) | 64.3 (36-100) | NS |
| GC < 50% | 20 (17.9) | 10 (17.5) | 13 (23.2) | |
| GC 50%-75% | 51 (45.5) | 23 (40.4) | 29 (51.8) | |
| GC > 75% | 41 (36.6) | 24 (42.1) | 14 (25) | |
P < 0.05. TAP: Transversus abdominis plane; POD: Post-operative day; UC: Urinary catheter; GC: Global compliance.
Compliance to early fluid intake on the day of surgery and soft diet on POD 1 was overall low and similar among groups. Discontinuation of intravenous fluid within POD2 was generally more difficult in Group C (P = 0.032) and the compliance for carbohydrate rich drink consumption was twofold in Group A and B compared to Group C (42.9% vs 45.6% vs 23.2%; P = 0.022).
Independently from age, early mobilization on chair was accomplished in a large majority of patients on POD 0 or on the morning after surgery, while walking on POD 1 was less frequently achieved in Group B and C (50.9% vs 40.4% vs 37.5%; P = 0.032).
Considering the whole cohort, older patients presented lower rates of early urinary catheter removal (58.9% vs 70.2% vs 42.9%; P = 0.013) but opioid analgesia avoidance was more frequently regarded in this group (P = 0.007).
Global compliance (GC), defined as the percentage of protocol goals achieved by each patient, was similar among groups. Good compliance was defined as adherence to more than 75% of the ERP items while, adherence to < 50% and 50%-75% of the items was classified as poor and borderline compliance, respectively (Table 2). No statistical correlation was demonstrated between age groups and GC, suggesting that ERAS goals can be achieved by elderly patients as well.
Post-operative outcomes
Post-operative outcomes are shown in Table 3. Major complication, reoperation and readmission rates were comparably low among the 3 groups. Besides a higher overall complication rate in Group B and C (25.9% vs 36.8% vs 42.9%), no differences were detected in surgery specific complications such as post-operative prolonged ileus or anastomotic leak. Older patients needed post-operative red blood cells transfusion (RBC) more frequently, even though the percentage was anyhow low (5.4% vs 3.5% vs 9%). No post-operative mortality was observed during the study period.
Table 3.
Post-operative complications according to age grouping for the 225 patients under study, n (%)
| Age group | ||||
| Group A | Group B | Group C | P value | |
| (n = 112) | (n = 57) | (n = 56) | ||
| Overall complications | 29 (25.9) | 21 (36.8) | 24 (42.9) | NS |
| Major complications | NS | |||
| (Clavien-Dindo ≥ III) | 5 (4.5) | 2 (3.5) | 1 (1.8) | |
| General complicationsa | 9 (8.1) | 13 (22.8) | 11 (19.6) | 0.045 |
| Cardiovascular | 2 (1.8) | 3 (5.3) | 7 (12.4) | |
| Respiratory | 3 (2.7) | 3 (5.3) | 2 (3.6) | |
| Urinary tract | 1 (0.9) | 4 (7) | 2 (3.6) | |
| Anemia | 1 (0.9) | 1 (1.8) | - | |
| Others | 2 (1.8) | 2 (3.5) | - | |
| Surgical complications | 22 (19.6) | 11 (19.3) | 13 (23.2) | NS |
| Anastomotic leak | 3 (2.7) | 1 (1.8) | 1 (1.8) | |
| Bowel obstruction | 1 (0.9) | 2 (3.5) | - | |
| Prolonged post-operative ileus | 7 (6.3) | 7 (12.2) | 6 (10.7) | |
| Bleeding | 2 (1.8) | 1 (1.8) | 1 (1.8) | |
| Gastrointestinal bleeding | 1 (0.9) | - | - | |
| Surgical site infection | 2 (1.8) | - | 4 (7.1) | |
| Others | 6 (5.4) | - | 1 (1.8) | |
| Infective complications | 6 (5.4) | 4 (7) | 7 (12.5) | NS |
| RBC transfusion | 6 (5.4) | 2 (3.5) | 5 (9) | NS |
| Redo Surgery | 4 (3.6) | 2 (3.5) | 1 (1.8) | NS |
| Anastomotic leak | 3 (3.6) | - | 1 (1.8) | |
| Internal hernia | 1 (.9) | 2 (3.5) | - | |
| 30-d readmission | 3 (3.6) | - | 1 (1.8) | NS |
| 30-d mortality | - | - | - | |
P < 0.05. Data are expressed as number of patients (%). RBC: Red blood cells.
As showed in Table 4, median LOS was one day shorter in Group A (5 d vs 6 d vs 6 d), although the difference did not reach statistical significance. According to the defined discharge criteria, the number of patients who could have been discharged on POD 3 progressively decreased according to age (64.3% vs 61.4% vs 48.2%). Median TRD was significantly shorter in Group A and B (P = 0.040) though DD did not differ in the 3 groups.
Table 4.
Meeting criteria for discharge according to age grouping
| Age group | ||||
| Group A | Group B | Group C | P value | |
| (n = 112) | (n = 57) | (n = 56) | ||
| Fluid intakea | 1 (0-5) | 1 (0-7) | 1 (0-7) | 0.039 |
| Soft diet | 2 (1-6) | 2 (1-13) | 2 (1-9) | NS |
| Early mobilization | 1 (0-3) | 1 (0-7) | 1 (0-4) | NS |
| Walking | 1 (0-4) | 2 (1-8) | 2 (1-8) | NS |
| Bowel open to gas | 1 (0-6) | 1 (0-4) | 1 (0-4) | NS |
| Bowel open to stoolsa | 2 (0-8) | 3 (1-9) | 3 (1-9) | 0.002 |
| Pain control with oral analgesics | 3 (2-4) | 3 (1-5) | 3 (1-4) | NS |
| Length of stay | 5 (2-40) | 5 (3-26) | 6 (3-22) | NS |
| Ready for discharge on POD 3, n (%) | 72 (64.3) | 35 (61.4) | 27 (48.2) | NS |
| Time to readiness for dischargea | 3 (3-35) | 3 (3-22) | 4 (3-18) | 0.040 |
| Discharge delay | 1 (0-8) | 2 (0-8) | 2 (0-4) | NS |
P < 0.05. Data are expressed as number of patients (%) or median (range). POD: Post-operative day.
DISCUSSION
Colorectal cancer is still the 2nd most common cause of death from neoplastic disease in men and the 3rd in women with a peak incidence between the 7th and 8th decades; over 70% of colorectal cancers are currently diagnosed in patients over the age of 65 [19]. Life expectancy, defined as the average number of years that a person at a defined age can be expected to live, is increasing worldwide. In 1985 in Italy, life expectancy at the age of 65 years was assumed to be 14.2 years for males and 17.4 years for females, in 2016 it is increased to 19.4 years for males and 22.9 years for females. Likewise, life expectancy at 75 years is expected to be 12 years for males and 14.5 years for females, one of the highest among Western countries[20]. In this regard, a steadily increasing number of colorectal cancers are expected to be operated on in older patients in the next future[21]. Most of the studies analyzing safety and feasibility of ERPs did not include elderly since, full adhesion to all fast-track items was assumed to be unfeasible in consideration of physical impairment and accompanying comorbidities[22]. This idea seems to be supported by a systematic review from Bagnall et al[23] which highlighted the lack of evidence to support ERP application at advanced ages. Conversely, several experiences focused on ERP application in the elderly highlighting its safety and efficacy on post-operative outcomes[24-28].
Our study reports the results of ERP application in a complete laparoscopic series of patients undergoing colorectal resection without age limit. Most of the recent studies still consider heterogeneous cohorts with open and laparoscopic approach[24-27] and this could lead to an underestimation of ERP benefits. We believe that minimally invasive surgery is one of the cornerstones of a successful fast-track program since it reduces surgical stress[6,7] and improves compliance to ERP items[6,25]. For this reason, we privileged to analyze the impact of age on fast-track results in a large and fully laparoscopic cohort.
Since the very beginning of ERP adoption in our unit, elderly patients were included in the protocol, consequently our results are probably affected negatively by the enlarged inclusion criteria. As previously documented[29], a good implementation of ERP requires a starting period for personnel training and acquaintance with some innovating items. We believe that most of the poorer results here described for the elderly are related to the need of more time for ERP implementation in this subgroup. For this reason, further investigation analyzing fast-track results in age groups in different periods is advisable.
When analyzing global compliance for ERP interventions, an adherence higher than 60% was achieved independently from age. The aim of a 90% compliance was obtained in 4 items: fully laparoscopic procedure without conversion to open surgery, post-operative respiratory training program, prophylactic antiemetics administration and intra-operative patient warming. Good results in early mobilization were achieved independently from age thanks to an optimal pain management. In our experience, one of the key aspects in post-operative pain management was the use of transversus abdominis pain (TAP) block that proved to reduce significantly the use of opioid analgesics and to ensure an optimal pain control[13,30], without the adverse effects of epidural analgesia, such as vasodilatation and hypotension. Limiting the side effects of opioids and epidural seems of particular benefit in elderly that are more sensitive to sedation and blood pressure variations.
The main differences in favor of younger patients were observed in carbohydrate rich drink consumption, independence from intravenous fluid stop and early walking. In our opinion these data should be interpreted as the result of the association of a more protective attitude of health personnel and a stronger reluctance of the elderly to get out of bed or drink after the day of surgery. These results confirm the experience of Feroci et al[31] which reported significant differences both in early liquid and solid diet intake when comparing patients younger or older than 75 years old. The need for an extra effort from the caregivers should be stressed together with a stronger information on ERP items safety for personnel and patients. Later resumption of walking in the elderly was probably related to a lower rate of early UC removal. In a recent review of the literature[32], this item has proved to be one of the most difficult goals to achieve, although the presented results should be considered generally good[24,35]. In our opinion, room for further improvement in GC, is to be found in strict adhesion to early UC removal and iv fluid withdrawal which should lead to a higher rate of patients’ early mobilization.
Regarding 30-d post-operative outcomes, no mortality was observed in the 225 patients. Our data showed that 57% of patients aged more than 75 years old did not experience any complication and only one patient experienced a major complication requiring reiterative surgery (anastomotic leak); readmission rate was low as well. As previously assessed[27], these results confirm the safety of ERPs at all ages despite a significantly higher comorbidity rate. Considering the 3 groups, the occurrence of surgery-related adverse events was comparable whilst, the rate of general complications was almost doubled in Groups B and C compared to Group A. This difference was mainly related to the progressive increase in cardiovascular complications observed with age increasing (2% vs 5% vs 12%). Conversely, no differences were found in respiratory complications rate that, in accordance with recent literature (2%-7%), was less than 5% in the 3 groups[25,28]. These results confirm the role of ERPs in preventing pulmonary complications and support the data denying a relationship between early oral intake and higher risks of inhalation.
Surgery specific complications were equally distributed among the 3 groups, with an overall anastomotic leak rate of 2.2% and prolonged post-operative ileus rate of 8.9%, in line with those reported in other studies[24,26,33]. In our experience, the median overall LOS of 5 d (2-40) was in line with the recent European literature[24-27]. Elderly patients equally benefitted from ERP as younger patients in terms of LOS although, fewer patients fulfilled the clinical discharge criteria on POD 3 so that, in accordance to the results from the PeriOperative Italian Society Registry, time to readiness for discharge was one day longer in patients aged more than 75 years[25]. When analyzing the causes for a delayed discharge, logistical challenges such as home care or hosting structure availability, are the most important factors[24]. Social and organizational issues or further care factors can account for about 11.5% of failures to discharge[22,34]. In our study delayed discharge was similar in the 3 groups proving that adequate counselling and family information on post-operative fast-track course reduce the time delay between time to readiness for discharge and the actual return to home or hosting structure for elderly patients.
Our study has some major limitations that should be mentioned. First, although data were prospectively acquired, the study design is retrospective. Therefore, data on specific scores evaluating patients at risk for surgery as ColoRectal Physiological and Operative Severity Score for the enumeration of Mortality and Morbidity (CR-POSSUM) score, were not included in data collection. Although colorectal CR-POSSUM and other frailty indexes[11] have proved to identify patients at risk for possible failure of ERPs[24,35], these scores tend to overestimate morbidity and mortality, since firstly elaborated for open surgery[36]. Considering this drawback and the limited use in clinical practice, such information was not considered in data collection. We should also consider that the limited number of patients in Group B and C could have limited the evaluation of confounding factors such as the higher number of rectal resections in Group A. Analysis of larger populations also considering multicentric study design should be carried out to reduce influence of confounding factors. Second, lack of analysis of patients pre-operatively excluded from the ERP. At the time we started our ERP, we established to include all patients independently from age and extent of colorectal resection. But severe comorbidities were considered as exclusions criteria since perioperative management could have been altered greatly. Recently, Braga et al[25] reported that older patients with high ASA grade (III-IV) do not require a specifically tailored pathway and can benefit from ERP both in terms of morbidity and LOS[25]. In our experience patients older than 75 years required post-operative ITU stay in 52% of the cases (15 out of 29; data not shown). Furthermore, two third of patients were excluded from study protocol due to their own or family refusal and due to severe neurological impairment, that hampered their participation into ERP (Figure 1). A specifically designed protocol with tailored goals has now been implemented in our practice since, it is our belief that the two subgroups need to be managed differently in order to optimize post-operative results in both populations.
Third, a complete prehabilitation program considering all aspects influencing post-operative short-term results, such as nutritional status, anemia correction, improvement of muscle function, etc., was not regularly accomplished; herein the idea that short-term outcomes could be further improved. A comprehensive prehabilitation program has been recently implemented in our clinical practice for all patients undergoing colorectal resection although, a major benefit is expected for elderly population.
CONCLUSION
Our study confirms that ERP can be safely and successfully applied to most of the elderly patients undergoing laparoscopic colorectal resection who are able and willing to participate in fast-track protocols. Although patients aged more than 75 years showed a lower GC rate and required a longer time to achieve discharge criteria (TRD), complication rate, readmission rates and LOS were comparable to those of younger patients. The value added from standardized prehabilitation protocols in improving short-term outcomes in elderly population should be further evaluated.
ARTICLE HIGHLIGHTS
Research background
Life expectancy is increasing worldwide, and a growing number of colorectal resections are expected to be operated in older patients in the next future. Age has been traditionally considered a risk factor for poor surgical outcomes and delayed recovery after surgery. After the advent of laparoscopy, more recently, enhanced recovery protocols (ERP) aimed at further improvement in surgical results for elderly patients.
Research motivation
Fast-track protocols have proved their efficacy in improving length of stay, morbidity and recovery after colorectal surgery. Nevertheless, most studies have excluded elderly patients assuming greater frailty and lower compliance to ERP. Moreover, few papers have evaluated the most challenging recovery goals for this population.
Research objectives
The main objectives of this study were to evaluate the feasibility and safety of ERP in elderly patients undergoing colorectal resection with minimally invasive approach. Global compliance to fast-track items was evaluated together with its impact on discharge delay.
Research methods
Our prospectively maintained departmental database of patients undergoing colorectal resection between March 2014 and July 2018 was examined to identify patients enrolled in fast-track protocol. According to the World Health Organization’s definition of elderly and old elderly, patients were divided in 3 groups (Group A, ≤ 65 years old, Group B, 66-75 years old and Group C, > 76 years old). Clinic and pathologic characteristics of the three groups were compared. Further analysis included short-term outcomes and recovery results considering fast-track protocol compliance as the amount of ERP’s items successfully achieved.
Research results
Of 317 patients who underwent laparoscopic colorectal resection during the study period, 225 met the inclusion criteria and were divided in Group A (n = 112), Group B (n = 57) and Group C (n = 56). Although a higher rate of patients with more than two comorbidities was observed in Group B and C (P < 0.001), major complication, reoperation and readmission rates were comparably low among the three groups. Whilst the median time to fulfil the proposed discharge criteria was significantly shorter in Group A and B (P = 0.040), median length of hospital stay (LOS) was comparable within groups. The most difficult ERP goals to be achieved in the elderly were carbohydrate rich drink consumption (P = 0.022) and walking resumption on the first post-operative day (P = 0.032). Furthermore, Group C resulted less efficient in early urinary catheter removal (P = 0.013).
Research conclusions
This study found no age-related differences in the main short-term outcomes after laparoscopic colorectal resection performed within a fast-track protocol. Morbidity, reoperation and surgical complication rates were similar in the three groups. Even tough elderly patients required more time to fulfil discharge criteria no differences in LOS were observed. Global compliance within Group B and C was satisfying although room for specific items’ improvement was highlighted.
Research perspectives
Our results suggest that elderly patients can be safely enrolled within ERP. Reasons for fast-track goals failure should be registered in prospectively collected databases and considered for further research. The evidence of characteristic age-related difficulties in achieving ERP objectives could then lead to the definition of specific targets for prehabilitation programs.
ACKNOWLEDGEMENTS
We would like to thank Brittany Davis MD for the help in English language revision without receiving funding and for having kindly supported the study.
Footnotes
Institutional review board statement: The study was reviewed and approved by the Ethics Committee of University of Verona, Verona, Italy, with ID number: 53538.
Informed consent statement: Patients were not required to give informed consent to the study because the analysis used anonymous data that were obtained after each patient agreed to treatment by written consent.
Conflict-of-interest statement: The authors have no conflicts of interest to declare.
Data sharing statement: Deidentified participant data from prospectively collected database are available upon reasonable request to the corresponding author.
STROBE statement: The authors have read the STROBE Statement - checklist of items, and the manuscript was prepared and revised according to the STROBE Statement - checklist of items.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Peer-review started: April 19, 2019
First decision: August 2, 2019
Article in press: October 18, 2019
Specialty type: Gastroenterology and hepatology
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Martini F, Ng DCK, Wang DR S-Editor: Ma RY L-Editor: A E-Editor: Qi LL
Contributor Information
Corrado Pedrazzani, Division of General and Hepatobiliary Surgery, Department of Surgical Sciences, Dentistry, Gynecology and Pediatrics, University of Verona Hospital Trust, Verona 37134, Italy. corrado.pedrazzani@univr.it.
Cristian Conti, Division of General and Hepatobiliary Surgery, Department of Surgical Sciences, Dentistry, Gynecology and Pediatrics, University of Verona Hospital Trust, Verona 37134, Italy.
Giulia Turri, Division of General and Hepatobiliary Surgery, Department of Surgical Sciences, Dentistry, Gynecology and Pediatrics, University of Verona Hospital Trust, Verona 37134, Italy.
Enrico Lazzarini, Division of General and Hepatobiliary Surgery, Department of Surgical Sciences, Dentistry, Gynecology and Pediatrics, University of Verona Hospital Trust, Verona 37134, Italy.
Marzia Tripepi, Division of General and Hepatobiliary Surgery, Department of Surgical Sciences, Dentistry, Gynecology and Pediatrics, University of Verona Hospital Trust, Verona 37134, Italy.
Giovanni Scotton, Division of General and Hepatobiliary Surgery, Department of Surgical Sciences, Dentistry, Gynecology and Pediatrics, University of Verona Hospital Trust, Verona 37134, Italy.
Matteo Rivelli, Division of General and Hepatobiliary Surgery, Department of Surgical Sciences, Dentistry, Gynecology and Pediatrics, University of Verona Hospital Trust, Verona 37134, Italy.
Alfredo Guglielmi, Division of General and Hepatobiliary Surgery, Department of Surgical Sciences, Dentistry, Gynecology and Pediatrics, University of Verona Hospital Trust, Verona 37134, Italy.
References
- 1.Gustafsson UO, Scott MJ, Schwenk W, Demartines N, Roulin D, Francis N, McNaught CE, Macfie J, Liberman AS, Soop M, Hill A, Kennedy RH, Lobo DN, Fearon K, Ljungqvist O Enhanced Recovery After Surgery (ERAS) Society, for Perioperative Care; European Society for Clinical Nutrition and Metabolism (ESPEN); International Association for Surgical Metabolism and Nutrition (IASMEN) Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations. World J Surg. 2013;37:259–284. doi: 10.1007/s00268-012-1772-0. [DOI] [PubMed] [Google Scholar]
- 2.Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg. 2002;183:630–641. doi: 10.1016/s0002-9610(02)00866-8. [DOI] [PubMed] [Google Scholar]
- 3.Nicholson A, Lowe MC, Parker J, Lewis SR, Alderson P, Smith AF. Systematic review and meta-analysis of enhanced recovery programmes in surgical patients. Br J Surg. 2014;101:172–188. doi: 10.1002/bjs.9394. [DOI] [PubMed] [Google Scholar]
- 4.King PM, Blazeby JM, Ewings P, Longman RJ, Kipling RM, Franks PJ, Sheffield JP, Evans LB, Soulsby M, Bulley SH, Kennedy RH. The influence of an enhanced recovery programme on clinical outcomes, costs and quality of life after surgery for colorectal cancer. Colorectal Dis. 2006;8:506–513. doi: 10.1111/j.1463-1318.2006.00963.x. [DOI] [PubMed] [Google Scholar]
- 5.Aarts MA, Okrainec A, Glicksman A, Pearsall E, Victor JC, McLeod RS. Adoption of enhanced recovery after surgery (ERAS) strategies for colorectal surgery at academic teaching hospitals and impact on total length of hospital stay. Surg Endosc. 2012;26:442–450. doi: 10.1007/s00464-011-1897-5. [DOI] [PubMed] [Google Scholar]
- 6.Vlug MS, Wind J, Hollmann MW, Ubbink DT, Cense HA, Engel AF, Gerhards MF, van Wagensveld BA, van der Zaag ES, van Geloven AA, Sprangers MA, Cuesta MA, Bemelman WA LAFA study group. Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study) Ann Surg. 2011;254:868–875. doi: 10.1097/SLA.0b013e31821fd1ce. [DOI] [PubMed] [Google Scholar]
- 7.Spanjersberg WR, van Sambeeck JD, Bremers A, Rosman C, van Laarhoven CJ. Systematic review and meta-analysis for laparoscopic versus open colon surgery with or without an ERAS programme. Surg Endosc. 2015;29:3443–3453. doi: 10.1007/s00464-015-4148-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lyon A, Payne CJ, Mackay GJ. Enhanced recovery programme in colorectal surgery: does one size fit all? World J Gastroenterol. 2012;18:5661–5663. doi: 10.3748/wjg.v18.i40.5661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahmed J, Khan S, Lim M, Chandrasekaran TV, MacFie J. Enhanced recovery after surgery protocols - compliance and variations in practice during routine colorectal surgery. Colorectal Dis. 2012;14:1045–1051. doi: 10.1111/j.1463-1318.2011.02856.x. [DOI] [PubMed] [Google Scholar]
- 10.Reisinger KW, van Vugt JL, Tegels JJ, Snijders C, Hulsewé KW, Hoofwijk AG, Stoot JH, Von Meyenfeldt MF, Beets GL, Derikx JP, Poeze M. Functional compromise reflected by sarcopenia, frailty, and nutritional depletion predicts adverse postoperative outcome after colorectal cancer surgery. Ann Surg. 2015;261:345–352. doi: 10.1097/SLA.0000000000000628. [DOI] [PubMed] [Google Scholar]
- 11.Keller DS, Bankwitz B, Nobel T, Delaney CP. Using frailty to predict who will fail early discharge after laparoscopic colorectal surgery with an established recovery pathway. Dis Colon Rectum. 2014;57:337–342. doi: 10.1097/01.dcr.0000442661.76345.f5. [DOI] [PubMed] [Google Scholar]
- 12.Hendry PO, Hausel J, Nygren J, Lassen K, Dejong CH, Ljungqvist O, Fearon KC Enhanced Recovery After Surgery Study Group. Determinants of outcome after colorectal resection within an enhanced recovery programme. Br J Surg. 2009;96:197–205. doi: 10.1002/bjs.6445. [DOI] [PubMed] [Google Scholar]
- 13.Pedrazzani C, Conti C, Mantovani G, Fernandes E, Turri G, Lazzarini E, Menestrina N, Ruzzenente A, Guglielmi A. Laparoscopic colorectal surgery and Enhanced Recovery After Surgery (ERAS) program: Experience with 200 cases from a single Italian center. Medicine (Baltimore) 2018;97:e12137. doi: 10.1097/MD.0000000000012137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pedrazzani C, Menestrina N, Moro M, Brazzo G, Mantovani G, Polati E, Guglielmi A. Local wound infiltration plus transversus abdominis plane (TAP) block versus local wound infiltration in laparoscopic colorectal surgery and ERAS program. Surg Endosc. 2016;30:5117–5125. doi: 10.1007/s00464-016-4862-5. [DOI] [PubMed] [Google Scholar]
- 15.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fiore JF, Jr, Faragher IG, Bialocerkowski A, Browning L, Denehy L. Time to readiness for discharge is a valid and reliable measure of short-term recovery after colorectal surgery. World J Surg. 2013;37:2927–2934. doi: 10.1007/s00268-013-2208-1. [DOI] [PubMed] [Google Scholar]
- 17.Pedrazzani C, Moro M, Mantovani G, Lazzarini E, Conci S, Ruzzenente A, Lippi G, Guglielmi A. C-reactive protein as early predictor of complications after minimally invasive colorectal resection. J Surg Res. 2017;210:261–268. doi: 10.1016/j.jss.2016.11.047. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. Definition of an older or elderly person. [accessed 2018 December 30] Available from: http://www.who.int/healthinfo/survey/ageingdefnolder/en/index.html. [Google Scholar]
- 19.Stępień R, Głuszek S, Kozieł D, Kaczmarczyk M. The risk of surgical treatment in patients aged 85+, with special consideration of colorectal cancer. Pol Przegl Chir. 2014;86:132–140. doi: 10.2478/pjs-2014-0025. [DOI] [PubMed] [Google Scholar]
- 20.EUROSTAT. [accessed 2018 December 30] Available from: http://ec.europa.eu/eurostat/data/database?node_code=demo_mlexpec.
- 21.Nascimbeni R, Di Fabio F, Di Betta E, Salerni B. The changing impact of age on colorectal cancer surgery. A trend analysis. Colorectal Dis. 2009;11:13–18. doi: 10.1111/j.1463-1318.2008.01491.x. [DOI] [PubMed] [Google Scholar]
- 22.Pawa N, Cathcart PL, Arulampalam TH, Tutton MG, Motson RW. Enhanced recovery program following colorectal resection in the elderly patient. World J Surg. 2012;36:415–423. doi: 10.1007/s00268-011-1328-8. [DOI] [PubMed] [Google Scholar]
- 23.Bagnall NM, Malietzis G, Kennedy RH, Athanasiou T, Faiz O, Darzi A. A systematic review of enhanced recovery care after colorectal surgery in elderly patients. Colorectal Dis. 2014;16:947–956. doi: 10.1111/codi.12718. [DOI] [PubMed] [Google Scholar]
- 24.Gonzalez-Ayora S, Pastor C, Guadalajara H, Ramirez JM, Royo P, Redondo E, Arroyo A, Moya P, Garcia-Olmo D. Enhanced recovery care after colorectal surgery in elderly patients. Compliance and outcomes of a multicenter study from the Spanish working group on ERAS. Int J Colorectal Dis. 2016;31:1625–1631. doi: 10.1007/s00384-016-2621-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Braga M, Pecorelli N, Scatizzi M, Borghi F, Missana G, Radrizzani D PeriOperative Italian Society. Enhanced Recovery Program in High-Risk Patients Undergoing Colorectal Surgery: Results from the PeriOperative Italian Society Registry. World J Surg. 2017;41:860–867. doi: 10.1007/s00268-016-3766-9. [DOI] [PubMed] [Google Scholar]
- 26.Tejedor P, Pastor C, Gonzalez-Ayora S, Ortega-Lopez M, Guadalajara H, Garcia-Olmo D. Short-term outcomes and benefits of ERAS program in elderly patients undergoing colorectal surgery: a case-matched study compared to conventional care. Int J Colorectal Dis. 2018;33:1251–1258. doi: 10.1007/s00384-018-3057-z. [DOI] [PubMed] [Google Scholar]
- 27.Hallam S, Rickard F, Reeves N, Messenger D, Shabbir J. Compliance with enhanced recovery protocols in elderly patients undergoing colorectal resection. Ann R Coll Surg Engl. 2018;100:570–579. doi: 10.1308/rcsann.2018.0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pirrera B, Lucchi A, Gabbianelli C, Alagna V, Martorelli G, Berti P, Panzini I, Fabbri E, Garulli G. E.R.A.S. pathway in colorectal surgery in elderly: Our experience: A retrospective cohort study. Int J Surg. 2017;43:101–106. doi: 10.1016/j.ijsu.2017.05.013. [DOI] [PubMed] [Google Scholar]
- 29.Pędziwiatr M, Kisialeuski M, Wierdak M, Stanek M, Natkaniec M, Matłok M, Major P, Małczak P, Budzyński A. Early implementation of Enhanced Recovery After Surgery (ERAS®) protocol - Compliance improves outcomes: A prospective cohort study. Int J Surg. 2015;21:75–81. doi: 10.1016/j.ijsu.2015.06.087. [DOI] [PubMed] [Google Scholar]
- 30.Park JS, Choi GS, Kwak KH, Jung H, Jeon Y, Park S, Yeo J. Effect of local wound infiltration and transversus abdominis plane block on morphine use after laparoscopic colectomy: a nonrandomized, single-blind prospective study. J Surg Res. 2015;195:61–66. doi: 10.1016/j.jss.2014.12.034. [DOI] [PubMed] [Google Scholar]
- 31.Feroci F, Lenzi E, Baraghini M, Garzi A, Vannucchi A, Cantafio S, Scatizzi M. Fast-track surgery in real life: how patient factors influence outcomes and compliance with an enhanced recovery clinical pathway after colorectal surgery. Surg Laparosc Endosc Percutan Tech. 2013;23:259–265. doi: 10.1097/SLE.0b013e31828ba16f. [DOI] [PubMed] [Google Scholar]
- 32.Launay-Savary MV, Mathonnet M, Theissen A, Ostermann S, Raynaud-Simon A, Slim K GRACE (Groupe francophone de Réhabilitation Améliorée après Chirurgie) Are enhanced recovery programs in colorectal surgery feasible and useful in the elderly? A systematic review of the literature. J Visc Surg. 2017;154:29–35. doi: 10.1016/j.jviscsurg.2016.09.016. [DOI] [PubMed] [Google Scholar]
- 33.Naef M, Käsemodel GK, Mouton WG, Wagner HE. Outcome of colorectal cancer surgery in the early fast-track era with special regard to elderly patients. Int Surg. 2010;95:153–159. [PubMed] [Google Scholar]
- 34.Maessen JM, Dejong CH, Kessels AG, von Meyenfeldt MF Enhanced Recovery After Surgery (ERAS) Group. Length of stay: an inappropriate readout of the success of enhanced recovery programs. World J Surg. 2008;32:971–975. doi: 10.1007/s00268-007-9404-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Renz BW, Kasparek MS, Seeliger H, Worthley DL, Jauch KW, Kreis ME, Smith MJ, Mueller MH. The CR-POSSUM Risk Calculator Predicts Failure of Enhanced Recovery after Colorectal Surgery. Acta Chir Belg. 2015;115:20–26. [PubMed] [Google Scholar]
- 36.Bagnall NM, Pring ET, Malietzis G, Athanasiou T, Faiz OD, Kennedy RH, Jenkins JT. Perioperative risk prediction in the era of enhanced recovery: a comparison of POSSUM, ACPGBI, and E-PASS scoring systems in major surgical procedures of the colorectal surgeon. Int J Colorectal Dis. 2018;33:1627–1634. doi: 10.1007/s00384-018-3141-4. [DOI] [PMC free article] [PubMed] [Google Scholar]