Maternal health in the United States is in crisis. There are almost 4 million births every year in this country.1 Delivery is the most frequent cause of hospitalization,2 cesarean deliveries remain the most common surgery performed,3 and the United States spends almost twice as much as other high-income countries on medical care.4 Yet, more mothers are dying from pregnancy-related causes in this country than in any other high-income country.5 Every year in the United States approximately 700 woman die from pregnancy-related causes.6
Even more concerning is the fact that maternal death rates in the US have doubled over the last 20 years, albeit partly due to improved ascertainment, while other high-income countries have reduced their rates.7 As maternal deaths rise, so, too, do severe complications from childbirth. For every maternal death, over 100 women suffer severe maternal morbidity, resulting in over 50,000 women every year experiencing a life-threatening complication related to childbirth.8 Pregnancy and childbirth are often framed as organic stages in a woman’s reproductive journey, but these numbers and statistics make it evident that healthy outcomes for mothers are not guaranteed.
Our poor performance in reducing US maternal mortality rates is linked to significant and persistent racial and ethnic disparities in such rates. Black women are three to four times more likely to die from pregnancy-related causes than are white women.9 Native Americans, some Asians and some Latinas also experience a higher number of maternal deaths relative to white women.10 Similarly, significant racial and ethnic disparities exist for severe maternal morbidity rates in the United States, with black and Latina women having elevated rates.11
Despite these alarming trends in maternal mortality and severe maternal morbidity rates and entrenched racial and ethnic disparities in such outcomes, 60% of pregnancy-related deaths and severe maternal morbidities in the United States are thought to be preventable.6, A recent Centers for Disease Control and Prevention (CDC) review of maternal deaths across nine states found that the deaths were related to clinician, facility and system factors, such as inadequate training, missed or delayed diagnosis of complications, poor communication and lack of coordination between clinicians.6,7 These findings and others reinforce the fact that any efforts to reduce maternal mortality must focus on ensuring quality and safety of maternity care for all women. Further, given the entrenched racial and ethnic disparities in these outcomes, these efforts must also be rooted in health equity. The purpose of this article is to frame the maternal mortality crisis and identify ways to narrow the racial/ethnic disparity gap within a quality of care framework.
Definitions
The World Health Organization defines maternal mortality as the death of a woman while pregnant or within 42 days of termination of pregnancy from any cause related to or aggravated by pregnancy or its management but not from incidental or accidental causes and this is the definition utilized for international comparisons.13 A pregnancy-related mortality is defined as the death of a woman while pregnant or within 1 year of termination of pregnancy from causes related to the pregnancy and this statistic is monitored by the CDC.13
Health disparities are defined as “a particular type of health difference that is closely linked with economic, social or environmental disadvantage.”14 Many experts have emphasized the importance of clarity about the concepts of health disparities and health equity and stressed the underlying notion of social justice.15,16 A useful definition is one by Dr. Paula Braveman: “Health equity and health disparities are intertwined. Health equity means social justice in health (i.e. no one is denied the possibility to be healthy for belonging to a group that has historically been economically/ socially disadvantaged). Health disparities are the metric we use to measure progress toward achieving health equity.”15
Contributing factors
Developing targeted and actionable interventions requires untangling a complex web of factors that contribute to racial disparities in maternal healthcare. It is useful to conceptualize the components that contribute to maternal death as consisting of a vertical dimension, representing agents involved in the healthcare system from institution to individual, and a horizontal dimension comprising a longitudinal continuum of care, from preconception to maternity and beyond, including the postpartum period and inter-pregnancy intervals. The intersections between the horizontal and vertical elements represent touch points between mother and clinicians that shape and determine the patient’s health outcome.
Using this conceptual framework, we can start at the individual level. A patient has a set of intrinsic characteristics that determine her health status. Patient factors include non-modifiable items like age and race and are also linked to social determinants of health, including education, literacy, employment and poverty, which ultimately mold a patient’s knowledge, beliefs, and perceptions of health.17 The external environment also informs a patient’s health status. Women living in poorer communities and neighborhoods often have less access to healthy foods and safe parks, are exposed to more toxins, and are at higher risk for poor perinatal outcomes.18–20 Comorbid illnesses complicate a patient’s medical story even more and women from racial and ethnic minority communities have a higher prevalence of common diseases like hypertension, diabetes, and obesity.21
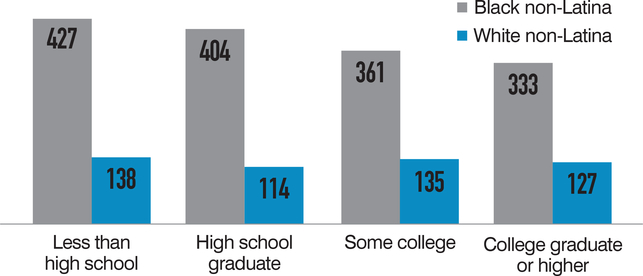
It is important to note the ways in which structural racism have shaped the health and opportunity for women of color. Historical and economic forces, including restrictions on housing options, jobs and education, have entrenched women who belong to racial and ethnic minority groups in cycles of marginalization and inequality.22,23 Social determinants are important contributors to racial and ethnic disparities in maternal outcomes, but they do not fully explain the higher rate of maternal death and severe maternal morbidities among racial and ethnic minority women. For example, in New York City, a black woman with a college education is almost three times as likely to suffer severe maternal morbidity as a white woman who has less than a high school education (Figure 1).24
FIGURE 1. Severe maternal morbidity by education attainment, New York City.
Source: New York City Department of Health and Mental Hygiene (2016).Severe Maternal Morbidity in New York City 2008–2012. New York, NY.
Clinicians, including nurses, midwives and doctors, as well as support persons such as doulas, are partners in a patient’s health throughout the course of her life. A clinician’s’ knowledge and experience contribute to a patient’s preparedness and comfort with her pregnancy, labor and delivery and the postpartum period. This relationship can be influenced by implicit bias, cultural competence and communication skills.25 Implicit bias refers to behaviors in reaction to a patient’s characteristics like age, race, ethnicity, gender, sexual orientation, physicality, and disability that shape our behavior and actions and informs clinical decisions.26 These biases are deeply rooted and are deployed unconsciously.26
Quality of care for pregnant women is important across the care continuum. Delivery care represents another significant “touch point” between the patient and clinician, where severe maternal morbidity and mortality often occur and where racial and ethnic disparities in maternal outcomes manifest. Data suggest that racial and ethnic disparities in severe maternal morbidity and mortality are due to disparities both within (intra-hospital) and between institutions (interhospital). For example, in the United States, nearly 75% of black women deliver at a quarter of all delivery hospitals while only 18% of white women deliver in those same hospitals. Both black and white women have higher severe maternal morbidity rates at those hospitals regardless of patient risk factors.27
Intra-hospital differences also contribute to racial/ethnic disparities in maternal mortality rates. In a study examining how racial/ethnic minority-serving hospitals performed on 15 birth-related indicators, significant racial/ethnic disparities in delivery-related indicators were reported within each type of hospital (e.g. black-serving, white-serving).28
Delivery care is only one part of the care continuum for pregnant women. Preconception care is critical for optimizing contraceptive counseling, management of chronic illness and addressing the health needs of women. There is substantial evidence that racial/ethnic women have less access to preconception care.29 Antenatal care is crucial to optimizing the health of mom and fetus and we know that access differs across the United States, depending on insurance status and race/ethnicity.30 Postpartum care has been given less emphasis in traditional frameworks of maternal healthcare and yet this period of time presents a window of opportunity to address both physical and emotional needs of mothers from gestational diabetes to postpartum depression. However, rates of postpartum visits are low: 16% to 36% of women do not attend the 6-week follow-up visit and those who do report inadequate care and guidance at that time.31,32
Eight steps for narrowing gaps
Actionable steps are required if we are to improve maternal healthcare and address the unacceptable racial and ethnic disparities that exist. Many of the recommended steps will improve care for all pregnant women. Additional steps address the unique circumstances that many women of color face when encountering the healthcare system. Although not every initiative has a strong evidence base, the proposed recommendations are rooted in lessons from other areas of medicine, expert opinion, quality improvement science, and the extensive work done by the Council on Patient Safety in Women’s Health Care and the Alliance for Innovation in Maternal Health (https://safehealthcareforeverywoman.org/patient-safety-bundles/reduction-of-peripartum-racialethnic-disparities).33 We present eight recommended steps to narrow disparities within a quality-of-care framework (Table 1).
TABLE 1.
Eight steps to narrow disparities across the care
| ■ Enhance communications |
| ■ Address implicit bias |
| ■ Implement a disparities dashboard |
| ■ Perform enhanced maternal mortality and severe maternal morbidity reviews |
| ■ Standardize care on labor and delivery |
| ■ Promote a culture of equity |
| ■ Develop new models of care across the care continuum |
| ■ Engage key stakeholders |
ENHANCE COMMUNICATION AND IMPLEMENT UNCONSCIOUS BIAS TRAINING.
Improving communication between patient and provider can avoid mismanagement, delays or failure in diagnosis and poor patient advocacy. Shared decision- making is a practice rooted in patient-centered care. It entails a process of weighing patient’s goals, decisions and expectations against clinical guidelines and best practices in an open and honest conversation between patients and clinicians.34 Shared decision-making is necessary to develop and deliver treatment plans that address differences and narrow disparities. Relaying clinical information effectively may require the use of aids and teach-back methods to appropriately convey risk and benefits, given cultural and language barriers.35 Assessing non-English language proficiency and educating staff on the availability and need for interpreter services are important for creating a culture of equity as it relates to patient empowerment and access to knowledge.36 Addressing implicit bias is less concrete but nevertheless needed. Tactics include individuation, or rather “intentionally focusing on individual patients’ information apart from their social group” 37 Implicit bias/unconscious bias trainings are now being offered at some healthcare institutions. Two additional tactics include incorporating cultural competency as part of training currículums and ensuring diversity in clinicians and staff, both of which will improve the quality of communication skills.38
IMPLEMENT DISPARITIES DASHBOARD AND PERFORM ENHANCED MATERNAL MORTALITY AND SEVERE MATERNAL MORBIDITY REVIEWS.
To implement a disparities dashboard, a few steps are needed. First, self-identified race and ethnicity as well as language and place of birth should be captured in the medical record. There is evidence on how to train staff to ask these questions and how to best explain to patients why it is important to collect this information.39,40 The next step is to review quality metrics stratified by race and ethnicity to ensure hospitals are aware of their performance for different racial and ethnic groups. Results from the disparities dashboard should be regularly shared with leadership and staff.41 Next, quality improvement tools should be used to address the disparities identified. Ultimately, by putting hospital system performance under review, quality improvement tools can be deployed to narrow the disparity gap. Learning from every death and severe complication is a very important step to preventing future events. As recommended in the recent Alliance for Innovation on Maternal Health (AIM) bundle, multidisciplinary case reviews are an essential part of the process and should consider the role of race, ethnicity, language, poverty, literacy and racism.33
STANDARDIZE CARE AND BUILD A CULTURE OF EQUITY.
While quality improvement tools are often designed to focus on human error and accordingly, prompt system redesign, they can also address gaping disparities. Given that the majority of maternal deaths and severe complications related to childbirth and deliveries in the United States are preventable, we need to ensure equal standards of care for patients of all racial and ethnic groups. Standardization of care with use of the AIM bundles, such as those directed at hypertension, hemorrhage, and venous thrombotic disease, is a first step in the right direction.32 Utilization of quality improvement tools such as triggers, protocols, drills, evidence-based practices, policies and procedures, checklists, simulation training, and other items is crucial not only for quality improvement initiatives but also for ensuring equal standards across hospitals.17,41,42 Team training is also recommended by various oversight committees, including the Institute for Healthcare Improvement.17
We must promote a culture of equity in our institutions by employing many of the tools we have used to emphasize a culture of safety, in addition to acknowledging, discussing, measuring, monitoring, and utilizing continuous quality improvement efforts to address disparities.32 Reports of inequity, miscommunication, and disrespect warrant careful review to identify system-level opportunities to better meet the needs of racial and ethnic minority population.33
DEVELOP NEW MODELS OF CARE ACROSS THE CONTINUUM.
New models that promote women’s health across the life course need to be developed to address our fragmented healthcare system. Preconception care should include development of a reproductive plan and judgment-free and noncoercive contraceptive counseling25 and address questions and concerns regarding family planning. Counseling at this stage allows for early intervention for health conditions and behaviors such as obesity, hypertension, and tobacco use and can ultimately improve patient health status before pregnancy.
Preconception care can also extend to inter-pregnancy intervals with emphasis on childbirth spacing. While prenatal care is known to be crucial for ensuring healthy perinatal outcomes, timing and receipt of prenatal care can be low among low-income women of color.21 Structuring care differently might yield better outcomes versus traditional models. Group prenatal care models such as CenteringPregnancy provide prenatal care in group settings according to due date and have demonstrated some promising results, though the impact of reducing maternal deaths or severe complications through these initiatives has yet to be studied.21,43 They do, however, offer alternative models for health empowerment for mothers through their pregnancies. Similarly, case management and patient navigation programs can assist in coordinating postpartum care, an important touchpoint for women following pregnancy.44 The importance of comprehensive care in the postpartum period has recently been emphasized by the American College of Obstetricians and Gynecologists (ACOG).45
ENGAGE KEY STAKEHOLDERS.
Rallying key stakeholders allows for wide implementation of multidisciplinary initiatives to tackle maternal mortality. Stakeholders can include state agencies, organizations like ACOG or the American College of Nurse-Midwives, health care systems, patient advocacy groups, local communities and patients.43 California has created a model of organizing public-private partnerships through coordinated efforts of the California Department of Public Heath and the California Maternal Quality Care Collaborative (CMQCC). In that state, rates of maternal death have been reduced by one-half (from 13.1 to 7.2 for every 100,000 live births).46
The approach included four distinct parts, as outlined by the CMQCC:
using public health data to develop quality improvement measures on causes of death and pregnancy-related complication;
engaging public and private stakeholders;
establishing a data system to track and monitor quality improvement efforts; and
affecting change through larger interventions by coordinating between clinical providers and public health services.
Mobilizing the California Department of Public Health, CMQCC, consisting of various stakeholders and the California Pregnancy-Associated Mortality Review committee, created a larger network of ideas, resources, and funding streams. While health equity was not a primary goal of the initiative, California displayed an overall reduction in maternal mortality for all racial and ethnic groups from 1999 to 2001 through 2011 to 2013, although the mortality disparity ratio, the gap between black and white women, remained the same.43
Conclusion
Addressing racial and ethnic disparities within the larger maternal mortality crisis requires targeted efforts towards modifiable factors, grounded in healthy equity and quality improvement. Promoting a culture of equity involves addressing implicit bias and individual and systemic racism, while also utilizing quality improvement tools and transforming culture. Enhanced communication, reduced bias, careful monitoring, and improvement of performance for all of our populations and engagement of key stakeholders can begin to narrow the maternal mortality and severe maternal morbidity disparity gaps. Ultimately, these actions will elevate the quality of care received by all mothers, including those who belong to racial/ethnic communities. ■
QUICK TAKES.
Maternal morbidity and mortality rates in the US are linked to significant and persistent racial and ethnic disparities.
Recommendations are based on lessons from other areas of medicine as well as expert opinions, quality improvment science, and extensive work by patient safety and womens health care organizations.
Given the entrenched racial and ethnic disparities in these outcomes, these efforts must also be rooted in health equity.
Biography
DR HOWELL

MS AHMED
Footnotes
DISCLOSURES National Institute on Minority Health and Health Disparities (R01MD007651)
The Blavatnik Family Foundation
This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Contributor Information
DR ELIZABETH A. HOWELL, The Blavatnik Family Women’s Health Research Institute, Mount Sinai Health System vice chair for research and professor in the Department of Obstetrics, Gynecology, and Reproductive Science at Icahn School of Medicine at Mount Sinai, New York..
MS ZAINAB N. AHMED, Icahn School of Medicine at Mount Sinai, New York..
REFERENCES
- 1.Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P Births: Final data for 2016. Natl Vital Stat Rep 2018. January;67(1):1–55. [PubMed] [Google Scholar]
- 2.Hall MJ, DeFrances CJ, Williams SN, Golo-sinskiy A, Schwartzman A. National Hospital Discharge Survey: 2007 summary. Natl Health Stat Report. 2010. October 26;(29):1–20, 24. [PubMed] [Google Scholar]
- 3.McDermott KW (IBM Watson Health), Freeman WJ (AHRQ), Elixhauser A (AHRQ). Overview of Operating Room Procedures During Inpatient Stays in U.S. Hospitals, 2014 HCUP Statistical Brief #233. December 2017. Agency for Healthcare Research and Quality, Rockville, MD: Available at www.hcup-us.ahrq.gov/reports/statbriefs/sb233-Operating-Room-Procedures-United-States-2014.pdf Accessed December 2, 2018. [PubMed] [Google Scholar]
- 4.Papanicolas I, Woskie LR, Jha AK. Health Care Spending in the United States and Other High- Income Countries. JAMA. 2018;319(10):1024–1039. doi: 10.1001/jama.2018.1150 [DOI] [PubMed] [Google Scholar]
- 5.Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1775–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Building U.S. Capacity to Review and Prevent Maternal Deaths. (2018). Report from nine maternal mortality review committees. Available from http://reviewtoaction.org/Report_from_Nine_MMRCs Accessed December 2, 2018.
- 7.Lu MC. Reducing Maternal Mortality in the United States. JAMA. 2018;320(12):1237–1238 [DOI] [PubMed] [Google Scholar]
- 8.CDC. Severe Maternal Morbidity in the United States. Available at: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/sever-ematernalmorbidity.html
- 9.ACOG Committee Opinion No. 649: racial and ethnic disparities in obstetrics and gynecology. Obstet Gynecol. 2015;126:e130–e134. [DOI] [PubMed] [Google Scholar]
- 10.Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Race, ethnicity, and nativity differentials in pregnancy-related mortality in the United States: 1993–2006. Obstet Gynecol. 2012. August;120(2 Pt 1):261–8. [DOI] [PubMed] [Google Scholar]
- 11.Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol. 2012. November;120(5):1029–36. [DOI] [PubMed] [Google Scholar]
- 12.Berg CJ, Harper MA, Atkinson SM, et al. Preventability of pregnancy-related deaths: results of a state-wide review. Obstet Gynecol 2005; 106(6):1228–1234. [DOI] [PubMed] [Google Scholar]
- 13.Callaghan WM. Overview of Maternal Mortality in the United States. Semin Perinatol. 2012;36(1):2–6. [DOI] [PubMed] [Google Scholar]
- 14.U.S. Department of Health and Human Services. The Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020. Phase I report: Recommendations for the framework and format of Healthy People 2020. Available at: https://www.healthypeople.gov/sites/default/files/PhaseI_0.pdf Accessed December 2, 2018).
- 15.Braveman P What are health disparities and health equity? We need to be clear. Public Health Rep. Jan-Feb 2014;129 Suppl 2:5–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hebert PL, Sisk JE, Howell EA. When Does A Difference Become a Disparity? Conceptualizing Racial and Ethnic Disparities in Health. Health Affairs. 2008;27:(2):374–382. [DOI] [PubMed] [Google Scholar]
- 17.Howell EA, Zeitlin J. Improving hospital quality to reduce disparities in severe maternal morbidity and mortality. Semin Perinatol. 2017(41):5, 266–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miranda ML, Maxson P Edwards S. Environmental contributions to disparities in pregnancy outcomes. Epidem Re. 2009;31(1): 67–83. [DOI] [PubMed] [Google Scholar]
- 19.Borders AE, Grobman WA, Amsden LB, Holl JL. Chronic stress and low birth weight neonates in a low-income population of women. Obstet Gynecol. 2007;109:331–338. [DOI] [PubMed] [Google Scholar]
- 20.Nowak AL, Giurgescu C The built environment and birth outcomes: a systematic review. MCN Am J Matern Child Nur. 2017. Jan-Feb;42(1):14–20. [DOI] [PubMed] [Google Scholar]
- 21.Howell EA. Reducing disparities in severe maternal and morbidity and mortality. Clin ObstetGynecol. 2018;61(2):387–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Health coverage by race and ethnicity: the potential impact of the Affordable Care Act. Available at: http://www.kff.org/dis-parities-policy/issue-brief/health-coverage-by-race-and-ethnicity-the-potential-impact-of-the-affordable-care-act/ Accessed December 2, 2018.
- 23.Jones CP Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90:1212–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.New York City Department of Health and Mental Hygiene (2016). Severe Maternal Morbidity in New York City, 2008–2012. New York, NY [Google Scholar]
- 25.Howell EA, Brown H, Brumley J, et al. Reduction of peripartum racial and ethnic disparities: a conceptual framework and maternal safety consensus bundle. Obstet Gynecol. 2018;131(5):770–782. [DOI] [PubMed] [Google Scholar]
- 26.Blair IV Steiner JF, Havranek EP Unconscious (implicit) bias and health disparities: where do we go from here?.Perm J. 2011;15(2):71–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Howell EA, Egorova N, Balbierz A, Zeitlin J, Hebert PL. Black-white differences in severe maternal morbidity and site of care. Am J Obstet Gynecol. 2015;214(1):122.e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Creanga AA, Bateman BT Mhyre JM, Kuklina E, Shilkrut A, Callaghan WM. Within hospital differences: Performance of racial and ethnic minority-serving hospitals on delivery-related indicators. Am J Obstet Gynecol. 2014. December; 211(6):647.e1–16. [DOI] [PubMed] [Google Scholar]
- 29.Denny CH, Floyd RL, Green PP et al. Racial and ethnic disparities in preconception risk factors and preconception care. J Womens Health (Larchmt). 2012;21:720–729. [DOI] [PubMed] [Google Scholar]
- 30.Howell EA, Egorova NN, Balbierz A, et al. Site of delivery contribution to black-white severe maternal morbidity disparity. Am J Obstet Gynecol. 2016;215:143–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilcox A, Levi EE & Garrett JM Predictors of Non-Attendance to the Postpartum Follow-up Visit. Matern Child Health J, 2016;20(Suppl 1):22–27. [DOI] [PubMed] [Google Scholar]
- 32.Cheng C, Fowles E, Walker L. Postpartum maternal health care in the united states: a critical review. J Perinat Educ. 2006. Summer;15(3):34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Council on Patient Safety in Women’s Health Care Alliance for innovation on maternal health (AIM). Safe health care for every woman: Reduction of peripartum racial/ethnic disparities. Available at: https://safehealthcareforeverywoman.org/patient-safety-bundles/reduction-of-peripartum-raciale-thnic-disparities/. Accessed December 2, 2018.
- 34.Kaplan RM. Shared medical decision-making. A new tool for preventive medicine. Am J Prev Med. 2004;26:81–83. [DOI] [PubMed] [Google Scholar]
- 35.The Joint Commission. Advancing effective communication, cultural competence, and patients and family-centered care: a roadmap for hospitals. Available at: https://www.jointcommission.org/assets/1/6/aroadmapforhospitalsfinalversion727.pdf Accessed December 2, 2018.
- 36.Howell EA, Brown H, Brumley J, et al. , Reduction of peripartum racial and ethnic disparities: a conceptual framework and maternal safety consensus bundle. J Obstet, Gynecol Neonatal Nurs.. 2018. May;47(3)L275–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chapman EN, Kaatz A, Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28:1504–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weech-Maldonado R, Dreachslin JL, Epane JP Gail J, Gupta S, Wainio JA. Hospital cultural competency as a systematic organizational intervention: key findings from the National Center for Healthcare Leadership Diversity Demonstration Project. Health Care Manage Rev. 2016;43:30–41. [DOI] [PubMed] [Google Scholar]
- 39.New York State Department of Health. New York State Toolkit to Reduce Health Care Disparities (2014): Improving Race and Ethnicity. Available at: https://www.albany.edu/sph/cphce/mrt_nys_toolkit_to_reduce_healthcare_disparities.pdf Accessed December 3, 2018.
- 40.Hasnain-Wynia R, Baker DW. Obtaining data on patient race, ethnicity, and primary language in health care organizations: current challenges and proposed solutions. Health Serv Res. 2006;41(4 Pt 1):1501–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mass General Hospital Institute for Health Policy. Improving Quality and Achieving Equity: A Guide for Hospital Leaders. Available at https://mghdi-sparitiessolutions.files.wordpress.com/2015/12/improving-quality-safety-guide-hospital-leaders.pdf Accessed December 2 2018.
- 42.Arora KS, Shields LE, Grobman WA, et al. Triggers, bundles, protocols, and checklists— what every maternal care provider needs to know. Am J Obstet Gynecol. 2016;214:444–451. [DOI] [PubMed] [Google Scholar]
- 43.Garretto Diana et al. Centering Pregnancy: an innovative approach to prenatal care delivery. Am J Obstet Gynecol. 210(1):14–15. [DOI] [PubMed] [Google Scholar]
- 44.Howell EA, Padrón NA, Beane SJ, et al. Delivery and payment redesign to reduce disparities in high risk postpartum care. Matern Child Health J. 2017;21(3):432–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McKinney J, Keyser L, Clinton S, Pagliano Co. ACOG Committee Opinion No. 736: Optimizing postpartum care.. Obstet Gynecol. 2018. September;132(3):784–785. [DOI] [PubMed] [Google Scholar]
- 46.Main EK, Markhow C, Gould J. Addressing maternal mortality and morbidity in California through public-private partnerships. Health Affairs. 2018;(37)9:1484–1493. [DOI] [PubMed] [Google Scholar]