Abstract
The aim of this issue is to describe endosseous distal extension (EDE) surgical technique. This implant technique was conceived and applied since 1993 by Dr Luca Dal Carlo, as an evolution of the classical ramus blade implant technique. With this technique, you attain great stability of the blade implant, due to the following difference compared with the classical blade implant technique: the hard and soft tissues lying behind implant abutment are not being destroyed at all. A slot is made on the upper side of the bone ridge, and the blade is inserted into it and pushed backwards, so that the implant is embedded under untouched tissues. Using blade implants specially drawn for this particular surgery, the slot’s length turns out to be about half of the implant’s length. Piezo bistoury is useful to facilitate surgical proceedings. If we compare the regenerated bone on the mesial part of the implant and the bone that had remained untouched on the distal side, we will see a difference in the tissue density even after a long time. EDE technique is suitable for those cases in which the lower distal sector is characterized by scarceness of cancellous bone. Data collected during 22 years of clinical practice (97.7% 5-year success rate) allow to suggest employing this technique with asymmetric blades to treat D3-D4 narrow ridges located in the posterior mandible. Soft tissue response results are very good.
Keywords: blade implants, endosseous distal extension, inferior posterior ridges, mandibular ramus, plate-form implants
Introduction
Endosseous distal extension (EDE) is an implant dentistry technique consisting the use of blade implants in the posterior mandible, making the blade to enter through an anterior slot, so as to insert its posterior part without damaging the superficial bony cortex and soft tissues. This variant of the classical insertion technique provides an exceptionally stable distal implant, engaged between the overlying untouched superficial cortex and the underlying mylohyoid line and inferior alveolar canal. EDE technique can be performed both in healed ridges and immediately post-extractive treatment of last molars. EDE technique was first performed by Dr Luca Dal Carlo1 in 1993 and was first published in 2001.
Data carefully collected2 for 22 years (1993–2015) show very good outcomes, which lead us to suggest this technique as a standard solution in D3-D4 posterior inferior bony ridges. Blade implants osseointegration has been widely proven by means of several histologic and radiographic examinations.3–8
Since a blade implant does not need a wide bony ridge, it can be embedded into a narrow as well as a wide bone ridge; nevertheless, blade implants fit perfectly to less than 5-mm wide bone ridges. Blade implant has a basic and unique position among the different techniques applied in dental surgery, as it implies the best use of the available bone layer, which is generally a primary axiom for conservative implant dentistry.
While embedding a blade implant, the superficial cortical tissue is demolished, and the way it recovers and regenerates upon the implant’s shoulder is dramatically important for a long-lasting success of the implant. If the regenerated bone tissue has not thoroughly covered the implant’s shoulder, it is normally very difficult to keep the horizontal bone layer in good conditions for a long time. In these cases, we normally observe an increasing shrinking of the bone tissue towards the apex until the implant cannot support the functional loads anymore.
If the implant has been embedded at the right depth and the conditions guaranteeing its absolute immobility during its bone regeneration are absolved, we have to consider the individual’s own ability to regenerate the bone tissue upon the implant, which may sometimes be insufficient. The degree of bone regeneration upon the shoulder of a blade implant is therefore not predictable and may be deceiving.
This is the reason why the idea of destroying a smaller amount of bone tissue arose, just what is strictly necessary, keeping intact as much surface bone ridge as possible.
Purpose of this technique
Usually, the blade’s abutment is exactly in its middle point, that is, equidistant from both ends. Surgical procedure guidelines suggest making an opening that must be as long as the blade and about 2 mm deeper than the blade itself.8,9
EDE idea is to make a slot which is as long as the distance between blade’s anterior end and distal edge of its abutment. By this way, it is possible to insert the posterior side of the blade under a portion of the superficial cortical bone and mucous membrane, which remains therefore untouched. Asymmetrical blades, derived from the Roberts plate-form ramus implants,10 provided with a combination of cutting edges (Linkow wedge-form concept) and non-cutting edges (Roberts plate-form concept) fit perfectly to this surgical technique (Figure 1).
Figure 1.
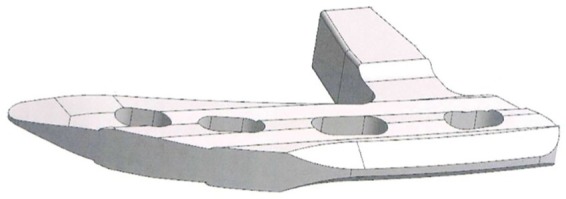
Technical drawing of the asymmetrical EDE blade, inferior view (Bio Micron Sas, Limbiate, Italy).
Procedure with EDE technique
Different from the traditional techniques, where the abutment is positioned in the middle of the slot, in this case, it must be positioned at the distal end of the slot. If we are dealing with the posterior end of the inferior jaw, the best choice is an asymmetric blade (Figures 1–4).
Figure 2.
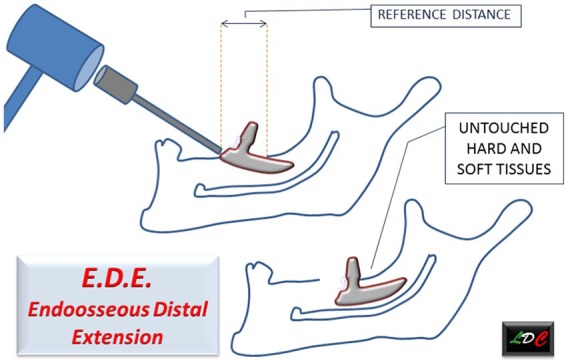
Scheme showing reference distance, embedment inclination, definitive implant position and untouched tissues overhanging blade distal extension.
Figure 3.
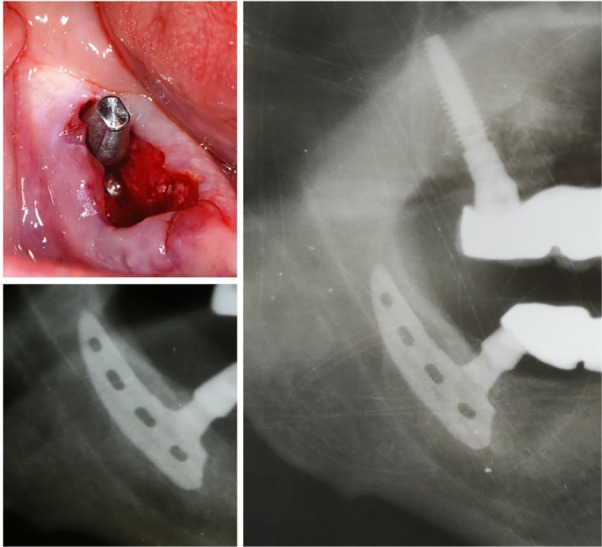
At left: picture and X-ray of an asymmetric blade inserted following EDE proceedings, correctly engaged between untouched superficial cortex and inferior alveolar canal. Implant has been penetrating through anterior slot. Implant was immediately loaded. At right: X-ray control 4 years later.
Figure 4.
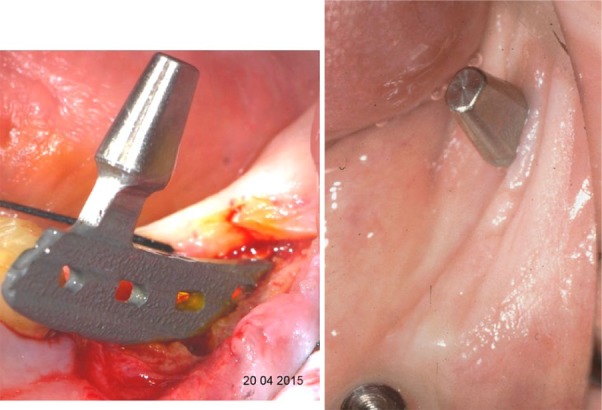
Left: asymmetric blade inclination during insertion following EDE insertion technique. Right: soft tissues surrounding blade abutment.
These types of blades are similar to ramus blades, with some peculiar characteristics added: the posterior extremity and the inferior anterior edge are cut to allow penetration, and the superior shoulder and the inferior posterior edge are smooth, to avoid damaging inferior alveolar nerve and surface cortex.
Proceedings
In order to open the surgical groove, cut the surface cortical bone using a 0.9-mm bur and/or a piezoelectric bistoury. The opening length repeats the distance from distal end of the blade’s abutment neck to the blade’s mesial end.
When the groove is ready, work with the bur or piezo, keeping in mind that the implant is going to be embedded deeper inside than the thickness of the surface cortical bone that lies distally to the abutment’s neck.
If necessary, go further down inside with the piezo, under the surface cortical bone lying distally to groove’s distal end, in order to help the implant slide backwards through the cancellous bone.
Insert the implant diagonally into the opening while pushing it distally with a dental forceps.
Hammer down the implant with a scalpel in order to make it glide distally, until its mesial edge is aligned with the mesial edge of the opening.
With the scalpel’s point on the blade’s mesial surface, hammer the blade, first downwards and then distally, until it reaches the right position.
Different from the traditional technique, where the length of the slot corresponds to the length of the implant, with this technique, the slot lies on an empty area because the implant glides distally under untouched tissue.
Main advantages of this technique are as follows:
The implant is embedded under a portion of untouched tissue that will not collapse even in case the implant should be subject to traction forces;
Immediate stabilization of the implant in its own seat, excluding any possibility of being shifted by the tongue or by any masticatory trauma during the bone tissue integration period;
The recovering of the posterior surface tissue does not depend on the patient’s own regenerating capacity.
Main difficulties that must be prevented are as follows:
Procedure problems because of teeth lying anteriorly to the area that is being treated;
Particularly hard cancellous bone, opposing strong resistance to the distal progression of the implant. Piezo surgery allows to overcome this problem, using suitable tips;
Spots of thicker bone tissue, which can make implant progression difficult.
In order to prevent such situations, it is advisable to make a thorough X-ray overview of the area and to objectively consider the situation before proceeding with implant surgery.
This technique was applied to patients since June 1993, using standard shaped implants. The first scientific article was issued in 2001.1 Trying to get the best from the technique, here we described an asymmetric implant with the posterior end bigger than the mesial end was selected as most suitable item (Figure 3). Using this kind of implant, the opening needed is remarkably shorter, since the cut which is necessary to the embedment of the implant must be as long as the distance between the mesial edge of the implant and the distal edge of blade’s neck (Figure 2).
EDE method is suitable as well in case you want to embed an implant proceeding backwards from the area where a tooth has been extracted (Figure 3).11 Since these implants are inserted between the cortical bone of the mandibular canal and the superficial compact bone, these implants can bear remarkable functional loads.12
Clinical case
Mrs P.D., a 60-year-old woman, needed full-arch rehabilitation both in the upper and lower jaws. In the inferior, while in the inter-foraminal area the substitution of the present teeth looked easy, the posterior areas were thin and there was scarce depth above the nerve. The inferior rehabilitation planning was based on EDE asymmetric blade implants in the posterior and screw implants in the anterior, added to one pre-existing one-piece screw implant, still valid (zone 3.2).
A full-arch 14 teeth fix prosthesis was fixed to the eight implants inserted in the inferior jaw (Figure 5).
Figure 5.
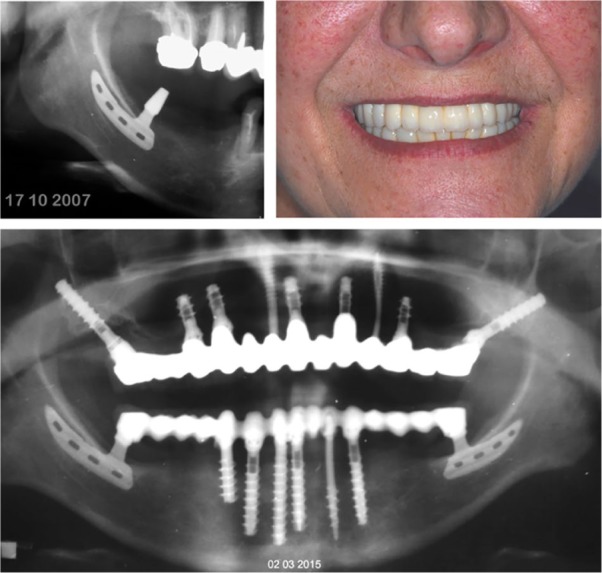
Upper left: X-ray of the asymmetric blade inserted in zone 4.7 following EDE proceedings. Upper right: patient’s smile after end of inferior and superior works. Lower: panoramic X-ray at 7 years follow-up.
The 7-year panoramic X-ray confirms stability of bone integration of all implants.
Statistical data
Statistical data, in relation to EDE technique, were collected for a period of 22 years.2 Since 1993, 111 posterior ridges have been treated (including two superior posterior sectors; inferior posterior sectors were 109). Among the 109 posterior ridges, 2/3 (73) were female and 1/3 (36) were male patients. In 1998, asymmetric blades took the place of the standard blades previously utilized. A total of 90 ridges have been treated before 2010, more than 5 years before the date of this publication. A total of 87 of the 90 over 5 years implants were trackable. Just 2 of the 87 implants were lost (97.7% 5-year success). A total of 63 ridges were treated before 2005, more than 10 years before the date of this publication. A total of 50 of the 63 over 10 years implants were trackable. A total of 7 of the 50 implants were lost (86% 10-year success). If we separate the data about standard and asymmetric blades, we see that while 10-year success rate with standard blades was 82.8% (29/42), 10-year success with asymmetric blades was 93.3% (14/15). Asymmetric blades utilized during the last 5 years got no failures. In fact, this shape allows to engage a long posterior part of the implant inside a solid housing, between the untouched superficial cortex and deep anatomical structures (mylohyoid line and inferior alveolar canal).
Discussion
Treatment of the inferior posterior atrophic ridges is particularly important to provide correct chewing function and occlusal balance. The posterior sectors are subject to intense forces, both during chewing and during swallowing. Due to these considerations, while natural teeth are missing, we need to provide valid posterior pillars.
The aim of this technique is making the blade insertion surgery less traumatic, starting from the following principle: the less bone ridge tissue destroyed during an implant surgery, the better is the healing prognosis. In order to proceed more comfortably, the direction of the blade’s insertion runs obviously backwards.
Among the advantages of this insertion technique, we can observe an immediate stabilization of the implant; furthermore, this implant is less subject to any movement caused by forces of various intensity and different directions.
This technique’s actual innovation is that a part of the implant is inserted under absolutely untouched bone cortical and soft tissue that are not therefore subject to the reabsorption of the bone ridge.
The over 25 years clinical experience and statistical data gathered about this technique during the 22 years are really very encouraging.
Due to their 93.3% 10-year success rate registered with asymmetric EDE blades, we suggest the use of this kind of implant for the application of this technique. With this kind of implants, EDE insertion technique permits minimized risks of failure, because implant stability is very high since the moment of insertion. EDE technique allows to exploit the posterior parts of the mandible, which otherwise would be untreated. Data collected during 22 years of clinical practice (97.7% 5-year success rate) allow to suggest to employ this technique with asymmetric blades to treat D3-D4 narrow ridges located in the posterior mandible.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
ORCID iD: Dorina Lauritano  https://orcid.org/0000-0002-3550-1812
https://orcid.org/0000-0002-3550-1812
References
- 1. Dal Carlo L. (2001) A new technique for inserting blade implants: Endosseous distal extension. Dental Cadmos 69(Part 16): 41–50. [Google Scholar]
- 2. Dal Carlo L. (2016) Study over 7000 endosseous implants inserted during 25 years in 3300 interventions: Clinical results in different anatomical and functional situations. Statistical data and over 20 years iconographic documentation. Journal of Dental and Oral Health 2(6): 048. [Google Scholar]
- 3. Linkow LI. (1989) Implant Dentistry Today: A Multidisciplinary Approach. Padova: Piccin. [Google Scholar]
- 4. Bianchi AE, Gallini G, Fassina R, et al. (1994) Sem analysis of bone-titanium interface of a blade-vent implant. Il Dentista Moderno 7: 1107–1113. [Google Scholar]
- 5. Trisi R, Quaranta M, Emanuelli M, et al. (1993) A light microscopy, scanning electron microscopy and laser scanning microscopy analysis of retrieved blade implants after 7 to 20 years of clinical function. A report of 3 cases. Journal of Periodontology 64(5): 374–378. [DOI] [PubMed] [Google Scholar]
- 6. Di Stefano D, Iezzi G, Scarano A, et al. (2006) Immediately loaded blade implant retrieved from a man after a 20 year loading period: A histologic and histomorphometric case report. Journal of Oral Implantology 32(4): 171–176. [DOI] [PubMed] [Google Scholar]
- 7. Dal Carlo L, Pasqualini ME, Carinci F, et al. (2013) A brief history and guidelines of blade implant technique: A retrospective study on 522 implants. Annals of Oral & Maxillofacial Surgery 1(1): 3. [Google Scholar]
- 8. Diotallevi P, Dal Carlo L, Pasqualini ME, et al. (2014) Radiological evalutation of long term complications of oral rehabilitations of thin ridges with titanium blade implants. Journal of Osseointegration 6(1): 11–14. [Google Scholar]
- 9. Linkow LI. (1984) Endosseous Bladevent implant insertion guidelines. Dentistry Today III: 6. [Google Scholar]
- 10. Roberts RA. (1996) Types, uses, and evaluation of the plate-form implant. The Journal of Oral Implantology 22(2): 111–118. [PubMed] [Google Scholar]
- 11. Dal Carlo L. (2014) Edes: Posterior lower molar substitution with combination of blade and screw implants. Doctor OS FEB XXV(2): 102–109. [Google Scholar]
- 12. Linkow LI, Winkler S, Shulman M, et al. (2016) A new look at the blade implant. The Journal of Oral Implantology 42(4): 373–380. [DOI] [PubMed] [Google Scholar]


