Abstract
Context:
Superior labral anterior-posterior (SLAP) lesions often result in significant sporting limitations for athletes. Return to sport is a significant outcome that often needs to be considered by athletes undergoing the procedure.
Objective:
To evaluate return to sport among individuals undergoing arthroscopic SLAP repair.
Data Sources:
Four databases (MEDLINE, EMBASE, PubMed, and Cochrane) were searched from database inception through January 29, 2018.
Study Selection:
English-language articles reporting on return-to-activity rates after arthroscopic SLAP repairs were included.
Study Design:
Systematic review.
Level of Evidence:
Level 4.
Data Extraction:
Data including patient demographics, surgical procedure, and return to activity were extracted. The methodological quality of included studies was evaluated using the Methodological Index for Non-Randomized Studies (MINORS) tool.
Results:
Of 1938 screened abstracts, 22 articles involving a total of 944 patients undergoing arthroscopic SLAP repair met inclusion criteria. Of the total included patients, 270 were identified as overhead athletes, with 146 pitchers. Across all patients, 69.6% (657/944 patients) of individuals undergoing arthroscopic SLAP repair returned to sport. There was a 69.0% (562/815 patients) return to previous level of play, with a mean time to return to sport of 8.9 ± 2.4 months (range, 6.0-11.7 months). The return-to-sport rate for pitchers compared with the return-to-activity rate for nonpitchers, encompassing return to work and return to sport, was 57.5% (84/146 patients) and 87.1% (572/657 patients), respectively, after arthroscopic SLAP repair.
Conclusion:
Arthroscopic SLAP repair is associated with a fair return to sport, with 69.6% of individuals undergoing arthroscopic SLAP repair returning to sport. SLAP repair in pitchers has significantly decreased return to sport in comparison with nonpitching athletes. Athletes on average return to sport within 9 months postoperatively.
Keywords: superior labral anterior-posterior repair, SLAP repair, return to sport, pitchers
Superior labral anterior-posterior (SLAP) lesions pose significant limitations for many athletes, in particular, those participating in repetitive overhead movements. SLAP lesions are characterized by injury to the superior labrum beginning posteriorly and extending anteriorly, stopping before or at the mid-glenoid notch and including the “anchor” of the biceps tendon to the labrum.35 Lesions are traditionally divided into 4 types based on morphology of the tear and involvement of the biceps anchor.35 Type II lesions are the most common type identified in overhead athletes, making up approximately 50% of SLAP lesions.5 Type II lesions are characterized by the detachment of the biceps anchor and the superior labrum.22,29,34 With throwers, torsional peel-back of the biceps tendon on the labrum is experienced every time the arm is brought into the cocked position, increasing the risk of developing a SLAP lesion.6,7
Arthroscopic SLAP repair is often indicated for SLAP lesions, as it has good to excellent results in the majority of athletes, as well as high patient satisfaction.12,16,24,29 Furthermore, functional outcomes, such as visual analog scale scores and range of motion, improve after arthroscopic SLAP repair.15 However, SLAP repair is not without complications, including postoperative pain and stiffness.31,36 Return to sport is critical to athletes; therefore, athletes undergoing arthroscopic SLAP repair often will inquire regarding return-to-sport timeline and ability to return to previous level of performance.26
The purpose of this study was to assess rates of return to sport and rates of return to sport at the athlete’s preoperative level of competition after arthroscopic SLAP repair to better elucidate the success of the procedure and the limitations it may have for athletic populations.
Methods
The study was conducted in accordance with the methods outlined in the Cochrane Handbook and is reported according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement.21
Search Strategy and Eligibility
A systematic literature search was conducted in PubMed, EMBASE, MEDLINE, and Cochrane (CENTRAL) databases beginning from database inception through January 29, 2018 (see Appendix Table A1, available in the online version of this article). Medical subject headings and Emtree headings and subheadings were used in various combinations in Ovid and supplemented with free text. A manual search of related references and cited articles was also performed to identify any additional relevant studies for inclusion.
Inclusion criteria consisted of the following: (1) patients undergoing arthroscopic SLAP repair; (2) a minimum of 5 eligible patients; (3) patients reporting a return to activity as defined by return to sport, return to previous level of play, or return to work; and (4) level 4 evidence or higher.
Articles were excluded if the study did not meet the above exclusion criteria, was published only in abstract format, or was a review article, surgical technique guide, imaging study, medical conference abstract, cadaveric study, or biomechanical study.
Screening
Two reviewers independently screened the titles and abstracts of all studies for eligibility using piloted screening forms. Duplicate articles were excluded using Refworks. Both reviewers assessed the full text of all potentially eligible studies identified by title and abstract screening to determine final eligibility. All discrepancies were resolved by consensus.
Data Extraction and Risk of Bias Assessment
Data were extracted in duplicate and independently by the 2 reviewers using an electronic data extraction form. The data extracted included the following: year and country of publication; type of study; number of patients; patient demographics; length of follow-up; SLAP lesion type; nature of SLAP repair procedure; number and type of complications or adverse events; whether revision surgery was required; time to revision surgery; functional outcomes; time to return to activity; percentage return to activity, as defined by return to sport and return to work; and percentage return to same level of competition. Both reviewers independently assessed the methodological quality of the included studies using the Methodological Index for Non-Randomized Studies (MINORS) tool for all nonrandomized studies and the Cochrane risk of bias tool for all randomized controlled trials.
Data Analysis
The return-to-sport measures were calculated by forming a proportion of the total patients that returned to sport after arthroscopic SLAP repair out of the entire population that underwent arthroscopic SLAP repair across included studies. Interrater reliability for study eligibility was measured using the kappa (κ) statistic. A κ of 0 to 0.2 represents slight agreement, 0.21 to 0.40 fair agreement, 0.41 to 0.60 moderate agreement, and 0.61 to 0.80 substantial agreement. A value greater than 0.80 is considered almost perfect agreement, according to the guidelines of Landis and Koch.19
Methodologic quality was assessed independently by 2 reviewers using the MINORS tool for included, nonrandomized studies. A score of 0, 1, or 2 was given for each of the 12 items on the MINORS checklist, with a maximum score of 16 for noncomparative studies and 24 for comparative studies. Methodologic quality was categorized a priori as follows: 0 to 6, very low quality of evidence, 7-10 to indicate low quality of evidence, 10 to 14, fair quality of evidence, and >16, good quality of evidence for nonrandomized studies.
Interobserver agreement for assessment of methodologic quality was calculated using the intraclass correlation coefficient (ICC). Both κ and ICC were calculated using GraphPad Software.
Results
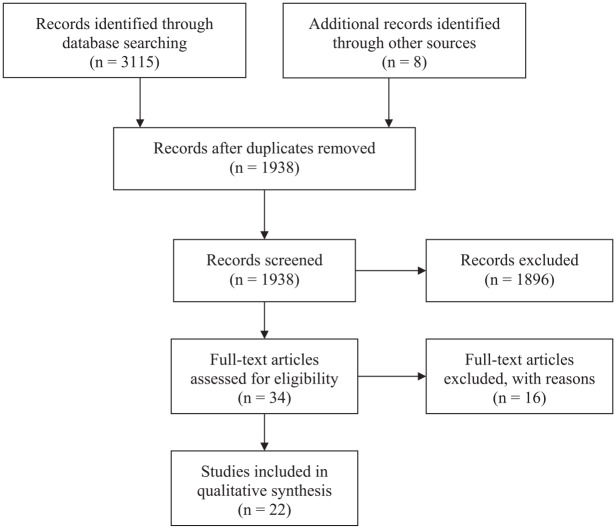
The literature search generated 3115 articles. After removing duplicates, 1938 articles were screened by title and abstract, leaving 34 eligible articles for full-text review. Finally, 22 articles met the inclusion criteria of this review (Figure 1).2-4,8-13,16-18,20,23-25,27-29,33,37,38 The κ value for overall agreement between reviewers for the initial eligibility decision was 0.73 (95% CI, 0.61-0.85), indicating substantial agreement.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram for systematic review of superior labral anterior-posterior repair.
Study and Patient Characteristics
A total of 944 patients undergoing SLAP repair (84.3% male) were included across studies, with a mean sample size of 43 patients (range, 10-179) per study. The patient population included 270 overhead athletes, with 146 pitchers. The total population consisted of athletes, overhead and nonoverhead, the majority of whom were engaged in baseball (n = 138; 14.6%), tennis (n = 8; 0.8%), and volleyball (n = 6; 0.6%). The most common concomitant pathologies were partial or full rotator cuff injury (n = 91; 9.6%) and subacromial impingement (n = 35; 3.7%). Other less common pathologies included Bankart tears (n = 10; 1.1%) and glenohumeral osteoarthritis (n = 8; 0.8%). Mean follow-up was 42.6 months (range, 27.6-78.0 months). Mean age across patients at the time of surgery was 30.5 years (range, 19.5-45.2 years) (Table 1).
Table 1.
Characteristics of studies reporting on return to sport, previous level of play, and duty after isolated arthroscopic SLAP repaira,b
| Study | Location | No. of Included Patients | Mean Age at Time of Surgery, y | Mean Follow-up, mo (range) | Mean MINORS Score | Level of Evidence |
|---|---|---|---|---|---|---|
| Boesmueller et al, 20172 | Austria | 11 | 31.8 | 41.9 (36.1-48.4) | 14/16 | 4 |
| Boileau et al, 20093 | France | 10 | 37 | 35 (24-69) | 20/24 | 2 |
| Brockmeier et al, 20094 | USA | 47 | 36 | 32.3 (25.1-48.7) | 12/16 | 4 |
| Chalmers et al, 20168 | USA | 45 | 35 | 49.2 (12.0-58.8) | 9.5/16 | 3 |
| Cohen et al, 20069 | USA | 29 | 34 | 44 (25-97) | 10/16 | 4 |
| Denard et al, 201410 | USA | 20 | 45.2 | 63.2b | 10/16 | 4 |
| Fedoriw et al, 201411 | USA | 40 | 23.7 | — | 10.5/16 | 4 |
| Friel et al, 201012 | USA | 48 | 33.1 | 40.8 (24-68.4) | 10.5/16 | 4 |
| Gilliam et al, 201813 | USA | 133 | 19.5 | 78 (27-146) | 9.5/16 | 4 |
| Ide et al, 200516 | Japan | 40 | 26 | 41 (24-58) | 10.5/16 | 4 |
| Kim et al, 201217 | South Korea | 14 | 26 | 31.4 (25-46) | 20/24 | 2 |
| Kim et al, 200218 | South Korea | 34 | 39.1 | 33b | 10/16 | 4 |
| Maier et al, 201320 | Germany | 24 | 36.5 | 46.2b | 19.5/24 | 4 |
| Neri et al, 201123 | USA | 50 | 35 | 41.5 (18-45) | 9/16 | 2 |
| Neuman et al, 201124 | USA | 30 | 24 | 42 (18-96) | 11/16 | 4 |
| Park et al, 201325 | South Korea | 24 | 22.7 | 45.8 (24-68) | 10/16 | 4 |
| Provencher et al, 201327 | USA | 179 | 31.6 | 40.4 (26-62) | 10.5/16 | 3 |
| Rhee et al, 200528 | South Korea | 41 | 24 | 33 (25-67) | 11/16 | 4 |
| Samani et al, 200129 | USA | 25 | 36 | 35 (24-51) | 10.5/16 | 4 |
| Smith et al, 201633 | USA | 24 | 27.8 | — | 9.5/16 | 4 |
| Waterman et al, 201537 | USA | 60 | 35 | 50b | 17.5/24 | 3 |
| Yung et al, 200838 | China | 16 | 24.2 | 27.6 (24-31) | 11/16 | 2 |
MINORS, Methodological Index for Non-Randomized Studies; SLAP, superior labral anterior-posterior.
Dashes refer to data not reported.
Unavailable range.
Study Quality
All studies included were case-control,8,27,37 case series,2,4,9-13,16,18,20,24,25,28,29,33 or cohort studies3,17,23,38 of level 2 to 4 evidence. There were no randomized controlled trials or level 1 studies included. The mean MINORS score was 10.5 ± 1.1 out of 16 (Table 1). Agreement between reviewers in the assessment of study quality was good (intraclass correlation coefficient, 0.88; 95% CI, 0.67-0.94).
Surgical Techniques
All SLAP repairs were performed arthroscopically. Three studies3,8,10 compared the effect of biceps tenodesis with arthroscopic SLAP repair, with 18 shoulders undergoing combined SLAP repair and biceps tenodesis, 53 individuals undergoing biceps tenodesis alone, and 75 patients undergoing isolated SLAP repair. From these 3 studies, only patients undergoing SLAP repair in isolation were included. At least 21 patients with concomitant partial-thickness rotator cuff tears or osteoarthritic lesions were treated with debridement in addition to the arthroscopic SLAP repair procedure.18,25,29 The most common concomitant procedures were subacromial decompression (46/131; 35.1%) and debridement (35/131; 26.7%) (Appendix Table A2, available online). Further information about surgical techniques, such as how portal configuration varied across studies, can be found in Appendix Table A2.
Rehabilitation Protocol
Rehabilitation after arthroscopic SLAP repair focused on physical therapy. The protocols differed slightly between studies; however, each followed a similar regimen. Patients used a sling for 1 to 6 weeks with either immobilization or limited mobility and gentle passive range of motion. Passive range of motion was allowed from any time after the first postoperative visit to 6 weeks after surgery. Active range of motion usually started at 3 to 9 weeks postoperatively. Strengthening exercises were started from any time after the first postoperative visit to 16 weeks postoperatively. Sport-specific training was instituted between 7 and 24 weeks postoperatively. Patients were allowed to return to sport at 3 to 6 months postoperative. In overhead athletes, the majority of studies reported return to throwing 4.5 to 7 months postoperatively after a structured throwing program.
There were variable rehabilitation protocols among the biceps tenodesis procedures performed in comparison studies; however, most studies assumed the same protocol as SLAP repair. Chalmers et al8 had patients avoid resisted elbow flexion or forearm supination for the first 4 weeks to protect the tenodesis, whereas Denard et al10 had patients immobilized in a sling for 6 weeks postoperatively. Active elbow flexion and extension and passive forward elevation and external rotation were allowed immediately as tolerated, while strengthening was delayed until 12 weeks postoperatively.10
Return to Sport
Overall, the return to sport across all patients was 69.6% (657/944 patients). From the 17 studies reporting previous level of play, 69.0% (562/815) of patients were able to return to previous level of play.2-4,8-12,13,16,18,20,23,27,29,33,38 Three studies4,12,20 reported specifically on level of play of overhead athletes, and pooled results indicated 65.0% (39/60) return to previous level of sport for overhead athletes.
Three studies11,13,33 with a total of 146 pitchers reported a return to sport rate of 57.5% (84/146 patients) for pitchers alone, in contrast to 87.1% (572/657 patients) return to activity rate for all nonpitchers. Four studies3,23,24,38 consisting of 143 patients reported on time to return to sport (Table 2). The mean time to return to sport was 8.9 ± 2.4 months (range, 6.0-11.7 months) across the studies that reported on it. Duration of return to sport was only reported by Smith et al,33 citing mean career length on return to play as 3.67 ± 1.91 years, bringing into question the true long-term success of SLAP repair as reported in the studies. Of the total included patients, 270 were identified as overhead athletes and 146 as pitchers. The return to activity, as encompassed by return to work and return to sport, for those participating in overhead activities compared with nonoverhead activities were 70.3% and 72.4%, respectively, after arthroscopic SLAP repair. Fifteen studies reporting no concomitant shoulder pathology were associated with a higher pooled return-to-sport rate of 69.8% (353/496 patients),2,3,8,9,11,16-18,20,23-25,27,33,38 compared with the return-to-sport rate for the 7 studies that did report concomitant pathologies in their population, which was 68.0% (305/448 patients) (Table 2).4,10,12,13,28,29,37
Table 2.
Characteristics of SLAP lesion, fixation, return-to-activity rates, and complicationsa
| Study | Injury to Dominant Extremity, n (%) | Type of SLAP Lesion | Fixation | No. of Patients Who Returned to Activity (%) | No. of Compli-cations | Mean Time to Return to Sport |
|---|---|---|---|---|---|---|
| Boesmueller et al, 20172 | 9 (82) | II | Anchor | 11 (100) | 4 | — |
| Boileau et al, 20093 | 9 (90) | II | Anchor | 2 (20) | 6 | — |
| Brockmeier et al, 20094 | 34 (72) | II | Anchor | 35 (74) | 5 | 6 mo |
| Chalmers et al, 20168 | 27 (61) | I-IV | — | 30 (64) | 8 | — |
| Cohen et al, 20069 | 14 (48) | II | Tack | 14 (48) | 1 | — |
| Denard et al, 201410 | 13 (65) | II | Anchor | 17 (86) | 2 | — |
| Fedoriw et al, 201411 | — | II | Anchor | 24 (60) | — | — |
| Friel et al, 201012 | 29 (60) | II | Anchor | 30 (62) | 4 | — |
| Gilliam et al, 201813 | — | — | Anchor | 82 (62) | 35 | — |
| Ide et al, 200516 | 38 (95) | — | Anchor | 36 (90) | — | — |
| Kim et al, 201217 | 10 (71) | II and V | Anchor | 13 (93) | 1 | — |
| Kim et al, 200218 | — | — | Anchor | 34 (100) | 2 | — |
| Maier et al, 201320 | — | II | Anchor | 16 (66.7) | 2 | — |
| Neri et al, 201123 | 50 (100) | II | Anchor | 39 (78) | — | 8.45 mo for<40 y; 11 mo for ≥40 yb |
| Neuman et al, 201124 | — | II | Anchor | 24 (80) | — | 11.7 mo |
| Park et al, 201325 | — | II | Anchor | 12 (50) | 5 | — |
| Provencher et al, 201327 | 101 (56) | II | Anchor | 113 (63) | — | — |
| Rhee et al, 200528 | — | II-IV | Tack | 31 (76) | 6 | — |
| Samani et al, 200129 | 20 (80) | II | Tack | 23 (92) | 5 | — |
| Smith et al, 201633 | — | — | — | 15 (63) | — | — |
| Waterman et al, 201537 | — | II, V, IX, VII | Anchor | 42 (70) | — | — |
| Yung et al, 200838 | — | II | Anchor | 15 (94) | 0 | 9.4 mo |
SLAP, superior labral anterior-posterior.
Dashes refer to data not available.
40 y indicative of age of player.
There were variable criteria for return to previous level of play across all studies; however, all players returned to the same sport when authors reported on return to previous level of play. Two studies16,18 specified return to preinjury levels as being grade 0, indicating no limitation and a complete return to preinjury levels, with higher levels representing mild to severe limitation. For pitchers, 2 studies11,33 specified return to preinjury levels as having an earned run average (ERA) within 2.00 and walks plus hits per inning pitched (WHIP) within 0.500. Most studies used patient-reported outcomes to assess return to previous level of play.2-5,9,10,12,13,17,20,23-25,27-29,37,38
Complications and Revision Surgery
The overall complication rate across the studies included was 9.1% (86/944 patients) (Table 2). The most common adverse effects reported involved pain or postoperative stiffness (56/944 patients; 5.9%) and recurrent tearing (23/944 patients; 2.4%).2-4,8-10,12,13,17,18,20,25,28,29
The rate of revision surgery was 13.5% (125/944 patients). Of the studies reporting on the reasons for performing revision surgery, the most common reasons were persistent postoperative pain or stiffness (30/944 patients; 3.2%) or retearing (19/944 patients; 2.0%), with the majority of revision surgeries including biceps tenodesis (78/127 patients; 61.4%) or revision SLAP repair (29/127 patients; 22.8%).
Discussion
SLAP lesions pose significant sporting limitations for athletes.24,25 We found a pooled return to sport rate of 69.6% (657/944 patients) after SLAP repair. Although there is large variation in the reported rates of return to sport, overall, the literature supports a high level of return to sport for patients other than those participating in pitching sports. The return-to-sport rate for pitchers compared with the return-to-activity rate for nonpitchers, as defined by return to sport or return to work, was 57.5% (84/146 patients) and 87.1% (572/657), respectively. Overall, the literature supports a return to sport at the same level for 69.0% (562/815) of patients. The time to return to activity for most patients was approximately 9 months.
Similar systematic reviews have been conducted by Gorantla et al,14 Sayde et al,30 and Sciascia et al32; however, no systematic reviews on this topic have been conducted since 2015. This study provides an update on the literature, with several studies included since then.2,8,13,33,37 The study by Sciascia et al32 only included studies performed up to 2013, despite having been published in 2015. Furthermore, Gorantla et al14 and Sciascia et al32 do not specify whether screening was performed independently in duplicate. There were certain studies that should have been included in these reviews that may have been overlooked. In the study by Sayde et al,30 although articles were searched up until December 2010, the study failed to include the investigation by Rhee et al28 in 2005. Sciascia et al32 failed to include studies by Kim et al17 (2012), Neuman et al24 (2011), Boileau et al3 (2009), and Rhee et al28 (2005) despite their search ending in 2013. Gorantla et al14 failed to include the study by Rhee et al28 (2005) despite the search ending in 2009.
Concomitant shoulder pathologies may also compromise return to sport after arthroscopic SLAP repair. Glenohumeral instability and rotator cuff tears were prevalent among the patients studied, and they were associated with similar return-to-sport rates in comparison with the studies reporting no concomitant pathologies.10,11,13,18,23,24,29,37 Patients with concomitant shoulder pathology also were found to have higher rates of postoperative complications, which may affect time to return to sport. The most common concomitant pathologies were partial or full rotator cuff injury (91; 9.6%) and subacromial impingement (35; 3.7%).
Very few studies reported on time to return to sport, making it difficult to provide an accurate estimate of the true recovery time period. Although the studies that reported on time to return to sport had variable follow-up periods and return-to-sport rates, the studies all reported a time to return to sport between 6 months and 1 year.23,38 Time to return to sport is also dependent on factors outside of the pathology or surgery, such as the aggressive or conservative nature of the surgeon’s approach as well as the nature of the trainer’s rehabilitation protocol.
Injury to the dominant versus the nondominant extremity also may dictate whether the athlete is able to return to sport. For example, Boileau et al3 reported 90% of athletes experienced injury to the dominant extremity and only 20% returned to their previous level of play.3 However, Ide et al16 reported 95% of patients having injured their dominant extremity but still had a 90% return-to-sport rate. Similarly, Neri et al23 reported 100% of patients experiencing injury to their dominant arm and a 78% return-to-sport rate overall.23 Therefore, it remains somewhat unclear how much undergoing a SLAP repair on the dominant arm as opposed to the nondominant arm affects return-to-sport rates.
Other patient factors such as the patient’s age may also affect the patient’s ability to return to sport. According to the findings by Neri et al,23 older age is associated with a significantly longer time to return to sport, with patients 40 years and older experiencing a slower return to sport (74%) after arthroscopic SLAP repair than patients younger than 40 (80%).
Some studies that were included compared the outcomes of SLAP repair with other interventions such as biceps tenodesis and combined SLAP repair and biceps tenodesis. Chalmers et al8 found that combined biceps tenodesis and SLAP repair was associated with less favorable return-to-work rates (60%) compared with SLAP repair (88%) or biceps tenodesis (75%). However, Denard et al10 found that biceps tenodesis had improved return-to-sport rates (100%) in comparison with SLAP repair (77%). Boileau et al3 also found that patients who require revision surgery for persistent pain after SLAP repair can often be successfully managed with a biceps tenodesis.
There are limitations associated with this review, such as the variable follow-up periods among the studies, possibly accounting for the variability in return-to-sport rates. Furthermore, some studies defined their overall return-to-sport rate as return to sport at the previous level of play and did not report an overall rate of return to sport at any level. In these cases, the rates of return to sport at any level were assumed to be equal to the rate of return to sport at the preoperative level, which likely resulted in an underestimate in the true return-to-sport rate at any level.2-4,8-10,27,38
Furthermore, the criteria for return to previous level of play or work varied across studies, if objectively reported at all, making it difficult to provide a concrete definition for return to preinjury level of play or work. For example, Fedoriw et al11 indicated that return to previous level of play was indicated by returning to play for at least 1 season while maintaining the same league or ascending leagues and achieving similar statistics to those at the time of injury. For pitchers who returned for at least 1 year and to their same or higher league, an ERA within 2.00 and WHIP within 0.500 were considered similar to before their injury, and for position players, a batting average within 0.100 was considered similar.11 In the investigation by Smith et al,33 return to previous level of play among pitchers was also defined as an ERA within 2.00 and WHIP within 0.500 of preoperative values. Two studies16,18 specified return to preinjury levels as being grade 0, indicating no limitation and a complete return to preinjury levels, with higher levels representing mild to severe limitation. Most studies used patient-reported outcomes to assess return to previous level of play.2-5,9,10,12,13,17,20,23-25,27-29,37,38 All players returned to the same sport when authors reported on return to previous level of play. Although patients may have been successful at returning to sport, they may not be pain- or symptom-free.
Duration of return to sport was only reported by Smith et al,33 citing mean career length on return to play being 3.67 ± 1.91 years, bringing into question the true long-term success of SLAP repair as reported in the studies. The lack of reporting on duration of return to sport offers a limitation in assessing return to preinjury levels for a sustained period, thus future studies may offer benefit by more carefully delineating an objective measure for return to preinjury levels while also monitoring length of return to sport prospectively.
Many authors discussing the results of SLAP repair have not adequately measured outcomes, such as duration of return to sport and changes in player statistics such as ERA, making true success difficult to discern from the included studies. There is heterogeneity associated with operative techniques, surgical indications, definition of return to sport, concomitant surgeries associated with SLAP repair, and postoperative rehabilitation, which may affect the generalizability of the return-to-sport rates. Although operative techniques varied mainly in terms of portal configuration, it has not been shown to have a significant impact on outcomes after SLAP repair.1
Last, the significant heterogeneity in operative technique and nonstandardized postoperative rehabilitation protocols, in combination with the lack of comparative studies, prevented a meta-analysis from being performed.2-4,9-11,13,17,18,20,23,25,27,37,38
Conclusion
Arthroscopic SLAP repair is associated with a fair return to sport, with 70% of individuals undergoing arthroscopic SLAP repair returning to sport. Concomitant shoulder pathologies in athletes are often associated with significantly higher complication rates and lower rates of return to sport. Athletes on average return to sport within approximately 9 months postoperatively. Return to sport among pitchers has been shown to be much lower (57.5%) than return to activity for nonpitcher counterparts (87.1%).
Supplemental Material
Supplemental material, DS_10.1177_1941738119873892_Appendix_1 for Return to Sport After Arthroscopic Superior Labral Anterior-Posterior Repair: A Systematic Review by Aarabi Thayaparan, James Yu, Nolan S. Horner, Timothy Leroux, Bashar Alolabi and Moin Khan in Sports Health: A Multidisciplinary Approach
Supplemental Material
Supplemental material, DS_10.1177_1941738119873892_Appendix_2 for Return to Sport After Arthroscopic Superior Labral Anterior-Posterior Repair: A Systematic Review by Aarabi Thayaparan, James Yu, Nolan S. Horner, Timothy Leroux, Bashar Alolabi and Moin Khan in Sports Health: A Multidisciplinary Approach
Footnotes
The following author declared potential conflicts of interest: Moin Khan is an Associate Editor for Sports Health.
References
- 1. Arroyo W, Misenhimer J, Cotter EJ, et al. Effect of anterior anchor on clinical outcomes of type II SLAP repairs in an active population. Orthopedics. 2019;42:e32-e38. [DOI] [PubMed] [Google Scholar]
- 2. Boesmueller S, Tiefenboeck TM, Hofbauer M, et al. Progression of function and pain relief as indicators for returning to sports after arthroscopic isolated type II SLAP repair—a prospective study. BMC Musculoskelet Disord. 2017;18:257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Boileau P, Parratte S, Chuinard C, Roussanne Y, Shia D, Bicknell R. Arthroscopic treatment of isolated type II SLAP lesions: biceps tenodesis as an alternative to reinsertion. Am J Sports Med. 2009;37:929-936. [DOI] [PubMed] [Google Scholar]
- 4. Brockmeier SF, Voos JE, Williams RJ, 3rd, Altchek DW, Cordasco FA, Allen AA. Outcomes after arthroscopic repair of type-II SLAP lesions. J Bone Joint Surg Am. 2009;91:1595-1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Burkhart SS, Morgan C. SLAP lesions in the overhead athlete. Orthop Clin North Am. 2001;32:431-441. [DOI] [PubMed] [Google Scholar]
- 6. Burkhart SS, Morgan CD. The peel-back mechanism: its role in producing and extending posterior type II SLAP lesions and its effect on SLAP repair rehabilitation. Arthroscopy. 1998;14:637-640. [DOI] [PubMed] [Google Scholar]
- 7. Burkhart SS, Morgan CD, Kibler WB. Shoulder injuries in overhead athletes: The “dead arm” revisited. Clin Sports Med. 2000;19:125-158. [DOI] [PubMed] [Google Scholar]
- 8. Chalmers PN, Monson B, Frank RM, et al. Combined SLAP repair and biceps tenodesis for superior labral anterior–posterior tears. Knee Surg Sports Traumatol Arthrosc. 2016;24:3870-3876. [DOI] [PubMed] [Google Scholar]
- 9. Cohen DB, Coleman S, Drakos MC, et al. Outcomes of isolated type II SLAP lesions treated with arthroscopic fixation using a bioabsorbable tack. Arthroscopy. 2006;22:136-142. [DOI] [PubMed] [Google Scholar]
- 10. Denard PJ, Lädermann A, Parsley BK, Burkhart SS. Arthroscopic biceps tenodesis compared with repair of isolated type II SLAP lesions in patients older than 35 years. Orthopedics. 2014;37:e292-e297. [DOI] [PubMed] [Google Scholar]
- 11. Fedoriw WW, Ramkumar P, McCulloch PC, Lintner DM. Return to play after treatment of superior labral tears in professional baseball players. Am J Sports Med. 2014;42:1155-1160. [DOI] [PubMed] [Google Scholar]
- 12. Friel NA, Karas V, Slabaugh MA, Cole BJ. Outcomes of type II superior labrum, anterior to posterior (SLAP) repair: prospective evaluation at a minimum two-year follow-up. J Shoulder Elbow Surg. 2010;19:859-867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gilliam BD, Douglas L, Fleisig GS, et al. Return to play and outcomes in baseball players after superior labral anterior-posterior repairs. Am J Sports Med. 2018;46:109-115. [DOI] [PubMed] [Google Scholar]
- 14. Gorantla K, Gill C, Wright RW. The outcome of type II SLAP repair: a systematic review. Arthroscopy. 2010;26:537-545. [DOI] [PubMed] [Google Scholar]
- 15. Huang H, Zheng X, Li P, Shen H. Arthroscopic reconstruction of shoulder’s labrum with extensive tears. Int J Surg. 2013;11:876-881. [DOI] [PubMed] [Google Scholar]
- 16. Ide J, Maeda S, Takagi K. Sports activity after arthroscopic superior labral repair using suture anchors in overhead-throwing athletes. Am J Sports Med. 2005;33:507-514. [DOI] [PubMed] [Google Scholar]
- 17. Kim DS, Park HK, Park JH, Yoon WS. Ganglion cyst of the spinoglenoid notch: comparison between SLAP repair alone and SLAP repair with cyst decompression. J Shoulder Elbow Surg. 2012;21:1456-1463. [DOI] [PubMed] [Google Scholar]
- 18. Kim SH, Ha KI, Kim SH, Choi HJ. Results of arthroscopic treatment of superior labral lesions. J Bone Joint Surg Am. 2002;84:981-985. [DOI] [PubMed] [Google Scholar]
- 19. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159-174. [PubMed] [Google Scholar]
- 20. Maier D, Jaeger M, Ogon P, Bornebusch L, Izadpanah K, Suedkamp NP. Suture anchors or transglenoidal sutures for arthroscopic repair of isolated SLAP-2 lesions? A matched-pair comparison of functional outcome and return to sports. Arch Orthop Trauma Surg. 2013;133:227-235. [DOI] [PubMed] [Google Scholar]
- 21. Moher D, Liberati A, Tetzlaff J, Altman DG; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Morgan CD, Burkhart SS, Palmeri M, Gillespie M. Type II slap lesions: three subtypes and their relationships to superior instability and rotator cuff tears. Arthroscopy. 1998;553-565. [DOI] [PubMed] [Google Scholar]
- 23. Neri BR, ElAttrache NS, Owsley KC, Mohr K, Yocum LA. Outcome of type II superior labral anterior posterior repairs in elite overhead athletes: effect of concomitant partial-thickness rotator cuff tears. Am J Sports Med. 2011;39:114-120. [DOI] [PubMed] [Google Scholar]
- 24. Neuman BJ, Boisvert CB, Reiter B, Lawson K, Ciccotti MG, Cohen SB. Results of arthroscopic repair of type II superior labral anterior posterior lesions in overhead athletes: assessment of return to preinjury playing level and satisfaction. Am J Sports Med. 2011;39:1883-1888. [DOI] [PubMed] [Google Scholar]
- 25. Park JY, Chung SW, Jeon SH, Lee JG, Oh KS. Clinical and radiological outcomes of type 2 superior labral anterior posterior repairs in elite overhead athletes. Am J Sports Med. 2013;41:1372-1379. [DOI] [PubMed] [Google Scholar]
- 26. Podlog L, Dimmock J, Miller J. A review of return to sport concerns following injury rehabilitation: practitioner strategies for enhancing recovery outcomes. Phys Ther Sport. 2011;12:36-42. [DOI] [PubMed] [Google Scholar]
- 27. Provencher MT, McCormick F, Dewing C, McIntire S, Solomon D. A prospective analysis of 179 type 2 superior labrum anterior and posterior repairs: outcomes and factors associated with success and failure. Am J Sports Med. 2013;41:880-886. [DOI] [PubMed] [Google Scholar]
- 28. Rhee YG, Lee D, Lim C. Unstable isolated SLAP lesion: clinical presentation and outcome of arthroscopic fixation. Arthroscopy. 2005;21:1099. [DOI] [PubMed] [Google Scholar]
- 29. Samani JE, Marston SB, Buss DD. Arthroscopic stabilization of type II SLAP lesions using an absorbable tack. Arthroscopy. 2001;17:19-24. [DOI] [PubMed] [Google Scholar]
- 30. Sayde WM, Cohen SB, Ciccotti MG, Dodson CC. Return to play after type II superior labral anterior-posterior lesion repairs in athletes: a systematic review. Clin Orthop Relat Res. 2012;470:1595-1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Schroder CP, Skare O, Gjengedal E, Uppheim G, Reikerås O, Brox JI. Long-term results after SLAP repair: a 5-year follow-up study of 107 patients with comparison of patients aged over and under 40 years. Arthroscopy. 2012;28:1601-1607. [DOI] [PubMed] [Google Scholar]
- 32. Sciascia A, Myers N, Kibler WB, Uhl TL. Return to preinjury levels of participation after superior labral repair in overhead athletes: a systematic review. J Athl Train. 2015;50:767-777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Smith R, Lombardo DJ, Petersen-Fitts GR, et al. Return to play and prior performance in Major League Baseball pitchers after repair of superior labral anterior-posterior tears. Orthop J Sports Med. 2016;4:2325967116675822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Snyder SJ, Banas MP, Karzel RP. An analysis of 140 injuries to the superior glenoid labrum. J Shoulder Elbow Surg. 1995;4:243-248. [DOI] [PubMed] [Google Scholar]
- 35. Snyder SJ, Karzel RP, Pizzo WD, Ferkel RD, Friedman MJ. Arthroscopy classics. SLAP lesions of the shoulder. Arthroscopy. 2010;26:1117. [DOI] [PubMed] [Google Scholar]
- 36. Trantalis JN, Sohmer S, More KD, et al. Arthroscopic repair of type II SLAP lesions: clinical and anatomic follow-up. Int J Shoulder Surg. 2015;9:74-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Waterman BR, Arroyo W, Heida K, Burks R, Pallis M. SLAP repairs with combined procedures have lower failure rate than isolated repairs in a military population: surgical outcomes with minimum 2-year follow-up. Orthop J Sports Med. 2015;3:2325967115599154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Yung PS, Fong DT, Kong MF, et al. Arthroscopic repair of isolated type II superior labrum anterior-posterior lesion. Knee Surg Sports Traumatol Arthrosc. 2008;16:1151-1157. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, DS_10.1177_1941738119873892_Appendix_1 for Return to Sport After Arthroscopic Superior Labral Anterior-Posterior Repair: A Systematic Review by Aarabi Thayaparan, James Yu, Nolan S. Horner, Timothy Leroux, Bashar Alolabi and Moin Khan in Sports Health: A Multidisciplinary Approach
Supplemental material, DS_10.1177_1941738119873892_Appendix_2 for Return to Sport After Arthroscopic Superior Labral Anterior-Posterior Repair: A Systematic Review by Aarabi Thayaparan, James Yu, Nolan S. Horner, Timothy Leroux, Bashar Alolabi and Moin Khan in Sports Health: A Multidisciplinary Approach