Supplemental Digital Content is Available in the Text.
Key Words: chronic pain, HIV, opioid, substance use disorder
Background:
Chronic pain is common in people living with HIV (PLWH). Few studies have evaluated the association between the diagnoses of chronic pain, substance use disorder (SUD), and HIV-related outcomes in clinical settings over a 10-year period.
Methods:
Using electronic medical records, the study described psychiatric diagnoses, pain medication, and HIV-related variables in PLWH and examined the factors associated with pain diagnosis and HIV-related outcomes.
Results:
Among 3528 PLWH, more than one-third exhibited a chronic pain diagnosis and more than one-third a psychiatric disorder. Chronic pain diagnosis has been associated with SUD and mood and anxiety disorders and occurred before SUD or psychiatric disorders about half of the time. Opioids have been commonly prescribed for pain management, more often than nonopioid analgesic, without any change in prescription pattern over the 10-year period. A dual diagnosis of pain and SUD has been associated with more psychiatric disorders and had a negative impact on the pain management by requesting more health care utilization and higher frequency of both opioid and nonopioid medication prescriptions. Chronic pain and SUD had a negative impact on ART adherence. SUD but not chronic pain has been associated with an unsuppressed HIV viral load.
Conclusions:
In the current intertwining opioid prescription and opioid epidemic, opioids are still commonly prescribed in PLWH in HIV care. A diagnosis of chronic pain and/or SUD worsened the HIV-related outcomes, emphasizing the potential risk of the HIV epidemic. These findings called for a better coordinated care program in HIV clinics.
INTRODUCTION
Chronic pain is a common comorbidity in people living with HIV (PLWH). Pain conditions, neuropathic and musculoskeletal pain principally, can affect individuals at any stage of the HIV illness.1 The improvement of combination antiretroviral therapy (ART) has decreased the side effects and notably neuropathic pain.2 However, pain symptoms are still more prevalent in PLWH than general population.3 Psychiatric disorders are also reported more often by PLWH than noninfected individuals.4,5 Recent literature has recognized that chronic pain has a negative impact on HIV care, with a decrease of ART adherence,6 elevated depressive symptoms also correlated with a decrease of ART adherence,7 and an increase of substance use.8 Despite these negative correlations, chronic pain is still undertreated in PLWH probably because of the complexity of ART regimen and potential interactions with pain medication, the higher risks of side effects, and the psychiatric and substance use comorbidities.9,10
Although clinical guidelines for the treatment of chronic pain11 stated that opioid should not be a first-line treatment for chronic pain, opioids have been often prescribed.12,13 In the context of widely diverted and improperly used opioids leading to the current national epidemic of opioid overdoses and opiate use disorders in the United States, prescribing practices for opioids has been questioned. A history of substance use and depression is common among HIV-positive individuals and has been identified as risk factors for opioid medication diversion14 and opiate use disorder.15 Opioid medication has been associated with high risk of injection drug use,16 poorer ART adherence,16 and increased sex risk behavior,17 representing a potential risk of the HIV epidemic. However, little is known on the existence of a detailed evaluation of substance use and psychiatric comorbidities before the opioid prescriptions in clinical settings. Similarly, the prescription patterns of nonopioid medications for pain management have been rarely reported. Furthermore, little is known on the impact of pain management and PLWH comorbidities on HIV care in clinical settings.
Routinely collected electronic health records offered the opportunity to examine integrated and real-time health care use and practices in large-scale and diverse samples.18
The objective of this article was to examine chronic noncancer pain, mental health, and substance use disorder (SUD) diagnoses and to evaluate their associations with HIV-related outcomes in PLWH in HIV care using medical health records.
METHODS
Study Sample
This study, approved by the University of Pennsylvania Institutional Review Board, used deidentified health record database that aggregated electronic medical records of any individual who has ever received care in any of the University of Pennsylvania health system facilities.
In the database, we identified PLWH aged 18 years and older who have received HIV care at one of the outpatient HIV clinics within the University of Pennsylvania health system between 2007 and 2017. Although the database gathered records since 1995, we did not select individuals who have received HIV care before 2007 to limit the bias of the type of ART (with potential more side effects) they received.
Measures
Sociodemographic variables, encounter and outpatient visit details, International Classification of Diseases (ICD-9 and ICD-10) coded diagnosis, prescribed medications, and laboratory test results were extracted from the database.
Diagnoses of chronic noncancer pain (ie, musculoskeletal chronic pain, neuralgia, neuritis, radiculopathy, facial pain, fibromyalgia, causalgia, and chronic pain), psychiatric disorders (ie, mood disorders, anxiety disorders, psychosis, suicide attempt, and ideation), and SUDs have been defined from ICD-9 or ICD-10 diagnoses. The ICD-9 and ICD-10 codes used for the query can be found in Supplemental material (see Table S1, Supplemental Digital Content, http://links.lww.com/QAI/B374).
Individuals have been considered receiving pharmacological treatment for chronic pain if they received either more than 1 prescription, either a prescription for at least 90-day worst of medication. Pain medications have been grouped by class, ie, opioids, nonsteroidal anti-inflammatory drug (NSAID), muscle relaxant, antidepressant, antianxiety, and antipsychotic agents.
Retention in HIV care has been defined according to the WHO standard, ie, encounter 2 visits per year 6 months apart and/or antiretroviral prescription refill every 6 months. The viral load has been classified as detectable if the last available measure reported more than 40 copies/mL.
Analyses
The characteristics of the sample including demographic, psychiatric and chronic pain diagnoses, prescribed pain medications, and encounter visits have been described for the whole sample.
Changes in the management of chronic pain between 2007 and 2017 have been evaluated by comparing (Pearson χ2) the prevalence of pharmacological treatment and the type of medication prescribed for pain management according to the year of the chronic pain diagnosis.
We defined 4 groups of individuals according to chronic noncancer pain and SUD diagnosis endorsement, ie, no chronic pain and no SUD, no chronic pain and SUD, chronic pain and no SUD, and chronic pain and SUD. We examined group differences on demographics, psychiatric diagnoses, pain medications, and HIV care outcomes (χ2 tests for categorical variables and analysis of variance for continuous variables).
Multivariable logistic model has been performed to examine the factors associated with a chronic pain diagnosis at any time during the follow-up (no pain as a reference), controlling for demographics and length of observation (defined as time between first to last visit on the medical records).
Another multivariable logistic model has been performed to evaluate the factors associated with suppressed viral load, evaluated as the last available viral load measure after at least 18 months of treatment. This last model has been performed on a sample of individuals who has been in HIV care for at least 18 months to only count individuals who have received ART long enough to potentially achieve suppressed viral load (n = 949).
All data have been analyzed using JMP Pro Version 13.2 (SAS Institute, Inc., Cary, NC).
RESULTS
Sample Characteristics
The sample included 3528 individuals, mainly male (73.3%), African American (64.1%), and white (27.6%). The individuals were 41.9 (SD = 13.1) years old on average at their first HIV care encounter visit within the University of Pennsylvania health system. They had an average clinical record history of 1788 days (SD = 1,120, median = 1661, q1 = 682, q3 = 2681) at the HIV clinic.
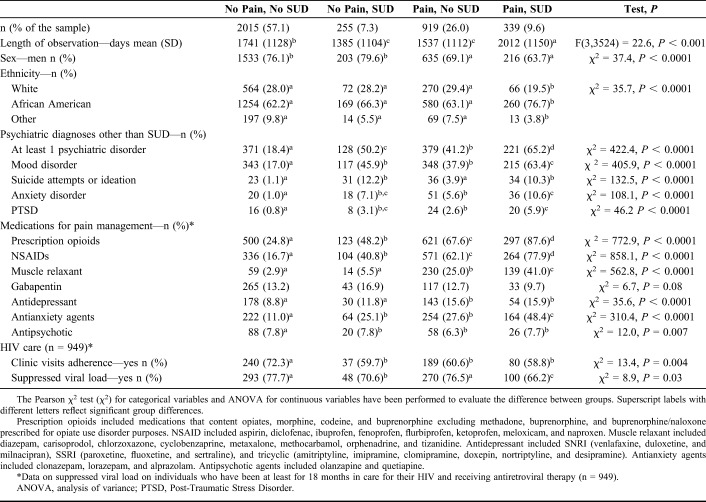
More than one-third exhibited at least 1 psychiatric disorder (38.1%), mostly mood disorder (29.0%) and SUD (16.8%) (Fig. 1). The type of SUD was unspecified for 23% of the individuals; the others met the following SUDs: cocaine (17.6%), alcohol (17.1%), opiate (14.6%), cannabis (6.6%), amphetamines (3.9%), and sedatives (1.2%).
FIGURE 1.
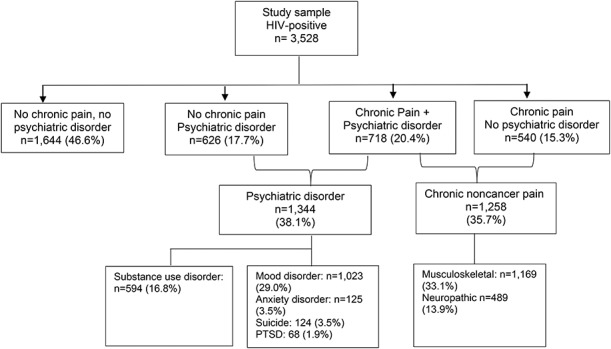
Diagnoses (ICD-9 or ICD-10) encounters for HIV-positive individuals engaged in HIV care at the University of Pennsylvania health system during the 2007–2017 period (n = 3528).
More than one-third exhibited a chronic noncancer pain diagnosis (35.7%), mostly musculoskeletal chronic pain (33.1%) (Fig. 1). Most of the individuals (84.3%) received a diagnosis of chronic pain after HIV diagnosis. The mean length of time from the first visit at HIV clinic and the pain diagnosis was 951.1 days (SD = 902.3, median = 693.5, q1 = 186.8, q3 = 1519.3). On average, the individuals had 11.2 visits (SD = 17.9, median = 5.0, q1 = 2.0, q3 = 13.0) for pain management.
More than half (57.1%) of the individuals with a diagnosis of chronic pain also met a diagnosis of psychiatric disorder (including SUD). The diagnosis of chronic pain was made before a mental health disorder (excluding SUD) diagnosis for 30.0%, within the same year for 31.3% and after for 38.7% of the individuals. The diagnosis of chronic pain was made before an SUD diagnosis for 58.7%, within the same year for 23.9% and after for 17.4% of the individuals.
Comorbid diagnoses of SUD and/or mental health disorder to the chronic pain diagnosis were significantly associated with the number of visits for pain management (P < 0.0001), with 10.4 visits (SD = 16.8) for individuals who met chronic pain diagnosis only, 13.4 visits (SD = 21.4) for individuals who met chronic pain diagnosis and SUD diagnosis, 17.7 visits (SD = 21.8) for individuals who met chronic pain diagnosis and mental health disorder diagnosis, and 29.2 visits (SD = 26.5) for individuals who met chronic pain diagnosis and both substance use and mental health disorder diagnoses.
Treatment of Chronic Noncancer Pain Over the Period 2007–2017
The majority (93.1%) of the individuals who endorsed a chronic pain diagnosis received more than 1 prescription or a prescription covering 90 days or more of pharmacological treatment for pain management.
Figure 2 displays the type of pharmacological treatment prescribed per year of the chronic pain diagnosis. Opioids have been commonly prescribed (41.4%), followed by NSAIDs (36.1%), antianxiety agents (33.2%), gabapentin (13.0%), muscle relaxant (12.5%), antidepressants (11.5%), and antipsychotics (5.4%). There was no change over the past 10 years for opioids (P = 0.15), gabapentin (P = 0.26), antidepressants (P = 0.41), antianxiety agents (P = 0.54), and antipsychotics (P = 0.08). There was a significant change in NSAIDs (P = 0.04) and muscle relaxants (P < 0.001) which became less prescribed after 2009.
FIGURE 2.
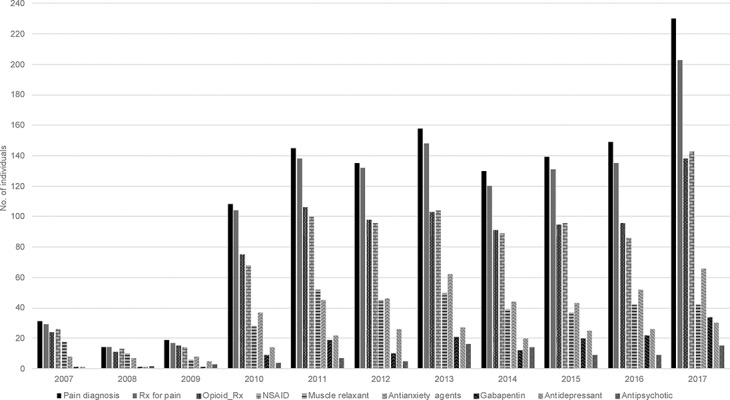
Change in noncancer chronic pain diagnosis and prescribed medications for pain management by year of pain diagnosis (2007–2017). Prescription opioids included medications that content opiates, morphine, codeine, and buprenorphine excluding methadone, buprenorphine, and buprenorphine/naloxone prescribed for opiate use disorder purposes. NSAID included aspirin, diclofenac, ibuprofen, fenoprofen, flurbiprofen, ketoprofen, meloxicam, and naproxen. Muscle relaxant included diazepam, carisoprodol, chlorzoxazone, cyclobenzaprine, metaxalone, methocarbamol, orphenadrine, and tizanidine. Antidepressant included SNRI (venlafaxine, duloxetine, and milnacipran), SSRI (paroxetine, fluoxetine, and sertraline), and tricyclic (amitriptyline, imipramine, clomipramine, doxepin, nortriptyline, and desipramine). Antianxiety agents included clonazepam, lorazepam, and alprazolam. Antipsychotic agents included olanzapine and quetiapine. Rx for pain, number of individuals who received a prescription of at least one of these above medications. SNRI, Serotonine Norepinephrine Reuptake Inhibitor; SSRI, Selective Serotonine Reuptake Inhibitor.
Comparison According to Chronic Pain and SUD Diagnoses
Table 1 displays the comparison between the 4 groups, ie, no chronic pain and no SUD (n = 2015), no chronic pain and SUD (n = 255), chronic pain and no SUD (n = 919), and chronic pain and SUD (n = 339).
TABLE 1.
Characteristic of the Individuals According to the Diagnoses of Noncancer Chronic Pain (Pain) and SUD (n = 3528)
Although the sample consisted in a majority of men, there were more women in the groups who met chronic pain diagnosis (P < 0.0001). Exhibiting 1 diagnosis of either pain either SUD increased the likelihood to endorse at least 1 psychiatric disorder, while exhibiting a dual diagnosis of pain and SUD increased this likelihood even more for mood (P < 0.0001), suicide (P < 0.0001), anxiety (P < 0.0001), and post-traumatic stress disorder (P < 0.0001). Opioid prescriptions for pain management have been highly common even in the group that did not meet chronic pain diagnosis, questioning either the need for opioid prescription or the accuracy of the diagnosis. Individuals with a dual diagnosis of chronic pain and SUD received significantly more often an opioid prescription for pain management than individuals who endorsed chronic pain only (87.6% vs. 67.6, P < 0.0001). Similarly, the dual diagnosis group was more likely to receive NSAID (P < 0.0001), muscle relaxant (P < 0.0001), antidepressants (P < 0.0001), and antianxiety agents (P < 0.0001) for pain management.
Factors Associated With a Diagnosis of Chronic Noncancer Pain
The logistic model showed that individuals with a diagnosis of chronic pain were more likely women [odds ratio (OR) = 1.75, 95% confidence interval (CI): 1.18 to 2.59], met at least 1 SUD diagnosis (OR = 1.72, 95% CI: 1.14 to 2.61), met mood disorder diagnosis (OR = 2.03, 95% CI: 1.42 to 2.89), and met anxiety disorder diagnosis (OR = 3.61, 95% CI: 1.34 to 9.71).
HIV-Related Outcomes
Individuals who endorsed a chronic pain diagnosis or an SUD diagnosis were significantly less adherent to their HIV care (P = 0.004).
Among individuals who were enrolled in HIV care and received ART for at least 18 months (n = 949), those with an unsuppressed viral load were more likely African American (OR = 2.75, 95% CI: 1.73 to 4.60) or another race (OR = 2.50, 95% CI: 1.07 to 5.58) than white and met SUD diagnosis (OR = 1.70, 95% CI: 1.18 to 2.45). A diagnosis of chronic pain was not associated with viral load suppression.
DISCUSSION
This study provides a picture of the prevalence and the management of chronic noncancer pain occurring in HIV clinic settings using 10-year PLWH health records of a large health care database. Our findings showed that more than one-third of the PLWH in HIV care met chronic noncancer pain diagnosis, in the 24%–48% range previously reported in the antiretroviral-era literature.7,10,19–21 Psychiatric comorbidities were prevalent (38%), and 20% met diagnoses for both psychiatric disorder and chronic pain, also consistent with previous literature that found associations between chronic pain and depression,9,20,22 and history of SUD9,22–24 in PLWH.
More than half of the chronic pain diagnoses have been recorded before SUD diagnoses. Previous studies have reported that most opiate use disorder individuals developed the disorder after chronic pain.22 Almost all the PLWH who have been identified as having chronic pain received a pharmacological treatment for the management of the chronic pain, inconsistent with a literature review that concluded that chronic pain is untreated in PWLH.6,24 Although short-term course of short-acting and low-dose opioids could be an efficient medication for acute pain, individuals with an history of SUD represent a more vulnerable population to develop SUD.25,26 The most prescribed medications for pain management were opiates, without any change over the 10-year study period, although the guidelines for the management of chronic pain in PWLH highlighted the interaction between opioid medication and ART and stated that opioids should not be the first-line treatment for pain management.11 These findings are consistent with previous studies showing that opioids are commonly prescribed in PWLH.3,13,16,27,28 Because of the intertwining opioid prescriptions and opioid epidemic in the United States, states have responded to this crisis through several interventions including new regulations and legislations. Although interventions occurred in Pennsylvania, recent available data showed an increase of opioid prescriptions between 2006 and 2017.29 However, parallel to the opioid prescriptions, nonopioid prescriptions were also common. PWLH with a dual diagnosis of chronic pain and SUD received more often both opioid and nonopioid prescriptions for pain management. Because primary care providers deliver the majority of pain care and they are not typically trained in pain medicine25 might have explained the high rates of pharmacological medications for pain management.
Interestingly, approximately 25% of the sample received several prescriptions for pain management, although they did not have any recorded chronic pain diagnosis. Other studies have also reported prescription of antidepressants and opiates for pain management in PWLH even without a diagnosis of chronic pain.7 This could be inherent to the use of electronic medical records. Although the use of health records provides the most comprehensive individual health histories,30 the methodological rigor is weaker than data collected as part of a research study. The data captured in electronic health records are dependent on the physician documentation, and also, medical insurance requirements thus introduced uncontrolled biases. Thus, the accuracy of the diagnoses is uncertain, and some PWLH may not have been identified as meeting SUDs and chronic pain diagnosis. However, with our query similar to the one used in other studies,31 we could consider that the mislabeled of chronic pain was very limited but SUDs might have been underreported, as previously stated in other studies.22 Moreover, when reported, most of the SUD diagnosis have been nonspecified prevented us to explore association between opioid prescription and development of opiate use disorder. Also, as record-based research, we could not have access to PWLH diagnoses outside the university of Pennsylvania health system. Because the University of Pennsylvania health system predominantly serves individuals without private insurance, with Medicare, Medicaid, or no payer as payer sources, the generalizability of the findings could be potentially limited.
Despite these limitations, our study showed that chronic pain diagnosis was associated with SUDs and psychiatric disorders and that SUDs had an impact on the management of chronic pain, leading to an increase of health care service utilization and more visits for pain management, as reported in non-HIV population.22 SUD has also a negative impact on HIV care and has been found associated with unsuppressed viral load. We did not find association between pain and suppressed viral load. However, untreated pain increased the incidence of nonmedical use of prescription opioids in HIV and non-HIV individuals and has a negative impact on antiretroviral treatment adherence and viral load suppression in PWLH,4,6,8 as well as increased the risk to develop SUDs, including alcohol use disorder.8
The high rate of chronic pain and co-occurring substance use and psychiatric comorbidities in PLWH in HIV care underscores the need to develop more coordinated care plans integrating the management of pain and psychiatric disorders including SUDs in HIV clinic. The management of pain should align better with the pain management guidelines for PLWH and should minimize the use of opioid prescription, the benefits of which have been questionable in the management of chronic pain,14,15 and better integrate alternative treatments including nonopioid analgesics and nonpharmacologic techniques.15
Footnotes
This publication resulted in part from research supported by the Penn Center for AIDS Research (CFAR) (P30 AI 045008 - Ronald Collman, PI), the Penn Mental Health AIDS Research Center (PMHARC) (P30 MH 097488 - Dwight Evans, PI), P30 MH097488-06, and the CFAR Social & Behavioral Science Research Network National Scientific Meeting (SBSRN) (R13 HD 074468 - Michael Blank, PI).
The authors have no conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jaids.com).
REFERENCES
- 1.Krashin DL, Merrill JO, Trescot AM. Opioids in the management of HIV-related pain. Pain Physician. 2012;15(3 suppl):ES157–168. [PubMed] [Google Scholar]
- 2.Lee AJ, Bosch RJ, Evans SR, et al. Patterns of peripheral neuropathy in ART-naive patients initiating modern ART regimen. J Neurovirol. 2015;21:210–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Canan C, Alexander GC, Moore R, et al. Medicaid trends in prescription opioid and non-opioid use by HIV status. Drug Alcohol Depend. 2019;197:141–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barry DT, Goulet JL, Kerns RK, et al. Nonmedical use of prescription opioids and pain in veterans with and without HIV. Pain. 2011;152:1133–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jiao JM, So E, Jebakumar J, et al. Chronic pain disorders in HIV primary care: clinical characteristics and association with healthcare utilization. Pain. 2016;157:931–937. [DOI] [PubMed] [Google Scholar]
- 6.Surratt HL, Kurtz SP, Levi-Minzi MA, et al. Pain treatment and antiretroviral medication adherence among vulnerable HIV-positive patients. AIDS Patient Care STDs. 2015;29:186–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Uebelacker LA, Weisberg RB, Herman DS, et al. Chronic pain in HIV-infected patients: relationship to depression, substance use, and mental health and pain treatment. Pain Med. 2015;16:1870–1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Newville H, Roley J, Sorensen JL. Prescription medication misuse among HIV-infected individuals taking antiretroviral therapy. J Subst Abuse Treat. 2015;48:56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Isenberg SR, Maragh-Bass AC, Ridgeway K, et al. A qualitative exploration of chronic pain and opioid treatment among HIV patients with drug use disorders. J Opioid Manag. 2017;13:5–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miaskowski C, Penko JM, Guzman D, et al. Occurrence and characteristics of chronic pain in a community-based cohort of indigent adults living with HIV infection. J Pain. 2011;12:1004–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bruce RD, Merlin J, Lum PJ, et al. 2017 HIVMA of IDSA clinical practice guideline for the management of chronic pain in patients living with HIV. Clin Infect Dis. 2017;65:e1–e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mello A, Gravel T. HIV pain management challenges and alternative therapies. Nursing. 2017;47:67–70. [DOI] [PubMed] [Google Scholar]
- 13.Turner AN, Maierhofer C, Funderburg NT, et al. High levels of self-reported prescription opioid use by HIV-positive individuals. AIDS Care. 2016;28:1559–1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Voon P, Karamouzian M, Kerr T. Chronic pain and opioid misuse: a review of reviews. Substance Abuse Treat Prev Pol. 2017;12:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Volkow ND, McLellan AT. Opioid abuse in chronic pain—misconceptions and mitigation strategies. N Engl J Med. 2016;374:1253–1263. [DOI] [PubMed] [Google Scholar]
- 16.Canan CE, Chander G, Monroe AK, et al. High-risk prescription opioid use among people living with HIV. J Acquir Immune Defic Syndr. 2018;78:283–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Benotsch EG, Martin AM, Koester S, et al. Nonmedical use of prescription drugs and HIV risk behavior in gay and bisexual men. Sex Transm Dis. 2011;38:105–110. [DOI] [PubMed] [Google Scholar]
- 18.Kruse CS, Stein A, Thomas H, et al. The use of electronic health records to support population health: a systematic review of the literature. J Med Syst. 2018;42:214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cervia LD, McGowan JP, Weseley AJ. Clinical and demographic variables related to pain in HIV-infected individuals treated with effective, combination antiretroviral therapy (cART). Pain Med. 2010;11:498–503. [DOI] [PubMed] [Google Scholar]
- 20.Merlin JS, Westfall AO, Raper JL, et al. Pain, mood, and substance abuse in HIV: implications for clinic visit utilization, antiretroviral therapy adherence, and virologic failure. J Acquir Immune Defic Syndr. 2012;61:164–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Merlin JS. Chronic pain in patients with HIV infection: what clinicians need to know. Top Antivir Med. 2015;23:120–124. [PMC free article] [PubMed] [Google Scholar]
- 22.Hser YI, Mooney LJ, Saxon AJ, et al. Chronic pain among patients with opioid use disorder: results from electronic health records data. J Subst Abuse Treat. 2017;77:26–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tsao JC, Soto T. Pain in persons living with HIV and comorbid psychologic and substance use disorders. Clin J Pain. 2009;25:307–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parker R, Stein DJ, Jelsma J. Pain in people living with HIV/AIDS: a systematic review. J Int AIDS Soc. 2014;17:18719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cheatle MD. Facing the challenge of pain management and opioid misuse, abuse and opioid-related fatalities. Expert Rev Clin Pharmaco. 2016;9:751–754. [DOI] [PubMed] [Google Scholar]
- 26.Cheatle MD. The impact of prescription drug monitoring programs and prescribing guidelines on opioid prescribing behaviors: a time for institutional and regulatory changes. Pain Med. 2017;18:823–824. [DOI] [PubMed] [Google Scholar]
- 27.Sharma A, Hoover DR, Shi Q, et al. Frequent occurrence of pain and prescription opioid use for treatment of pain among women with and at risk for HIV infection. AIDS Behav. 2017;22:2008–2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Becker WC, Gordon K, Edelman EJ, et al. Trends in any and high-dose opioid analgesic receipt among aging patients with and without HIV. AIDS Behav. 2016;20:679–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schieber LZ, Guy GP, Jr, Seth P, et al. Trends and patterns of geographic variation in opioid prescribing practices by state, United States, 2006–2017. JAMA Netw Open. 2019;2:e190665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tu K, Mitiku TF, Ivers NM, et al. Evaluation of electronic medical record administrative data linked database (EMRALD). Am J Manag Care. 2014;20:e15–21. [PubMed] [Google Scholar]
- 31.Tian TY, Zlateva I, Anderson DR. Using electronic health records data to identify patients with chronic pain in a primary care setting. J Am Med Inform Assoc. 2013;20:e275–e280. [DOI] [PMC free article] [PubMed] [Google Scholar]