Abstract
Introduction:
The receipt of remote clinical care for children via telecommunications (pediatric telemedicine) appears to improve access to and quality of care in U.S. emergency departments (EDs), but the actual prevalence and characteristics of pediatric telemedicine receipt remain unclear. We determined the prevalence and current applications of pediatric telemedicine in U.S. EDs, focusing on EDs that received telemedicine from clinicians at other facilities.
Methods:
We surveyed all 5,375 U.S. EDs to characterize emergency care in 2016. We then randomly surveyed 130 (39%) of the 337 EDs who reported receiving pediatric telemedicine. The second survey was administered by phone to ED directors primarily. It confirmed that the ED received pediatric telemedicine services in 2017 and asked about ED staffing and the nature, purpose, and concerns with pediatric telemedicine implementation.
Results:
The first survey (4,507/5,375, 84% response) showed that 337 (8%) EDs reported receiving pediatric telemedicine. Among the randomly sampled EDs completing the second survey (107/130, 82% response), 96 (90%) confirmed 2016 use and 89 (83%) confirmed 2017 use. Reasons for discontinuation included technical and scheduling concerns. Almost all who confirmed their pediatric telemedicine use in 2017 also reported 24/7 availability (98%). The most widely reported use was for patient placement and transfer coordination (80%). Many EDs (39%) reported no challenges with implementing pediatric telemedicine and described its utility. However, the most frequently reported challenges were process concerns (30%), such as concerns about slowing or interrupting providers’ work flow and technological concerns (14%).
Conclusion:
Few EDs receive telemedicine for the delivery of pediatric emergency care nationally. Among EDs that do use telemedicine for pediatric care, many report process concerns. Addressing these barriers through focused education or interventions may support EDs in further developing and optimizing this technological adjunct to pediatric emergency care.
Telemedicine is the remote provision of clinical care via audio or visual communications and can be administered to a facility by other hospitals or private companies.1 Typically, clinicians in one facility provide telemedicine to patients in a different facility that receive these services. In emergency departments (EDs), receipt of telemedicine has led to higher patient satisfaction and better patient outcomes, especially when EDs lack in-person specialist care (e.g., pediatric emergency medicine [PEM]).2 Telemedicine use in referring EDs is associated with improved stabilization of children admitted to a pediatric intensive care unit (PICU).3 Furthermore, pediatric critical care telemedicine consultations in rural EDs have demonstrated higher physician-rated quality of care and lower risk of physician-related ED medication errors compared with either telephone or no consultation, underscoring the value of telemedicine in this population4,5 Nevertheless, the prevalence, characteristics, and applications of receipt of pediatric telemedicine remain unclear. To address these knowledge gaps, we investigated the use of telemedicine for pediatric emergency care among U.S. EDs who reported receiving telemedicine services for pediatrics.
METHODS
Study Design
We administered two national surveys, both available in Data Supplement S1 (available as supporting information in the online version of this paper, which is available at http://onlinelibrary.wiley.com/doi/10.1111/acem.13629/full). The institutional review board determined that this study was exempt.
Study Protocol
From January through October 2017, we conducted a nine-question national survey of all U.S. EDs to characterize emergency care in 2016. Potential respondents were identified using the National Emergency Department Inventory (NEDI)-USA database,6 which comprises all 5,375 nonfederal, nonspecialty EDs open 24 hours/day, 7 days/week. Each ED director was mailed a one-page survey up to three times. For nonresponding EDs, we contacted ED staff by telephone to complete the survey by interview. The survey took approximately 2 minutes to complete.
A random sample of 130 (39%) of the 337 respondents who reported receiving pediatric telemedicine on the 2016 NEDI-USA survey were further surveyed to characterize their pediatric telemedicine use during 2017. This random sample was selected via a random number macro (Excel, Microsoft). The sample size of 130 was determined by calculating the 95% confidence intervals of expected proportions (e.g., 50%) in different samples sizes; 130 EDs yielded sufficiently precise estimates for 426 EDs.
A nine-question survey was administered to these EDs by telephone from February through May 2018. Respondents were also given the option of completing the survey online. The director of each ED was surveyed whenever possible, and the survey took approximately 5 minutes to complete. These survey questions were developed based on feedback from several telemedicine and national survey research experts and were first piloted over the phone in a random sample of 20 EDs that reported that they receive pediatric telemedicine.
Measurements
For the 2016 NEDI-USA survey, data collection included ED location, visit volumes, and basic pediatric and telemedicine characteristics. Receipt of telemedicine was assessed with the question, “Does your ED receive telemedicine services for patient evaluation?” The follow-up question to this was, “If your ED receives telemedicine services, does your ED utilize telemedicine for: (check all that apply),” with “pediatrics” listed as a check-box option. For the follow-up survey, data collection included availability of pediatric telemedicine, staffing of ED, purposes (applications) for pediatric telemedicine use, and challenges with implementation.
Data Analysis
All analyses were performed using Stata 14.2 (Stata-Corp). Descriptive statistics are presented as proportions and medians with interquartile ranges (IQRs). We examined national use of pediatric telemedicine by ED characteristics using chi-square or Wilcoxon rank sum test, as appropriate. All p-values were two-tailed, with p < 0.05 considered statistically significant.
RESULTS
Overall, 84% of 5,375 EDs responded to the 2016 NEDI-USA survey. Among EDs that responded to the survey item pertaining to pediatric telemedicine use (n = 4,410), 337 (8%) reported receiving pediatric telemedicine. EDs receiving pediatric telemedicine had a lower median annual ED visit volume than EDs that did not: 9,490 vs. 21,845 (p < 0.001). EDs that received pediatric telemedicine had a similar annual pediatric visit volume as EDs that did not (19% [IQR = 12%–25%] vs. 18% [IQR = 11%–25%]). As shown in Table 1, EDs receiving pediatric telemedicine were less likely to be urban (located in a core-based statistical area) than EDs that did not receive pediatric telemedicine (p < 0.001) and EDs overall. Approximately half (54%) of EDs receiving pediatric telemedicine were critical access hospitals, compared to 24% of EDs that did not receive pediatric telemedicine.
Table 1.
Characteristics of U.S. EDs by Receipt of Pediatric Telemedicine (n = 4,410)
| ED Characteristics | All EDs, n = 4,410 | EDs That Do Not Receive Pediatric Telemedicine, n = 4,073 |
EDs That Receive Pediatric Telemedicine, n = 337 |
p-value |
|---|---|---|---|---|
| Annual total ED visits | <0.001 | |||
| <10,000 | 1,380 (31) | 1,209 (30) | 171 (51) | |
| 10,000–19,999 | 746 (17) | 696 (17) | 50 (15) | |
| 20,000–39,999 | 1.051 (24) | 992 (24) | 59 (18) | |
| ≥40,000 | 1,233 (28) | 1,176 (29) | 57 (17) | |
| Percentage of annual ED visits by children | 0.10 | |||
| <15% | 1,368 (31) | 1,272 (31) | 96 (28) | |
| 15%–24.9% | 1,546 (35) | 1,411 (35) | 135 (40) | |
| 25%–49.9% | 831 (19) | 763 (19) | 68 (20) | |
| ≥50% | 121 (3) | 112 (3) | 9 (3) | |
| Unknown | 544 (12) | 515 (13) | 29 (9) | |
| Any PECC | 844 (19) | 790 (19) | 54 (16) | 0.13 |
| Physician PECC | 527 (12) | 492 (12) | 35 (10) | 0.36 |
| Nurse PECC | 623 (14) | 585 (14) | 38 (11) | 0.12 |
| Other PECC | 64 (1) | 60 (1) | 4 (1) | 0.68 |
| Regional location | <0.001 | |||
| Northeast | 549 (12) | 508 (12) | 41 (12) | |
| Midwest | 1,205 (27) | 1,082 (27) | 123 (37) | |
| South | 1,826 (41) | 1,740 (43) | 86 (26) | |
| West | 830 (19) | 743 (18) | 87 (26) | |
| In core base statistical area | <0.001 | |||
| No | 959 (22) | 803 (20) | 156 (46) | |
| Yes | 3,451 (78) | 3,270 (80) | 181 (54) | |
| Council of teaching hospital | 213 (5) | 206 (5) | 7 (2) | 0.01 |
| Academic ED | 163 (4) | 160 (4) | 3 (1) | 0.004 |
| Critical access hospital | 1,168 (26) | 987 (24) | 181 (54) | <0.001 |
Data are reported as n (%).
IQR = interquartile range; PECC = pediatric emergency care coordinator.
In the follow-up survey, 107 (82%) of the 130 randomly selected EDs responded; 99 completed the survey via telephone, and eight completed the survey online. Of these, 96 (90%) confirmed pediatric tele-medicine use in 2016, and 89 (83%) further confirmed use in 2017 (Data Supplement S1, Table S1). Given the confirmation rate, we estimate that 7% of EDs used telemedicine for pediatrics in 2017. Of the 18 respondents who did not confirm use in 2017, seven reported that pediatric telemedicine either had previously been used and then discontinued or was being set up. They cited technical and scheduling difficulties as reasons for discontinuation. Of the other 11 EDs, seven received telemedicine for nonpediatric applications, and four did not receive telemedicine at all, indicating that 10% of ED respondents in the follow-up survey were misclassified.
Frequency
Of the 89 respondents who confirmed ED capacity to receive pediatric telemedicine, 76 (85%) reported using the service at least once in 2017. Almost half the respondents (48%) reported use for evaluation of at least one infant aged < 1 year, and most (81%) reported evaluation of at least one child aged between 1 and 17.9 years.
Staffing and Applications
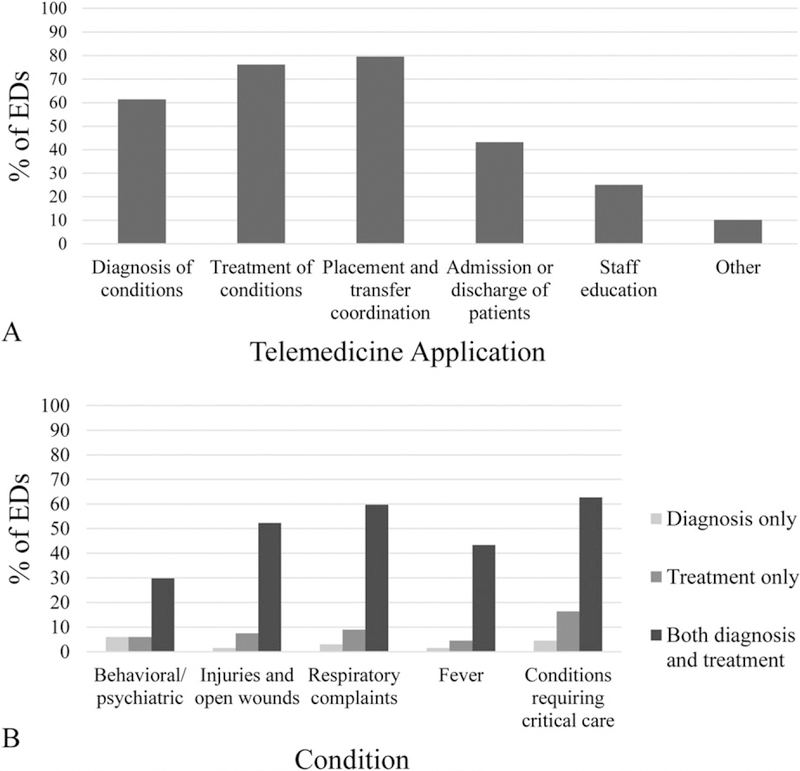
Almost all EDs receiving pediatric telemedicine reported never having a board-certified or board-eligible PEM physician (90%) or pediatrician (93%) working clinically in their ED. Among the none EDs with a PEM physician, four (44%) reported that they were on duty for ≥8 hours on a typical day. Among the six EDs with a pediatrician, one (17%) reported that they were on duty for ≥8 hours on a typical day. EDs also reported specific applications for pediatric telemedicine, and the conditions it was used to diagnose or treat (Figure 1); EDs most frequently reported using telemedicine for patient placement and transfer coordination (80%).
Figure 1.
Pediatric telemedicine use in U.S. EDs. (A) Applications of pediatric telemedicine use in U.S. EDs (n = 88). ED respondents selected all applicable applications. Write-in responses of “other” applications included neonatal resuscitation, pharmacy assistance, and orthopedics. (B) Conditions diagnosed and treated with pediatric telemedicine in U.S. EDs (n = 67). Figure excludes those that did not report using pediatric telemedicine to diagnose or treat any conditions (n = 21). ED respondents selected all applicable conditions. Bars within each condition are mutually exclusive, representing the percentage of responding EDs that used pediatric telemedicine to 1) only diagnose that condition, 2) only treat that condition, or 3) both diagnose and treat that condition.
Perceived Challenges
Many respondents (39%) reported no significant challenges with implementation of pediatric telemedicine in their ED. Others most frequently cited process (30%) and technology (14%) concerns (Table 1). Interestingly, 6% of total respondents reported an inadequate pediatric visit volume to observe challenges. Some respondents described difficulties getting staff members to remember pediatric telemedicine was available.
DISCUSSION
Telemedicine is defined as the remote provision of clinical care via audio or visual communications, and this study aimed to determine the prevalence, characteristics, and applications of telemedicine in EDs that receive pediatric telemedicine. Of the 4,410 U.S. EDs that responded to the NEDI-USA survey, 337 (8%) reported receiving pediatric telemedicine in 2016. This national survey allowed us to randomly sample a subset of EDs that receive pediatric telemedicine for a second, more focused survey on pediatric telemedicine. Briefly, most EDs receiving pediatric telemedicine had 24/7 access to this resource and were not staffed by a board-certified or board-eligible PEM physician or pediatrician, suggesting that telemedicine was filling a likely gap in pediatric specialist access. Placement and transfer coordination was the most commonly reported application, followed by treatment and diagnosis of conditions. Critical care conditions were most commonly treated or diagnosed with pediatric telemedicine. Although many EDs reported no concerns with implementing pediatric telemedicine, process and technology concerns were often cited, including difficulties incorporating into workflow and recalling resource availability. These are similar to the anticipated barriers (e.g., infrequent need to use) reported from a study that conducted qualitative interviews with ED providers.7 Of EDs that discontinued telemedicine between 2016 and 2017, scheduling and technical difficulties were frequently cited.
Many children in the United States lack timely access to EDs with high pediatric readiness, which underscores the potential benefit of pediatric telemedicine adoption in EDs in enabling access to pediatric-ready care where it otherwise would not be available.8 Further, pediatric telemedicine can improve equity and access to acute care in an urban setting, critical care quality in rural EDs,4,9 and stabilization of critical care transfers.3 Specifically, when compared with no consultations, pediatric telemedicine in rural EDs demonstrated higher physician-rated quality of care and lower risk of physician-related medication errors.5,9 Despite this evidence, we found only 8% of U.S. EDs currently receive pediatric telemedicine. Previously, clinicians identified factors affecting adoption of pediatric emergency telemedicine, including perceived usefulness and ease of use as well as contextual factors including geographical setting, culture, and personal experience.10 These factors are predictors that could increase the prevalence of this service nationwide. A survey of a different stakeholder group, caregivers whose children were transferred to pediatric EDs, showed that although most had never heard of telemedicine, they were receptive to its use.11
Approximately 15% of sampled EDs equipped with this technology did not use pediatric telemedicine at all in 2017. This infrequent use may be partially due to the challenges and concerns described above, particularly in EDs with low pediatric visit volumes. Moreover, while our surveys show that a subset of EDs across the U.S. do successfully implement this technology, factors such as perceived usefulness and ease of use will influence nationwide adoption, and education about telemedicine use among providers may help providers use this service more often in their EDs. This increased access to care may help improve patient outcomes both in underresourced rural settings with low pediatric volumes and in crowded urban EDs, narrowing gaps in access to pediatric emergency care.
LIMITATIONS
This study has several potential limitations. First, the NEDI-USA survey queried telemedicine use in 2016 while the follow-up survey queried 2017 use; however, this actually enabled us to identify EDs that discontinued use and to begin to understand reasons for discontinuation. Second, as a cross-sectional study, causal inferences are not possible. Third, because data were self-reported, there may be information bias, which we tried to mitigate by surveying ED leadership. Fourth, these two surveys do not address the actual process or clinical outcomes of receipt of pediatric telemedicine. Finally, while the national survey had 4,507 ED respondents, the follow-up survey only had 107 and only 89 confirmed receipt or capability to receive telemedicine for the evaluation of children in 2017. While response rates were strong (>80%), this limited our ability to examine independent relationships in multivariable regression models. As the 130 EDs in the follow-up survey comprise over one-third of the 337 EDs receiving pediatric telemedicine, we believe that this was a reasonable sample size to provide the first benchmark data on this topic.
CONCLUSIONS
Overall, 8% (337) of all EDs surveyed nationally reported receiving pediatric telemedicine in 2016. Of the 107 EDs further surveyed, 83% (89) confirmed use in 2017, from which we estimate that 7% of EDs used pediatric telemedicine. Most EDs using pediatric telemedicine were not staffed by board-certified or board-eligible pediatric emergency medicine physicians or pediatricians. Over one-third of respondents reported no challenges implementing pediatric telemedicine in their EDs, but this resource is used infrequently. We encourage further study of the reported challenges, particularly process and technological concerns and identification of the optimal approach to educating providers and staff on the role of pediatric telemedicine in EDs.
Supplementary Material
Acknowledgments
This study was supported by a grant from R Baby Foundation (New York, NY).
The funder had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
The authors have no relevant financial information or potential conflicts to disclose.
Supporting Information
The following supporting information is available in the online version of this paper available at http://onlinelibrary.wiley.com/doi/10.1111/acem.13629/full
Data Supplement S1. Supplemental material.
References
- 1.Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med 2017;377:1585–92. [DOI] [PubMed] [Google Scholar]
- 2.Ward MM, Jaana M, Natafgi N. Systematic review of telemedicine applications in emergency rooms. Int J Med Inform 2015;84:601–16 [DOI] [PubMed] [Google Scholar]
- 3.Dayal P, Hojman NM, Kissee JL, Litman RL, Nesbitt TS, Marcin JP. Impact of telemedicine on severity of illness and outcomes among children transferred from referring emergency departments to a children’s hospital PICU. Pediatr Crit Care Med 2016;17:516–21. [DOI] [PubMed] [Google Scholar]
- 4.Ronis SD, Mcconnochie KM, Wang H, Wood NE. Urban telemedicine enables equity in access to acute illness care. Telemed J E Health 2017;23:105–12. [DOI] [PubMed] [Google Scholar]
- 5.Dharmar M, Kuppermann N, Romano PS, et al. Telemedicine consultations and medication errors in rural emergency departments. Pediatrics 2013;132:1090–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sullivan AF, Richman IB, Ahn CJ, et al. A profile of US emergency departments in 2001. Ann Emerg Med 2006;48:694–701. [DOI] [PubMed] [Google Scholar]
- 7.Kim JW, Tiyyagura G, Langhan M. A qualitative analysis on general emergency medicine providers’ perceptions on pediatric emergency telemedicine. Pediatr Emerg Care 2017. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 8.Ray KN, Olson LM, Edgerton EA, et al. Access to high pediatric-readiness emergency care in the United States. J Pediatr 2018;194:225–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dharmar M, Romano PS, Kuppermann N, et al. Impact of critical care telemedicine consultations on children in rural emergency departments. Crit Care Med 2013;41:2388–95. [DOI] [PubMed] [Google Scholar]
- 10.Ray KN, Felmet KA, Hamilton MF, et al. Clinician attitudes toward adoption of pediatric emergency telemedicine in rural hospitals. Pediatr Emerg Care 2017;33:250–7. [DOI] [PubMed] [Google Scholar]
- 11.Mollen CJ, Henien M, Jacobs LM, Myers S. Parent perceptions on transfers to pediatric emergency departments and the role of telemedicine. Pediatr Emerg Care 2016. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.