Abstract
Objective
To assess the effectiveness of arthroscopic versus mini-open rotator cuff repair on function, pain and range of motion at 3-, 6- and 12-month follow ups.
Design
Systematic review and meta-analysis of randomized controlled trials.
Setting
Clinical setting.
Participants
Patients 18 years and older with a rotator cuff tear.
Intervention/Comparison
Arthroscopic/mini-open rotator cuff repair surgery followed by post operative rehabilitation.
Main outcome measures
Function and pain.
Results
Six RCTs (n = 670) were included. The pooled results, demonstrated no significant difference between arthroscopic and mini open approach to rotator cuff repair on function (very low quality, 4 RCTs, 495 patients, SMD 0.00, 3-month; very low quality, 4 RCTs, 495 patients, SMD -0.01, 6-month; very low quality, 3 RCTs, 462 patients, SMD -0.09, 12-months). For pain, the pooled results, were not statistically different between groups (very low quality, 3 RCTs, 254 patients, MD -0.21, 3-month; very low quality, 3 RCTs, 254 patients, MD -0.03, 6-month; very low quality, 2 RCTs, 194 patients, MD -0.35, 12-months).
Conclusion
The effects of arthroscopic compared to mini-open rotator cuff repair, on function, pain and range of motion are too small to be clinically important at 3-, 6- and 12-month follow ups.
Introduction
Across the general population, rotator cuff tears impact 1 in 5 individuals, and 1 in 3 of those with shoulder symptoms[1]. Rotator cuff tears are more prevalent in older adults, those involved in heavy labor, males as well as individuals with previous history of injury[1]. Studies have demonstrated that surgical interventions including mini-open or arthroscopic repairs to offer satisfactory outcomes [2–4]. The mini-open has been considered the gold standard technique, costs significantly less, and proved to attain good to excellent outcomes in 90% of patients [5–8]. On the other hand, factors such as lower postoperative pain, quicker recovery time, and superior cosmetic results have steered surgeons’ preferences to choosing an arthroscopic technique based on the to emerging evidence [9–11]. However, there is no consensus on whether one technique offers superior outcomes.
To date, three systematic reviews (SRs) have examined the effectiveness of clinical outcomes in patients with rotator cuff tears undergoing arthroscopic vs mini-open rotator cuff repairs [2–4] The Shan et al. (2014) review of 12 studies (3 RCTs, 9 observational), and the Huang et al. (2016) review of 18 studies (4 RCTs, 14 observational), both concluded that there were no differences in outcomes between the arthroscopic and mini-open rotator cuff repair techniques [2–3]. However, in these reviews, studies were pooled irrespective of their design (RCT and observational), which greatly limits our confidence in its effect estimates [2–3] Furthermore, the risk of bias in the included studies were not assessed. A third review by Ji et al. (2015), included 5 RCTs and again concluded that there were no differences in outcomes at the end of follow-up between the arthroscopic and mini-open rotator cuff repair techniques [4]
While the review by Ji et al. (2015) provides valuable insights, it has important limitations. For example, trials were pooled and meta-analyses conducted based on the last follow-up time point reported (range: 6–34 months), which might have in turn contributed to the high levels of heterogeneity in the pooled analyses [12]. The effectiveness of arthroscopic versus mini-open rotator cuff repair on outcomes function, pain and range of motion, at 3-, 6- and 12-month follow ups were not assessed. Furthermore, the review failed to provided ratings of the quality of the evidence across each outcome, according to Grading of Recommendations, Assessment, Development and Evaluation (GRADE) guidelines [13]. Therefore, the purpose of this review was to conduct a systematic review with meta-analysis that addresses the reported limitations of the aforementioned reviews.
The objectives of this review were
to quantify the effects of arthroscopic versus mini-open rotator cuff repair on function, pain and range of motion at 3-, 6- and 12-month follow ups,
to rate the quality of the body of literature that compares the effectiveness of arthroscopic versus mini-open rotator cuff repair according to GRADE guidelines across each outcome.
Methods
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and Cochrane collaboration guidelines [14–15]. (S1 PRISMA Checklist) PROSPERO registration number: CRD 42018097325.
Eligibility criteria
Studies were included in this systematic review if the below criteria were met [2–4]:
Design: randomized controlled trial (RCT) in English published in a peer reviewed journal between January 1998 –July 2019,
Participants: patients 18 years and older with a rotator cuff tear,
Intervention/ Comparison: trials that compared patients who underwent arthroscopic or mini-open rotator cuff repair followed by post operative rehabilitation,
Outcomes: function/disability, pain and shoulder range of motion.
Studies that included patients with degenerative arthritis, rheumatoid arthritis of glenohumeral joint, adhesive capsulitis/ shoulder fractures / previous surgery, that were conference abstract and posters were excluded from this systematic review [2–4].
Information sources
We conducted systematic electronic searches to identify relevant randomized controlled trials in MEDLINE, EMBASE, CINAHL and Google scholar from January 1998 to July 2019. Several different combinations of keywords were used, such as: “rotator cuff repair”, “randomized controlled trials”, “arthroscopic surgery”, “mini-open surgery”, “rehabilitation after arthroscopic”, “rehabilitation after mini-open”, “effectiveness of arthroscopic”, “effectiveness of mini-open”. In addition, we also performed a search in the clinical trial registers catalogues (ClinicalTrials.gov, EU registry and ISRCTN registry), and carried out a manual search of the reference lists of the previous systematic reviews and the references of all the included articles.
Study selection
Two independent reviewers (GN and ND) carried out the systematic electronic searches in each database. Duplicate studies were identified and removed. Next, we independently screened the titles and abstracts and retrieved in full text any article marked include or uncertain by either reviewer. Finally, we conducted an independent full text review to determine final eligibility. In case of disagreement, a third reviewer; the most experienced member (JM), provided a consensus through discussion.
Data collection process
Two independent researchers (GN and ND) extracted the data from the eligible trials. In case of disagreement, a third reviewer (JM), provided a consensus through discussion. Data extraction included the author, year, study population, sample size, age, intervention/comparison group, follow up periods, primary and secondary outcomes and the protocol for postoperative therapy. When insufficient data were presented, GN contacted the authors by email and requested further data.
Assessment of risk of bias in individual studies
Two independent review authors (GN and ND) assessed the trials for risk of bias. In case of disagreement, a third reviewer (JM), provided a consensus through discussion. The risk of bias assessment was performed using the Cochrane Risk of Bias tool [14]. The Cochrane Risk of Bias tool is based on 7 items, random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other bias [14]. The other bias category was defined as trials that did not include statements on sources of funding and potential sources of conflicts of interest. We then rated the adequacy of each of the seven risk of bias domains as “low”, “unclear” or “high” risk according to criteria provided in the Cochrane Handbook for Systematic Reviews of Interventions [14]. (S1 Table).
Assessing the quality of evidence
We used the GRADE approach for systematic reviews, to assess the quality of evidence related to each outcome to summarize the extent of our confidence in the estimates of the effect[16–21]. The GRADE approach considers the risk of bias, publication bias, consistency of findings, precision, and the applicability of the overall body of literature to provide a rating of quality of evidence (high, moderate, low, or very low) per outcome [16–21].
Summary measures
To quantify and interpret our data, a minimally clinically important difference (MCID) of 1.4 points (0–10) for pain [22], a standard deviation of 0.5 points for function [23], 11.7 degrees for active shoulder forward flexion range of motion and 4.9 degrees for active shoulder external rotation range of motion were used [24] Timing of outcome assessment were categorised as 3 months, 6-months and 12-months only.
Subgroup analysis and exploring heterogeneity
In the presence of heterogeneity, we planned to perform the following subgroup analyses (a priori): trials at low risk of bias (low risk of bias in allocation concealment and blinding of outcome assessor if objective outcomes were used) would show a smaller effect size, size of the tendon tear and postoperative therapy received. An I2 estimate of at least 50% and a statistically significant Chi2 statistic (P = 0.10) was interpreted as evidence of a substantial problem with heterogeneity [25].
Synthesis of results
We performed 12 meta-analyses of trials comparing arthroscopic vs mini open repair, using the outcome function, whether reported by WORC, DASH or Constant; pain, reported by VAS; and range of motion, at 3-, 6- and 12-month follow ups. We used the Review Manager 5.3 (RevMan 5.3) software to conduct our review and a random-effects model to pool outcomes. For outcomes of the same construct (function) that were measured using a different metric, we used the standardized mean difference (SMD). If all eligible trials measured an outcome using the same metric (pain, flexion and external range of motion), we used a weighted mean difference (WMD).
Results
Study selection
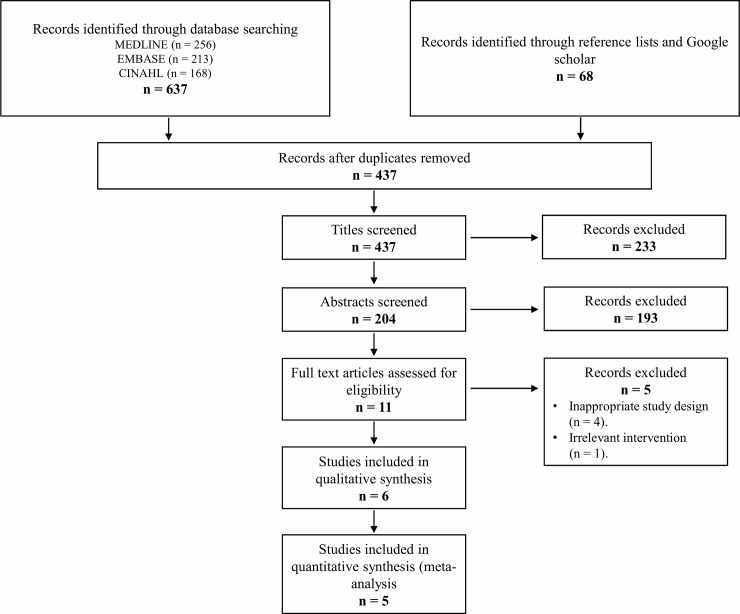
Initially, our search yielded 705 publications. After removal of the duplicates, 437 articles remained and were screened using their title and abstract; leaving 11 articles selected for full text review. Of these, 6 RCTs were eligible [26–31]. The flow of studies through the selection process is presented in Fig 1.
Fig 1. Selection of studies for inclusion in the systematic review.
Study characteristics
The 6 eligible RCTs were conducted between 2011 and 2018 and included 670 patients (337 arthroscopic and 333 mini-open) [26–31]. Study size ranged from 34 to 274 patients. Trials were conducted in Japan, Germany, South Korea, Netherlands, China and Canada[26–31]. Only one out of the six trials were registered in a clinical trials register[29]. In addition, 50% of the trials (n = 3) did not include statements on sources of funding or potential sources of conflicts of interest [26,30–31]. A summary description of all the included RCTs is displayed in Table 1.
Table 1. Summary of included randomized controlled trials (RCTs) studies.
| Study | Country | Population | Groups | Outcomes | Follow ups | Postoperative therapy (AR & MO) |
|---|---|---|---|---|---|---|
| Kasten et al. (2011) [27] | Germany | 34 patients with isolated rupture of the supraspinatus tendon (various degrees). | AR: 17 (9 men, 8 women; 60.1 ± 8.6 yrs.). MO: 17 (12 men, 5 women; 60.1 ± 9 yrs.) | Pain levels (VAS 0–10). Function (Constant). Pain and ADL (ASES). Range of motion. Patient satisfaction. | 1–12 weeks. 3, 6 months. 3, 6 months. 3, 6 months. 6 months | Four weeks abduction pillow with 30° of abduction and passive ROM exercises by a physiotherapist. Active ROM of the arm without limitations was allowed. Patients continued home exercises with a frequency of 2.5×/week in the AR group and 2.6×/week in the MO group. |
| Cho et al. (2012) [26] | South Korea | 60 patients scheduled to undergo repair for rotator cuff tears smaller than 3 cm. | AR: 30 (17 men, 13 women; 55.5 ± 7.8 yrs.). MO: 30 (17 men, 13 women; 56.2 ± 7.9 yrs.) | Pain levels (VAS 0–10). Range of motion. | 1–5 days, 2,6 weeks, 3 and 6 months. 5 days, 6 weeks, 3 and 6 months. | Wearing an abduction brace, patients engaged in pendulum and continuous passive motion machine exercises until postoperative day 5, and then passive range-of-motion exercises were started. Active range-of motion exercises were started at 6 weeks postoperatively, muscle-strengthening exercises were started at 3 months, and occupational or sports activities were started at 6 months. |
| Van der Zwaal et al. (2013) [30] | Netherlands | 95 patients with full-thickness rotator cuff tears. | AR: 47 (29 men, 18 women; 57.2 ± 8 yrs.). MO: 48 (28 men, 20 women; 57.8 ± 7.9 yrs.) | Pain levels (VAS 0–10). Range of motion. Function (Dash, Constant). | 6, 12, 26 and 52 weeks | Active exercises of the elbow, wrist, and hand were encouraged immediately. The rehabilitation protocol consisted of active abduction in the scapular plane limited to 70° and 0° of external rotation in the first 4 to 6 weeks as tolerated. After this, active range of motion exercises were started. When the patient was free of pain, scapula and rotator cuff isotonic strengthening exercises were initiated. |
| Zhang et al. (2014) [31] | China | 108 patients with partial & full thickness rotator cuff tears. | AR: 55 (28 men, 27 women; 53.9 yrs.) MO: 53 (27 men, 26 women; 54.2 yrs.) | Pain, function, range of motion, strength, and patient satisfaction (UCLA). Pain and ADL (ASES). Muscle strength. Range of motion. | mean of 29.4 months (range 24–35 months). | Continuous passive motion machine exercise was initiated from the first day after surgery. Patients used the machine for 2 h a day until discharge from the hospital. The arc of motion of the continuous passive motion was maintained within the comfortable range, which was < 80°elevation. The gentle pendulum exercise was started from the third to fifth day and continued to the first post-operative visit, which was 3 weeks after surgery. Thereafter, the passive and active assisted range of motion exercises were started using a rope and pulley. The rehabilitation was continued for 6 months. |
| Liu et al. (2017) [28] | China | 99 patients with full thickness rotator cuff tears. | AR: 50 (25 men, 25 women; 53.5 ± 4.3 yrs.). MO: 49 (24 men, 25 women; 52.5 ± 5 yrs.) | Pain levels (VAS 0–10). Range of motion. Function (Dash, Constant). | 3 days, 1,2 weeks, 1,3,6 months and 1 year. | Wearing an abduction brace, patients engaged in pendulum and continuous passive motion machine exercises until postoperative day 5, and then passive range-of-motion exercises were started. Active range-of-motion exercises were started at 6 weeks postoperatively, muscle-strengthening exercises were started at 3 months, and occupational or sports activities were started at 6 months. |
| MacDermid et al. (2019) [29] | Canada | 274 patients with small or medium rotator cuff tears. | AR: 138 (85 men, 53 women; 55.8 ± 8.5 yrs.). MO: 136 (80 men, 56 women; 54.6 ± 10.1 yrs.) | Function / quality of life (WORC). Pain and ADL (ASES, SPADI). Health related quality of life (SF-12). Range of motion. Strength. | 6 weeks, 3,6,12,18 and 24 months. | Standardized rehabilitation protocol of progressive mobilization and strengthening, which was semi-specific and adapted to patient presentation by their physical therapist. Adherence was monitored to rehab milestones at 2 weeks, 6 weeks and 3 months postoperative by asking the physical therapist to report the date when the patient was no longer wearing their sling, when active-assisted, strengthening, and functional endurance exercises had begun. The therapist was also asking to indicate whether the patient was compliant with activity precautions throughout recovery, whether the patient was progressing as expected and to describe any off-protocol or worrisome findings. |
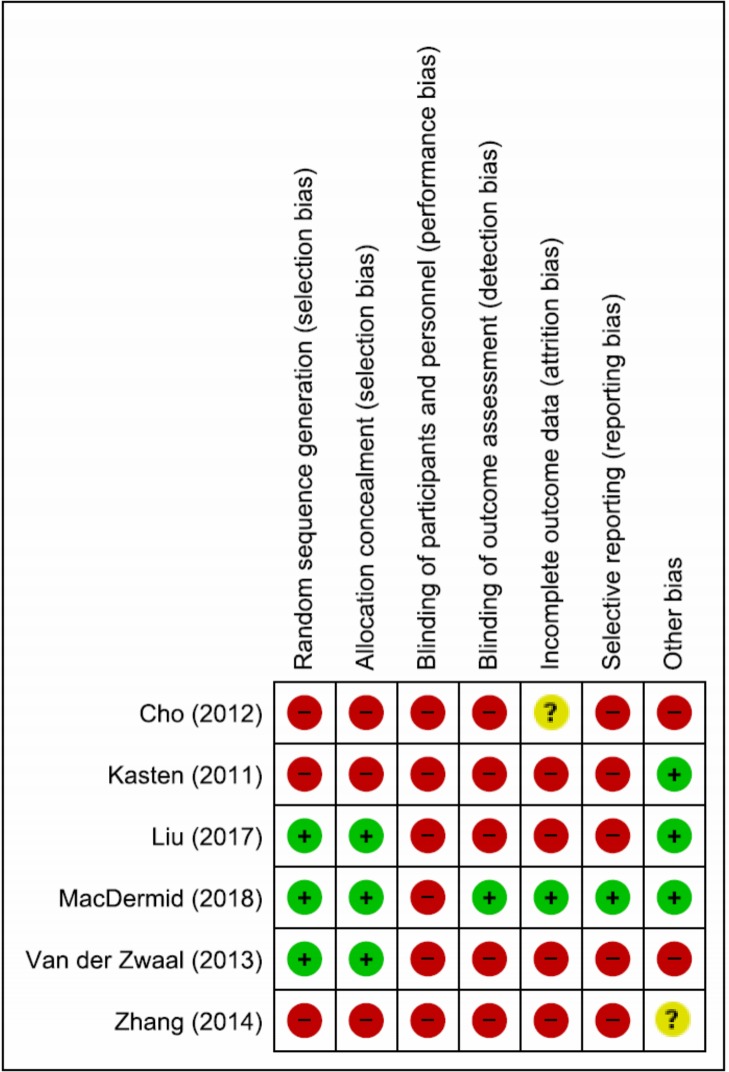
Risk of bias assessment in the individual studies
The risk of bias assessment is presented in Fig 2. Performance bias (lack of or inadequate blinding of participants who could influence how interventions, including co-interventions are performed/administered) was rated at high risk in all the included trials (n = 6)[26–31] Detection bias (lack of or inadequate blinding of participants who could influence the measurement or interpretation of outcomes) and Selective Reporting bias were rated at high risk in five trials[26, 27, 28, 30–31]. Selection bias and attrition bias (significant or imbalanced missing outcome data) were rated at high risk in three [26,27,31], and four trials respectively [26, 28, 30–31]. Other biases (RCTs with no statements on sources of funding/conflicts of interest) were rated at high risk in two trials[26,30]. Overall, all six included RCTs were rated at high risk of bias[26–31].
Fig 2. Risk of bias summary: Review authors’ judgements about each risk of bias item for each included study.
GRADE Evidence Profile (EP) and Summary of Findings (SoF)
The EP (Table 2) displays a detailed quality assessment and includes a judgment of each factor that determined the quality of evidence for each outcome. The SoF tables (Tables 3–5) include an assessment of the quality of evidence for each outcome.
Table 2. Grade evidence profile: Arthroscopic vs mini-open for patients with rotator cuff tears.
| Quality Assessment | Summary of Findings | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Outcome (No. of studies; design) |
Limitations | Inconsistency | Indirectness | Imprecision | Publication Bias | Mini-open | Arthroscopic | SMD / MD (95% CI) | Quality |
| Function at 3 months (4 RCTs) | Serious limitations | No serious inconsistency | No serious indirectness | Serious imprecisions | Likely | 247/495 | 248/495 | SMD 0.00 (-0.18–0.18) | ⊕⊝⊝⊝ very low |
| Function at 6 months (4 RCTs) | Serious limitations | No serious inconsistency | No serious indirectness | Serious imprecisions | Likely | 247/495 | 248/495 | SMD -0.01 (-0.23–0.21) | ⊕⊝⊝⊝ very low |
| Function at 12 months (3 RCTs) | Serious limitations | No serious inconsistency | No serious indirectness | Serious imprecisions | Likely | 231/462 | 231/462 | SMD -0.09 (-0.28–0.09) | ⊕⊝⊝⊝ very low |
| Pain at 3 months (3 RCTs) | Serious limitations | No serious inconsistency | No serious indirectness | Serious imprecisions | Likely | 127/254 | 127/254 | MD -0.21 (-0.91–0.50) | ⊕⊝⊝⊝ very low |
| Pain at 6 months (3 RCTs) | Serious limitations | No serious inconsistency | No serious indirectness | Serious imprecisions | Likely | 127/254 | 127/254 | MD -0.03 (-0.25–0.19) | ⊕⊝⊝⊝ very low |
| Pain at 12 months (2 RCTs) | Serious limitations | No serious inconsistency | No serious indirectness | Serious imprecisions | Likely | 97/194 | 97/194 | MD -0.35 (-1.02–0.31) | ⊕⊝⊝⊝ very low |
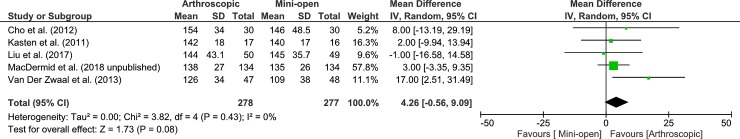
| ROM–Forward flexion at 3 months (5 RCTs) | Serious limitations | No serious inconsistency | Serious indirectness | Serious imprecisions | Likely | 277/555 | 278/555 | MD 4.26 (-0.56–9.09) | ⊕⊝⊝⊝ very low |
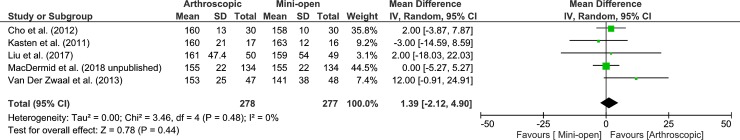
| ROM–Forward flexion at 6 months (5 RCTs) | Serious limitations | No serious inconsistency | Serious indirectness | Serious imprecisions | Likely | 277/555 | 278/555 | MD 1.39 (-2.12–4.90) | ⊕⊝⊝⊝ very low |
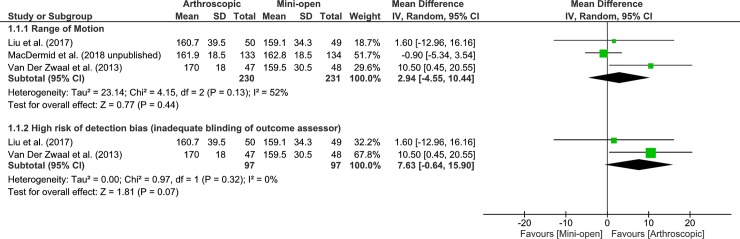
| ROM–Forward flexion at 12 months (3 RCTs) | Serious limitations | Serious inconsistency | Serious indirectness | Serious imprecisions | Likely | 231/461 | 230/461 | MD 2.94 (-4.55–10.44) | ⊕⊝⊝⊝ very low |
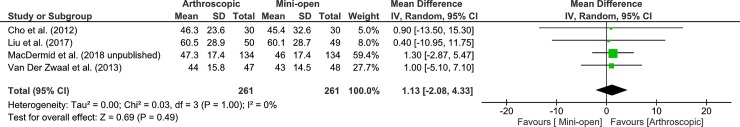
| ROM–External Rotation at 3 months (4 RCTs) | Serious limitations | No serious inconsistency | Serious indirectness | Serious imprecisions | Likely | 261/522 | 261/522 | MD 1.13 (-2.08–4.33) | ⊕⊝⊝⊝ very low |
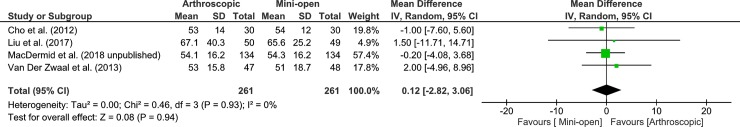
| ROM–External Rotation at 6 months (5 RCTs) | Serious limitations | No serious inconsistency | Serious indirectness | Serious imprecisions | Likely | 261/522 | 261/522 | MD 0.12 (-2.82–3.06) | ⊕⊝⊝⊝ very low |
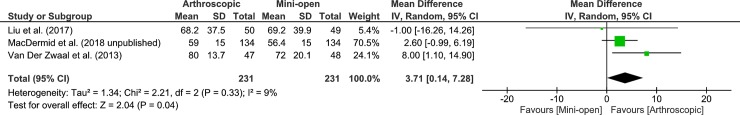
| ROM–External Rotation at 12 months (3 RCTs) | Serious limitations | No serious inconsistency | Serious indirectness | Serious imprecisions | Likely | 231/462 | 231/462 | MD 3.71 (0.14–7.28) | ⊕⊝⊝⊝ very low |
Table 3. Summary of findings.
Arthroscopic vs open-mini repair for rotator cuff tears (3-month).
| Population: patients with rotator cuff tears. Settings: inpatient clinics. Intervention: arthroscopic rotator cuff repair. Comparison: mini-open rotator cuff repair. Follow up: 3-months. | |||
|---|---|---|---|
| Outcomes | SMD / MD (95% C.I.) | No of participants (studies) | Quality of the evidence (GRADE) |
| Function: DASH, Constant, WORC: (0 to 100). Higher values indicate better function | SMD 0.00 (-0.18–0.18) | 495 (4 studies) | ⊕⊝⊝⊝ very low1,2,4 |
| Pain: VAS (0–10) Lower values indicate improved pain. | MD -0.21 (-0.91–0.50) | 254 (3 studies) | ⊕⊝⊝⊝ very low1,2,4 |
| Range of motion: (forward flexion—degrees) Higher values indicate better range of motion. | MD 4.26 (-0.56–9.09) | 555 (5 studies) | ⊕⊝⊝⊝ very low1,2,3,4 |
| Range of motion: (external rotation—degrees) Higher values indicate better range of motion. | MD 1.13 (-2.08–4.33) | 522 (4 studies) | ⊕⊝⊝⊝ very low1,2,3,4 |
1We downgraded by one level due to high risk of bias.
2We downgraded by one level due to a relatively small sample size.
3We downgraded by one level due to indirectness (surrogate outcomes).
4We downgraded by one level due to publication bias.
Abbreviations: VAS; visual analogue scale, DASH; Disabilities of Arm, Shoulder and Hand, WORC; western Ontario rotator cuff index, SMD; standardized mean difference, MD; mean difference, CI; confidence interval.
Table 5. Summary of findings.
Arthroscopic vs open-mini repair for rotator cuff tears (12-month).
| Population: patients with rotator cuff tears. Settings: inpatient clinics. Intervention: arthroscopic rotator cuff repair. Comparison: mini-open rotator cuff repair. Follow up: 12-months. | |||
|---|---|---|---|
| Outcomes | SMD / MD (95% C.I.) | No of participants (studies) | Quality of the evidence (GRADE) |
| Function: DASH, WORC: (0 to 100). Higher values indicate better function | SMD -0.09 (-0.28–0.09) | 462 (3 studies) | ⊕⊝⊝⊝ very low1,2,4 |
| Pain: VAS (0–10) Lower values indicate improved pain. | MD -0.35 (-1.02–0.31) | 194 (2 studies) | ⊕⊝⊝⊝ very low1,2,4 |
| Range of motion: (forward flexion—degrees) Higher values indicate better range of motion. | MD 2.94 (-4.55–10.44) | 461 (3 studies) | ⊕⊝⊝⊝ very low1,2,3,4,5 |
| Range of motion: (external rotation—degrees) Higher values indicate better range of motion. | MD 3.71 (0.14–7.28) | 462 (3 studies) | ⊕⊝⊝⊝ very low1,2,3,4 |
1We downgraded by one level due to high risk of bias.
2We downgraded by one level due to a relatively small sample size.
3We downgraded by one level due to indirectness (surrogate outcomes).
4We downgraded by one level due to publication bias.
5We downgraded by one level due to inconsistency.
Abbreviations: VAS; visual analogue scale, DASH; Disabilities of Arm, Shoulder and Hand, WORC; western Ontario rotator cuff index, SMD; standardized mean difference, MD; mean difference, CI; confidence interval.
Table 4. Summary of findings.
Arthroscopic vs open-mini repair for rotator cuff tears (6-month).
| Population: patients with rotator cuff tears. Settings: inpatient clinics. Intervention: arthroscopic rotator cuff repair. Comparison: mini-open rotator cuff repair. Follow up: 6-months. | |||
|---|---|---|---|
| Outcomes | SMD / MD (95% C.I.) | No of participants (studies) | Quality of the evidence (GRADE) |
| Function: DASH, Constant, WORC: (0 to 100). Higher values indicate better function | SMD—0.01 (-0.23–0.21) | 495 (4 studies) | ⊕⊝⊝⊝ very low1,2,4 |
| Pain: VAS (0–10) Lower values indicate improved pain. | MD -0.03 (-0.25–0.19) | 254 (3 studies) | ⊕⊝⊝⊝ very low1,2,4 |
| Range of motion: (forward flexion—degrees) Higher values indicate better range of motion. | MD 1.39 (-2.12–4.90) | 555 (5 studies) | ⊕⊝⊝⊝ very low1,2,3,4 |
| Range of motion: (external rotation—degrees) Higher values indicate better range of motion. | MD 0.12 (-2.82–3.06) | 522 (4 studies) | ⊕⊝⊝⊝ very low1,2,3,4 |
1We downgraded by one level due to high risk of bias.
2We downgraded by one level due to a relatively small sample size.
3We downgraded by one level due to indirectness (surrogate outcomes).
4We downgraded by one level due to publication bias.
Abbreviations: VAS; visual analogue scale, DASH; Disabilities of Arm, Shoulder and Hand, WORC; western Ontario rotator cuff index, SMD; standardized mean difference, MD; mean difference, CI; confidence interval.
Participants
Among the eligible RCTs, one recruited patients with an isolated rupture of the supraspinatus tendon (various degrees)[27], one included patients with rotator cuff tears smaller than 3 cm[26], two included patients with full-thickness rotator cuff tears[28,30], one recruited patients with partial and full thickness rotator cuff tears[31], and one included patients with small or medium rotator cuff tears[29].
Outcomes
Pain levels were measured using a Visual Analogue Scale (VAS)[26,27,28,30]. Function was measured using DASH[28,30], Constant[27,28,30] and WORC[29]. Range of motion, in degrees was assessed in all six trials[26–31]. The follow-up period was up to 41 months postoperatively.
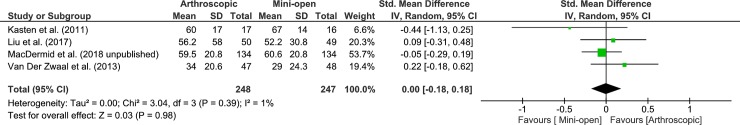
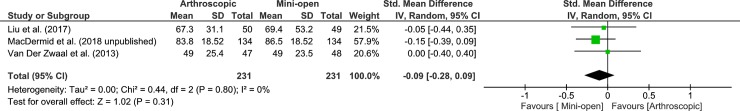
Effects on function (patient reported function)
Four studies were pooled to examine the effects of arthroscopic vs mini-open on function at 3-month follow up. The pooled results, demonstrated no significant difference between arthroscopic and mini open approach to rotator cuff repair (very low quality, 4 RCTs, 495 patients, SMD 0.00, 95% CI: -0.18 to 0.18, p = 0.98, Fig 3). We found similar results at 6-month follow up, (very low quality, 4 RCTs, 495 patients, SMD -0.01, 95% CI: -0.23 to 0.21, p = 0.93, Fig 4) and at 12-month follow up, (very low quality, 3 RCTs, 462 patients, SMD -0.09, 95% CI: -0.28 to 0.09, p = 0.31, Fig 5). Heterogeneity was low at 3 and 6 months and absent at 12 months. Given that an MCID is approximately 0.5 SD[23], and that the 95% CIs at each follow up exclude the MCID of 0.5 SD, for majority of patients either approach to rotator cuff repair will result in superior functional outcomes (12 month arthroscopic mean function 66.7/100; mini-open mean function 68.3/100).
Fig 3. Forest plot of comparison: Arthroscopic vs Open-mini, 3 months after surgery–rotator cuff repair, outcome: Function (DASH, Constant, WORC), 4 RCTs.
Higher values indicate better/improved function.
Fig 4. Forest plot of comparison: Arthroscopic vs Open-mini, 6 months after surgery–rotator cuff repair, outcome: Function (DASH, Constant, WORC), 4 RCTs.
Higher values indicate better/improved function.
Fig 5. Forest plot of comparison: Arthroscopic vs Open-mini, 12 months after surgery–rotator cuff repair, outcome: Function (DASH, WORC), 3 RCTs.
Higher values indicate better/improved function.
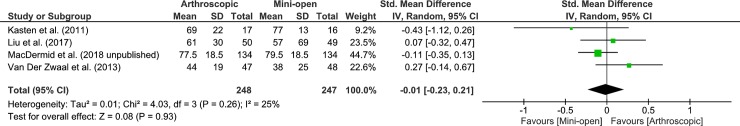
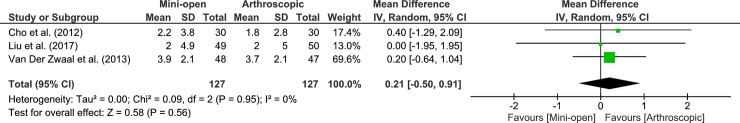
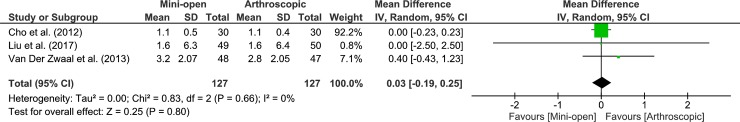
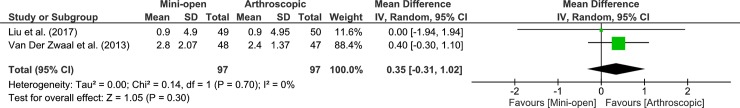
Effects on pain (patient reported pain)
Three studies were pooled to examine the effects of arthroscopic vs mini-open on pain levels at 3-month follow up. The pooled results, were not statistically different between groups (very low quality, 3 RCTs, 254 patients, MD -0.21, 95% CI: -0.91 to 0.50, p = 0.56, Fig 6). We found similar results at both 6- and 12-month follow ups, (very low quality, 3 RCTs, 254 patients, MD -0.03, 95% CI: -0.25 to 0.19, p = 0.80, Fig 7; very low quality, 2 RCTs, 194 patients, MD -0.35, 95% CI: -1.02 to 0.31, p = 0.30, Fig 8) respectively. Heterogeneity was absent for all analyses. Because the 95% CIs at each follow up exclude the MCID of 1.4 points on a 10-point scale[22], it is extremely unlikely that either approach to rotator cuff repair will result in lower pain levels.
Fig 6. Forest plot of comparison: Arthroscopic vs Open-mini, 3 months after surgery–rotator cuff repair, outcome: Pain (VAS 0–10), 3 RCTs.
Lower values indicate better/improved pain.
Fig 7. Forest plot of comparison: Arthroscopic vs Open-mini, 6 months after surgery–rotator cuff repair, outcome: Pain (VAS 0–10), 3 RCTs.
Lower values indicate better/improved pain.
Fig 8. Forest plot of comparison: Arthroscopic vs Open-mini, 12 months after surgery–rotator cuff repair, outcome: Pain (VAS 0–10), 2 RCTs.
Lower values indicate better/improved pain.
Effects on forward flexion range of motion (performance-based function)
Five studies were pooled to examine the effects of arthroscopic vs mini-open on shoulder forward flexion range of motion at 3-month follow up. The pooled results, showed no statistically significant difference between groups (very low quality, 5 RCTs, 555 patients, MD 4.26, 95% CI: -0.56 to 9.09, p = 0.08, Fig 9). Our findings were similar at both the 6- and 12-month follow ups, (very low quality, 5 RCTs, 555 patients, MD 1.39, 95% CI: -2.12 to 4.90, p = 0.44, Fig 10; very low quality, 3 RCTs, 461 patients, MD 2.94, 95% CI: -4.55 to 10.44, p = 0.44, Fig 11) respectively. Heterogeneity was absent in the analysis of 3 and 6 month follow up, and because the 95% CIs exclude the MCID of 11.7°[24], it is extremely unlikely that either approach to rotator cuff repair will result in better flexion range of motion. Heterogeneity was substantial in the analysis of 12 month follow up and our subgroup analysis of the two studies at high risk of detection bias indicated that the likely cause of substantial heterogeneity was due to inadequate blinding of outcome assessors. The one remaining MacDermid et al. (2018) study with adequate blinding of outcome assessors showed no statistically significant difference between groups (1 RCT, 267 patients, MD -0.90, 95% CI: -5.34 to 3.54, p = 0.69) and because the 95% CIs exclude the MCID of 11.7 degrees[24], it is unlikely that either approach to rotator cuff repair will result in better flexion range of motion.
Fig 9. Forest plot of comparison: Arthroscopic vs Open-mini, 3 months after surgery–rotator cuff repair, outcome: ROM (Forward Flexion°), 5 RCTs.
Higher values indicate better/improved ROM.
Fig 10. Forest plot of comparison: Arthroscopic vs Open-mini, 6 months after surgery–rotator cuff repair, outcome: ROM (Forward Flexion°), 5 RCTs.
Higher values indicate better/improved ROM.
Fig 11. Forest plot of comparison: Arthroscopic vs Open-mini, 12 months after surgery–rotator cuff repair, outcome: ROM (Forward Flexion°), 3 RCTs.
1.1.2 Subgroup analysis by high risk of detection bias, 2 RCTs. Higher values indicate better/improved ROM.
Effects on external rotation range of motion (performance-based function)
Five studies were pooled to examine the effects of arthroscopic vs mini-open on shoulder external rotation range of motion at 3-month follow up. The pooled results, showed no statistically significant difference between groups (very low quality, 4 RCTs, 522 patients, MD 1.13, 95% CI: -2.08 to 4.33, p = 0.49, Fig 12). Our findings were similar at the 6-month follow up (very low quality, 4 RCTs, 522 patients, MD 0.12, 95% CI: -2.82 to 3.06, p = 0.94, Fig 13). However, at 12-month follow up the pooled results showed statistically significant difference between groups (very low quality, 3 RCTs, 462 patients, MD 3.71, 95% CI: 0.14 to 7.28, p = 0.04, Fig 14). Heterogeneity was absent in the analysis of 3 and 6 month follow up and low at 12 months. Given the MCID of 4.9 degrees[24], we can confidently rule out the possibility that surgical approach will cause a difference in external rotation range of motion at 6 months. However, we are unable to make this same declaration for the results at 3 and 12 months as it remains possible that an arthroscopic approach could offer superior outcomes in terms of external rotation range of motion. More data is required to make a definitive conclusion.
Fig 12. Forest plot of comparison: Arthroscopic vs Open-mini, 3 months after surgery–rotator cuff repair, outcome: ROM (External Rotation°), 5 RCTs.
Higher values indicate better/improved ROM.
Fig 13. Forest plot of comparison: Arthroscopic vs Open-mini, 6 months after surgery–rotator cuff repair, outcome: ROM (External Rotation°), 4 RCTs.
Higher values indicate better/improved ROM.
Fig 14. Forest plot of comparison: Arthroscopic vs Open-mini, 12 months after surgery–rotator cuff repair, outcome: ROM (External Rotation°), 3 RCTs.
Higher values indicate better/improved ROM.
Discussions
We aimed to summarise the current evidence of the effects of arthroscopic vs mini-open rotator cuff repair on clinical outcomes. Our forest plots for flexion and external rotation range of motion outcomes displayed that when considering the results of individual studies (not pooled analyses), there is a trend, indicating that arthroscopic treatment may yield better outcomes. However, upon meta-analysis, we found no clinically important differences in function, pain, flexion or external rotation range of motion at 3-, 6- or 12-month follow ups.
Quality of the evidence
The rating of very low-quality evidence per outcome across trials was based on the judgement of serious limitations (risk of bias), serious imprecision and likely publication bias in all the outcomes across trials. All six trials identified in this review were rated at high risk of bias. However, we downgraded the evidence only by one level due to the fact that we did not find statistical differences between groups, suggesting that the included studies may not have been biased. Furthermore, serious indirectness was judged as an additional factor in rating down the quality of evidence for half the outcomes across trials. The very low-quality evidence synthesised limits our confidence in the effect estimates. However, given that MCID thresholds for function, pain and range of motions, as well as the 95% CI excluding these thresholds, it is unlikely that either approach to rotator cuff repair will result in superior clinical outcomes.
Agreements / Disagreements with other reviews
The results of our systematic review and meta-analysis could not directly be compared to the findings of Shan et al. (2014), Huang et al. (2016) or Ji et al. (2015) reviews[2–4]. The Shan et al. (2014) review of 12 studies (3 RCTs, 8 retrospective studies, 1 prospective study) concluded that there were no differences in clinical outcomes of pain, function and range of motion between the arthroscopic and mini-open rotator cuff repair approaches[4]. The Huang et al. (2016) review of 18 studies (4 RCTs, 12 retrospective studies, 2 prospective study) indicated that all-arthroscopic and mini-open rotator cuff repair surgical approaches are associated with similar clinical outcomes of function, pain and range of motion and that both surgical techniques can be used interchangeably based factors such as patient and rotator tear characteristics[2]. However, it is important to note that the aforementioned reviews pooled studies to provide effect estimates irrespective of their design; RCTs were combined with prospective and retrospective observational studies. This greatly limits our confidence in the effect estimates [2,4]. Furthermore, the reviews failed to define an MCID threshold a priori, to further support their well-conducted meta-analyses and ultimately their conclusions. The Ji et al. (2015) review included 5 RCTs and concluded that there were no differences in clinical outcomes between the arthroscopic and mini-open rotator cuff repair techniques[3]. However, it is important to highlight the fact that this review pooled RCTs based on the last follow-up time point reported, which ranged from 6-months to 34-months. It is likely that the underlying reason for the high levels of heterogeneity identified in the Ji et al. (2015) review were due to the pooling of trials with such wide range of follow-ups. In addition, the review did not provide ratings of the quality of evidence and similarly failed to define an MCID threshold a priori to further support their conclusions.
Our review provides the most up-to-date state of the evidence concerning the clinical outcomes of arthroscopic vs mini-open rotator cuff repair techniques. We provided ratings of the quality of evidence according to GRADE guidelines across each outcome, included two additional large trials and provided an analysis of precision by evaluating the MCID thresholds with the 95% confidence intervals, therefore, able to make definitive conclusions for most of the included clinical outcomes. We could not provide definitive statements on whether arthroscopic approach could offer superior outcomes in terms of external rotation range of motion at 3 and 12 months because our analysis of 555 and 462 patients respectively, did not meet the criteria for our calculated Optimal Information Size of 754. As a result, it produced wider confidence intervals, therefore, MCID threshold not excluded. (S1 Fig)
Hui et al. 2017 study of 226 patients compared the immediate costs associated in patients who received mini-open and arthroscopic rotator cuff repairs and indicated that immediate costs incurred by mini-open rotator cuff technique were significantly less than those of arthroscopic technique. However, it is important to note that this was a retrospective study, and outcomes were only analysed only at 1 year follow up[32].
Implications for research
We have limited confidence in our conclusions. Future well-designed large-scale RCTs investigating the effects of arthroscopic vs mini-open rotator cuff repair techniques on clinical outcomes of function, pain and range of motion are warranted to generate high quality evidence (i.e. greater confidence) to further ensure that the true effect lies close to that of the estimate of the effect. In addition, future cost-effectiveness trials comparing the two surgical technique are warranted.
Implications for practice
Both arthroscopic and mini-open approaches to rotator cuff repair with post-operative rehabilitation are effective means of improving function, pain and shoulder range of motion in patients with rotator cuff tears. Despite the very-low quality synthesized, we continue to suggest that the difference between the two surgical techniques are too small to be clinically important in terms of improving clinical outcomes of function, pain and range of motion.
Strengths & limitations
We were mainly concerned with identifying RCTs and therefore, did not included prospective or retrospective observational studies in this review. It is possible that there might be a source of publication bias within our search strategy. Two independent reviewers conducted the electronic searches in all the major databases. Furthermore, a protocol registration was undertaken prior to the conduct of this review.
Conclusions
The effects of arthroscopic compared to mini-open rotator cuff repair, on function, pain and range of motion are too small to be clinically important at 3-, 6- and 12-month follow ups.
Supporting information
(PDF)
(PDF)
(PDF)
Abbreviations
- SRs
Systematic Reviews
- RCTs
Randomized Controlled Trials
- GRADE
Grading of Recommendations Assessment, Development and Evaluation
- PICO
Population, Intervention, Comparator, Outcome
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- MCID
Minimally Clinically Important Differences
- SMD
Standardized Response Difference
- WMD
Weighted Mean Difference
- EP
Evidence Profile
- SoF
Summary of Findings
- SD
Standard Deviations
- WORC
Western Ontario Rotator Cuff Index
- DASH
Disabilities of the Arm, Shoulder and Hand
- VAS
Visual Analogue Scale
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010; 19(1):116–20. 10.1016/j.jse.2009.04.006 [DOI] [PubMed] [Google Scholar]
- 2.Huang R, Wang S, Wang Y, Qin X, and Suna Y. Systematic Review of All- Arthroscopic Versus Mini-Open Repair of Rotator Cuff Tears: A Meta-Analysis. Sci Rep. 2016; 6: 22857 10.1038/srep22857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ji X, Bi C, Wang F and Wang Q. Arthroscopic Versus Mini-Open Rotator Cuff Repair: An Up-to-Date Meta-analysis of Randomized Controlled Trials. Arthroscopy, 2015; 31(1):118–124. 10.1016/j.arthro.2014.08.017 [DOI] [PubMed] [Google Scholar]
- 4.Shan L, Fu D, Chen K, Cai Z and Li G. All-Arthroscopic versus Mini-Open Repair of Small to Large Sized Rotator Cuff Tears: A Meta-Analysis of Clinical Outcomes. PloS One, 2014. (9):4; e94421 10.1371/journal.pone.0094421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chahal J, Van Thiel GS, Mall N, Heard W, Bach BR, Cole BJ, et al. The role of plateletrich plasma in arthroscopic rotator cuff repair: A systematic review with quantitative synthesis. Arthroscopy 2012; 28: 1718–1727. 10.1016/j.arthro.2012.03.007 [DOI] [PubMed] [Google Scholar]
- 6.Peters KS, McCallum S, Briggs L and Murrell GA. A comparison of outcomes after arthroscopic repair of partial versus small or medium-sized full-thickness rotator cuff tears. J Bone Joint Surg Am 2012;94:1078–1085. 10.2106/JBJS.J.00519 [DOI] [PubMed] [Google Scholar]
- 7.Ames JB, Horan MP, Van der Meijden OA, et al. Association between acromial index and outcomes following arthroscopic repair of full-thickness rotator cuff tears. J Bone Joint Surg Am 2012;94:1862–1869. 10.2106/JBJS.K.01500 [DOI] [PubMed] [Google Scholar]
- 8.Denard PJ, Ladermann A, Jiwani AZ and Burkhart SS. Functional outcome after arthroscopic repair of massive rotator cuff tears in individuals with pseudo-paralysis. Arthroscopy 2012;28:1214–1219. 10.1016/j.arthro.2012.02.026 [DOI] [PubMed] [Google Scholar]
- 9.Verma NN, Dunn W, Adler RS, Cordasco FA, Allen A, MacGillivray J, et al. All-arthroscopic versus mini-open rotator cuff repair: A retrospective review with minimum 2-year follow-up. Arthroscopy 2006;22:587–594. 10.1016/j.arthro.2006.01.019 [DOI] [PubMed] [Google Scholar]
- 10.Kang L, Henn RF, Tashjian RZ and Green A et al. Early outcome of arthroscopic rotator cuff repair: A matched comparison with mini-open rotator cuff repair. Arthroscopy 2007;23: 573–582:582.e1-582.e2. 10.1016/j.arthro.2007.01.011 [DOI] [PubMed] [Google Scholar]
- 11.Pearsall AWIV, Ibrahim KA and Madanagopal SG. The results of arthroscopic versus mini-open repair for rotator cuff tears at mid-term follow-up. J Orthop Surg Res 2007;2:24 10.1186/1749-799X-2-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nazari G, MacDermid JC, Bryant D and Athwal GS. The effectiveness of surgical vs conservative interventions on pain and function in patients with shoulder impingement syndrome. A systematic review and meta-analysis. Plos One, 2019, 10.1371/journal.pone.0216961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Balshem H, Helfand M, Schu ¨nemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011; 64: 401–6. 10.1016/j.jclinepi.2010.07.015 [DOI] [PubMed] [Google Scholar]
- 14.Higgins JPT, Altman DG, Gøtzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Br Med J. 2011; 343: 889–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liberati A, Altman DG, Tetzlaff J, Cynthia Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009; 339: b2700 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011; 64(4):383–94. 10.1016/j.jclinepi.2010.04.026 [DOI] [PubMed] [Google Scholar]
- 17.Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, et al. GRADE guidelines: 4. Rating the quality of evidence—Study limitations (risk of bias). J Clin Epidemiol. 2011; 64 p. 407–15. 10.1016/j.jclinepi.2010.07.017 [DOI] [PubMed] [Google Scholar]
- 18.Guyatt GH, Oxman AD, Montori V, Vist G, Kunz R, Brozek J, et al. GRADE guidelines: 5. Rating the quality of evidence—Publication bias. J Clin Epidemiol. 2011; 64(12):1277–82. 10.1016/j.jclinepi.2011.01.011 [DOI] [PubMed] [Google Scholar]
- 19.Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence—Imprecision. J Clin Epidemiol. 2011; 64(12):1283–93. 10.1016/j.jclinepi.2011.01.012 [DOI] [PubMed] [Google Scholar]
- 20.Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 8. Rating the quality of evidence—Indirectness. J Clin Epidemiol. 2011; 64(12):1303–10. 10.1016/j.jclinepi.2011.04.014 [DOI] [PubMed] [Google Scholar]
- 21.Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 7. Rating the quality of evidence—Inconsistency. J Clin Epidemiol. 2011; 64: 1294–1302. 10.1016/j.jclinepi.2011.03.017 [DOI] [PubMed] [Google Scholar]
- 22.Tashjian RZ, Deloach J, Porucznik CA, Powell AP. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg. 2009; 18:927–932. 10.1016/j.jse.2009.03.021 [DOI] [PubMed] [Google Scholar]
- 23.Norman GR, Sloan JA, Wyrwich KW. The truly remarkable universality of half a standard deviation: Confirmation through another look. Vol. 4, Expert Review of Pharmacoeconomics and Outcomes Research. 2004; 581–585. 10.1586/14737167.4.5.581 [DOI] [PubMed] [Google Scholar]
- 24.Simovitch R, Flurin PH, Wright T, Zuckerman JD and Roche CP. Quantifying success after total shoulder arthroplasty: the minimal clinically important difference. J Shoulder Elbow Surg (2018) 27, 298–305. 10.1016/j.jse.2017.09.013 [DOI] [PubMed] [Google Scholar]
- 25.Higgins JPT, and Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) The Cochrane Collaboration, 2011. Available from handbook. cochrane.org. [Google Scholar]
- 26.Cho C-H, Song K-S, Jung G-H, Lee YK and Shin HK. Early Postoperative Outcomes Between Arthroscopic and Mini-open Repair for Rotator Cuff Tears. Orthopedics. 2012;35(9): e1347–52. 10.3928/01477447-20120822-20 [DOI] [PubMed] [Google Scholar]
- 27.Kasten P, Keil C, Grieser T, Raiss P, Streich N and Loew. Prospective randomised comparison of arthroscopic versus mini-open rotator cuff repair of the supraspinatus tendon. Int Orthop. 2011;35(11):1663–70. 10.1007/s00264-011-1262-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu J, Fan L, Zhu Y, Yu H, Xu T and Li G. Comparison of clinical outcomes in all-arthroscopic versus mini-open repair of rotator cuff tears. Med (Baltimore). 2017; 96(11). 10.1097/MD.0000000000006322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.MacDermid JC, Holtby R, Razmjou H, Bryant D and JOINTS Canada. Arthroscopic versus mini-open rotator cuff repair: A Randomized Trial and Meta-analysis. Protocol number [NCT00128076]. BMC Musculoskeletal Disorders 20067:25 10.1186/1471-2474-7-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Van Der Zwaal P, Thomassen BJW, Nieuwenhuijse MJ, Lindenburg R, Swen JW and Van Arkel ER. Clinical outcome in all-arthroscopic versus mini-open rotator cuff repair in small to medium-sized tears: A randomized controlled trial in 100 patients with 1-year follow-up. Arthroscopy, 2013;29(2):266–73. 10.1016/j.arthro.2012.08.022 [DOI] [PubMed] [Google Scholar]
- 31.Zhang Z, Gu B, Zhu W, Zhu L and Li Q. Arthroscopic versus mini-open rotator cuff repair: A prospective, randomized study with 24-month follow-up. Eur J Orthop Surg Traumatol. 2014;24(6):845–50. 10.1007/s00590-013-1263-5 [DOI] [PubMed] [Google Scholar]
- 32.Hui YJ, Teo AQA, Sharma S, Tan BHM, and Prem Kumar V. Immediate costs of mini-open versus arthroscopic rotator cuff repair in an Asian population. Journal of Orthopaedic Surgery, 2017. 10.1177/2309499016684496 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(PDF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.